Abstract
Background
The association of preexisting neurocognitive impairments with perioperative neurocognitive disorders is not well-established. The objective of this study was to record incidences of perioperative neurocognitive disorders, to record changes in perioperative neurocognition, and to analyze factors of perioperative neurocognitive changes after hip joint replacement surgeries.
Material/Methods
Patients scheduled for hip joint replacement surgery were included in the test group (n=499) and patients with osteoarthritis but who were not planned for any type of surgeries were included in the control group (n=499). The cognitive tests were evaluated at the time of enrollment and at 1 week, 3 months, 1 year, and 4 years after baseline. Neurocognitive disorders for the individual parameter was defined as more than 2 SD of mean below norms for that parameter. Neurocognitive disorders were defined as a significant worst condition in at least 2 parameters out of all parameters.
Results
Compared to baseline, after 3 months the numbers of patients with perioperative neurocognitive disorders were increased (55 vs. 81, p=0.021). After 4 years, there was a significant decline in numbers of patients with perioperative neurocognitive disorders in the test group (55 vs. 3, p<0.0001). At the end of the 3-month follow-up period, elderly patients (p=0.002) and patients with preexisting neurocognitive impairments (p=0.005) had a higher incidence of perioperative neurocognitive disorders.
Conclusions
Age and preexisting neurocognitive impairments are markers predicting the risk of perioperative neurocognitive disorders.
MeSH Keywords: Attention Deficit Disorder with Hyperactivity; Commitment of Mentally Ill; Demography; Hallucinations; Surgery Department, Hospital
Background
Hip joint replacement surgery improves patient quality of life but is associated with perioperative neurocognitive disorders [1]. Stress, pain, inflammation, anesthesia, and medications make operative patients transiently ill and this is unfavorable for the brain [2]. Perioperative neurocognitive disorders affect hospital stays [3], mortalities [4], recovery [3], quality of life [5], and memory [6] of operative patients. Also, longer hospital stays lead to delirium [7] and increase the cost of treatment [2]. Preexisting neurocognitive impairments are also reported in operative patients [6]. Perioperative neurocognitive disorders are well-documented in operative patients 3 months after surgery [6]. Data on preexisting neurocognitive impairments are required to predict future risk of perioperative neurocognitive disorders at the time of surgeries [1] because the association of preoperative cognitive functions with perioperative neurocognitive disorders is not well-established [6]. Mini-Mental state examinations are recommended to identify the association of preexisting neurocognitive impairments with perioperative neurocognitive disorders [4].
This study was performed with 3 objectives in Chinese patients who undergoing hip joint replacement surgeries: to record incidences of perioperative neurocognitive disorders, to record changes in perioperative neurocognition, and to analyze factors of perioperative neurocognitive changes.
Material and Methods
Drugs
Midazolam (Seizalam) was purchased from Meridian Medical Technologies, Inc., USA. Fentanyl (Duragesic®) was purchased from Johnson & Johnson, USA. Paracetamol (Perfalgan) was purchased from Bristol-Myers Squibb, New York, USA. Low molecular weight heparin was purchased from Roche Pharmaceuticals, Basel, Switzerland. Noradrenaline (Norad) was purchased from Neon Laboratories Limited, China.
Ethical considerations and consent to participate
The study was registered in the Research Registry (www.researchregistry.com), UID No.: researchregistry4578 dated 14 November 2013. The protocol (81870857/CL/11/14 dated 11 November 2013) was approved by the Xuzhou Central Hospital review board. The study adhered to the law of China, the 2008 Declaration of Helsinki (Chinese version), and the strengthening the reporting of observational studies in epidemiology (STROBE) statement. Informed consent was signed by all participating patients before surgeries regarding anesthesia, surgeries, and publication of the study in all formats (hard or electronics) irrespective of time and languages.
