Abstract
Background: Laser acupuncture (LA)—the use of nonthermal, low-intensity laser irradiation to stimulate acupuncture points—has become more common among acupuncture practitioners in recent years. LA is promoted as a safer pain-free alternative to traditional acupuncture, with minimal adverse effects and greater versatility. However, little is known about the mechanism of action of LA, laser characteristics, and effectiveness of LA therapy.
Objective: This concise review of LA describes basic parameters and procedures, potential mechanisms of action, and the current evidence for its clinical efficacy. The article also highlights the need for more robust research on LA that can be translated into evidence-based clinical practices.
Conclusions: LA has many features that make it an attractive option as a treatment modality, including minimal sensation; short duration of treatment; and minimal risks of infection, trauma, and bleeding complications. Future studies with high-quality methodologies, ample sample sizes, and consistent and reproducible laser parameters are critically needed to increase understanding and establish potential future clinical applications.
Keywords: complementary and integrative medicine, low-level laser therapy, traditional acupuncture
Introduction
Acupuncture, a key component of Traditional Chinese Medicine, is believed to have been practiced for more than 2500 years, and this modality is among the oldest healing practices in the world. Acupuncture is based on the idea that living beings have Qi, defined as an inner energy, and that it is an imbalance in Qi or interruption in the flow of Qi that causes illness and disease. Acupuncture therapy is focused on rebalancing the flow of Qi,1 and the practice is progressively gaining credibility as a primary or adjuvant therapy by Western medical providers.2
Historically, stimulation of skin at specific acupoints might have been performed with stones or bones; currently, traditional acupuncture is performed by inserting a metal filiform needle into the skin at an acupoint, and electric currents can be passed between needles (electroacupuncture [EA]).1 More recently, acupuncture practitioners have begun to use nonthermal, low-intensity laser irradiation to stimulate acupoints. Laser acupuncture (LA), also termed low-level laser therapy (LLLT), dates back to the 1970s with successful treatment of asthma and hypertension in the Soviet Union.3 In 1984, Zhou4 reported using LA as a type of controlled anesthetic during oromaxillofacial surgery. More recently, LA has been shown, via functional magnetic resonance imaging (fMRI), to elicit cerebral activation, with involved brain areas corresponding to specific acupoints.5 LA has also been incorporated into veterinary medicine as a way to accelerate healing in cases such as spinal-cord injury.6,7
LA may be the preferred acupuncture modality for specific patient populations—such as geriatric and pediatric patients—because it is noninvasive, pain-free, and possibly associated with fewer adverse effects. The treatment length of an individual LA session (10–60 seconds per acupuncture site) is shorter than that with metal needles (10–30-minute retention time), which can reduce the treatment time significantly.8 Portable LA machines can offer convenient, efficient, and cost-effective treatment. Application of LA involves many considerations, including existing data, technical parameters, clinical indications, safety, and future research to promote evidence-based clinical practices. The objectives of this review are to offer a summary of LA, including up-to-date knowledge and potential future of LA in medicine.
