Abstract
Objective: Immune checkpoint inhibitors, especially the programmed cell death receptor-1/ligand 1 (PD-1/L1) inhibitors, displayed promising efficacy in non-small cell lung cancer (NSCLC) patients. Incorporation of anti-PD-1/L1 antibodies into other therapeutic regimens (including CTLA-4 inhibitors, chemotherapy, EGFR-TKIs and IDO inhibitors) is currently in active clinical research. This meta-analysis summarized recent developments in four combination regimens of PD-1/L1 inhibitors.
Methods: We searched PubMed, the Cochrane Library and the Embase database up to July 2018, on the combination therapy of PD-1/L1 inhibitors in NSCLC patients.
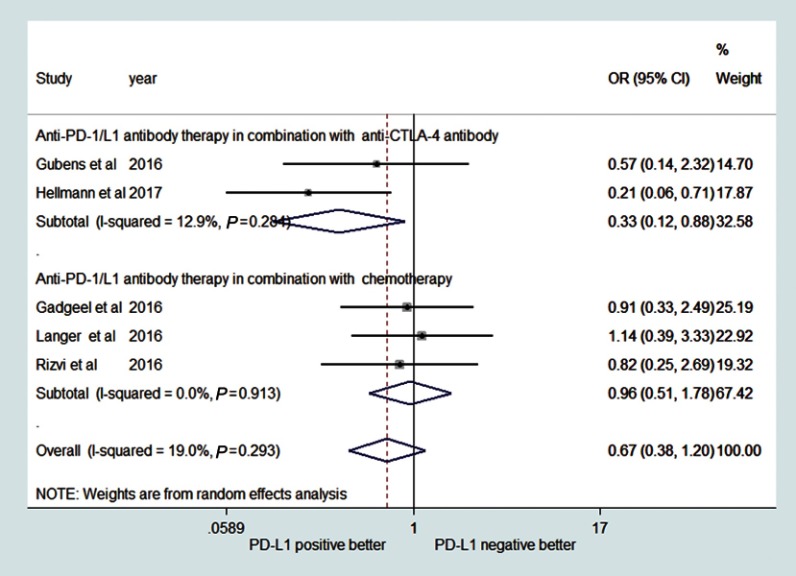
Results: Seventeen trials were finally included in the current meta-analysis. The combined objective response rate s (ORR) for PD-1/L1 inhibitors in combination with CTLA-4 inhibitors, chemotherapy, EGFR-TKIs, and IDO inhibitors were 32% (19%–44%), 49% (46%–53%), 55% (28%–83%) and 35% (20%–50%) respectively. The combined ORR for first line PD-1/L1 inhibitors combination with CTLA-4 inhibitors, chemotherapy, and EGFR-TKIs were 35% (17%–53%), 51% (46%–56%) and 43% (−7%–93%) respectively, and the combined ORR in the second or more line setting were 36% (8%–65%), 17% (−13%–46%), 39% (19%–59%) and 35% (20%–50%) respectively. The pooled 6-month progression-free survival rate (6m PFSr) and 1-year overall survival rate (1y OSr) for combination therapy of PD-1/L1 inhibitors with CTLA-4 inhibitors or chemotherapy were 35% or 65% (6m PFSr) and 31% or 70% (1y OSr) respectively. Anti-PD-1/L1 drugs combined with anti-CTLA-4 drugs exhibited a more potent efficacy on PD-L1 positive patients (OR=0.33, 95%CI: 0.12–0.88). This trend was not observed in patients receiving combination therapy of PD-1/L1 inhibitors with chemotherapy (OR=0.96, 95%CI: 0.51–1.78).
Conclusion: The included four combination regimens were potential treatment strategies and well tolerated for NSCLC patients. Further, the therapy lines and PD-L1 expression status were correlated with treatment efficacy.
Keywords: PD-1/L1 inhibitors, combination therapy, meta-analysis, non-small cell lung cancer
Introduction
Lung cancer has become the most common malignant tumor worldwide, with high mortality.1 In 2016, the epidemiological data from the USA displayed that the incidence and mortality rates of lung cancer were 57.3/100,000 and 46.0/100,000, respectively, and the newly diagnosed cases and estimated deaths were 224,390 and 158,050, respectively.2 Non-small cell lung cancer (NSCLC) comprised approximately 85% of all lung cancers and numerous patients with NSCLC at diagnosis already had metastatic disease.2,3
Figure 1.

Flow chart of the meta-analysis selection process.
Recently, the discovery of immune checkpoint inhibitors has led to a step forward in the treatment of advanced NSCLCs. Immune checkpoints such as PD-1/L1 and cytotoxic T-lymphocyte antigen-4 (CTLA-4) were considered as the main brakes of T cell immune response, creating a comfortable microenvironment for tumor growth and assisting tumor escape from the body’s immune response.4,5 Many tumor cells are capable of upregulating the expression of PD-L1, which results in the inability of cytotoxic T cells after ligand binding to PD-1.6–8 Therefore, blockade of the PD-1 pathway with monoclonal antibodies against PD-1 or PD-L1 can improve the body’s immune response against tumor cells.9 Indeed, immune checkpoint inhibitors achieved unprecedented antitumor efficacy, in particular, PD-1/L1 inhibitors.10–15 In 2015 and 2016, the FDA approved 3 immune checkpoint inhibitors (anti-PD-1 antibodies: nivolumab, pembrolizumab; anti-PD-L1 antibodies: atezolizumab) for the therapy of patients with metastatic NSCLC who have progressed on from first-line platinum-based doublet chemotherapy.16–18 In late 2016, the US Food and Drug Administration (FDA) further approved pembrolizumab for the first-line therapy for patients with advanced non-squamous or squamous NSCLC.19 However, primary resistance to anti-PD-1/L1 antibody was commonly observed.20 Under this circumstance, it is difficult to achieve a long-lasting antitumor efficacy with single-agent monotherapy, which only covers a small population of patients. To enhance clinical benefits of immunotherapy for NSCLC patients, anti-PD-1/L1 antibodies are being evaluated in combination with CTLA-4 inhibitors, chemotherapeutic agents, epidermal growth factor receptor-tyrosine kinase inhibitors (EGFR-TKIs), indoleamine-2,3-dioxygenase (IDO) inhibitors, etc. A series of phase I/II studies on NSCLC have confirmed the efficacy of combination therapy.21–24 However, most of those trials were performed without comparable forms, and usually as a single arm. Considering the small samples of these studies, therefore, we made a timely summarization by quantitative meta-analysis, in which all available evidence was incorporated to evaluate the efficacy and safety of PD-1/L1 inhibitors combination therapy including anti-CTLA-4 antibody, chemotherapy, EGFR-TKIs and IDO inhibitors on NSCLC patients.
Methods
Search strategy
This meta-analysis was performed in accordance with Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines. We searched PubMed, the Cochrane Library and the Embase database up to July 2018, for randomized clinical trials (RCTs) which including the combination therapy with the anti-PD-1/L1 MoAb for advanced NSCLC patients. The following search terms were used: “nivolumab” OR “opdivo” OR “ONO-4538” OR “BMS-936558” OR “MDX-1106” “atezolizumab” OR “Tecentriq” OR “MPDL-3280A” OR “RG-7446” OR “pembrolizumab” OR “Keytruda” OR “lambrolizumab” OR “MK-3475” OR “PEMBRO” OR “durvalumab” OR “MEDI-4736” OR “Imfinzi” OR “pidilizumab” OR “CT-011” OR “PD-1” OR “PD-L1” OR “PD-1/PD-L1” OR “programmed cell death 1” OR “programmed cell death ligand 1” and “NSCLC” OR “non-small-cell lung cancer” OR “non-small-cell lung carcinoma” and combined OR combination. We also reviewed the relevant abstracts from the American Society of Clinical Oncology (ASCO), World Conference on Lung Cancer (WCLC) and European Society of Medical Oncology (ESMO). We also searched the ClinicalTrials.Gov website (https://clinicaltrials.gov) to find ongoing studies and unpublished data.
