Because of its incidence and devastating consequences, Alzheimer's disease (AD) has attracted much research attention over the last decades. Intensive work has led to the identification of several cellular and molecular pathophysiological processes present in the disease, including tau alterations, β-amyloid (Aβ) deposition, lipid homeostasis dysregulation, excitotoxicity, neuroinflammation, and autophagy defects (Di Paolo and Kim, 2011; Ittner and Götz, 2011; Heppner et al., 2015; Menzies et al., 2015; Wang and Mandelkow, 2016). Despite much effort, how these different pathways interact and contribute to disease pathogenesis remains poorly understood.
Recent work has begun to investigate a possible role of microRNAs (miRNAs) in the development of AD (Femminella et al., 2015). miRNAs are a class of short noncoding regulatory RNAs that silence gene expression in plants, invertebrates, and mammals, including humans (Bartel, 2009). Mechanistically, miRNAs bind to short sequences found in target transcripts, resulting in mRNA destabilization and/or translational repression. The target sequence for a particular miRNA could be present in hundreds of mRNAs and a single transcript can, in turn, be targeted by multiple mRNAs (Huntzinger and Izaurralde, 2011). Because of this combinatorial mode of action, miRNAs are thought to act as high-order regulators of gene expression. Not surprisingly, miRNAs are involved in multiple biological processes (van Rooij et al., 2007; Pauli et al., 2011; Tan et al., 2013) and accumulating data suggest that disruption of miRNAs networks contribute to human disorders, including neurodegenerative diseases (Esteller, 2011; Gascon and Gao, 2012; Abe and Bonini, 2013). Moreover, transcriptomic studies have described specific and consistent alterations in miRNAs associated with AD, and some targets of these miRNAs have been implicated in pathophysiological cascades relevant to the disease (Femminella et al., 2015). Unfortunately, direct experimental data arguing for a causal role of miRNAs in AD are still scarce.
Work by Horie et al. (2010, 2012) suggests that miR-33 might be particularly important in these pathological cascades. They reported that miR-33 controls the expression of the cholesterol transporter, ABCA1, and reduces HDL cholesterol levels systemically (Horie et al., 2010). Genetic deletion of miR-33 induced plaque regression in a mouse model of atherosclerosis (Horie et al., 2012). This is relevant to AD because there is extensive literature support for a connection between cholesterol and β-amyloid homeostasis (Puglielli et al., 2001; Jiang et al., 2008; Choi et al., 2015). The presence of Aβ plaques, formed by the sequential cleavage of the amyloid precursor protein (APP) and deposition of Aβ oligomers, is a prominent neuropathologic feature of the disease and is thought to be central to AD development (Nhan et al., 2015). Moreover, polymorphisms of several genes encoding proteins that regulate cholesterol metabolism such as ApoE and ABCA1 have been associated with AD risk (Corder et al., 1993; Koldamova et al., 2010; Cramer et al., 2012). Therefore, if miR-33 also controls ABCA1 expression in the brain, it may have profound effects on cholesterol transport and therefore Aβ accumulation.
To test this idea, Kim et al. (2015) first examined miR-33 expression across different tissues and cell types. Remarkably, miR-33 was enriched in the brain—particularly in the cortex—and preferentially expressed by neurons. They next asked whether ABCA1 is a target of miR-33 in the brain. For that purpose, the authors quantified cortical levels of ABCA1 in miR-33−/− mice (Horie et al., 2010). Levels were significantly higher in miR-33-deficient animals than in wild-type, suggesting that ABCA1 is also a miR-33 target in the nervous system. miR-33 overexpression in a neuronal cell line as well as in primary astrocytes also regulated ABCA1 levels, further confirming the direct regulation of ABCA1 via miR-33.