Mechanism of Action
In acupuncture, needles are inserted at specific acupoints, which may be manually stimulated in various ways, including gentle twisting or up-and-down movements. In addition, the depth of needle penetration is also manipulated by the acupuncture practitioner. The patient may report sensations of De Qi, which are feelings of pressure, warmth, or tingling in the superficial layers of the skin. Many theories to explain how acupuncture works have been proposed, including the gate-control theory of pain and the endorphin-and-neurotransmitter model.1 Others have postulated that acupuncture modulates transmission of pain signals and alters release of endogenous endorphins and neurotransmitters, resulting in physiologic changes.1
One clear difference between needle acupuncture and LA is that LA does not physically penetrate the skin. Despite greater understanding of LA, it is unclear how nonthermal, low-intensity laser irradiation stimulates acupoints, and it is possible that the mechanism of LA is entirely separate from our present understanding of acupuncture. Current theories postulate that LLLT could have a positive effect on modulating inflammation, pain, and tissue repair, given appropriate irradiation parameters.9
Variables in LA could affect the degree of physiologic response. The structure of skin is multilayered, inhomogeneous, and anisotropic, which makes its optical properties complex. In addition, scattering and absorption causes incident light to generally decrease in an exponential- and wavelength-dependent manner as it passes through skin,10 and power output and energy doses also affect the level of light penetration and scattering. Furthermore, heterogeneity among individuals in terms of skin pigment, thickness, and location on the body makes light penetration inconsistent and difficult to standardize. Hemoglobin and melanin can absorb ultraviolet radiation and some wavelengths of visible light (380–625 nm), which limits light transmission through skin.10 In contrast, visible red light and infrared radiation (625–1000 nm) are absorbed less and thus are most often used for LA.11,12 In addition, different wavelengths, power outputs, and energy doses also affect the level of light penetration and scattering. Because of the many confounding variables inherent to LA, clear objective evaluation continues to be a challenge.
Several animal and human studies have provided additional insight into the potential physiologic effects of laser therapy.
Anti-Inflammatory Effect of Lasers
Inflammation reduction comparable to that of nonsteroidal anti-inflammatory drugs has been reported with animal studies that used red and near-infrared LLLT, with laser outputs ranging from 2.5 to 100 mW and delivered energy doses ranging from 0.6 to 9.6 Joules. Human studies have shown similar anti-inflammatory effects with LLLT, which may account for many of the associated positive clinical effects.13
Neural Modulation by Laser
Low-level laser stimulation of acupoints has been reported to influence peripheral and central nervous system activity. In an animal study, stimulation of acupoints LI 4 and ST 36 with a 780-nm laser decreased somatosensory-evoked potentials activated by noxious stimulation of tooth pulp.14 The reduction observed with lasers was similar to that associated with EA of the same acupoints. The reduced amplitude of somatosensory-evoked potentials corresponded to the production of analgesia.
In a human study, LA of the acupoint BL 67, empirically associated with ophthalmic disorders, resulted in activation of visual cortex areas on fMRI.5 Sham acupuncture at that acupoint did not show activation.
In a study of 50 patients with diabetes mellitus and mild-to-moderate, unilateral, carpal tunnel syndrome, application of an infrared laser (20 mW; dose: 4.8 Joules) was compared with ultrasound applied to the symptomatic volar wrist.15 One stimulation point was over the median nerve, 5 cm proximal to the volar wrist crease (approximate location of the PC 6 acupoint). The cohort receiving laser treatment had marked pain reduction (∼ 4.5 points on a 10-point visual analogue scale). In electrophysiologic tests, the laser cohort had significantly reduced (improved) median distal motor and sensory latencies (P ≤ 0.05 for both) and increased (improved) median compound muscle action potential amplitudes and median motor conduction velocity (P ≤ 0.03 for both).
Cellular Effects of LLLT
Red and infrared laser wavelengths are absorbed by cytochrome C oxidase protein in the mitochondrial cell membranes. This absorption is associated with increased adenosine triphosphate production by the mitochondria, which. in turn, increases intracellular calcium (Ca2+) and cyclic adenosine monophosphate, which serve as secondary messengers that aid in regulation of multiple body processes, including signal transfer in nerves and gene expression.16
Nitric oxide (NO) inhibits cytochrome C oxidase activity, but LLLT dissociates NO from cytochrome C oxidase and improves cell physiology through increased cellular respiration. LLLT also protects cells against NO-induced death.16
LLLT appears to improve cell physiology by increasing the overall cell redox potential toward greater oxidation and increased reactive oxygen species while simultaneously decreasing reactive nitrogen species. These changes in the redox state activate numerous intracellular-signaling pathways, including nucleic-acid synthesis, protein synthesis, enzyme activation, and cell cycle progression.17 LLLT also alters expression of genes that can enhance cell growth and inhibit cell apoptosis.16 These cellular effects of LLLT might reflect its ability to induce long-term changes in cells and LLLT's benefits for wound healing, nerve regeneration, and reduction of inflammation.