Selection criteria
The inclusion criteria for the eligible studies were as follows: I) patients who were histologically diagnosed with advanced NSCLC; II) studies reporting the combination therapy of anti-PD1/L1 antibody with CTLA-4 inhibitors/chemotherapy/EGFR-TKIs/IDO inhibitors; III) studies with available primary outcome (objective response rate: ORR); IV) studies published in English. In the event that studies with multiple follow-ups over time, we only reported the most up-to-date data. Studies failing to meet the inclusion criteria would be excluded in the current meta-analysis.
Data extraction
The work of data extraction and assessment was done by two different authors (Ning Wan and Bo Ji) independently, and discrepancies were further discussed with the third author (Tiantian Zhang) to reach consensus. For each clinical trial, the information of the first author, year of publication, number of patients, ORR, PFS, OS and safety outcomes including rate of Grade 3–Grade 5 drug-related adverse effects (G3-5 DRAEs), pneumonitis and drug-related death was recorded.
Risk of bias within studies
Risks of bias within studies without comparable arms were assessed using the methodological item for non-randomized studies (MINORS) reported by Slim.25 The Cochrane Risk of Bias tool was used for the randomized controlled trials. The study quality was assessed by two reviewers (Ning Wan and Bo Ji) independently, and the assessments were verified by the third reviewer (Chen Yang).
Statistic analysis
The pooled data of ORR, 6-month progression-free survival rate (6m PFSr), 1-year overall survival rate (1y OSr), G3–G5 DRAEs, pneumonitis, and drug-related death rate were obtained by Stata version 14.0 (Stata A Corp, College Station, TX, USA). In addition, ORR were further stratified depending on the PD-L1 expression status of the tumor. Since the definition of PD-L1 positivity was different in clinical trials,19 we selected PD-L1≥1% as a cutoff to identify PD-L1 positive patients in our studies according to the literature.26 The heterogeneity of the extracted data was evaluated by I2 statistic and chi-square Q test, in which I2≥50% (for the I2 statistic) or P≤0.05 (for the Q test) was considered significant heterogeneity. Random-effects model was applied under the circumstance of high potential heterogeneity, to avoid underestimating the standard errors of pooled data.
Assessment of publication bias
Funnel plot, Egger linear regression test, and Begg rank correlation method were applied to determine publication bias.
Results
Search results
As shown in Figure 1, a total of 1,505 records were yielded through the search strategy, which identified 271 articles in PubMed, 171 articles in the Cochrane Library, and 1,063 articles in the Embase database. Finally, 17 studies21-24,27–39 published in English were enrolled for meta-analysis according to the selection criteria, which involved 1,222 NSCLC patients.
Characteristics of included studies
Among these 17 studies, 6 studies21,27–31 reported the efficacy and toxicities of anti-PD-1/L1 antibody in combination with anti-CTLA-4 antibody therapy for the treatment of advanced NSCLC, and 384 patients were enrolled. Six studies22,32–36 involved research into the combination therapy of anti-PD-1/L1 antibody and chemotherapy involving 700 patients. Four studies23,37–39 reported the combination therapy of anti-PD-1/L1 antibody with EGFR-TKIs, and 95 patients were enrolled. One study24 reported the combination of pembrolizumab with epacadostat involving 43 patients. The ORR across the studies varied from 16.3% to 79%. The median follow-up duration varied from 6.7 to 19 months. Only 5 studies were available to determine the 6m PFSr, and 6 studies were available to extract the 1yOSr. In these 17 studies, only 3 studies22,30,33 were performed with control groups; others were performed as a single arm or multiple arms. The detailed characteristics of the enrolled studies are summarized in Table 1.
Table 1.
Characteristics of included studies for meta-analysis
| References | Trials number/name | Phase | Median follow up duration (months) | No. of participants | NSCLC stage | Previous treatment | Intervention | PD-L1 TPS | ORR (%) | 6m PFSr | 1y OSr |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Anti-PD-1/L1 antibody therapy in combination with anti-CTLA-4 antibody | |||||||||||
| Patnaik [2015]27 | NCT02039674 | I | NA | 11 | IIIB/IV | ≤2 prior regimens | Pembro+ Ipi |
NA | Total: 6/11 (54.5%) | NA | NA |
| Gubens [2016]28 | NCT02039674 | I/II | 7 | 45 | Advanced NSCLC | ≥1 prior regimen | Pembro+ Ipi |
<1% n=21 ≥1% n=24≥50%n=6 |
Total: 11/45 (24.4%) PD-L1 Expression <1% 4/21 (19.0%) ≥1% 7/24 (29.2%) ≥50% 1/6 (16.7%) | NA | NA |
| Antonia [2014]31 | CheckMate 012 | I | 6.7–10.8 (across 4 cohorts) | 49 | Advanced NSCLC. | Chemo- naive | Nivo+Ipi | <5% n=22≥5% n=16 | Total: 8/49 (16.3%) PD-L1 Expression <5% 3/22 (13.6%) ≥5% 3/16 (18.8%) |
17/49 (34.7%) | NA |
| Hellmann [2017]21 | NCT01454102/CheckMate 012 | I | 11·8–12.8 (across 2 cohorts) | 77 | IIIb/IV | Chemo- naive | Nivo+Ipi | <1% n=19≥1% n=46 ≥50%n=13 |
Total: 33/77 (42.8%) PD-L1 Expression <1% 4/19 (21%) ≥1% 26/46 (57%) ≥50%12/13 (92%) |
NA | 59/77 (76.6%) |
| Hellmann [2018]30 | NCT02477826/CheckMate 227 | III | 11.2 | 139 | IV or recurrent | Chemo- naive | Nivo+Ipi | <1% n=38 ≥1% n=101 |
Total: 63/139(45.3%) | * 59/139(42.6%) | 43/139(30.9%) |
| Antonia [2016]29 | NCT02000947 | Ib | 4.7 | 63 | Advanced or metastatic NSCLC | none/≥1 prior regimen | Durva+ Treme |
≥25% n=18 <25% n=37 0% n=24 unknown n=8 | Total: 11/63 (17.5%) PD-L1 Expression ≥25%: 4/18 (22.2%) <25%: 6/37 (16.2%) 0%: 5/24 (20.8%) unknown: 1/8 (12.5%) |
NA | NA |
| Anti-PD-1/L1 antibody therapy in combination with chemotherapy | |||||||||||
| Gadgeel [2016]32 | NCT02039674/KEYNOTE-021 | I | 12 | 74 | Advanced NSCLC | Chemo- naive | Pembro+ Chemo | <1% n=22≥1% n=51 ≥50% n=25 |
Total: 42/74 (56.8%) PD-L1 Expression <1% 12/22 (55%) ≥1% 29/51 (57%) ≥50%15/25 (60%) |
NA | NA |
| Langer [2016]33 | NCT02039674/KEYNOTE-021 | II | 10.6 | 60 | IIIB/IV | Chemo- naive | Pembro+ Chemo | <1% n=21≥1% n=39 ≥50%n=25 |
Total:34/60 (57%) <1% 12/21 (57%) ≥1% 21/39 (54%) ≥50% 16/25 (80%) |
46/60 (76.7%) | 46/60 (76.7%) |
| Gandhi [2018]22 | NCT02578680 | III | 10.5 | 410 | Metastatic NSCLC | none | Pembro+ Chemo | <1% n=127; ≥1% n=260; unknown‖n=23; |
Total: 195/410 (47.6%) <1% 41/127 (32%) ≥1% 143/260 (55%) |
*140/410 (34.1%) | 284/410 (69.2%) |
| Kanda [2016]34 | (JapicCTI)-132,071 | Ib | 3.19–9.43 (across 4 arms). | 24 | IIIB/IV, or recurrent NSCLC | none/≥1 prior regimen | Nivo+ Chemo | NA | Total: 13/23 (56.5%) | 14/24 (58.3%) | NA |
| Liu [2015]35 | NCT01633970 | Ib | NA | 76 | Advanced or metastatic NSCLC. | Chemo- naive | Atezo+ Chemo | NA | Total: 37/76 (49%) | NA | NA |
| Rizvi [2016]36 | NCT01454102 | I | 19 | 56 | IIIB/IV NSCLC | Chemo- naive | Nivo+ Chemo | <1% n=21; ≥1% n=23; unknown n=12; | Total: 24/56 (43%) PD-L1 Expression <1% 9/21 (43%) ≥1% 11/23 (48%) unknown 4/12 (33%) | 30/56 (53.6%) | 40/56(71.4%) |
| Anti-PD-1/L1 antibody therapy in combination with EGFR-TKIs | |||||||||||
| Rizvi [2014]37 | _ | I | 18 | 21 | IIIB/IV | Chemo- naive | Nivo+ E | NA | Total: 4/21 (19%) | 11/21 (52.4%) | 15/21 (71.4%) |
| Gibbons [2016]23 | NCT02088112 | I | NA | 20 | EGFR mutant NSCLC | TKI- naive | Durva+G | NA | Total: 15/19 (79%) | NA | NA |
| Ma [2016]38 | NCT02013219 | I | 11.2 | 20 | Advanced NSCLC | NA | Atezo+ E | NA | Total: 15/20 (75%) | NA | NA |
| Ahn [2016]39 | NCT02143466 | Ib | NA | 34 | EGFR mutant NSCLC | none/≥1 prior regimen | Durva+O | NA | Total: 16/33 (48%) | NA | NA |
| Anti-PD-1/L1 antibody therapy in combination with IDO inhibitors | |||||||||||
| Gangadhar [2017]24 | ECHO202/KEYNOTE-037 | I/II | NA | 43 | Advanced NSCLC | ≤2 prior regimen | Pembro+Epa | <50% n=17; ≥50% n=7; | Total: 14/40 (35%) PD-L1 Expression <50% 6/17 (35%) ≥50% 3/7 (43%) |
NA | NA |
Note: *1-year progression-free survival rate.