The authors next asked whether miR-33 affected Aβ production. Indeed, in cell lines expressing mutated APP, miR-33 transfection resulted not only in a reduction of ABCA1 but also in increased secretion of Aβ. The ability of different cell types to degrade synthetic Aβ was also impaired by miR-33. Remarkably, restoring ABCA1 levels (using a miR-33-resistant construct) abolished the effects of miR-33 on Aβ homeostasis. Together, these findings strongly suggested that miR-33 control Aβ deposition by modulating ABCA1 levels.
Finally, Kim et al. (2015) validated the involvement of miR-33 in Aβ regulation in vivo. First, they showed that miR-33−/− mice had reduced cortical levels of Aβ products (Aβ40 and Aβ42) but normal APP levels. Then, using a mouse model of AD, they found that chronic treatment with a miR-33 antagonist caused a significant decrease in Aβ40. Overall, the data presented by Kim et al. (2015) provided additional evidence of the links between cholesterol and Aβ metabolism in the brain and, more importantly, pinpointed the essential role of miR-33 in modulating this pathogenic pathway.
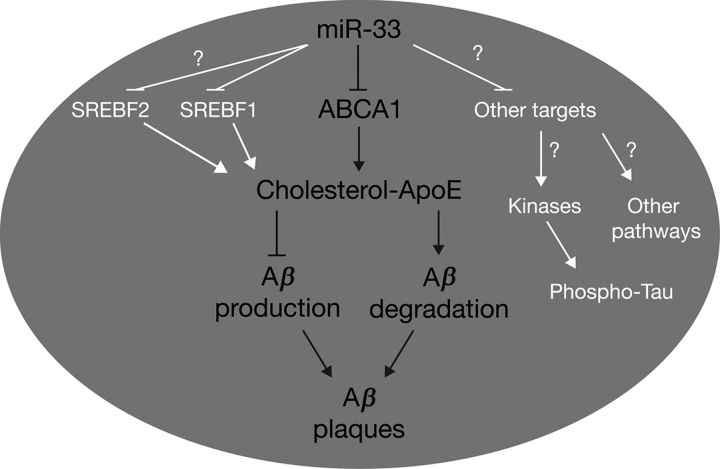
Kim et al. (2015) demonstrated that most cellular changes induced by manipulation of miR-33 levels could be rescued by ABCA1, indicating that this transporter is a central target in miR-33 regulatory events. Consistent with this notion, many previous studies have shown that some targets are more important than others depending on the context (Cassidy et al., 2013; Gascon et al., 2014). Nevertheless, miRNAs simultaneously silence multiple transcripts and regulation of other targets might result in synergistic effects. In this regard, it is worth noting that miR-33 controls the expression of SREBF1, a transcription factor known to modulate several genes involved in the synthesis and uptake of cholesterol (Horie et al., 2013). Furthermore, miR-33 is embedded in the locus of SREBF2, another member of the same family (Horie et al., 2010). Since intragenic miRNAs frequently target their host genes (Kos et al., 2012; Yuva-Aydemir et al., 2015), an attractive hypothesis is that miR-33 might control lipid homeostasis at multiple levels, thus acting as a molecular hub (Fig. 1).
Figure 1.
Schematic representation of the main findings reported in this study as well as of other pathways potentially regulated by miR-33 relevant to AD. Kim et al. (2015) demonstrated the essential function of miR-33 in modulating ABCA1 expression and how this transporter influenced cholesterol content of ApoE and, thereby, Aβ production and degradation (black fonts, center). miR-33 might exert further control on lipid metabolism by regulating the expression of the transcription factors SRBEF1 and 2 (white fonts, left). Other miR-33 targets (e.g., cyclin-dependent kinases) might further contribute to AD pathogenesis by activating complementary pathways [e.g., tau phosphorylation (white fonts, right)].