Laser Characteristics
Lasers with output exceeding 500 mW, which are used for heating and direct tissue effects (e.g., tissue coagulation in surgery applications) are categorized as Class 4 “hard” lasers.18 In contrast, lasers used for acupuncture applications typically have a power output of 5–499 mW and are categorized as Class 3b “soft” lasers. Some commercially available “laser devices” are not true lasers; rather, they use arrays of red or infrared light-emitting diodes (LEDs) that have noncollimated light outputs. Noncollimated light scatters and reflects at superficial skin layers, which limits energy penetration through the skin. Because the acupuncture meridians and their acupoints are thought to exist in the myofascial layer of the body,19 the low energy penetration of LED devices theoretically fails to stimulate acupoints. However, LED devices often compensate for light scatter by using higher-output LEDs to enhance energy penetration through the skin.
The power density of a laser, defined as laser energy supplied per area (W/cm2), influences its depth of energy penetration. A 50-mW laser with a beam size of 1 cm2 has an energy density of 0.05 W/cm2, whereas the same power laser with a beam size of 1 mm2 has an energy density of 5 W/cm2. A higher energy density results in deeper energy penetration through skin.
Energy transmission through the skin is also affected by absorption of light energy by skin structures. Light wavelengths from 650 to 900 nm have the best penetration through skin. Lower wavelengths are absorbed by melanin and hemoglobin, and wavelengths longer than 900 nm are absorbed by water. With a well-focused laser beam, red wavelengths (∼ 648 nm) can penetrate 2–4 cm beneath the skin surface, and infrared wavelengths (∼ 810 nm) can penetrate up to 6 cm.20,21
LA devices may have 1 beam (a single-channel device) or multiple beams. The Weber* laser needle system20 has 12 separate lasers to treat multiple acupoints simultaneously.
Safety of LA
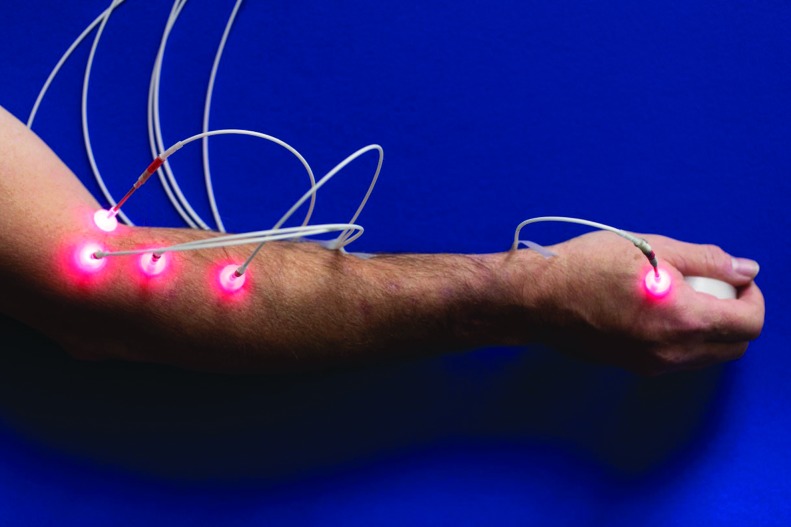
In contrast to needle acupuncture, LA is noninvasive and can be a more feasible treatment for young and elderly patients or those who are afraid of needles.22 Typically, patients do not feel any sensations when a low-light laser is used,23 although some patients have reported a tingling or “light touch” sensation.24 Adverse effects, such as transient dizziness, headaches, and fatigue have been reported with LA.24 The noninvasive nature of LA also minimizes the risk of adverse events, such as organ puncture, infection, or bleeding complications25 (Fig 1). LA also facilitates stimulation of areas that are difficult or uncomfortable to needle, such as auricular acupoints.26 By using a multichannel laser system, multiple acupoints can be treated simultaneously, just as in a metal-needle acupuncture treatment.20
FIG.1. Acupuncture of an upper extremity with red-laser needles.