Abbreviations: ORR, objective response rate; 6m PFSr, 6-month progression-free survival rate; 1y OSr, 1-year overall survival rate; TPS, tumor proportion score; NA, not available; Chemo, chemotherapy; Pembro, pembrolizumab; Ipi, ipilimumab; Nivo, nivolumab; Durva, durvalumab; Treme, tremelimumab; Atezo, atezolizumab; E, erlotinib; G, gefitinib; O, osimertinib; Epa, epacadostat.
Risk of bias in individual studies
The risks of bias within the 17 studies included in the current study are summarized in Tables S1 and S2.
Table S1.
Bias risk evaluation of the studies without comparable arms in the meta-analysis
| Reference | A clearly stated aim | Inclusion of consecutive patients | Prospective collection of data | Endpoints appropriate to the aim of the study | Unbiased assessment of the study endpoint | Follow-up period appropriate to the aim of the study | Loss to follow up less than 5% | Prospective calculation of the study size | Score |
|---|---|---|---|---|---|---|---|---|---|
| Patnaik [2015]1 | 1 | 2 | 0 | 2 | 0 | 0 | 1 | 1 | 7 |
| Gubens [2016]2 | 1 | 2 | 0 | 2 | 0 | 2 | 2 | 1 | 10 |
| Antonia [2014]3 | 1 | 2 | 0 | 2 | 0 | 2 | 2 | 1 | 10 |
| Hellmann [2017]4 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 14 |
| Antonia [2016]5 | 2 | 2 | 1 | 2 | 0 | 2 | 2 | 2 | 13 |
| Gadgeel [2016]6 | 1 | 2 | 0 | 2 | 0 | 2 | 2 | 1 | 10 |
| Kanda [2016]7 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 1 | 13 |
| Liu [2015]8 | 1 | 2 | 0 | 2 | 0 | 0 | 2 | 1 | 8 |
| Rizvi [2016]9 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 14 |
| Gettinger [2014]10 | 1 | 2 | 0 | 2 | 0 | 2 | 2 | 1 | 10 |
| Gibbons [2016]11 | 1 | 2 | 0 | 2 | 0 | 0 | 2 | 1 | 8 |
| Ma [2016]12 | 1 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 11 |
| Ahn [2016]13 | 2 | 2 | 0 | 2 | 0 | 0 | 2 | 1 | 9 |
| Gangadhar [2017]14 | 1 | 1 | 0 | 2 | 0 | 0 | 2 | 1 | 7 |
Table S2.
Bias risk evaluation of the randomized controlled trials included in the meta-analysis
| Reference | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other sources of bias |
|---|---|---|---|---|---|---|---|
| Hellmann [2018]15 | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | High risk | Unclear risk |
| Langer [2016]16 | Low risk | High risk | High risk | Low risk | Low risk | Low risk | Unclear risk |
| Gandhi [2018]17 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | unclear risk |
Meta-analysis results of anti-PD-1/L1 antibody combination therapy
Pooled ORR
ORR data were extracted from 17 studies for meta-analysis to assess the efficacy of combination regimens. The pooled ORR was 44% (95% CI: 36–52%) and the random effects model was applied as significant heterogeneity was detected (I2=86.0% P<0.001, Figure 2). We then performed a subgroup analysis of the combination regimens, dividing into four groups: anti-PD-1/L1 antibody combination therapy with anti-CTLA-4 antibody/chemotherapy/EGFR-TKIs/IDO inhibitors for NSCLC patients. The combined ORR values were 32% (95% CI: 19–44%), 49% (95% CI: 46–53%), 55% (95% CI: 28–83%) and 35% (95% CI: 20–50%) respectively (Figure 3).
Figure 2.
Forest plot of the pooled overall response rate (ORR) of anti-PD-1/L1 antibody combination therapy for NSCLC patients.
Abbreviation: NSCLC, non-small cell lung cancer.
Figure 3.
Forest plots of the subgroup analyses of the combination therapy of anti-PD-1/L1 antibody and anti-CTLA-4 antibody/chemotherapy/EGFR-TKIs/IDO inhibitors for NSCLC patients.
Abbreviation: NSCLC, non-small cell lung cancer.
Pooled ORR of combination therapy for first/second or more line therapy
A total of 11 eligible trials21,22,30–37,39 involving 990 patients were included to evaluate the efficacy of anti-PD-1/L1 antibody combination therapy in the first-line setting for NSCLC patients, and the ORRs ranged from 16% to 70%. As there was no study reporting the combination therapy of PD-1/L1 inhibitors with IDO inhibitors in the first line setting, we only evaluated PD-1/L1 inhibitor combination therapy with the 3 other therapeutic regimens. A random-effect model was performed to evaluate the pooled ORR with high heterogeneity (I2=81.7%; P<0.001). The combined ORR was 45.0% (95% CI: 37–53%, Figure 4A). The pooled ORR of anti-PD-1/L1 antibody combination therapy with anti-CTLA-4 antibody/chemotherapy/EGFR-TKIs in the first-line setting for NSCLC patients was 35% (95% CI: 17–53%), 51% (95% CI: 46–56%) and 43% (−7–93%) respectively (Figure 4A). A total of 5 eligible trials24,27,28,34,39 involving 125 patients were included to evaluate the efficacy of anti-PD-1/L1 antibody combination therapy in the second or more line setting for NSCLC patients, and the ORR ranged from 17% to 55%. The combined ORR was 32.0% (95% CI: 23–42%) (Figure 4B). The pooled ORR of anti-PD-1/L1 antibody combination therapy with anti-CTLA-4 antibody/chemotherapy/EGFR-TKIs/IDO inhibitors in the second or more line setting for NSCLC patients was 36% (95% CI: 8–65%), 17% (95% CI: −13–46%), 39% (95% CI:19–59%) and 35% (95% CI:20–50%), respectively (Figure 4B).
Figure 4.
Forest plot of the pooled overall response rate (ORR) of anti-PD-1/L1 antibody combination therapy as a first line treatment (A) and as second or more line treatment for NSCLC patients (B).
Abbreviation: NSCLC, non-small cell lung cancer.