Inclusion criteria
All patients age 18 years and above, admitted for the purposes of hip joint replacement surgery, were included in the test group. All patients age 18 years and above who had osteoarthritis but who were not planned for any type of surgery were included in the control group. We only included patients with 4 years of follow-up data available in the records of the institute.
Exclusion criteria
Patients who had not provided informed consent and those less than 18 years of age were excluded from the study. Patients who had Mini-Mental state examination scores less than 26 or clinical dementia scale more than 1, and ASA (American Society Anesthesiologists) physical status score IV or higher, were excluded from the test group. Patients who had been planned for surgeries were excluded from the control group. Drug abuse, chronic pain, psychiatric disorders, and psychological abnormality impair cognition function and also have confounding effects on outcomes. Therefore, such patients were excluded for the study.
Hip joint replacement surgery
All test group patients were subjected to intravenous propofol before surgeries, as well as intraoperative midazolam and fentanyl, and postoperative paracetamol infusion. The bispectral index was maintained below 60. A laryngeal mask (BD Medical Devices, Shanghai, China) was used for airway maintenance. Hypotension was controlled by noradrenaline [6]. A standard femoral neck osteotomy surgery (cemented or non-cement) was performed by orthopedic surgeons. Deep vein thrombosis prophylaxis was used.
Cohorts
Patients scheduled for hip joint replacement surgery were included in the test group (n=499) and patients with osteoarthritis but who were not scheduled for any type of surgery were included in the control group (n=499).
Mini-mental state examinations
The mental status questionnaires were performed by psychiatrists (each with at least 3 years of experience). The maximum score was 30 points [8].
Auditory-verbal learning test
The rate of learning, short-term auditory-verbal memory, retroactive interference, learning strategies, proactive interference, retention of information, and confabulation of information were evaluated by psychiatrists (each with at least 3 years of experience) [9]. The RAVLT (Rey Auditory-Verbal Learning Test) Adult Calculator was used to calculate the Auditory-Verbal Learning Test score [10], with 23 was considered as the norm value.
Trail making test
In part A, patients had to draw a line sequentially connecting 1 to 25 numbers (Supplementary Table 1), with 150 s and less was considered as the norm value. In part B, patients had to a draw line between 12 Chinese zodiacs (rat, ox, tiger, rabbit, dragon, snake, horse, goat, monkey, rooster, dog, pig) and 12 pictures (Supplementary Table 2). The time required to complete the task was the score for that part [11], with 150 s and less considered as the norm value. Both tests were performed by a trained instructor (with at least 3 years of experience) working at the institute.
Stroop color and word test
This test has 2 subtasks: congruous and incongruous. In the incongruous subtask, the color words were written in random order (pink, black, orange, and green) but printed in the same color ink (e.g., the word orange was printed in orange ink, Supplementary Figure 1). In the incongruous subtask, color words were printed in different ink color (e.g., the word pink printed in green ink, Supplementary Figure 2). Patients were required to name the color of the ink in both tasks. The time required to complete the task was the score for that part of the test [11]. The test was performed by a trained instructor (with at least 3 years of experience) working at the institute. The norm values for both tasks individually were 200 s and less for subjects age ≤70 years, 220 s and less for those age 70–80 years, and 330 s and less for those ≤80 years.
Digit symbol substitution test
