Abstract
Safe and stable housing is integral to addiction recovery. Across numerous studies, recovery housing has been found to be associated with improvements in a variety of domains. Although procedures for operating some types of recovery housing have been manualized and national standards established, there are few empirical findings identifying which recovery residence characteristics may lead to improved outcomes. Using data from 330 newly admitted residents recruited from 49 sober living houses in California and re-contacted for 6- and 12-month follow-up interviews, this study examines the effects of organizational, operational, and programming characteristics on substance use, criminal justice, and employment outcomes. Results from multilevel analyses adjusting for resident demographics and length of stay indicate that organizational characteristics were associated with outcomes. Residents recruited from houses that were part of a larger organization or group of houses had increased odds of total abstinence (aOR=3.98, p<0.001) and drug abstinence (aOR=3.19, p<0.001). Residents recruited from houses that were affiliated with a treatment program had increased odds of employment (aOR=2.92, p=0.003). Operational characteristics such as where the house was located and whether the house required incoming residents to be sober for at least 30 days prior to entry were also related to improved outcomes, but additional work is needed to develop tools to assess and measure recovery housing characteristics and to better understand how these factors contribute to improved outcomes.
Keywords: Sober living, sober living houses, recovery housing, recovery residences, recovery outcomes
1. Introduction
Although addiction is recognized as a chronic condition necessitating lifestyle change and ongoing care (American Society of Addiction Medicine, 2018; Dennis & Scott, 2007; McLellan, Lewis, O’Brien, & Kleber, 2000), most addiction treatment is time-limited and may not include the type of services clients prioritize as being most critical to their recovery from addiction (Duffy & Baldwin, 2013; Laudet, Stanick, & Sands, 2009; Laudet & White, 2010). Safe and stable housing is integral to recovery (Substance Abuse and Mental Health Services Administration, 2012), but nearly a third (32%) of individuals entering substance abuse treatment report being marginally housed in the 30 days prior to treatment entry (Eyrich-Garg, Cacciola, Carise, Lynch, & McLellan, 2008). Recovery housing generally refers to supportive living environments (e.g., Oxford Houses™, sober living, sober homes, recovery homes, halfway houses) that promote recovery from alcohol, drug use, and associated problems (Jason, Mericle, Polcin, & White, 2013). Reviews of the evidence base for recovery housing suggest that it can indeed have positive effects on many aspects of recovery, particularly with respect to substance use, employment, and criminal justice outcomes (Reif et al., 2014).
One of the more well-researched models of recovery housing is that of sober living houses (SLHs) in California. SLHs do not provide group counseling, case management, treatment planning, or a structure of daily activities. However, a study tracking 300 residents living in SLHs over an 18-month period, found that residents showed significant improvement on a wide variety of outcomes including alcohol and drug use, 6-month abstinence rates, alcohol and drug related problems, psychiatric symptoms, employment, and arrests (Polcin, Korcha, Bond, & Galloway, 2010a). All of the improvements between baseline and 6-month follow-up were maintained at 12- and 18-month follow up. Importantly, improvements were maintained even though the vast majority of residents left the SLHs by 18 months (Polcin, Korcha, Bond, & Galloway, 2010). Another study of 330 residents on probation or parole entering SLHs found similar improvements on substance abuse, criminal justice, HIV risk, and employment outcomes, but also found enhanced criminal justice outcomes among those randomized to Motivational Interviewing Case Management intervention who received at least one session (Polcin, Korcha, Witbrodt, Mericle, & Mahoney, in press).
1.1. Recovery residences as service delivery entities
Explaining how recovery housing improves outcomes can be challenging because recovery residences are often described in terms of what they do not do, rather than by what they do. Recovery from addiction is increasingly recognized as a process that results in, and is supported by, the accumulation of financial, social, human, and cultural resources, collectively termed, “recovery capital” (Cloud & Granfield, 2008; Granfield & Cloud, 1999). While some types of recovery residences may provide group or individual substance use treatment and/or recovery support services (Mericle, Miles, & Cacciola, 2015; Mericle, Polcin, Hemberg, & Miles, 2017), recovery residences can help residents build recovery capital across these domains in other ways through conscience decisions about where and how they operate and who they serve. For example, by providing residents with affordable housing, it can help residents accrue financial capital. Choice of location may be directly related to fees charged and other aspects of cost of living; it may also affect other forms of recovery capital as neighborhood context (e.g., neighborhood disadvantage, drug availability, community resources, and travel burden) has been postulated to be a critical component of retention in substance use treatment (Jacobson, 2004). Living amongst other peers in recovery has been shown to build social support and instill a sense of community (Ferrari, Jason, Olson, Davis, & Alvarez, 2002; Jason, Light, Stevens, & Beers, 2014; Jason, Stevens, & Light, 2016; Stevens, Guerrero, Green, & Jason, 2018; Stevens, Jason, Ram, & Light, 2015), and this may be enhanced in residences focusing on a specific segment of persons in recovery (Jason, Luna, Alvarez, & Stevens, 2016; Mericle, Carrico, Hemberg, de Guzman, 2017). Delineating and enforcing house rules, promoting accountability to members of the household, encouraging involvement in mutual aid groups, and fostering communal learning drawing from “collective experiential knowledge” (Borkman, 1999; Heslin et al., 2013; Jason, Davis, Ferrari, & Anderson, 2007) may enhance a variety of different aspects of human capital as well.