PD-L1 positive versus negative
Nine studies without the ORR data correlated with PD-L1 expression status were excluded in the related analysis. As we selected PD-L1≥1% as a cutoff to identify PD-L1 positive patients, studies24,29,31 reporting other PD-L1 expression levels were excluded. Five studies21,28,32,33,36 with 287 patients assessed the ORR correlated with the tumor PD-L1 expression status. Among 183 patients with PD-L1 expression positive status (≥1% of expression), the ORR was 50% (95% CI: 40–60%, Figure 5A). The pooled ORR of anti-PD-1/L1 antibody combination therapy with anti-CTLA-4 antibody/chemotherapy was 43% (95% CI: 17–70%)/54% (95% CI: 45–63%) respectively (Figure 5A). Among 104 patients with PD-L1 expression negative status (<1% of expression), the ORR was 38% (95% CI: 22–54%, Figure 5B). The pooled ORR of anti-PD-1/L1 antibody combination therapy with anti-CTLA-4 antibody/chemotherapy was 20% (95% CI: 8–32%)/52% (95% CI: 39–64%) respectively (Figure 5B).
Figure 5.
Forest plot of the pooled overall response rate (ORR) of anti-PD-1/L1 antibody combination therapy for PD-L1 expression positive (A) and negative (B) NSCLC patients.
Abbreviation: NSCLC, non-small cell lung cancer.
The pooled ORR of combination therapy involving PD-1/L1 inhibitors was similar in PD-L1 positive and negative NSCLC patients (OR=0.67, 95% CI: 0.38–1.20, Figure 6). For the patients receiving anti-PD-1/L1 therapy combination therapy with anti-CTLA-4 antibody, patients with PD-L1 positive status exhibited a superior ORR than those with PD-L1 negative status (OR=0.33, 95% CI: 0.12–0.88, Figure 6). For the patients receiving combination therapy of anti-PD-1/L1 therapy with chemotherapy, patients with PD-L1 positive status showed a similar ORR with those in PD-L1 negative status (OR=0.96, 95% CI: 0.51–1.78, Figure 6).
Figure 6.
Meta-analysis of the associations between overall response rate (ORR) and programmed death-ligand 1 (PD-L1) expression.
Pooled 6m PFSr and 1y OSr
6m PFSr data were extracted from 4 studies31,33,34,36 for meta-analysis. The pooled 6m PFSr was 55% (95% CI: 31–80%), and a random effects model was applied as significant heterogeneity was detected (I2=91.6% P<0.001, Figure 7A). We then performed a subgroup analysis of the combination regimens, dividing into two groups: anti-PD-1/L1 antibody combination therapy with anti-CTLA-4 antibody/chemotherapy for NSCLC patients. The combined ORR values were 35% (95% CI: 21–48%), 63%(95%Cl: 47%-80%) respectively (Figure 7A). The 1y OSr data were extracted from 4 studies22,30,33,36 for meta-analysis. The pooled 1y OSr was 62% (95% CI: 41–83%), and a random effects model was applied due to the significant heterogeneity (I2=96.4% P<0.001, Figure 7B). The subgroup analysis of the combination regimens achieved an ORR 31% (95% CI: 23–39%) with anti-CTLA-4 antibody, and 70% (95% CI: 67–74%) with chemotherapy (Figure 7B).
Figure 7.
Forest plot of the pooled 6m PFSr (A) and 1y OSr (B) of anti-PD-1/L1 antibody combination therapy for NSCLC patients.
Abbreviations: 6m PFSr, 6-month progression-free survival rate; 1y OSr, 1-year overall survival rate.
Adverse effects
Adverse effects including the rate of G3-5 DRAEs, pneumonitis and drug-related deaths are recorded in Table 2. Data of G3-5 DRAEs rate were not available in 4 studies,22,23,34,35 pneumonitis (≥G3) rate was not available in 3 studies,28,32,39 and drug-related death rates were not available in 5 studies,23,24,35,37,38 so that these studies were excluded in the correlated meta-analysis. A meta-analysis of the safety outcomes from different combination regimens is exhibited in Table 3. Here, we concluded the combination regimens that have data available, in fact, a large number of ongoing clinical trials are investigating these regimens for NSCLC patients. A summary of ongoing clinical trials enrolling NSCLC patients for the combination therapy of anti-PD1/L1 antibody with other treatments, including anti-CTLA-4 antibody, chemotherapy, targeted therapy or IDO inhibitors other immunotherapies, and chemotherapy, is presented in Table 4.
Table 2.
Safety outcomes of the included studies
| Study (Reference) | G3–5 DRAEs | Pneumonitis (≥G3) | Drug-related death |
|---|---|---|---|
| Patnaik [2015]26 | 2/17 (11.8%) | 0/17 | 0 |
| Gubens [2016]27 | 11/45 (24.4%) | NA | 1 |
| Antonia [2014]31 | 24/49 (49.0%) | 3/49 | 3 |
| Hellmann [2017]21 | 20/77 (26.0%) | 3/77 | 0 |
| Hellmann [2018]30 | 180/576(31.2%) | 13/576 | 7 |
| Antonia [2016]29 | 43/102 (42.2%) | 4/99 | 3 |
| Gadgeel [2016]32 | 30/74 (40.5%) | NA | 1 |
| Langer [2016]33 | 23/60 (38.3%) | 1/60 | 1 |
| Gandhi [2018]22 | NA | 11/410 | 27 |
| Kanda [2016]34 | NA | 1/24 | 0 |
| Rizvi [2016]36 | 25/56 (44.6%) | 4/56 | 0 |
| Liu [2015]35 | NA | 0/76 | NA |
| Gettinger [2014]37 | 5/21 (23.8%) | 0/21 | NA |
| Gibbons [2016]23 | NA | 1/20 | NA |
| Ma [2016]38 | 8/20 (40.0%) | 0/20 | NA |
| Ahn [2016]39 | 20/34 (58.8%) | NA | 0 |
| Gangadhar [2017]24 | 7/43 (16.3%) | 4/43 | NA |
Abbreviations: G3–5 DRAEs, Grade 3–Grade 5 drug-related adverse effects; NA, not available.
Table 3.
Meta-analysis of rate of G3-5 DRAEs, pneumonitis and drug-related death in combination therapy
| Combination regimens | Items for evaluation | Rate (%) | 95% CI |
|---|---|---|---|
| Anti-PD-1/L1 antibody therapy in combination with ipilimumab (IPI) | Rate of G3–5 DRAEs | 31 | 23–39% |
| Rate of pneumonitis | 3 | 2–4% | |
| Rate of drug-related death | 1 | 1–2% | |
| Anti-PD-1/L1 antibody therapy in combination with chemotherapy | Rate of G3–5 DRAEs | 41 | 34–48% |
| Rate of pneumonitis | 2 | 1–3% | |
| Drug-related death | 3 | 0–5% | |
| Anti-PD-1/L1 antibody therapy in combination with EGFR-TKIs | Rate of G3–5 DRAEs | 41 | 20–62% |
| Rate of pneumonitis | 3 | −1–7% | |
| Drug-related death | 1 | −3–6% | |
| Anti-PD-1/L1 antibody therapy in combination with IDO inhibitors | Rate of G3–5 DRAEs | 16 | 5–27% |
| Rate of pneumonitis | 9 | 1–18% | |
| Drug-related death | - | - |
Table 4.