This test is used to estimate the magnitude of cognitive dysfunction in patients with depressive disorder [12] and is performed to assess spatial decision-making, psychomotor speed, and motor skills. In the test, a digit (e.g., yuan) was substituted with a symbol (e.g., ¥). A total of 133 digits were presented in the test, and participants were allowed 2 min to complete it. Each correct answer had a 1-point score, with a score range of 0–133 [13]. The test was performed by a trained instructor (with at least 3 years of experience) working at the institute. A score of 80 or more was considered as the norm value.
Verbal fluency test
Patients were asked to list the names of as many animals as possible within 1 min [14]. The test was performed by a trained instructor (with at least 3 years of experience). A score of 15 or more was considered as the norm value.
All measures for neurocognitive disorders were evaluated 1 week before surgeries (baseline) in the test group and in the control group (at the time of the enrollment). In the control group, all outcome measures were evaluated at 1 week, 3 months, 1 year, and 4 years after baseline during the follow-up period. In the test group, all outcome measures were evaluated at 1 week, 3 months, 1 year, and 4 years after baseline. Preexisting neurocognitive impairments were defined as a significantly worst condition in at least 2 out of all parameters. Neurocognitive disorders for the individual parameter were defined as more than 2 SD of mean below norms for that parameter [15]. The norms of individual parameters were defined by the institute (not published). Perioperative neurocognitive disorders were defined as a significantly worst condition in at least 2 out of all parameters as compared to baseline [6].
Statistical analysis
InStat (version window) GraphPad (San Diego, CA) was used for statistical analysis. The chi-square Independence test [6] was used for categorical variables and the 2-tailed paired t test was used for continuous variables [16]. One-way analysis of variance (ANOVA) followed by Tukey multiple comparison tests (considering critical value [q] >3.858 as significant) [17] was used for postoperative outcomes at different time intervals. Univariable and multivariable analysis was performed to develop associations between the postoperative outcome measures and demographical characteristics of baseline [6]. The individual effect was evaluated by Cohen’s d defined as per norms [15]. The results were considered significant at 95% confidence level.
Results
The medical history at the time of enrollment
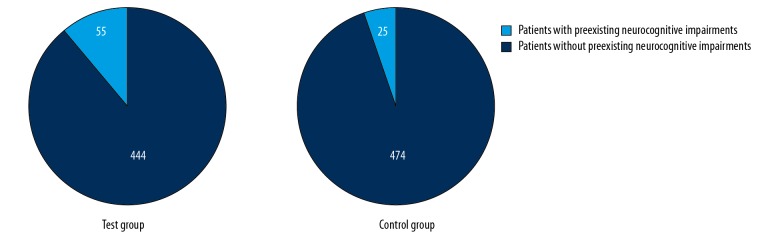
From 15 November 2013 to 1 November 2014 at the Xuzhou Central Hospital, China and the referring hospitals of China, 526 patients were admitted for hip joint replacement surgery and 527 patients were available at an outpatient setting with complaints of osteoarthritis. Among the patients who underwent hip joint replacement surgery, 15 patients had Mini-Mental state examination scores less than 26, and 12 patients had ASA physical status scores IV or more. Therefore, they were excluded from the study. Among the patients with complaints of osteoarthritis, 28 patients were planned for the surgery; therefore, they were also excluded from the study. A total of 499 patients were included in the test group and 499 patients were included in the control group. The flow diagram of the study is represented in Figure 1.
Figure 1.
Flow diagram of the study.
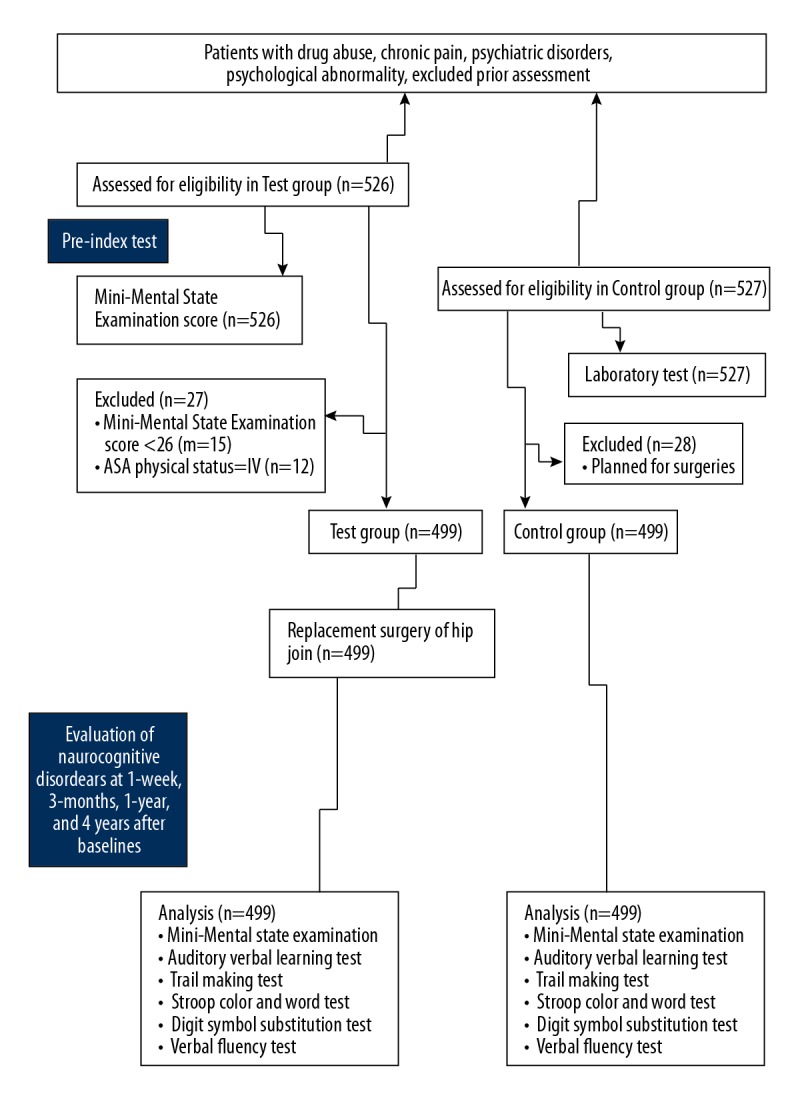
The test group was 35% male and 65% female. The control group was 29% male and 71% females. About 90% of enrolled patients were non-smokers and 25% of patients were from rural areas, while 75% of patients from an urban area of PR China. Preexisting neurocognitive impairments were higher in the test group than in the control group (p=0.0007) at the time of the enrollment (Figure 2). The other details of medical history of the enrolled patients are reported in Table 1.
Figure 2.
Distributions of preexisting neurocognitive impairments among the population. The neurocognitive disorder was defined as a significant worst condition in at least 2 parameters.
Table 1.
Demographical, social, anthropological, and neurological parameters of the enrolled patients.
| Characteristics | Group | Comparisons between groups | ||
|---|---|---|---|---|
| Test | Control | |||
| Patients included in the study (sample size) | 499 | 499 | p-Value | |
| Age (years) | Minimum | 50 | 49 | 0.193 |
| Maximum | 77 | 81 | ||