As mentioned above, SLHs do not provide treatment services, but residents are either encouraged or required to attend 12-step meetings, and they can stay as long as they wish, provided they abide by house rules (such as maintaining abstinence from alcohol and drugs) and pay fees for rent, utilities, etc. (Polcin & Henderson, 2008). Further, in SLHs like in other types of recovery housing, a social model philosophy of recovery (Kaskutas, Greenfield, Borkman, & Room, 1998) is promoted. Evolving from the traditions of AA, social model programs emphasize resident input into house operations and management, experiential knowledge and peer support for recovery, and resident responsibility for maintaining the home (Borkman, Kaskutas, Room, Bryan, & Barrows, 1998; Room, Kaskutas, & Piroth, 1998), all facets that contribute to the inherent therapeutic nature of the setting, which has shown to produce abstinence outcomes independent of residents’ 12-step involvement (Majer, Jason, Aase, Droege, & Ferrari, 2013). Thus, operational characteristics reflecting where housing is located, fees charged and amenities provided, who is served, and house rules as well as the overall program orientation or philosophy are critical components to the service delivered in recovery housing more generally but SLHs in particular.
1.2. Recovery residences as human service organizations
By providing a service in an organized and systematic manner to maintain or promote the overall quality of life of a population, recovery residences, like substance use treatment programs more generally, can be conceptualized as providing human services (Hasenfeld, 2010; Zins, 2001). Theories applied to understanding organizations, including human service organizations, are often categorized into rational, natural, and open-systems perspectives (Scott & Davis, 2007). Open-systems theories view organizations as engaging in a series of exchanges with various stakeholders to obtain resources (funding, residents, staff, licensing/accreditation). These theories as well as management and treatment technology factors (e.g., staffing and expertise) may be particularly useful to understanding substance use treatment programs (D’Aunno, 2006; Ghose, 2008). One particularly influential open-systems theory, resource dependency theory (Pfeffer & Salancik, 1978), speaks to how organizations act to reduce environmental uncertainty and interact with other organizations to reduce scarcity, such as with mergers and vertical integration, joint ventures, and other inter-organizational relationships (Hillman, Withers, & Collins, 2009).
Resource dependence theory is relevant to understanding recovery housing, especially among types like SLHs that do not provide treatment, because recovery residences are often providing a service to those who may have recently completed treatment but may have ongoing needs for services that are not provided by the operator. In the literature, there are examples of treatment providers operating their own recovery residences (Polcin, 2009), recovery residence operators opening their own treatment programs (Mericle et al., 2017), and, as they are often a critical component of a recovery-oriented system of care (White, 2008), recovery residences having linkages with a variety of different types of service providers in diverse service delivery sectors (Mericle et al., 2015). Further, whether it be to expand the reach of their service geographically or to a broader population of residents or even to create different levels of care, it is also common for recovery residence operators to operate more than one recovery residence (Miles, Reif, & Mericle, 2017; Polcin, Korcha, Bond, & Galloway, 2010b).
Staffing and management practices are also important factors in understanding recovery housing because some types of recovery housing have no paid staff in the house, and models that have house managers (like SLHs) generally prioritize experiential knowledge over counseling or other allied professional degrees. Further, because most recovery housing models operate by residents paying out-of-pocket for expenses associated with operating the residence (as in the SLH model), there is often a direct relationship between the number of residents in the house and fees charged per resident. Lack of staff education and training as well as high client-to-staff ratios have been found to be associated with worse outcomes among those in residential substance use treatment settings (Grella & Stein, 2006; Hser, Joshi, Maglione, Chou, & Anglin, 2001), but it is unclear whether the potential benefits of experiential knowledge and affordability may result in different effects in recovery housing settings.