Ongoing clinical trials of anti-PD-1/L1therapy combination therapy for NSCLC patients
| Clinical Trials. Gov number | Trial name | Phase | Pathology or histology | Agents |
|---|---|---|---|---|
| Combination with anti-CTLA-4 antibody | ||||
| NCT02659059 | CheckMate568 | II | Treatment-naive, metastatic NSCLC | Nivolumab+ ipilimumab |
| NCT02864251 | CheckMate722 | III | EGFR mutation, T790M negative NSCLC | Nivolumab vs nivolumab+ ipilimumab vs carboplatin/pemetrexed |
| NCT02352948 | ARCTIC | III | Previously treated NSCLC | Durvalumab±tremelimumab vs SOC |
| NCT02542293 | NEPTUNE | III | Treatment-naive,stage IV NSCLC | Durvalumab±tremelimumab vs SOC |
| NCT02453282 | MYSTIC | III | Treatment-naive, stage IV NSCLC | Durvalumab±tremelimumab vs SOC |
| Combination with chemotherapy | ||||
| NCT02477826 | CheckMate227 | III | Treatment naive, metastatic or recurrent NSCLC | Nivolumab+ PT-DC |
| NCT01840579 | KEYNOTE-011 | I | Advanced NSCLC (stage III B/IV) | Pembrolizumab+PT-DC or ipilimumab |
| NCT02775435 | KEYNOTE407 | III | Metastatic,squamous cell NSCLC (first line) | Pembrolizumab +carboplatin/Nab -paclitaxel (or paclitaxel) |
| NCT02366143 | IMpower 150 | III | Treatment-naïve NSCLC, non squamous cell histology | Atezolizumab + PT-DC therapy with or without bevacizumab |
| NCT02657434 | IMpower132 | III | Chemotherapy-naive, stage IV, non squamous cell NSCLC | Atezolizumab +carboplatin or cisplatin/pemetrexed |
| NCT02367794 | IMpower 131 | III | Stage IV squamous NSCLC | Atezolizumb + carboplatin/nab-paclitaxel (or paclitaxel) |
| NCT02367781 | IMpower 130 | III | Stage IV Non-Squamous NSCLC | Atezolizumb + carboplatin/nab- paclitaxel |
| Combination with targeted therapy | ||||
| NCT02039674 | KEYNOTE-021 | I/II | Stage IIIb/IV NSCLC | Cohort E and F: Pembrolizumab+ erlotinib or gefitinib |
| NCT02364609 | – | I | EGFR mutant after resistance to EGFR TKI NSCLC | Pembrolizumab + afatinib |
| NCT02574078 | CheckMate370 | I/II | EGFR/ALK mutant treatment naïve NSCLC |
Nivolumab + erlotinib or crizotinib |
| NCT02393625 | – | I | ALK mutant NSCLC | Nivolumab+ ceritinib |
| NCT02511184 | KEYNOTE-050 | I | ALK mutant treatment naïve NSCLC | Pembrolizumab + crizotinib |
| NCT02584634 | Javelin Lung 101 | I/II | ALK mutant or not NSCLC | Avelumab+Lorlatinib or crizotinib |
| NCT02323126 | – | II | EGFR mutant or MET positive NSCLC |
Nivolumab+EGF816 or capmatinib |
| NCT02898116 | – | I/II | ALK mutant NSCLC | Durvalumab + ensartinib |
| NCT01998126 | _ | I | Stage IV NSCLC, failed prior platinum-based therapy | Nivolumab + erlotinib (EGFR mutant) or crizotinib (ALK mutant) |
| NCT01454102 | CheckMate012 | I | Stage IIIB/IV (NSCLC) | Cohort D: nivolumab + bevacizumab maintenance |
| NCT02574078 | CheckMate370 | I/II | Locally advanced or stage IV NSCLC | Nivolumab + bevacizumab or pemetrexed maintenance |
| NCT02681549 | – | II | Non-squamous NSCLC | Pembrolizumab + bevacizumab |
| NCT02443324 | – | I | Nonsquamous or squamous NSCLC | Pembrolizumab + Ramucirumab |
| Combination with IDO inhibitors | ||||
| NCT02298153 | ECHO-110 | I | Advanced NSCLC and urothelial carcinoma | Atezolizumab+ epacadostat |
| NCT02327078 | ECHO-204 | I/II | SCCHN and NSCLC | Nivolumab+ epacadostat |
| NCT03322566 | ECHO-306/KEYNOTE-715 | III | mNSCLC | Pembrolizumab+epacadostat with or without platinum-based chemotherapy |
| NCT03322540 | ECHO-305/KEYNOTE-654 | III | mNSCLC with high PD-L1 levels | Pembrolizumab+epacadostat |
Abbreviations: NSCLC, non–small cell lung cancer; PT-DC, platinum doublet chemotherapy; SOC, standard of care; EGFR, epidermal growth factor receptor; ALK, anaplastic lymphoma kinase; SCCHN, squamous cell carcinoma of head and neck; mNSCLC, metastatic non–small cell lung cancer.
Sensitivity analysis
In order to detect how the uncertain factors impacted the final results, a sensitivity analysis was performed in the current study. The sensitivity analysis indicated that none of the single studies would significantly affect the results of PD-1/L1 inhibitor combination therapy (data not shown).
Publication bias
A funnel plot analysis of the studies of PD-1/L1 inhibitor combination therapy indicated an asymmetric distribution (Figure S1); the Egger linear regression test (t=3.67, P=0.002) verified that there was potential publication bias (Figure S2). However, the Begg rank correlation method (z=−0.16, P=0.869) indicated there was no publication bias (Figure S3). As Egger’s linear regression method was reported to have stronger statistical and discriminatory powers than Begg’s method for detecting publication bias40 and combining the results of the funnel plot, we identified that there was potential publication bias in the current study. One possible reason is the small sample size of trials.
Discussion
The current meta-analysis observed that the combination therapy involving PD-1/L1 inhibitors with other therapeutic regimens (including CTLA-4 inhibitors, chemotherapy, EGFR-TKIs and IDO inhibitors) demonstrated promising efficacy and tolerable safety profile. We also found that combination therapy of PD-1/L1 inhibitors with CTLA-4 inhibitors exhibits potent efficacy to PD-L1 positive patients. Meanwhile, for patients receiving combination therapy of PD-1/L1 inhibitors with chemotherapy, it showed similar efficacy in PD-L1 positive or negative patients.
Xu et al41 performed a meta-analysis to investigate potential treatment strategies using combinations of PD-1/L1 inhibitors with chemotherapy or other CTLA4 inhibitors in the first-line setting for lung cancer patients. In our meta-analysis, we focused on the combination regimens of PD-1/L1 inhibitors for NSCLC patients. To supplement this, we updated the data of combinations of PD-1/L1 inhibitors with chemotherapy or CTLA4 inhibitors, and the combination of PD-1/L1 inhibitors with EGFR-TKIs or IDO inhibitors was also included. In addition, the first line and second or more line settings for NSCLC patients were analyzed in the current meta-analysis. More importantly, we further evaluated the impact of PD-L1 status on combination therapy of PD-1/L1 inhibitors with CTLA-4 inhibitors or chemotherapy.
Oncogenic alteration in the EGFR pathway is related to the induction of PD-L1 expression and makes lung tumors susceptible to PD-1 blockade in a preclinical model,42 which demonstrated that a combination of EGFR TKIs with PD-1/L1 inhibitors might be a promising therapeutic regimen to prolong the duration of response and prevent or delay resistance.43 In the current meta-analysis, we pooled the available data for combination therapy of PD-1/L1 inhibitors with EGFR TKIs for NSCLC patients. IDO is an enzyme mediating cleavage of tryptocan to kynurenine. High expression of IDO often leads to an immunosuppressive tumor microenvironment, which increased the differentiation of regulatory T (Treg) cells, impaired the activity of effector T cells, and decreased the functions of dendritic cells.44 It was reported IDO inhibitors had synergistic antitumor effects in melanoma models with immune checkpoint inhibitors.45 These preclinical data establish a strong foundation for exploration of clinical combination therapy of PD-1/L1 inhibitors with IDO inhibitors. Therefore, in the current meta-analysis, we also pooled the available data for combination therapy of PD-1/L1 inhibitors with IDO inhibitors for NSCLC patients.