| Mean ±SD | 63.52±6.72 | 64.15±8.45 | ||
| Gender | Male | 174 (35) | 145 (29) | 0.057 |
| Female | 325 (65) | 354 (71) | ||
| Body mass index (kg/m2) | 27.45±5.11 | 27.01±5.21 | 0.178 | |
| Smoking | Smoker | 14 (3) | 21 (4) | 0.461 |
| Previous smoker | 41 (8) | 38 (8) | ||
| Non-smoker | 444 (89) | 440 (88) | ||
| Diabetes# | 45 (9) | 41 (8) | 0.735 | |
| Hypertension## | 15 (3) | 16 (3) | 0.855 | |
| Education | Under graduate | 241 (48) | 276 (55) | 0.085 |
| Graduate | 127 (25) | 111 (22) | ||
| Postgraduate | 131 (27) | 112 (23) | ||
| Residence | Rural | 125 (25) | 131 (26) | 0.717 |
| Urban | 374 (75) | 368 (74) | ||
| Mini-mental state examinations score### | 27.49±1.41 | 27.68±1.89 | 0.072 | |
| Auditory-verbal learning test score@ | 17.01±4.12 | 17.59±5.21 | 0.051 | |
| Trail making test (sec)@@ | Part A | 52.45±8.45 | 51.52±7.51 | 0.066 |
| Part B | 111.12±13.12 | 109.59±12.01 | 0.055 | |
| Stroop color and word test (sec)@@ | Congruous | 31.15±4.12 | 30.79±5.01 | 0.215 |
| Incongruous | 51.12±5.02 | 50.51±4.91 | 0.053 | |
| Digit symbol substitution test@@@ | 97.13±6.15 | 97.95±7.21 | 0.054 | |
| Verbal fluency test& | 15.17±5.15 | 15.82±5.89 | 0.064 | |
| Preexisting neurocognitive impairments&& | 55 (11)* | 25 (5) | 0.0007 | |
Random blood glucose >140 mg/dL;
Blood pressure >90/130 mmHg;
The maximum score was 30 points;
As per RAVLT Adult Calculator;
The time required to complete the task;
The score range: 0–133;
The numbers of animals listed within 1 min;
Defined as a significant worst condition in at least 2 parameters out of all parameters.
Categorial variables were represented as a number (percentage), continuous variables were represented as mean ±SD. Data of test group recorded 1 week before surgeries. The chi-square Independence test for categorical variables and two-tailed paired t test for continuous variables were used for statistical analysis. A p<0.05 was considered significant. All patients are of PR Chinese origin.
Significantly higher than the control group.
Incidences of neurocognitive disorders
In the control group, 25 patients were reported to have preexisting neurocognitive impairments at baseline. At 1 week (25 vs. 26, p=0.886), 3 months (25 vs. 31, p=0.492), and 1 year (25 vs. 40, p=0.073), there was no progression of neurocognitive disorders among the patients. However, after 4 years, neurocognitive disorders were progressively noted in the control group (25 vs. 42, p=0.043).
In the test group, 55 patients were reported to have preexisting neurocognitive impairments at baseline. As compared to baseline, at 1 week after surgeries (55 vs. 86, p=0.006) and at 3 months after surgeries (55 vs. 81, p=0.021) numbers of patients with perioperative neurocognitive disorders were increased. However, at 1 year after surgeries, there was a decreased number of patients with perioperative neurocognitive disorders as compared to preexisting neurocognitive impairments (55 vs. 15, p<0.0001), and at 4 years there was a significant decline in numbers of patients with perioperative neurocognitive disorders as compared to baseline (55 vs. 3, p<0.0001). No mortality was reported during the 4-year follow-up period in the control or the test group.
Changes in perioperative neurocognitive disorders
Perioperative neurocognitive disorders in the test group at 1-week follow-up and even after 3-month follow-up after surgeries were no different from those at baseline. However, as per the definition of neurocognitive disorders, at 4-year follow-up and even after 1-year follow-up, there was no incidence of perioperative neurocognitive disorders (Table 2).
Table 2.
Postoperative outcomes in the test group.
| Characteristics | Outcome measures | Comparisons between results | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| During the follow-up period | |||||||||||
| BL (I) | After 1 week (II) | After 3 months (III) | After 1 year (IV) | After 4 years (V) | p-Value | q-Value | |||||
| I vs. II | I vs. III | I vs. IV | I vs. V | ||||||||
| Patients included in the study (sample size) | 499 | 499 | 499 | 499 | 499 | ||||||
| Mini-mental state examinations score### | 27.49±1.41 | 26.21±1.21* | 27.01±1.35* | 27.51±1.42 | 27.52±1.43 | <0.0001 | 20.93 | 7.85 | 0.33 | 0.49 | |