1.3. Need to establish best practices
Despite growing recognition of its importance to a robust recovery-oriented system of care, increasing evidence of its effectiveness, and renewed efforts to establish best practices, recovery housing is still all too often viewed with skepticism by the lay media, addiction professionals, and substance use treatment researchers (Polcin, Mericle, Callahan, Harvey, & Jason, 2016). To facilitate replication of the Oxford House concept, the Oxford House model has been manualized (Oxford House Inc., 2015), and recovery residences calling themselves Oxford Houses must obtain a charter from and be in good standing with Oxford House, Inc. Further, the National Alliance for Recovery Residences (NARR) has developed standards and ethical guidelines for recovery housing (National Alliance for Recovery Residences, 2017a, 2017b) and has affiliates in 26 states across the US that inspect and certify that member recovery residences are operating to these standards. Yet, significant gaps in the literature remain due to insufficient empirical evidence on how various operational, programming, and organizational aspects of recovery housing affect resident outcomes; filling in these gaps could help establish best practices for operating recovery housing.
1.4. Aims and hypotheses
To begin to address these gaps in the literature, the aim of this study was to identify factors across organizational, operational, and program orientation domains associated with improved outcomes (e.g., abstinence, arrest, and employment) using multilevel modeling among residents recruited from 49 SLHs in Southern California and followed for a year post entry. While largely exploratory in nature, we had general expectations regarding how factors in these domains may be related to resident outcomes.
1.4.1. Organizational hypotheses.
Based on relevant organizational theory, we hypothesized that residents in houses that were part of a larger organization of group of houses, were affiliated with a treatment program, and had referral arrangements with probation/parole would have better outcomes, as these factors would reduce resource scarcity. Drawing from empirical findings regarding staffing and management practices, we hypothesized that residents who lived in houses where the manager lived onsite would have better outcomes. Although there is some evidence to suggest that having 8 or more residents in a house is beneficial to residents (Jason et al., 2008) as it likely increases social interactions among them, based on finding from the treatment literature, we hypothesized that residents living in houses with large numbers of residents would have worse outcomes.
1.4.2. Residence and operational hypotheses.
With respect to residence and operational characteristics, we anticipated that there may be differences by geographic location based on prior work finding significant clustering of SLHs and variation in density by neighborhood characteristics (Mericle, Karriker-Jaffe, Gupta, Sheridan, & Polcin, 2016). However, our measure of location (Sober Living Network Chapter) could reflect multiple neighborhoods, so we refrained from putting forth a priori hypotheses with respect to location. We hypothesized that residents living in houses with lower fees and that provided meals would have better outcomes as this would allow residents to accrue financial capital; sharing meals together might also contribute to creating a home-like atmosphere and facilitate social interactions and sense of community (De Leon, 2000; Ferrari, Jason, Sasser, Davis, & Olson, 2006). We hypothesized that greater resident homogeneity (i.e., more “peerness”) would be associated with improved outcomes, such that residents living in single-gender houses (men’s or women’s houses) would have better outcomes than those in co-ed houses. Further, because we were recruiting a criminal justice population, we hypothesized that residents in houses with a larger proportion of criminal justice involved residents would have better outcomes. Finally, we hypothesized that house rules pertaining to substance use and mutual aid involvement would also be associated with improved outcomes such that residents living in houses that required residents to have been sober 30 days prior to entry, that implemented drug tests at intake, and mandated that residents attend AA and/or NA would have better outcomes.
1.4.3. Program orientation hypotheses.
SLHs do not provide treatment services, so we were limited in what we could examine regarding programming. However, SLHs are social model programs which themselves are rooted in the of 12-step principles. We hypothesized that residents who lived in houses that scored higher on levels of adherence to the social model philosophy and that were more 12-step oriented would have better outcomes.
2. Methods
Data for this study were collected as part of a larger study testing the effectiveness of a brief motivational interviewing and case management intervention designed to help incoming SLH residents involved in the criminal justice system and at particularly high risk for HIV/AIDS resolve potential ambivalence about their recovery and engage in other community-based services (see Polcin et al., in press for a description of the intervention). All procedures involving human subjects were approved of and monitored by the Institutional Review Board of the Public Health Institute.
2.1. Sites and participants
This study was conducted in Los Angeles (LA) County between 2013 and 2017. LA County is an ideal location to study SLHs due to its large and diverse geographic and population characteristics as well as the large number of SLHs located in LA (Mericle et al., 2016). SLHs for this study were selected from those who were members of the Sober Living Network. The Sober Living Network is a nonprofit organization comprised of six county-level coalitions, and it oversees each coalition’s application, quality control, inspection, and membership certification procedures. Since the LA County Coalition grew to be so large, the members formed five chapters based upon geographic location of each SLH. The Sober Living Network is an affiliate of the NARR and implements housing standards used in recovery residences across the United States.