Along the same lines, computational algorithms (e.g., TargetScan) indicate that miR-33 may target multiple kinases families including those involved in tau phosphorylation, such as cyclin-dependent kinases or mitogen-activated protein kinases (Rudrabhatla, 2014). It is important to remember that although multiple theoretical scenarios regarding AD pathogenesis have been postulated, no single theory can successfully account for the clinical heterogeneity observed in the disease. Kim et al. (2015) demonstrated, in vitro and in vivo, a connection between Aβ deposition, cholesterol homeostasis, and miR-33 in the brain, suggesting that multiple mechanisms may simultaneously contribute to disease. It would be therefore interesting to assess, for example, whether miR-33 affects other known cascades, such as tau phosphorylation (Fig. 1).
It is important to note that Kim et al. (2015) did not investigate miR-33 levels in the brain of AD patients. A rapid survey to the deposited data in GEO (Gene Expression Omnibus) profiles showed that no changes in either miR-33a or miR-33b (two miR-33 homologs found in humans) were observed in three independent studies (Hébert et al., 2013; Lau et al., 2013; Santa-Maria et al., 2015). Although these data do not support the hypothesis that miR-33 contributes to AD pathology, they should be interpreted cautiously given the number of confounding variables intrinsic to these profiling studies. In addition to the heterogeneity of AD itself, variable comorbidities in analyzed cohorts, different postmortem intervals, or technical disparities might preclude the detection of miRNAs changes. In this regard, one could take advantage of miRNA profiling in mouse models of AD. Here, again, miR-33 expression was not significantly modified in the hippocampus of two different transgenic mice overexpressing APP (Barak et al., 2013; Noh et al., 2014), suggesting that miR-33 might not be involved in the pathogenesis of the disease. Nonetheless, as Kim et al. (2015) stated in their discussion, miR-33 may represent an attractive therapeutic target.
Regarding the therapeutic potential of miR-33 in AD, one should first address an essential question: would altering miR-33 levels alleviate cognitive deficits associated with AD? This is an important question that remains unexplored. Notably, there is conflicting evidence regarding the contribution of Aβ burden on functional impairment: some treatments have been shown to improve behavioral deficits without affecting Aβ pathology (Jankowsky et al., 2005; Cuadrado-Tejedor et al., 2011) whereas others found an inverse correlation between plaque content and behavioral performance (Cramer et al., 2012; Verma et al., 2015). Nevertheless, accumulating data indicate that soluble Aβ, rather than the insoluble material in the plaques, is the toxic species in AD (Fedele et al., 2015; Ferreira et al., 2015). Since miR-33 modulates both the generation and removal of Aβ oligomers, results obtained in this study support a positive effect of manipulating miR-33 levels on behavioral outcomes. Further work should evaluate this crucial issue and clarify whether treatments targeting miR-33 in mice are beneficial in reverting memory loss or other AD-associated symptoms as well as molecular pathology.
Footnotes
Editor's Note: These short, critical reviews of recent papers in the Journal, written exclusively by graduate students or postdoctoral fellows, are intended to summarize the important findings of the paper and provide additional insight and commentary. For more information on the format and purpose of the Journal Club, please see http://www.jneurosci.org/misc/ifa_features.shtml.
The authors declare no competing financial interests.