| Auditory-verbal learning test score@ | 17.01±4.12 | 16.41±3.85 | 16.81±4.01 | 16.91±4.11 | 16.99±4.13 | 0.119 | N/A | N/A | N/A | N/A | |
| Trail making test (s)@@ | Part A | 52.45±8.45 | 54.21±9.15* | 53.21±9.01 | 52.41±8.41 | 51.45±7.99 | <0.0001 | 4.57 | 1.97 | 0.1 | 2.6 |
| Part B | 111.12±13.12 | 119.22±14.15* | 118.21±13.15* | 111.21±13.25 | 111.19±13.26 | <0.0001 | 13.51 | 11.83 | 0.15 | 0.12 | |
| Stroop color and word test (s)@@ | Congruous | 31.15±4.12 | 35.12±6.15* | 33.21±5.15* | 31.16±4.21 | 31.14±4.01 | <0.0001 | 18.48 | 9.59 | 0.05 | 0.05 |
| Incongruous | 51.12±5.02 | 55.21±7.15* | 53.21±6.25* | 51.21±5.21 | 51.11±5.21 | <0.0001 | 15.68 | 8.01 | 0.34 | 0.04 | |
| Digit symbol substitution test@@@ | 97.13±6.15 | 95.15±5.15* | 96.15±5.45 | 97.01±6.01 | 97.12±6.14 | <0.0001 | 7.63 | 3.78 | 0.46 | 0.04 | |
| Verbal fluency test& | 15.17±5.15 | 13.85±4.12* | 15.01±4.89 | 15.11±5.01 | 15.16±5.02 | <0.0001 | 6.08 | 0.74 | 0.28 | 0.05 | |
BL – baseline: 1 week before surgeries.
The maximum score was 30 points;
As per RAVLT Adult Calculator;
The time required to complete the task;
The score range: 0–133;
The numbers of animals listed within 1 min.
Variables were represented as mean ±SD. One-way ANOVA following Tukey post hoc test was used for statistical analysis. A p<0.05 and q>3.858 were considered significant. Perioperative neurocognitive disorder was defined as a significant worst condition in at least 2 parameters as compared to baseline.
Significantly worst condition compared to baseline.
Analysis of factors for perioperative neurocognitive disorders
At 1 week after surgeries, older adults (p<0.0001), females (p=0.002), obese patients (p=0.003), and patients with preexisting neurocognitive impairments (p<0.0001) had higher incidence of perioperative neurocognitive disorders. At the end of the 3-month follow-up period, older adults (p=0.002) and patients with preexisting neurocognitive impairments (p=0.005) had a higher incidence of perioperative neurocognitive disorders. However, at 1 year after surgeries, age, gender, body mass index, and preexisting neurocognitive impairments of the patients were not found to be associated with worse perioperative neurocognitive disorders (Table 3).
Table 3.
Univariable and multivariable analysis for demographical characteristics and postoperative outcomes in the test group.
| Follow-up period | The p-value for the analysis of parameter for perioperative neurocognitive disorders@@ | ||||
|---|---|---|---|---|---|
| After 1 week | After 3 months | After 1 year | After 4 years | ||
| Patients included in the study (sample size) | 499 | 499 | 499 | 499 | |
| Demographical characteristics | Age (years) | <0.0001* | 0.002* | 0.12 | 0.54 |
| Gender | 0.002* | 0.12 | 0.21 | 0.41 | |
| Body mass index (kg/m2) | 0.003* | 0.13 | 0.32 | 0.51 | |
| Smoking | 0.12 | 0.14 | 0.35 | 0.61 | |
| Diabetes&& | 0.13 | 0.15 | 0.36 | 0.71 | |
| Education | 0.45 | 0.16 | 0.38 | 0.72 | |
| Preexisting neurocognitive impairments@ | <0.0001* | 0.005* | 0.31 | 0.64 | |
| Hypertension## | 0.12 | 0.55 | 0.63 | 0.85 | |
| Residence (urban or rural) | 0.18 | 0.86 | 0.91 | 0.99 | |
A p<0.05 was considered significant.
Significant parameter associated with worst cognitive dysfunction.
Defined as a significant worst condition in at least 2 parameters out of all parameters;
defined as a significant worst condition in at least 2 parameters out of all parameters as compared to baseline.
Control group was used as the reference standard.
Random blood glucose > 140 mg/dL;
Blood pressure >90/130 mmHg.
Discussion
Patients with preexisting neurocognitive impairments had perioperative neurocognitive disorders at 1 week after surgery (p<0.0001) and at 3 months after surgery (p=0.005), but there was no incidence of perioperative neurocognitive disorders at 1-year postoperative follow-up (p=0.31) and at 4 years (p=0.64) after surgeries. The results of the study were in line with previous available studies [1,6,15,18–20]. Surgery may not affect areas of neurocognition [18]. Also, patients with normal neurocognitive function have less risk of perioperative neurocognitive disorders [21]. Our results show that preexisting impairments is an independent risk factor for long-term perioperative neurocognitive disorders.