In addition to recruiting from only those SLHs that were members of the Sober Living Network, we also focused on those located in the Central, Western, and Harbor regions of LA County. We specifically targeted SLHs that reported large number of residents involved in the criminal justice system and those that charged less than $1500/month. Resident inclusion criteria comprised of current criminal justice involvement (i.e., probation, parole, drug court, etc.) and being HIV positive or having a lifetime history of at least one HIV risk behavior, broadly defined as men who had sex with men, commercial sex work, or injection drug use. Unprotected sex with two or more partners during the past six months qualified as an HIV risk as well. Residents who could not provide informed consent were excluded.
2.2. Recruitment and data collection procedures
Data for the present study come from a variety of sources: administrative data provided by the Sober Living Network on member houses, interviews with house managers/owners about their houses, and interviews with residents. SLHs meeting the above criteria based on information provided by the Sober Living Network were approached about serving as a potential recruitment site for the study. Project staff met with a representative of the house (either the house manager or the owner) to describe the nature of the study and to gather additional information about the characteristics and operations of the house. Houses taking part in the study were asked to sign a Letter of Agreement outlining their role as a recruitment site. To reduce contamination across conditions, randomization to the brief motivational interviewing and case management intervention condition was done at the house level. Participating houses received an annual stipend based on the number of residents recruited to participate in the study in that year.
Of the 396 houses that were members of the Sober Living Network during the study period, 59 were randomized and participants were recruited from 49 of these houses (28 houses assigned to the control condition and 21 houses assigned to the intervention condition). A total of 271 houses were determined to be ineligible, the most common reasons being that they dropped out of the Sober Living Network prior to potential participation (n=176) or charged monthly fees greater than $1500 (n=93). Forty-seven houses were approached but declined to participate or never returned calls about potential participation, leaving 19 left unapproached at the end of the recruitment phase. Houses that declined participation (actively or passively) were more likely to be single-gender houses (men’s or women’s houses as opposed to co-ed) and smaller than other eligible houses.
When a new resident entered one of the participating houses, they were provided a flyer about the study which included basic information about the study and ways to reach research interviewers. Research interviewers also maintained regular contact with house managers and were informed when new residents entered. Residents meeting eligibility criteria provided written informed consent, supplied detailed locating information to facilitate contact for follow-up interviews, and completed their baseline interview within one month after entering the house. Interviews were completed at the participant’s sober living home, the study office, or at mutually agreed upon public location where the interview could be conducted with privacy. Follow-up interviews were conducted 6 and 12 months post completion of the baseline interview, regardless of whether the resident was still at the house. A total of 56 interviews were completed in the LA County jail and 63 were completed over the phone because the participant moved out of the area. Interviews typically lasted 1–2 hours. Residents were given $30 for their time completing the baseline interview, $50 for completing the 6-month interview, and $50 for completing the 12-month follow-up interview. Residents who confirmed locating information were provided with an additional $5 at a 3-month check-in and $10 at a 9-month check-in.
During the study period, 916 residents were screened for potential participation and 379 met our inclusion/exclusion criteria. The primary reasons persons were screened out were lack of a criminal justice status (i.e. not on probation or parole; n=335), lack of lifetime HIV risk (n=133), or having been in the house longer than one month (n=69). Of the 379 who met the screening criteria, 330 were enrolled—6 of the eligible participants refused participation, 8 were unable to provide consent, and 35 consented but were no shows for their baseline interview. Of those who completed baseline interviews, 88% completed at least one-follow-up interview; 77% completed a 6-month follow-up interview and 81% completed their 12-month follow-up interview. There were no significant differences observed at baseline between the 40 participants who did not complete a follow-up and those who did complete follow-up interviews in terms of treatment condition, demographics, drug/alcohol use, arrests, employment, and house characteristics. The number of residents recruited within each house ranged from 1–24, with 20 of the 49 participating houses contributing 3 or fewer participants and 11 houses contributing the majority (52%) of the participants into the study.
2.3. Instruments and measures
2.3.1. House organizational, operational, and program orientation characteristics.
Data routinely tracked by the Sober Living Network and provided to the study included the gender of residents served by the house (men, women, co-ed), number of beds in the house (categorized into 0–10, 11–20, 21 or more), monthly fees charged, and chapter to which the house belonged (LA Metro, San Fernando Valley/San Gabriel Valley, South Bay Long Beach, West LA). To these data, we added whether a house was affiliated with a treatment program (as a step-down from a residential treatment program or otherwise affiliated with an outpatient treatment program) and whether the house was one of a group of houses run by a larger operator/organization.