The pooled ORR of the combination regimens of PD-1/L1 inhibitors for NSCLC patients was 44% in our meta-analysis. As there was significant heterogeneity, we then performed a subgroup analysis of the combination regimens for NSCLC patients. The combined ORR for first line PD-1/L1 inhibitors, in combination with CTLA-4 inhibitors and chemotherapy were 35% and 51%, respectively, which was consistent with previous results.41 However, one of the included studies for combination therapy of PD-1/L1 with inhibitors in their meta-analysis enrolled patients who had received ≥2 prior lines (55%).29 In the current study, the ORR of combination therapy for the second or more line setting was also evaluated. It worth noting that the ORR of PD-1/L1 combination therapy with chemotherapy or EGFR-TKIs in the second or more line setting decreased compared with that in the first line setting. This might be partly associated with the reason that monotherapy of PD-1/L1 inhibitors achieved lower efficacy in the second or more line setting for NSCLC patients.46
In the subgroup analysis, the pooled 6m PFSr and 1y OSr for combination therapy of PD-1/L1 with CTLA-4 or chemotherapy were 35% or 65% (6m PFSr) and 31% or 70% (1y OSr), respectively. The results were in line with the study41 of the combination therapy of PD-1/L1 inhibitors and chemotherapy, while the results were not available for the combination therapy of PD-1/L1 inhibitors and CTLA-4 inhibitors in Xu’s study.
PD-L1 expression in immune cells and tumor cells has become a biomarker which can assist in decision-making in clinical treatment strategies.47 Nearly 50% of NSCLC patients are reported to have high expression of PD-L1, and this may result in poor prognosis.48 Wang et al49 and Zhang et al50 found that NSCLC patients exhibited poor OS with positive PD-L1 expression. Our result showed that the pooled ORR of combination therapy of PD-1/L1 inhibitors for PD-L1 positive or negative NSCLC patients had no significant difference. As for subgroup analysis, anti-PD-1/L1 drugs combined with anti-CTLA-4 drugs exhibited a more potent efficacy on patients with high expression of PD-L1. This trend was not observed in patients receiving combination therapy of PD-1/L1 inhibitors and chemotherapy. As was reported in a recent phase III study, the efficacy of nivolumab was uncorrelated with PD-L1 expression in squamous-cell NSCLC.11 In our study, we did not report the related outcome for NSCLC patients with different histologies due to the limitation of RCTs, which may account for the results in our study to some extent.
Despite the impressive response rates of immune checkpoint inhibitors, they can contribute to both unique and severe toxicities.51–53 In the current meta-analysis, the results showed that the combined strategies were relatively safe and remained tolerable.
The use of the PD-1/L1 inhibitors had been reported to correlate with the development of severe pneumonitis which had resulted in drug-related deaths in clinical trials.11–13,15 Hence we also assessed the rate of pneumonitis in the combination regimens. The combination of PD-1/L1 inhibitors with IDO inhibitors showed a relatively high rate of pneumonitis. As for the rate of drug-related death, the four combination regimens were almost the same.
Despite the data of combination regimens discussed in the meta-analysis, plenty of clinical trials are ongoing. The ongoing clinical trials for combination therapy of PD-1/L1 inhibitors with CTLA-4 inhibitors, chemotherapy, EGFR-TKIs, and IDO inhibitors are described in Table 1. Recently, a phase III RCT, named the MYSTIC study (NCT02453282), failed to fulfill its primary endpoint. The strategy of durvalumab combined with tremelimumab (CTLA-4 inhibitors) failed to prolong PFS compared with chemotherapy in NSCLC patients with PD-L1 expression>25%. The recent results of CheckMate370 (NCT02574078), a phase II/III RCT, were promulgated.54 Thirteen patients were treated with nivolumab plus crizotinib, and 5 patients (38%) discontinued the combination therapy due to severe hepatic toxicities. Two of the 5 patients died, which might be caused by the presence of severe hepatic toxicities. Enrollment for combination therapy was closed, and the treatment strategy discontinued due to severe hepatic toxicities (Grade≥3). Only 5 patients (38%) had a partial response. Overall, the results of the study do not support further assessment of the current combination regimens.
There are several limitations to the current meta-analysis. Firstly, most of the included studies in the meta-analysis were performed without comparable arms, and some of them only had a very small sample size. Even so, large numbers of studies focusing on PD-1/L1 inhibitors in combination with other agents are ongoing, and we will update the meta-analysis in the future. Secondly, the definition of PD-L1 positive status varied in the recent studies, and the optimal cutoff value for PD-L1 positive status is controversial. Hence, to identify a specific biomarker for anti-PD-1/L1 therapy becomes imperative. Thirdly, we have not distinguished the impact of histology subtype of NSCLC (squamous or non-squamous) on the efficacy of combination therapy, due to the limitation of included trials. Additionally, we did not analyze the PFS and OS due to limitations of the included data, and a potential impact of selection bias and publication bias existed. Finally, compared with a traditional meta-analysis, the pooled single arm meta-analysis was not yet mature.
Conclusion
In summary, the four combination regimens involving PD-1/L1 inhibitors with CTLA-4 inhibitors, chemotherapy, EGFR-TKIs and IDO inhibitors were potential treatment strategies and well tolerated for NSCLC patients. Further, the therapy lines and PD-L1 expression status were correlated with treatment efficacy.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (Grant No. 71704064), the Natural Science Foundation of Guangdong Province, China (Grant No. 2017A030310174), the Fundamental Research Funds for the Central Universities (Grant No. 21616324) and Science and Technology Program of Guangzhou, China (Grant No. 201709010006).
Disclosure
The authors report no conflicts of interest in this work.
Supplementary materials
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–E386. doi: 10.1002/ijc.29210 [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics. CA Cancer J Clin. 2016;66(1):7–30. doi: 10.3322/caac.21332 [DOI] [PubMed] [Google Scholar]
- 3.Feinstein AR, Wells CK. A clinical-severity staging system for patients with lung cancer. Medicine (Baltimore). 1990;69(1):1–33. [DOI] [PubMed] [Google Scholar]
- 4.Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–2454. doi: 10.1056/NEJMoa1200690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brahmer JR, Tykodi SS, Chow LQ, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455–2465. doi: 10.1056/NEJMoa1200694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ishida Y, Agata Y, Shibahara K, et al. Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. Embo J. 1992;11(11):3887–3895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freeman GJ, Long AJ, Iwai Y, et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J Exp Med. 2000;192(7):1027–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Keir ME, Liang SC, Guleria I, et al. Tissue expression of PD-L1 mediates peripheral T cell tolerance. J Exp Med. 2006;203(4):883–895. doi: 10.1084/jem.20051776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: A common denominator approach to cancer therapy. Cancer Cell. 2015;27(4):451–461. doi: 10.1016/j.ccell.2015.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ribas A. Releasing the Brakes on Cancer Immunotherapy. N Engl J Med. 2015;373(16):1490–1492. doi: 10.1056/NEJMp1510079 [DOI] [PubMed] [Google Scholar]