Only older adults had perioperative neurocognitive disorders at 1 week (p<0.0001) and at 3 months (p=0.002) after surgeries, but there was no association of perioperative neurocognitive disorders with age at 1-year (p=0.12) and 4-years (p=0.54) postoperative follow-ups. These results are in line with available studies [4,6,19,22,23]. Preexisting neurocognitive impairment is also evidence of aging [4]. Hip fractures cause lower functional recovery in older adults [19]. Surgical technique, anesthetic procedures, and medical history can affect the postoperative outcomes [22]. Patients’ attitudes about potentially losing their intellectual function and having reduced physical activity may contribute to perioperative neurocognitive disorders [4]. Our results show that age is an independent factor predicting perioperative neurocognitive disorders in younger patients.
To investigate perioperative neurocognitive disorders, we matched gender, age, body mass index, education, and the other demographical parameters with the nonsurgical control group. To determine perioperative neurocognitive disorders, it is mandatory to add a non-operative control group [6,24]. A nonsurgical group with positive osteoarthritis is more appropriately matched to the study population than is a healthy population.
This study is the first to perform 4-year follow-up after hip joint replacement surgeries to evaluate perioperative neurocognitive disorders. Longer-term postoperative outcomes need to be evaluated in noncardiac surgical patients to track neurocognitive decline [6]. The available studies evaluated postoperative outcomes for 1 year [1,3,4,6,25], for 3 months [22], and for 1 week [26]. The results of the present study are more reliable due to its longer follow-up period.
Factors such as anesthesia [7,22], type of surgeries [22], intraoperative analgesic [26], microemboli count [25], and duration of preoperative fluid fasting [26] also have effects on perioperative neurocognitive disorders, but were not assessed in the present study. Randomization has precise results for translating research data into clinical practice because it allows balancing known and unknown confounders to make control and treatment groups as balanced as possible [27], but randomization was not possible because the intervention was given in 1 group only. The participants in this study were recruited from PR China only. Therefore, the results might not be representative of the other regions of the world and it remains uncertain whether the findings in the analysis could be generalized to populations speaking languages other than Chinese. Cognitive tests were not repeated. The possible justification for performing a test once only is that the test-retest intervals can influence performance of participants. Finally, many older Chinese adults have little education. Therefore, these limitations may have affected the results of our study.
Conclusions
Older adults and patients with preexisting neurocognitive impairments had an increased incidence of perioperative neurocognitive disorders at 1 week and 3 months after hip joint replacement surgery. Age and preexisting neurocognitive impairments are markers for predicting the risk of perioperative neurocognitive disorders for hip joint replacement surgery. However, preexisting neurocognitive impairments and age may have no association with long-term perioperative neurocognitive disorders.
Supplementary Files
Supplementary Table 1.
English translation of Trail Making Test Part A.
| Number | In words | Number | In words | Number | In words | Number | In words | Number | In words |
|---|---|---|---|---|---|---|---|---|---|
| 1 | One | 6 | Six | 11 | Eleven | 16 | Sixteen | 21 | Twenty-one |
| 2 | Two | 7 | Seven | 12 | Twelve | 17 | Seventeen | 22 | Twenty-two |
| 3 | Three | 8 | Eight | 13 | Thirteen | 18 | Eighteen | 23 | Twenty-three |
| 4 | Four | 9 | Nine | 14 | Fourteen | 19 | Nineteen | 24 | Twenty-four |
| 5 | Five | 10 | Ten | 15 | Fifteen | 20 | Twenty | 25 | Twenty-five |
150 sec and less was considered as norm value.
Supplementary Table 2.
English translation of Trail Making Test Part B.
| Chinese Zodiacs | Respective picture | Chinese Zodiacs | Respective picture | Chinese Zodiacs | Respective picture |
|---|---|---|---|---|---|
| Rat |