Because the lasers used in LA are Class 3b lasers, irradiation could potentially cause serious eye damage; therefore, patients and providers must wear protective eyewear during treatment. In addition, other precautions should be undertaken, including not directing the laser toward the fetus if a patient is pregnant, not irradiating the heart region of patients with cardiac conditions, and avoiding hemorrhagic areas and the gonads. The epiphyseal line in children should be avoided, and children younger than age 2 should not receive LA. Direct irradiation of tumors should be avoided because it may stimulate their growth.27
Clinical Evidence of LA's Effectiveness
Globally, LA continues to be used clinically and experimentally as a sole or adjunct modality for various indications, most commonly management of chronic pain.28 Studies on LA have mostly examined musculoskeletal disorders, with pain reduction as the primary endpoint.9 Despite the growth, popularity, safety profile, and versatility of LA, its effectiveness in the clinical setting remains unclear. The skepticism surrounding LA is compounded by the fact that its mechanisms of action are understood poorly. In addition, no specific guidelines have been developed for LA with regard to laser parameters and energy dosages; hence, studies are difficult to replicate and results are inconsistent.29 Conclusions of previous studies have been challenged because of the poor methodology and inconsistent laser parameters used.10
In 2008, Baxter and colleagues28 conducted a systematic review of randomized controlled trials (RCTs) to examine the clinical effectiveness of LA. These researchers identified moderate evidence supporting LA as an effective treatment for reducing myofascial pain and moderate evidence supporting the use of LA for postoperative nausea and vomiting. LA has limited evidence supporting its use for treating chronic tension headaches and insufficient evidence for treating lateral epicondylitis. In 2015, Law and colleagues29 conducted a systematic review and similarly reported moderate evidence supporting the use of LA for managing musculoskeletal pain, when applied in appropriate treatment dosages. Other systematic reviews that included LA as a treatment modality for asthma in children noted that total sample sizes were small and the methodologic quality of the studies was low, with no compelling evidence to suggest that LA was an effective treatment option.30 Similarly, LA was not effective for obesity management.31
Discussion
This concise review of LA, we provides additional insight and understanding about a kind of treatment that is becoming more common among acupuncture practitioners. Although LA is promoted as a safer, pain-free alternative to traditional acupuncture, with minimal adverse effects and greater versatility, much remains to be learned about its mechanism of action, how laser characteristics interact with human tissue, and ultimately, the effectiveness of LA.
Existing evidence provides some insight into the anti-inflammatory effects, neuromodulation, and cellular effects of LLLT; however, the data remain sparse overall. Only a limited number of studies have assessed the effects of LLLT on specific acupoints. More robust studies are needed to examine the effects of LLLT on additional acupoints and to determine how these effects may be translated into clinical outcomes. Differences in laser characteristics—such as wavelength, power output, and energy dose—affect the level of light scattering and penetration through skin tissue. In addition, light penetration is difficult to standardize because of the complex optical properties of skin and heterogeneity in skin characteristics and treatment locations among individuals. The skepticism surrounding LA is compounded by the absence of guidelines for laser parameters and energy dosages. Studies remain difficult to replicate, and published results are inconsistent. However, systematic reviews of RCTs examining the clinical effectiveness of LA show promise in supporting it as an effective treatment for reducing myofascial pain and for managing musculoskeletal pain, and support LA's use for addressing postoperative nausea and vomiting.
LA has many features that make it an attractive treatment option, compared with classic acupuncture, for certain patient populations. LA may be preferred by pediatric and geriatric patients and by patients with needle phobias because it does not penetrate the skin, and LA is associated with minimal sensation and minimal risk of infection, trauma, and bleeding complications. These features may make LA more feasible in patients with serious comorbid conditions, hospitalized patients, and other patients with increased risks of complications such as bleeding and infection. In addition, the duration of treatment is generally shorter, and more acupoints can be used during finite treatment times.