References
- Abe M, Bonini NM. MicroRNAs and neurodegeneration: role and impact. Trends Cell Biol. 2013;23:30–36. doi: 10.1016/j.tcb.2012.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barak B, Shvarts-Serebro I, Modai S, Gilam A, Okun E, Michaelson DM, Mattson MP, Shomron N, Ashery U. Opposing actions of environmental enrichment and Alzheimer's disease on the expression of hippocampal microRNAs in mouse models. Transl Psychiatry. 2013;3:e304. doi: 10.1038/tp.2013.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136:215–233. doi: 10.1016/j.cell.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy JJ, Jha AR, Posadas DM, Giri R, Venken KJ, Ji J, Jiang H, Bellen HJ, White KP, Carthew RW. miR-9a minimizes the phenotypic impact of genomic diversity by buffering a transcription factor. Cell. 2013;155:1556–1567. doi: 10.1016/j.cell.2013.10.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J, Gao J, Kim J, Hong C, Kim J, Tontonoz P. The E3 ubiquitin ligase Idol controls brain LDL receptor expression, ApoE clearance, and Abeta amyloidosis. Sci Transl Med. 2015;7:314ra184. doi: 10.1126/scitranslmed.aad1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, Roses AD, Haines JL, Pericak-Vance MA. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer's disease in late onset families. Science. 1993;261:921–923. doi: 10.1126/science.8346443. [DOI] [PubMed] [Google Scholar]
- Cramer PE, Cirrito JR, Wesson DW, Lee CY, Karlo JC, Zinn AE, Casali BT, Restivo JL, Goebel WD, James MJ, Brunden KR, Wilson DA, Landreth GE. ApoE-directed therapeutics rapidly clear beta-amyloid and reverse deficits in AD mouse models. Science. 2012;335:1503–1506. doi: 10.1126/science.1217697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuadrado-Tejedor M, Hervias I, Ricobaraza A, Puerta E, Pérez-Roldán JM, García-Barroso C, Franco R, Aguirre N, García-Osta A. Sildenafil restores cognitive function without affecting beta-amyloid burden in a mouse model of Alzheimer's disease. Br J Pharmacol. 2011;164:2029–2041. doi: 10.1111/j.1476-5381.2011.01517.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Paolo G, Kim TW. Linking lipids to Alzheimer's disease: cholesterol and beyond. Nat Rev Neurosci. 2011;12:284–296. doi: 10.1038/nrn3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esteller M. Non-coding RNAs in human disease. Nat Rev Genet. 2011;12:861–874. doi: 10.1038/nrg3074. [DOI] [PubMed] [Google Scholar]
- Fedele E, Rivera D, Marengo B, Pronzato MA, Ricciarelli R. Amyloid beta: walking on the dark side of the moon. Mech Ageing Dev. 2015;152:1–4. doi: 10.1016/j.mad.2015.09.001. [DOI] [PubMed] [Google Scholar]
- Femminella GD, Ferrara N, Rengo G. The emerging role of microRNAs in Alzheimer's disease. Front Physiol. 2015;6:40. doi: 10.3389/fphys.2015.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira ST, Lourenco MV, Oliveira MM, De Felice FG. Soluble amyloid-beta oligomers as synaptotoxins leading to cognitive impairment in Alzheimer's disease. Front Cell Neurosci. 2015;9:191. doi: 10.3389/fncel.2015.00191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gascon E, Gao FB. Cause or effect: misregulation of microRNA pathways in neurodegeneration. Front Neurosci. 2012;6:48. doi: 10.3389/fnins.2012.