|
Dragon |

|
Monkey |

|
| Ox |

|
Snake |

|
Rooster |

|
| Tiger |

|
Horse |

|
Dog |

|
| Rabbit |

|
Goat |

|
Pig |

|
150 s and less was considered as norm value.
English translation of Stroop Color and Word Test: Congruous subtask. We considered 200 s and less (≤70 years), 220 s and less (70–80 years), and 330 s and less (≥80 years) as norm values.
English translation of Stroop Color and Word Test: Incongruous subtask. We considered 200 s and less (≤70 years), 220 s and less (70–80 years), and 330 s and less (≥80 years) as norm values.
Acknowledgments
Authors are thankful to all medical and non-medical staff of Xuzhou Central Hospital, Xuzhou, China.
Abbreviations
- STROBE
the strengthening the reporting of observational studies in epidemiology
- ASA
American Society Anesthesiologists
- RAVLT
Rey Auditory-Verbal Learning Test
- ANOVA
analysis of variance
Footnotes
Source of support: This study was supported by the National Natural Science Foundation of China (No. 81870857)
Conflict of interest
None.
References
- 1.Price CC, Tanner JJ, Schmalfuss I, et al. A pilot study evaluating presurgery neuroanatomical biomarkers for postoperative cognitive decline after total knee arthroplasty in older adults. Anesthesiology. 2014;120:601–3. doi: 10.1097/ALN.0000000000000080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crosby G, Culley DJ, Hyman BT. Preoperative cognitive assessment of the elderly surgical patient: A call for action. Anesthesiology. 2001;114:1265–68. doi: 10.1097/ALN.0b013e31821b1bc8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silbert BS, Scott DA, Evered LA, et al. A comparison of the effect of high- and low-dose fentanyl on the incidence of postoperative cognitive dysfunction after coronary artery bypass surgery in the elderly. Anesthesiology. 2006;104:1137–45. doi: 10.1097/00000542-200606000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Monk TG, Weldon BC, Garvan CW, et al. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology. 2008;108:18–30. doi: 10.1097/01.anes.0000296071.19434.1e. [DOI] [PubMed] [Google Scholar]
- 5.Pan CW, Wang X, Ma Q, et al. Cognitive dysfunction and health-related quality of life among older Chinese. Sci Rep. 2015;5:17301. doi: 10.1038/srep17301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silbert B, Evered L, Scott DA, et al. Preexisting cognitive impairment is associated with postoperative cognitive dysfunction after hip joint replacement surgery. Anesthesiology. 2015;122:1224–34. doi: 10.1097/ALN.0000000000000671. [DOI] [PubMed] [Google Scholar]
- 7.Leung JM. Postoperative delirium: Are there modifiable risk factors? Eur J Anaesthesiol. 2010;27:403–5. doi: 10.1097/EJA.0b013e3283340a99. [DOI] [PubMed] [Google Scholar]
- 8.Li H, Jia J, Yang Z. Mini-mental state examination in elderly Chinese: A population-based normative study. J Alzheimers Dis. 2016;53:487–96. doi: 10.3233/JAD-160119. [DOI] [PubMed] [Google Scholar]
- 9.Li X, Zhou Z, Jia S, et al. Cognitive study on Chinese patients with idiopathic REM sleep behavior disorder. J Neurol Sci. 2016;366:82–86. doi: 10.1016/j.jns.2016.04.047. [DOI] [PubMed] [Google Scholar]
- 10.RAVLT Adult Calculator. Available at: http://www.beaumont.ie/media/RAVLTAdultcalculator1.xls.
- 11.Wang R-Y, Zhou J-H, Huang Y-C, Yang Y-R. Reliability of the Chinese version of the Trail Making Test and Stroop Color and Word Test among older adults. Int J Gerontol. 2018;12:336–39. [Google Scholar]
- 12.Jaeger J, Domingo ZS. The Digit Symbol Substitution Test (DSST): Psychometric properties and clinical utility in major depressive disorder, in the 29th ECNP Congress; Vienna, Austria. 2016; p. 1.j.033. [Google Scholar]
- 13.Shi C, Wang G, Tian F, et al. Reliability and validity of Chinese version of perceived deficits questionnaire for depression in patients with MDD. Psychiatry Res. 2017;252:319–24. doi: 10.1016/j.psychres.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 14.Wang LJ, Lin PY, Lee Y, et al. Validation of the Chinese version of brief assessment of cognition in schizophrenia. Neuropsychiatr Dis Treat. 2016;12:2819–26. doi: 10.2147/NDT.S118110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evered LA, Silbert BS, Scott DA, et al. Preexisting cognitive impairment and mild cognitive impairment in subjects presenting for total hip joint replacement. Anesthesiology. 2011;114:1297–304. doi: 10.1097/ALN.0b013e31821b1aab. [DOI] [PubMed] [Google Scholar]