Conclusions
Despite the growing understanding of the physiologic effects of LLLT and its interactions with animal and human tissue, the mechanism of action of LA is still not understood clearly. Conclusions drawn from systematic reviews of the existing published trials are often weakened by inconsistencies in methodology and laser parameters used and by the small sample sizes, highlighting the critical need to conduct additional studies with high-quality methodologies, greater sample sizes, and laser parameters that are consistent and reproducible. These changes will increase understanding of LA and can be used to establish clear recommendations for its clinical applications.
Author Disclosure Statement
No competing financial interests exist.
The Mayo Clinic does not endorse specific products or services included in this article.
References
- 1. Chon TY, Lee MC. Acupuncture. Mayo Clin Proc. 2013;88(10):1141–1146 [DOI] [PubMed] [Google Scholar]
- 2. Astin JA, Marie A, Pelletier KR, Hansen E, Haskell WL. A review of the incorporation of complementary and alternative medicine by mainstream physicians. Arch Intern Med. 1998;158(21):2303–2310 [DOI] [PubMed] [Google Scholar]
- 3. Gamaleya NF. Laser biomedical research in the USSR. In: Wolbarsht ML, ed. Laser Applications in Medicine and Biology. New York: Plenum; 1977 [Google Scholar]
- 4. Zhou YC. An advanced clinical trial with laser acupuncture anesthesia for minor operations in the oro-maxillofacial region. Lasers Surg Med. 1984;4(3):297–303 [DOI] [PubMed] [Google Scholar]
- 5. Siedentopf CM, Golaszewski SM, Mottaghy FM, Ruff CC, Felber S, Schlager A. Functional magnetic resonance imaging detects activation of the visual association cortex during laser acupuncture of the foot in humans. Neurosci Lett. 2002;327(1):53–56 [DOI] [PubMed] [Google Scholar]
- 6. Riegel RJ, Godbold JCJ. Part 1: The history of laser therapy. In: Laser Therapy in Veterinary Medicine. Photobiomodulation, 1st ed: Hoboken, NJ: Wiley–Blackwell; 2017:3–6 [Google Scholar]
- 7. Habacher G, Pittler MH, Ernst E. Effectiveness of acupuncture in veterinary medicine: Systematic review. J Vet Intern Med. 2006;20(3):480–488 [DOI] [PubMed] [Google Scholar]
- 8. Hu WL, Chang CH, Hung YC, Tseng YJ, Hung IL, Hsu SF. Laser acupuncture therapy in patients with treatment-resistant temporomandibular disorders. PLoS One. 2014;9(10):e110528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516–533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Whittaker P. Laser acupuncture: Past, present, and future. Lasers Med Sci. 2004;19(2):69–80 [DOI] [PubMed] [Google Scholar]
- 11. Wan S, Parrish JA, Anderson RR, Madden M. Transmittance of nonionizing radiation in human tissues. Photochem Photobiol. 1981;34(6):679–681 [DOI] [PubMed] [Google Scholar]
- 12. Anderson RR, Parrish JA. The optics of human skin. J Invest Dermatol. 1981;77(1):13–19 [DOI] [PubMed] [Google Scholar]
- 13. Bjordal JM, Lopes-Martins RAB, Joensen J, Iversen VV. The anti-inflammatory mechanism of low level laser therapy and its relevance for clinical use in physiotherapy. Physical Ther Rev. 2010;15(4):286–293 [Google Scholar]
- 14. Sing T, Yang MM. Electroacupuncture and laser stimulation treatment: Evaluated by somatosensory evoked potential in conscious rabbits. Am J Chin Med. 1997;25(3–4):263–271 [DOI] [PubMed] [Google Scholar]