Semi-structured interviews with house operators about serving as a recruitment site were audio-recorded, and we extracted from these interviews information on whether a house manger lived onsite at the house, whether the house had any sort of referral arrangements with parole/probation, the estimated percent of clients in the house that were on probation/parole at any given time (dichotomized at the median, indicating 15% or greater), and whether the house had rules requiring that residents attend AA/NA meetings. When additional houses were recruited from an organization with multiple houses and the operator indicated that sibling houses were similar to houses already participating in the study, we did not always conduct additional recruitment interviews to collect data on the sibling houses. Of the 49 houses participating in the study, recruitment interviews were only conducted for 43 of them, affecting 24 participants recruited from houses not interviewed. Houses that were missing recruitment interview data were all members of the Sober Living Network’s LA Metro or South Beach chapters and more likely to be affiliated with a treatment program (Fisher’s exact test, p=0.003) and smaller (10 or fewer beds; Fisher’s exact test, p=0.010).
To gather additional structured information about the houses, we later administered an augmented version of the Social Model Philosophy Scale (SMPS; Kaskutas et al., 1998), which was designed to measure the extent to which substance use programs adhere to a social model approach by assessing aspects of physical environment, staff roles, authority base, views on dealing with substance use problems, governance, and community orientation. The 33-item SMPS has been shown to have high internal reliability (α = 0.92), and test-retest analyses have shown high consistency across time, administrators, and respondents (Kaskutas et al. 1998). Items in this measure were summed according to criteria outlined in the scoring manual and converted to a percentage ranging from 0–100, with higher scores indicating greater adherence to the social model philosophy (Room & Kaskutas, 2008). To provide guidance to the field regarding critical levels of adherence to the social model, we created an indicator to reflect scores at the median or higher (≥ 63). We also asked whether residents were administered drug tests at intake, how many days residents needed to have been sober upon intake (used to create an indicator of 30 days or more), and the extent to which the house was run based on the 12-step principles (not at all, a little, somewhat, quite a bit, completely). Because these data were collected later in the study, some houses had closed or had otherwise completed their participation in the study, and these data were only collected on 39 of the 49 houses, affecting 25 participants recruited from houses not interviewed. Houses missing data from this interview were more likely to be affiliated with a larger group of houses (Fisher’s exact test, p=0.045) and members of the LA Metro or West LA chapters of the Sober Living Network (Fisher’s exact test, p=0.007).
2.3.2. Resident outcomes and characteristics.
Across a variety of studies, recovery housing has been found to be associated with improved substance use, criminal justice and employment outcomes (Jason et al., 2007; Reif et al., 2014), so we chose to focus on specifically on these. The Timeline Follow-Back (TLFB) was used to record the participants’ self-reported days of alcohol and drug use over the past 6 months (Sobell et al., 1996) at each interview. Because recovery housing is based on abstinence from both alcohol and illicit drug use (Jason et al., 2013), we created an indicator of total abstinence in the past 6 months. However, we also created separate indicators of past 6-month alcohol and drug abstinence, as drug use confers different consequences, particularly for those involved in the criminal justice system. Past 30-day data collected with Addiction Severity Index Lite (ASI; Cacciola, Alterman, McLellan, Lin, & Lynch, 2007; McLellan et al., 1992) regarding criminal justice involvement was augmented to assess whether the participant had any arrests in the past 6 months as well. We used an item from the California Drug and Alcohol Treatment Assessment study (Gerstein et al., 1994) assessing the number of days worked in the past 6 month to create an indicator of whether the participant was employed during that time.
To isolate the effects of housing characteristics, our models adjusted for resident demographic characteristics and length of stay. Demographic characteristics (gender, race/ethnicity, age, educational attainment) were collected at baseline with the ASI. We also collected data on the date the participants entered the house from which they were recruited and the date that they left to calculate length of stay and adjusted outcomes for the amount of exposure to the environment. Length of stay could be calculated for 285 residents and ranged from 1 to 452 days with the average being 149 days and the median being 101 days.
2.4. Statistical analyses
We used descriptive analytic techniques to present how frequently categories of responses were endorsed as well measures of central tendency and dispersion for continuous measures. Differences between groups at various time points were examined using Pearson’s chi-square, Fisher’s exact, and Student’s t-tests. Due to the exploratory nature of this study, separate multilevel/mixed effects models (Laird & Ware, 1982) were used to examine the effects of each house-level characteristic on changes in resident substance use, criminal justice, and employment outcomes over time. Multilevel/mixed effects models are particularly appropriate when data are nested or organized at more than one level (Gibbons, Hedeker, & DuToit, 2010; Raudenbush & Bryk, 2002). In these analyses, observations at various time points are nested within participants, and participants are nested within the houses from which they were recruited, representing a three-level model. All models were run in Stata v15 (StataCorp., 2017) as random intercept models. We examined intraclass correlation coefficients at each level and Likelihood Ratio statistics testing models with and without the random intercepts to confirm the appropriateness of the multilevel/mixed effects approach. All models examining the effects of house-level characteristics on outcomes included a term for time (categorical) and study condition and adjusted for gender, race/ethnicity, age, educational attainment, and length of stay. Coefficients from multilevel/mixed effects logistic models were expressed as odds ratios.