- 16.Zhang WT, Wang YF. Efficacy of methylphenidate for the treatment of mental sequelae after traumatic brain injury. Medicine. 2017;96:e6960. doi: 10.1097/MD.0000000000006960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ashara KC, Shah KV. The study of chloramphenicol for ophthalmic formulation. IJSRR. 2018;7:173–81. [Google Scholar]
- 18.Bekker A, Lee C, de Santi S, et al. Does mild cognitive impairment increase the risk of developing postoperative cognitive dysfunction? Am J Surg. 2010;199:782–88. doi: 10.1016/j.amjsurg.2009.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guo Y, Sun T, Wang X, et al. Cognitive impairment and 1-year outcome in elderly patients with hip fracture. Med Sci Monit. 2014;20:1963–68. doi: 10.12659/MSM.892304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li J, Zhou J, Wan Y, et al. Association between ABO blood type and postoperative cognitive dysfunction in elderly patients undergoing unilateral total hip arthroplasty surgery in China. Med Sci Monit. 2017;23:2584–89. doi: 10.12659/MSM.901736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guthrie BL. Commentary on “Does mild cognitive impairment increase the risk of developing postoperative cognitive dysfunction?”. Am J Surg. 2010;199:791. doi: 10.1016/j.amjsurg.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 22.Evered L, Scott DA, Silbert B, Maruff P. Postoperative cognitive dysfunction is independent of type of surgery and anesthetic. Anesth Analg. 2011;112:1179–85. doi: 10.1213/ANE.0b013e318215217e. [DOI] [PubMed] [Google Scholar]
- 23.Silbert B, Evered L, Scott DA. Cognitive decline in the elderly: Is anaesthesia implicated? Best Pract Res Clin Anaesthesiol. 2011;25:379–93. doi: 10.1016/j.bpa.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 24.Lewisa M, Maruff P, Silbert B. Statistical and conceptual issues in defining post-operative cognitive dysfunction. Neurosci Biobehav Rev. 2004;28:433–40. doi: 10.1016/j.neubiorev.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Koch S, Forteza A, Lavernia C, et al. Cerebral fat microembolism and cognitive decline after hip and knee replacement. Stroke. 2007;38:1079–81. doi: 10.1161/01.STR.0000258104.01627.50. [DOI] [PubMed] [Google Scholar]
- 26.Radtke FM, Franck M, MacGuill M, et al. Duration of fluid fasting and choice of analgesic are modifiable factors for early postoperative delirium. Eur J Anaesthesiol. 2010;27:411–16. doi: 10.1097/EJA.0b013e3283335cee. [DOI] [PubMed] [Google Scholar]
- 27.Spieth PM, Kubasch AS, Penzlin AI, et al. Randomized controlled trials – A matter of design. Neuropsychiatr Dis Treat. 2016;12:1341–49. doi: 10.2147/NDT.S101938. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1.
English translation of Trail Making Test Part A.
| Number | In words | Number | In words | Number | In words | Number | In words | Number | In words |
|---|---|---|---|---|---|---|---|---|---|
| 1 | One | 6 | Six | 11 | Eleven | 16 | Sixteen | 21 | Twenty-one |
| 2 | Two | 7 | Seven | 12 | Twelve | 17 | Seventeen | 22 | Twenty-two |
| 3 | Three | 8 | Eight | 13 | Thirteen | 18 | Eighteen | 23 | Twenty-three |
| 4 | Four | 9 | Nine | 14 | Fourteen | 19 | Nineteen | 24 | Twenty-four |
| 5 | Five | 10 | Ten | 15 | Fifteen | 20 | Twenty | 25 | Twenty-five |
150 sec and less was considered as norm value.
Supplementary Table 2.
English translation of Trail Making Test Part B.
| Chinese Zodiacs | Respective picture | Chinese Zodiacs | Respective picture | Chinese Zodiacs | Respective picture |
|---|---|---|---|---|---|
| Rat |

|
Dragon |

|
Monkey |

|
| Ox |

|
Snake |

|
Rooster |

|
| Tiger |

|
Horse |

|
Dog |

|
| Rabbit |

|
Goat |

|
Pig |

|
150 s and less was considered as norm value.
English translation of Stroop Color and Word Test: Congruous subtask. We considered 200 s and less (≤70 years), 220 s and less (70–80 years), and 330 s and less (≥80 years) as norm values.
English translation of Stroop Color and Word Test: Incongruous subtask. We considered 200 s and less (≤70 years), 220 s and less (70–80 years), and 330 s and less (≥80 years) as norm values.