- 15. Ahmed OF, Elkharbotly AM, Taha N, Bekheet AB. Treatment of mild to moderate carpal tunnel syndrome in patients with diabetic neuropathy using low level laser therapy versus ultrasound controlled comparative study. BBA Clin. 2017;8:43–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Farivar S, Malekshahabi T, Shiari R. Biological effects of low level laser therapy. J Lasers Med Sci. 2014;5(2):58–62 [PMC free article] [PubMed] [Google Scholar]
- 17. Cotler HB, Chow RT, Hamblin MR, Carroll J. The use of low level laser therapy (LLLT) for musculoskeletal pain. MOJ Orthop Rheumatol. 2015;2(5).pii: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. International Electrotechnical Commission (IEC). IEC 60825-1:2014/ISH1:2017 Interpretation Sheet 1—Safety of Laser Products—Part 1: Equipment Classification and Requirements. Geneva: International Electrotechnical Commission; 2017. Online document at: www.nen.nl/pdfpreview/preview_242393.pdf Accessed May20, 2019 [Google Scholar]
- 19. O'Connor J, Bensky D. Acupuncture: A Comprehensive Text. Seattle: Eastland Press; 1981 [Google Scholar]
- 20. Weber M, Fussganger-May T, Wolf T. “Needles of Light”: A new therapeutic approach. Med Acupunct. 2007;19(3):141–150 [Google Scholar]
- 21. Romberg H. How is (laser)-light working? COMED. 2001;11:27–33 [Google Scholar]
- 22. Radmayr C, Schlager A, Studen M, Bartsch G. Prospective randomized trial using laser acupuncture versus desmopressin in the treatment of nocturnal enuresis. Eur Urol. 2001;40(2):201–205 [DOI] [PubMed] [Google Scholar]
- 23. Quah-Smith I, Sachdev PS, Wen W, Chen X, Williams MA. The brain effects of laser acupuncture in healthy individuals: An FMRI investigation. PLoS One. 2010;5(9):e12619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Quah-Smith I, Williams MA, Lundeberg T, Suo C, Sachdev P. Differential brain effects of laser and needle acupuncture at LR8 using functional MRI. Acupunct Med. 2013;31(3):282–289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM. Efficacy of low-level laser therapy in the management of neck pain: A systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet. 2009;374(9705):1897–1908 [DOI] [PubMed] [Google Scholar]
- 26. Round R, Litscher G, Bahr F. Auricular acupuncture with laser. Evid Based Complement Alternat Med. 2013;2013:984763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Uemoto L, Nascimento de Azevedo R, Almeida Alfaya T, Nunes Jardim Reis R, Depes de Gouvêa CV, Cavalcanti Garcia MA. Myofascial trigger point therapy: Laser therapy and dry needling. Curr Pain Headache Rep. 2013;17(9):357. [DOI] [PubMed] [Google Scholar]
- 28. Baxter GD, Bleakley C, McDonough S. Clinical effectiveness of laser acupuncture: A systematic review. J Acupunct Meridian Stud. 2008;1(2):65–82 [DOI] [PubMed] [Google Scholar]
- 29. Law D, McDonough S, Bleakley C, Baxter GD, Tumilty S. Laser acupuncture for treating musculoskeletal pain: A systematic review with meta-analysis. J Acupunct Meridian Stud. 2015;8(1):2–16 [DOI] [PubMed] [Google Scholar]
- 30. Zhang J, Li X, Xu J, Ernst E. Laser acupuncture for the treatment of asthma in children: A systematic review of randomized controlled trials. J Asthma. 2012;49(7):773–777 [DOI] [PubMed] [Google Scholar]
- 31. Namazi N, Khodamoradi K, Larijani B, Ayati MH. Is laser acupuncture an effective complementary therapy for obesity management? A systematic review of clinical trials. Acupunct Med. 2017;35(6):452–459 [DOI] [PubMed] [Google Scholar]