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gascon E, Lynch K, Ruan H, Almeida S, Verheyden JM, Seeley WW, Dickson DW, Petrucelli L, Sun D, Jiao J, Zhou H, Jakovcevski M, Akbarian S, Yao WD, Gao FB. Alterations in microRNA-124 and AMPA receptors contribute to social behavioral deficits in frontotemporal dementia. Nat Med. 2014;20:1444–1451. doi: 10.1038/nm.3717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hébert SS, Wang WX, Zhu Q, Nelson PT. A study of small RNAs from cerebral neocortex of pathology-verified Alzheimer's disease, dementia with lewy bodies, hippocampal sclerosis, frontotemporal lobar dementia, and non-demented human controls. J Alzheimers Dis. 2013;35:335–348. doi: 10.3233/JAD-122350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heppner FL, Ransohoff RM, Becher B. Immune attack: the role of inflammation in Alzheimer disease. Nat Rev Neurosci. 2015;16:358–372. doi: 10.1038/nrn3880. [DOI] [PubMed] [Google Scholar]
- Horie T, Ono K, Horiguchi M, Nishi H, Nakamura T, Nagao K, Kinoshita M, Kuwabara Y, Marusawa H, Iwanaga Y, Hasegawa K, Yokode M, Kimura T, Kita T. MicroRNA-33 encoded by an intron of sterol regulatory element-binding protein 2 (Srebp2) regulates HDL in vivo. Proc Natl Acad Sci U S A. 2010;107:17321–17326. doi: 10.1073/pnas.1008499107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horie T, Baba O, Kuwabara Y, Chujo Y, Watanabe S, Kinoshita M, Horiguchi M, Nakamura T, Chonabayashi K, Hishizawa M, Hasegawa K, Kume N, Yokode M, Kita T, Kimura T, Ono K. MicroRNA-33 deficiency reduces the progression of atherosclerotic plaque in ApoE−/− mice. J Am Heart Assoc. 2012;1:e003376. doi: 10.1161/JAHA.112.003376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horie T, Nishino T, Baba O, Kuwabara Y, Nakao T, Nishiga M, Usami S, Izuhara M, Sowa N, Yahagi N, Shimano H, Matsumura S, Inoue K, Marusawa H, Nakamura T, Hasegawa K, Kume N, Yokode M, Kita T, Kimura T, Ono K. MicroRNA-33 regulates sterol regulatory element-binding protein 1 expression in mice. Nat Commun. 2013;4:2883. doi: 10.1038/ncomms3883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huntzinger E, Izaurralde E. Gene silencing by microRNAs: contributions of translational repression and mRNA decay. Nat Rev Genet. 2011;12:99–110. doi: 10.1038/nrg2936. [DOI] [PubMed] [Google Scholar]
- Ittner LM, Götz J. Amyloid-beta and tau—a toxic pas de deux in Alzheimer's disease. Nat Rev Neurosci. 2011;12:65–72. doi: 10.1038/nrn2967. [DOI] [PubMed] [Google Scholar]
- Jankowsky JL, Melnikova T, Fadale DJ, Xu GM, Slunt HH, Gonzales V, Younkin LH, Younkin SG, Borchelt DR, Savonenko AV. Environmental enrichment mitigates cognitive deficits in a mouse model of Alzheimer's disease. J Neurosci. 2005;25:5217–5224. doi: 10.1523/JNEUROSCI.5080-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Q, Lee CY, Mandrekar S, Wilkinson B, Cramer P, Zelcer N, Mann K, Lamb B, Willson TM, Collins JL, Richardson JC, Smith JD, Comery TA, Riddell D, Holtzman DM, Tontonoz P, Landreth GE. ApoE promotes the proteolytic degradation of Abeta. Neuron. 2008;58:681–693. doi: 10.1016/j.neuron.2008.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Yoon H, Horie T, Burchett JM, Restivo JL, Rotllan N, Ramírez CM, Verghese PB, Ihara M, Hoe HS, Esau C, Fernández-Hernando C, Holtzman DM, Cirrito JR, Ono K, Kim J. microRNA-33 regulates ApoE lipidation and amyloid-beta metabolism in the brain. J Neurosci. 2015;35:14717–14726. doi: 10.1523/JNEUROSCI.2053-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koldamova R, Fitz NF, Lefterov I. The role of ATP-binding cassette transporter A1 in Alzheimer's disease and neurodegeneration. Biochim Biophys Acta. 2010;1801:824–830. doi: 10.1016/j.bbalip.