- 11.Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373(2):123–135. doi: 10.1056/NEJMoa1504627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387(10027):1540–1550. doi: 10.1016/S0140-6736(15)01281-7 [DOI] [PubMed] [Google Scholar]
- 13.Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373(17):1627–1639. doi: 10.1056/NEJMoa1507643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fehrenbacher L, Spira A, Ballinger M, et al. Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): a multicentre, open-label, phase 2 randomised controlled trial. Lancet. 2016;387(10030):1837–1846. doi: 10.1016/S0140-6736(16)00587-0 [DOI] [PubMed] [Google Scholar]
- 15.Rittmeyer A, Barlesi F, Waterkamp D, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet (London, England). 2017. doi: 10.1016/S0140-6736(16)32517-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kazandjian D, Khozin S, Blumenthal G, et al. Benefit-risk summary of nivolumab for patients with metastatic squamous cell lung cancer after platinum-based chemotherapy: a report from the US food and drug administration. JAMA Oncol. 2016. doi: 10.1001/jamaoncol.2015.3934 [DOI] [PubMed] [Google Scholar]
- 17.Kazandjian D, Suzman DL, Blumenthal G, et al. FDA approval summary: Nivolumab for the treatment of metastatic non-small cell lung cancer with progression on or after platinum-based chemotherapy. Oncologist. 2016;21(5):634–642. doi: 10.1634/theoncologist.2015-0507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sul J, Blumenthal GM, Jiang X, et al. FDA approval summary: Pembrolizumab for the treatment of patients with metastatic non-small cell lung cancer whose tumors express programmed death-ligand 1. Oncologist. 2016;21(5):643–650. doi: 10.1634/theoncologist.2015-0498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ettinger DS, Wood DE, Aisner DL, et al. Non-Small Cell Lung Cancer, Version 9.2017, NCCN Clinical Practice Guidelines in Oncology. 2017. [DOI] [PubMed]
- 20.O’Donnell JS, Long GV, Scolyer RA, et al. Resistance to PD1/PDL1 checkpoint inhibition. Cancer Treat Rev. 2017;52:71–81. doi: 10.1016/j.ctrv.2016.11.007 [DOI] [PubMed] [Google Scholar]
- 21.Hellmann M, Rizvi N, Goldman J, et al. Nivolumab plus ipilimumab as first-line treatment for advanced non-small-cell lung cancer (CheckMate 012): results of an open-label, phase 1, multicohort study. Lancet Oncol. 2017;18:31–41. doi: 10.1016/S1470-2045(16)30624-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gandhi L, Rodriguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378:2078–2092. doi: 10.1056/NEJMoa1801005 [DOI] [PubMed] [Google Scholar]
- 23.Gibbons DL, Chow LQ, Kim DW, et al. Efficacy, safety and tolerability of MEDI4736 (durvalumab [D]), a human IgG1 antiprogrammed cell death-ligand-1 (PD-L1) antibody, combined with gefitinib (G): a phase I expansion in TKI-naïve patients (pts) with EGFR mutant NSCLC. J Thorac Oncol. 2016;11(4):S79. doi: 10.1016/S1556-0864(16)30171-X [DOI] [Google Scholar]
- 24.Gangadhar TC. Efficacy and safety of epacadostat plus pembrolizumab treatment of NSCLC: preliminary phaseI/II results of ECHO-202/KEYNOTE-037. ASCO Annu Meeting Proc. 2017;35(15S):p9014. [Google Scholar]
- 25.Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 26.Passiglia F, Galvano A, Rizzo S, et al. Looking for the best immune-checkpoint inhibitor in pre-treated NSCLC patients: an indirect comparison between nivolumab, pembrolizumab and atezolizumab. Int J Cancer. 2018;142(6):1277–1284. doi: 10.1002/ijc.31136 [DOI] [PubMed] [Google Scholar]
- 27.Patnaik A, Socinski MA, Gubens MA, et al. Phase 1 study of pembrolizumab (pembro; MK-3475) plus ipilimumab (IPI) as second-line therapy for advanced non-small cell lung cancer (NSCLC): KEYNOTE-021 cohort D. J Clin Oncol. 2015;33:15. doi: 10.1200/jco.2015.33.15_suppl.8011 [DOI] [Google Scholar]
- 28.Gubens MA, Sequist LV, Stevenson J, et al. Phase I/II study of pembrolizumab (pembro) plus ipilimumab (ipi) as second-line therapy for NSCLC: KEYNOTE-021 cohorts D and H. J Clin Oncol. 2016;34:9027. doi: 10.1200/JCO.2016.34.15_suppl.9027 [DOI] [Google Scholar]
- 29.Antonia S, Goldberg S, Balmanoukian A, et al. Safety and antitumour activity of durvalumab plus tremelimumab in non-small cell lung cancer: a multicentre, phase 1b study. Lancet Oncol. 2016;17:299–308. doi: 10.1016/S1470-2045(15)00544-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hellmann MD, Ciuleanu TE, Pluzanski A, et al. Nivolumab plus Ipilimumab in Lung Cancer with a High Tumor Mutational Burden. N Engl J Med. 2018;378(22):2093–2104. doi: 10.1056/NEJMoa1801946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Antonia SJ, Gettinger SN, Chow LQM, et al. Nivolumab (anti-PD-1; BMS-936558, ONO-4538) and ipilimumab in first-line NSCLC: interim phase I results. J Clin Oncol. 2014;32(15). doi: 10.1200/JCO.2013.54.6911 [DOI] [Google Scholar]
- 32.Gadgeel SM, Stevenson J, Langer CJ, et al. Pembrolizumab (pembro) plus chemotherapy as front-line therapy for advanced NSCLC: KEYNOTE-021 cohorts A-C. J Clin Oncol. 2016;34(15)suppl. doi: 10.1200/JCO.2016.34.15_suppl.9016 [DOI] [Google Scholar]
- 33.Langer CJ, Gadgeel SM, Borghaei H, et al. Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol. 2016;17(11):1497–1508. doi: 10.1016/S1470-2045(16)30498-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kanda S, Goto K, Shiraishi H, et al. Safety and efficacy of nivolumab and standard chemotherapy drug combination in patients with advanced non-small-cell lung cancer: a four arms phase Ib study. Ann Oncol. 2016;27(12):2242–2250. doi: 10.1093/annonc/mdw416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu SV, Powderly JD, Camidge DR, et al. Safety and efficacy of MPDL3280A (anti-PD-L1) in combination with platinum-based doublet chemotherapy in patients with advanced non-small cell lung cancer (NSCLC). J Clin Oncol. 2015;33(15):8030. doi: 10.1200/jco.2015.33.15_suppl.8030 [DOI] [Google Scholar]
- 36.Rizvi N, Hellmann M, Brahmer J, et al. Nivolumab in combination with platinum-based doublet chemotherapy for first-line treatment of advanced non-small-cell lung cancer. J Clin Oncol. 2016;34:2969–2979. doi: 10.1200/JCO.2016.66.9861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gettinger S, Chow LQ, Borghaei H, et al. Safety and response with nivolumab (anti-PD-1; BMS-936558, ONO-4538) plus erlotinib in patients (PTS) with epidermal growth factor receptor mutant (EGFR MT) advanced non-small cell lung cancer (NSCLC). Inte J Radiat Oncol Biol Phys. 2014;90(5):S34–S35. [Google Scholar]
- 38.Ma BBY, Rudin CM, Cervantes A, et al. Preliminary safety and clinical activity of erlotinib plus atezolizumab from a Phase Ib study in advanced NSCLC. Ann Oncol. 2016;27:ix141. doi: 10.1093/annonc/mdw141 [DOI] [Google Scholar]
- 39.Ahn MJ, Yang J, Yu H, et al. Osimertinib combined with durvalumab in EGFR-mutant non-small cell lung cancer: results from the TATTON phase Ib trial. J Thorac Oncol. 2016;11(4):S115. doi: 10.1016/S1556-0864(16)30246-5 [DOI] [Google Scholar]
- 40.Hayashino Y, Noguchi Y, Fukui T. Systematic evaluation and comparison of statistical tests for publication bias. J Epidemiol. 2005;15(6):235–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu X, Huang Z, Zheng L, et al. The efficacy and safety of anti-PD-1/PD-L1 antibodies combined with chemotherapy or CTLA4 antibody as a first-line treatment for advanced lung cancer. Int J Cancer. 2018;142(11):2344–2354. doi: 10.1002/ijc.31252 [DOI] [PubMed] [Google Scholar]