Missing data at the resident-level was generally minimal, however house managers from only 34 of the 49 houses participated in both the recruitment interview and the later interview to collect data on adherence to the social model approach. In the multilevel framework, missing data in higher levels is problematic because most statistical software packages discard complete records at the lower levels via listwise deletion, resulting in severe loss of information as well as potential bias (van Buuren, 2011). Listwise deletion yields unbiased estimates under the condition that data are missing completely at random, and it may yield valid inference in logistic models under broader assumptions and be more robust than other more sophisticated techniques to violations of assumptions that data are missing at random (Allison, 2001). However, even though simulations studies varying the amount of missing data in multilevel models have demonstrated that listwise deletion can produce estimates that do not differ from models without missing data (Gibson & Olejnik, 2003), this technique is generally not recommended (Grund, Lüdtke, & Robitzsch, 2018).
To check for potential bias in our findings, estimates of missing house-level characteristics were generated with multiple imputation techniques using house-level characteristics without missing data and merging these estimates (N=10) with the individual-level data so that cases missing house-level data could be retained (Gibson & Olejnik, 2003). Because this sort of “flat file” imputation ignores the multilevel structure of the data, we also conducted additional sensitivity analyses by running the models as two-level, random intercept-only latent growth models in Mplus Version 7.4 (Curran, Obeidat, & Losardo, 2010; Muthén & Asparouhov, 2011; Muthén & Muthén, 1998–2012), which implements a modeling approach to missing data whereby imputations for group-level data can be obtained from conditioning on observed group-level variables and individual-level variables (Asparouhov & Muthen, 2010; Grund et al., 2018). We similarly created 10 imputed datasets for each model using house characteristics without missing data, but also included individual level characteristics in the imputation models as well.
Finally, because examining the effects of house characteristics in separate models could increase Type 1 error rates, we also tested those that were found to be robustly related any outcomes (across imputation approaches) together in a single simultaneous multivariable multilevel models which adjusted for interview time period, condition, time-invariant resident characteristics, and length of stay.
3. Results
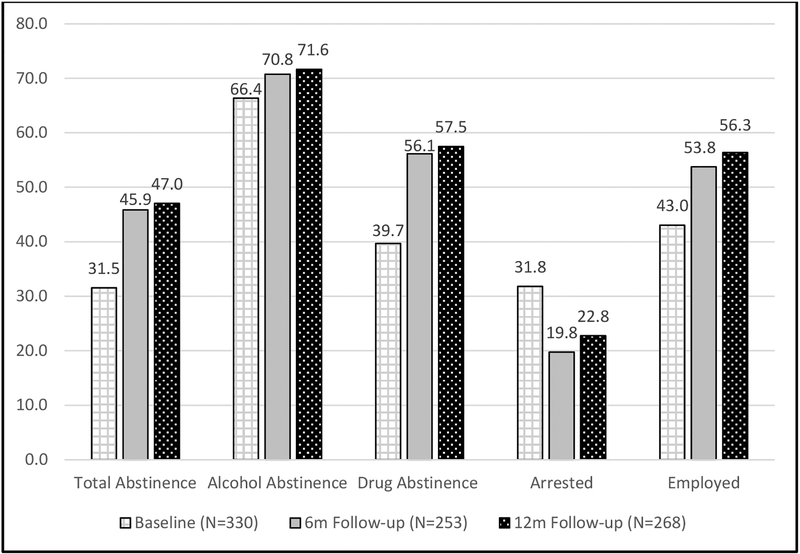
Baseline characteristics of residents recruited into the study can be found in Table 1, characteristics of the SLHs from which residents were recruited are listed in Table 2, and unadjusted prevalence of various outcomes at each interview time point are depicted in Figure 1. Results from multilevel models can be found in Tables 3.
Table 1.