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kos A, Olde Loohuis NF, Wieczorek ML, Glennon JC, Martens GJ, Kolk SM, Aschrafi A. A potential regulatory role for intronic microRNA-338-3p for its host gene encoding apoptosis-associated tyrosine kinase. PLoS One. 2012;7:e31022. doi: 10.1371/journal.pone.0031022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau P, Bossers K, Janky R, Salta E, Frigerio CS, Barbash S, Rothman R, Sierksma AS, Thathiah A, Greenberg D, Papadopoulou AS, Achsel T, Ayoubi T, Soreq H, Verhaagen J, Swaab DF, Aerts S, De Strooper B. Alteration of the microRNA network during the progression of Alzheimer's disease. EMBO Mol Med. 2013;5:1613–1634. doi: 10.1002/emmm.201201974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menzies FM, Fleming A, Rubinsztein DC. Compromised autophagy and neurodegenerative diseases. Nat Rev Neurosci. 2015;16:345–357. doi: 10.1038/nrn3961. [DOI] [PubMed] [Google Scholar]
- Nhan HS, Chiang K, Koo EH. The multifaceted nature of amyloid precursor protein and its proteolytic fragments: friends and foes. Acta Neuropathol. 2015;129:1–19. doi: 10.1007/s00401-014-1347-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noh H, Park C, Park S, Lee YS, Cho SY, Seo H. Prediction of miRNA-mRNA associations in Alzheimer's disease mice using network topology. BMC Genomics. 2014;15:644. doi: 10.1186/1471-2164-15-644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pauli A, Rinn JL, Schier AF. Non-coding RNAs as regulators of embryogenesis. Nat Rev Genet. 2011;12:136–149. doi: 10.1038/nrg2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puglielli L, Konopka G, Pack-Chung E, Ingano LA, Berezovska O, Hyman BT, Chang TY, Tanzi RE, Kovacs DM. Acyl-coenzyme A: cholesterol acyltransferase modulates the generation of the amyloid beta-peptide. Nat Cell Biol. 2001;3:905–912. doi: 10.1038/ncb1001-905. [DOI] [PubMed] [Google Scholar]
- Rudrabhatla P. Regulation of neuronal cytoskeletal protein phosphorylation in neurodegenerative diseases. J Alzheimers Dis. 2014;41:671–684. doi: 10.3233/JAD-130794. [DOI] [PubMed] [Google Scholar]
- Santa-Maria I, Alaniz ME, Renwick N, Cela C, Fulga TA, Van Vactor D, Tuschl T, Clark LN, Shelanski ML, McCabe BD, Crary JF. Dysregulation of microRNA-219 promotes neurodegeneration through post-transcriptional regulation of tau. J Clin Invest. 2015;125:681–686. doi: 10.1172/JCI78421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan CL, Plotkin JL, Venø MT, von Schimmelmann M, Feinberg P, Mann S, Handler A, Kjems J, Surmeier DJ, O'Carroll D, Greengard P, Schaefer A. MicroRNA-128 governs neuronal excitability and motor behavior in mice. Science. 2013;342:1254–1258. doi: 10.1126/science.1244193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Rooij E, Sutherland LB, Qi X, Richardson JA, Hill J, Olson EN. Control of stress-dependent cardiac growth and gene expression by a microRNA. Science. 2007;316:575–579. doi: 10.1126/science.1139089. [DOI] [PubMed] [Google Scholar]
- Verma M, Beaulieu-Abdelahad D, Ait-Ghezala G, Li R, Crawford F, Mullan M, Paris D. Chronic anatabine treatment reduces Alzheimer's disease (AD)-like pathology and improves socio-behavioral deficits in a transgenic mouse model of AD. PLoS One. 2015;10:e0128224. doi: 10.1371/journal.pone.0128224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Mandelkow E. Tau in physiology and pathology. Nat Rev Neurosci. 2016;17:22–35. doi: 10.1038/nrn.2015.1. [DOI] [PubMed] [Google Scholar]
- Yuva-Aydemir Y, Xu XL, Aydemir O, Gascon E, Sayin S, Zhou W, Hong Y, Gao FB. Downregulation of the host gene jigr1 by miR-92 is essential for neuroblast self-renewal in Drosophila. PLoS Genet. 2015;11:e1005264. doi: 10.1371/journal.pgen.1005264. [DOI] [PMC free article] [PubMed] [Google Scholar]