- 42.Akbay EA, Koyama S, Carretero J, et al. Activation of the PD-1 pathway contributes to immune escape in EGFR-driven lung tumors. Cancer Discov. 2013;3(12):1355–1363. doi: 10.1158/2159-8290.CD-13-0310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ahn MJ, Sun JM, Lee SH, et al. EGFR TKI combination with immunotherapy in non-small cell lung cancer. Expert Opin Drug Saf. 2017;16(4):465–469. doi: 10.1080/14740338.2017.1300656 [DOI] [PubMed] [Google Scholar]
- 44.Mellor AL, Munn DH. IDO expression by dendritic cells: tolerance and tryptophan catabolism. Nat Rev Immunol. 2004;4(10):762–774. doi: 10.1038/nri1457 [DOI] [PubMed] [Google Scholar]
- 45.Spranger S, Koblish HK, Horton B, et al. Mechanism of tumor rejection with doublets of CTLA-4, PD-1/PD-L1, or IDO blockade involves restored IL-2 production and proliferation of CD8(+) T cells directly within the tumor microenvironment. J Immunother Cancer. 2014;2:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhuansun Y, Huang F, Du Y, et al. Anti-PD-1/PD-L1 antibody versus conventional chemotherapy for previously-treated, advanced non-small-cell lung cancer: a meta-analysis of randomized controlled trials. J Thorac Dis. 2017;9(3):655–665. doi: 10.21037/jtd.2017.03.104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Daud AI, Wolchok JD, Robert C, et al. Programmed death-ligand 1 expression and response to the anti-programmed death 1 antibody pembrolizumab in melanoma. J Clin Oncol. 2016;34(34):4102–4109. doi: 10.1200/JCO.2016.67.2477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mu CY, Huang JA, Chen Y, et al. High expression of PD-L1 in lung cancer may contribute to poor prognosis and tumor cells immune escape through suppressing tumor infiltrating dendritic cells maturation. Med Oncol. 2011;28(3):682–688. doi: 10.1007/s12032-010-9515-2 [DOI] [PubMed] [Google Scholar]
- 49.Wang A, Wang HY, Liu Y, et al. The prognostic value of PD-L1 expression for non-small cell lung cancer patients: a meta-analysis. Eur J Surg Oncol. 2015;41(4):450–456. doi: 10.1016/j.ejso.2015.01.020 [DOI] [PubMed] [Google Scholar]
- 50.Zhang Y, Kang S, Shen J, et al. Prognostic significance of programmed cell death 1 (PD-1) or PD-1 ligand 1 (PD-L1) Expression in epithelial-originated cancer: a meta-analysis. Medicine (Baltimore). 2015;94(6):e515. doi: 10.1097/MD.0000000000000874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Michot JM, Bigenwald C, Champiat S, et al. Immune-related adverse events with immune checkpoint blockade: a comprehensive review. Eur J Cancer. 2016;54:139–148. doi: 10.1016/j.ejca.2015.11.016 [DOI] [PubMed] [Google Scholar]
- 52.Postow MA, Sidlow R, Hellmann MD. Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med. 2018;378(2):158–168. doi: 10.1056/NEJMra1703481 [DOI] [PubMed] [Google Scholar]
- 53.Wang DY, Johnson DB, Davis EJ. Toxicities associated with PD-1/PD-L1 blockade. Cancer J. 2018;24(1):36–40. doi: 10.1097/PPO.0000000000000296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Spigel DR, Reynolds C, Waterhouse D, et al. Phase 1/2 study of the safety and tolerability of nivolumab plus crizotinib for the first-line treatment of anaplastic lymphoma kinase translocation — positive advanced non–small cell lung cancer (CheckMate 370). J Thorac Oncol. 2018;13(5):682–688. doi: 10.1016/j.jtho.2018.02.022 [DOI] [PubMed] [Google Scholar]
References
- 1.Patnaik A, Socinski MA, Gubens MA, et al. Phase 1 study of pembrolizumab (pembro; MK-3475) plus ipilimumab (IPI) as second-line therapy for advanced non-small cell lung cancer (NSCLC): KEYNOTE-021 cohort D. J Clin Oncol. 2015;33:15. doi: 10.1200/jco.2015.33.15_suppl.8011 [DOI] [Google Scholar]
- 2.Gubens MA, Sequist LV, Stevenson J, et al. Phase I/II study of pembrolizumab (pembro) plus ipilimumab (ipi) as second-line therapy for NSCLC: KEYNOTE-021 cohorts D and H. J Clin Oncol. 2016;34:9027. doi: 10.1200/JCO.2016.34.15_suppl.9027 [DOI] [Google Scholar]
- 3.Antonia SJ, Gettinger SN, Chow LQM, et al. Nivolumab (anti-PD-1; BMS-936558, ONO-4538) and ipilimumab in first-line NSCLC: interim phase I results. J Clin Oncol. 2014;32(15). doi: 10.1200/JCO.2013.54.6911 [DOI] [Google Scholar]
- 4.Hellmann M, Rizvi N, Goldman J, et al. Nivolumab plus ipilimumab as first-line treatment for advanced non-small-cell lung cancer (CheckMate 012): results of an open-label, phase 1, multicohort study. Lancet Oncol. 2017;18:31–41. doi: 10.1016/S1470-2045(16)30624-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Antonia S, Goldberg S, Balmanoukian A, et al. Safety and antitumour activity of durvalumab plus tremelimumab in non-small cell lung cancer: a multicentre, phase 1b study. Lancet Oncol. 2016;17:299–308. doi: 10.1016/S1470-2045(15)00544-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gadgeel SM, Stevenson J, Langer CJ, et al. Pembrolizumab (pembro) plus chemotherapy as front-line therapy for advanced NSCLC: KEYNOTE-021 cohorts A-C. J Clin Oncol. 2016;34:9016. doi: 10.1200/JCO.2016.34.15_suppl.9016 [DOI] [Google Scholar]
- 7.Kanda S, Goto K, Shiraishi H, et al. Safety and efficacy of nivolumab and standard chemotherapy drug combination in patients with advanced non-small-cell lung cancer: a four arms phase Ib study. Ann Oncol. 2016;27(12):2242–2250. doi: 10.1093/annonc/mdw416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu SV, Powderly JD, Camidge DR, et al. Safety and efficacy of MPDL3280A (anti-PD-L1) in combination with platinum-based doublet chemotherapy in patients with advanced non-small cell lung cancer (NSCLC). J Clin Oncol. 2015;33(15):8030. doi: 10.1200/jco.2015.33.15_suppl.8030 [DOI] [Google Scholar]
- 9.Rizvi N, Hellmann M, Brahmer J, et al. Nivolumab in combination with platinum-based doublet chemotherapy for first-line treatment of advanced non-small-cell lung cancer. J Clin Oncol. 2016;34:2969–2979. doi: 10.1200/JCO.2016.66.9861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gettinger S, Chow LQ, Borghaei H, et al. Safety and response with nivolumab (anti-PD-1; BMS-936558, ONO-4538) plus erlotinib in patients (PTS) with epidermal growth factor receptor mutant (EGFR MT) advanced non-small cell lung cancer (NSCLC). Inte J Radiat Oncol Biol Phys. 2014;90(5):S34–S35. [Google Scholar]
- 11.Gibbons DL, Chow LQ, Kim DW, et al. Efficacy, safety and tolerability of MEDI4736 (durvalumab [D]), a human IgG1 antiprogrammed cell death-ligand-1 (PD-L1) antibody, combined with gefitinib (G): a phase I expansion in TKI-naïve patients (pts) with EGFR mutant NSCLC. J Thorac Oncol. 2016;11(4):S79. doi: 10.1016/S1556-0864(16)30171-X [DOI] [Google Scholar]
- 12.Ma BBY, Rudin CM, Cervantes A, et al. Preliminary safety and clinical activity of erlotinib plus atezolizumab from a Phase Ib study in advanced NSCLC. Ann Oncol. 2016;27:ix141. doi: 10.1093/annonc/mdw141 [DOI] [Google Scholar]
- 13.Ahn MJ, Yang J, Yu H, et al. Osimertinib combined with durvalumab in EGFR-mutant non-small cell lung cancer: results from the TATTON phase Ib trial. J Thorac Oncol. 2016;11(4):S115. doi: 10.1016/S1556-0864(16)30246-5 [DOI] [Google Scholar]
- 14.Gangadhar TC. Efficacy and safety of epacadostat plus pembrolizumab treatment of NSCLC: preliminary phaseI/II results of ECHO-202/KEYNOTE-037. ASCO Annu Meeting Proc. 2017; 35: p9014. [Google Scholar]
- 15.Hellmann MD, Ciuleanu TE, Pluzanski A, et al. Nivolumab plus Ipilimumab in Lung Cancer with a High Tumor Mutational Burden. N Engl J Med. 2018;378(22):2093–2104. doi: 10.1056/NEJMoa1801946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Langer CJ, Gadgeel SM, Borghaei H, et al. Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol. 2016;17(11):1497–1508. doi: 10.1016/S1470-2045(16)30498-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gandhi L, Rodriguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018; 378: 2078–2092. doi: 10.1056/NEJMoa1801005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.