Baseline Resident Demographic Characteristics by Condition (N=330)
| Total (N=330) | Control (N=181) | Intervention (N=149) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Men | 245 | 74.2 | 140 | 77.4 | 105 | 70.5 |
| Race/Ethnicity | ||||||
| Caucasian/White | 156 | 47.3 | 88 | 48.6 | 68 | 45.6 |
| Black/African American | 80 | 24.2 | 34 | 18.8 | 46 | 30.9 |
| Latino/Hispanic | 63 | 19.1 | 40 | 22.1 | 23 | 15.4 |
| Other/Mixed | 31 | 9.4 | 19 | 10.5 | 12 | 8.1 |
| College/Some College | 118 | 35.8 | 63 | 34.8 | 55 | 36.9 |
| Age (M, SD) | 38.7 | 11.7 | 38.0 | 11.9 | 39.5 | 11.5 |
NOTES. Of the 330 recruited at baseline, a total of 253 participants completed a 6-month follow-up interview and 268 participants completed a 12-month follow-up interview. A total of 290 participants (88%) recruited at baseline completed a 6-month or a 12-month follow-up interview; 231 (70%) completed both follow-ups. The 40 participants lost at follow-up did not vary at baseline on treatment condition, demographics, drug/alcohol use, arrests, employment, or house characteristics from those who completed 1 or more follow-up interviews. There were no demographic differences (e.g., gender, race/ethnicity, education, age) by treatment group among those who completed follow-up interviews.
Table 2.
SLH Characteristics (N=49)
| Total (N=49) | Control (N=28) | Inter-vention (N=21) | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Organizational Characteristics | |||||||
| Part of a Larger Organization1 | 36 | 73.5 | 23 | 82.1 | 13 | 61.9 | |
| Affiliated with a Treatment Program1 | 13 | 26.5 | 11 | 39.3 | 2 | 9.5 | * |
| Referral Arrangement with Parole/Probation (N=42)2 | 20 | 47.6 | 12 | 52.2 | 8 | 42.1 | |
| House Manger Lives Onsite (N=43)2 | 32 | 74.4 | 20 | 83.3 | 12 | 63.2 | |
| Capacity (Number of beds; 7–50)1 | |||||||
| 0–10 beds | 10 | 20.4 | 6 | 21.4 | 4 | 19.1 | |
| 11–20 beds | 23 | 46.9 | 12 | 42.9 | 11 | 52.4 | |
| 21 or more | 16 | 32.7 | 10 | 35.7 | 35.7 | 28.6 | |
| Residence & Operational Characteristics | |||||||
| SLN Chapter1 | * | ||||||
| LA Metro | 14 | 28.6 | 3 | 10.7 | 11 | 52.4 | |
| San Fernando Valley/San Gabriel Valley | 7 | 14.3 | 6 | 21.4 | 1 | 4.8 | |
| South Bay/Long Beach | 18 | 36.7 | 12 | 42.9 | 6 | 28.6 | |
| West LA | 9 | 18.4 | 6 | 21.4 | 3 | 14.3 | |
| Monthly Fees Charged ($375–1500)1 | ** | ||||||
| $0–599 | 23 | 46.9 | 6 | 21.4 | 17 | 81.0 | |
| $600+ | 26 | 53.1 | 22 | 78.6 | 4 | 19.1 | |
| Meals Provided (N=43)2 | 13 | 30.2 | 6 | 25.0 | 7 | 36.8 | |
| House Gender1 | |||||||
| Co-ed | 15 | 30.6 | 9 | 32.1 | 6 | 28.6 | |
| Women | 9 | 18.4 | 3 | 10.7 | 6 | 28.6 | |
| Men | 25 | 51.0 | 16 | 57.1 | 9 | 42.9 | |
| % Residents on Parole/Probation (N=37; 0–100; M, SD)2 | 32.4 | 32.7 | 37.9 | 35.8 | 27.1 | 29.5 | |
| Required Days Sober (N=39; 0–730; M, SD)3 | 40.9 | 116.9 | 49.4 | 154.3 | 29.8 | 31.4 | |
| Drug Testing at Intake (N=39)3 | 30 | 76.9 | 16 | 72.7 | 14 | 82.4 | |
| Mandated AA/NA Attendance (N=43)2 | 33 | 76.7 | 17 | 70.8 | 16 | 84.2 | |
| Program Orientation | |||||||
| SMPS Total Score (N=39; 48–75; M, SD)3 | 61.0 | 7.4 | 61.3 | 7.2 | 60.6 | 7.9 | |
| 12-step Orientation (N=39)3 | |||||||
| Not at all | 2 | 5.1 | 2 | 9.1 | 0 | 0.0 | |
| A little | 4 | 10.3 | 1 | 4.6 | 3 | 17.7 | |
| Somewhat | 6 | 15.4 | 2 | 9.1 | 4 | 23.5 | |
| Quite a bit | 13 | 33.3 | 9 | 40.9 | 4 | 23.5 | |
| Completely | 14 | 35.9 | 8 | 36.4 | 6 | 35.3 | |
Notes. Valid summary statistics presented with data source and sample size noted. Differences by study condition were tested with chi-square, Fisher’s Exact, and Student’s t tests.
p<0.05;
p<0.01.
Data were obtained from the Sober Living Network and available for all houses.
House manager interviews were conducted for 43 houses; due to the semi-structured nature of the interview, not all questions were asked of those who participated.
Data collected with the augmented SMPS were only collected on 39 houses.
Figure 1.
Unadjusted 6-month Prevalence of Various Outcomes by Interview
Table 3.
Multilevel Models Examining the Relationship Between House Characteristics and Resident Outcomes
| Total Abstinence | Alcohol Abstinence | Drug Abstinence | Arrested | Employed | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| aOR | SE | p | aOR | SE | p | aOR | SE | p | aOR | SE | p | aOR | SE | p | |
| Organizational Characteristics | |||||||||||||||
| Part of a Larger Organization | 3.98 | 1.46 | 0.000† | 3.04 | 1.22 | 0.006 | 3.19 | 1.02 | 0.000† | 0.59 | 0.19 | 0.109 | 1.11 | 0.43 | 0.790 |
| Affiliated with a Treatment Program | 2.56 | 1.20 | 0.045 | 1.98 | 0.94 | 0.149 | 1.83 | 0.78 | 0.151 | 0.87 | 0.30 | 0.675 | 2.92 | 1.06 | 0.003† |
| Referral agreement with Parole/Probation | 1.52 | 0.62 | 0.304 | 1.13 | 0.51 | 0.786 | 1.62 | 0.58 | 0.180 | 0.55 | 0.15 | 0.025 | 2.43 | 0.78 | 0.006 |
| Manager Lives Onsite* | 0.94 | 0.57 | 0.913 | 1.21 | 0.78 | 0.770 | 0.63 | 0.34 | 0.387 | 1.85 | 0.77 | 0.142 | 1.70 | 0.86 | 0.297 |
| Capacity (Number of beds; 7–50) | |||||||||||||||
| 0–10 (reference) | |||||||||||||||
| 11–20 | 0.63 | 0.40 | 0.469 | 0.76 | 0.50 | 0.677 | 0.64 | 0.37 | 0.441 | 0.56 | 0.25 | 0.193 | 0.60 | 0.31 | 0.329 |
| 21 or more | 0.50 | 0.32 | 0.275 | 0.45 | 0.30 | 0.236 | 0.79 | 0.47 | 0.695 | 0.89 | 0.39 | 0.796 | 0.33 | 0.18 | 0.039 |
| Wald Test of Capacity | 0.547 | 0.388 | 0.716 | 0.253 | 0.086 | ||||||||||
| Residence & Operational Characteristics | |||||||||||||||
| SLN Chapter | |||||||||||||||
| LA Metro (Reference) | |||||||||||||||
| San Fernando Valley/San Gabriel Valley | 1.55 | 1.05 | 0.521 | 4.39 | 2.39 | 0.006† | 2.23 | 1.33 | 0.182 | 0.84 | 0.42 | 0.722 | 1.95 | 1.05 | 0.213 |
| South Bay Long Beach | 1.10 | 0.57 | 0.858 | 1.09 | 0.43 | 0.829 | 0.93 | 0.43 | 0.871 | 0.80 | 0.33 | 0.579 | 1.89 | 0.80 | 0.133 |
| West LA | 2.26 | 1.50 | 0.221 | 8.54 | 5.04 | 0.000† | 1.60 | 0.97 | 0.434 | 1.08 | 0.55 | 0.883 | 5.04 | 2.75 | 0.003 |
| Wald Test of SLN Chapter | 0.585 | 0.000† | 0.359 | 0.878 | 0.032† | ||||||||||
| Monthly Fees of $600 or More | 2.63 | 1.49 | 0.088 | 3.18 | 1.76 | 0.036 | 2.65 | 1.34 | 0.053 | 2.09 | 0.82 | 0.063 | 1.96 | 0.95 | 0.165 |
| Meals Provided* | 1.76 | 0.73 | 0.171 | 1.84 | 0.78 | 0.151 | 1.74 | 0.66 | 0.147 | 1.10 | 0.33 | 0.739 | 0.75 | 0.27 | 0.415 |
| House Gender | |||||||||||||||
| Co-ed (Reference) | |||||||||||||||
| Women | 1.83 | 1.29 | 0.395 | 1.67 | 1.20 | 0.480 | 1.87 | 1.21 | 0.333 | 1.72 | 0.94 | 0.325 | 2.54 | 1.58 | 0.134 |
| Men | 2.34 | 1.19 | 0.095 | 2.90 | 1.42 | 0.031 | 2.05 | 0.94 | 0.114 | 1.33 | 0.49 | 0.440 | 1.44 | 0.62 | 0.392 |
| Wald Test of Gender | 0.219 | 0.090 | 0.231 | 0.525 | 0.278 | ||||||||||
| 15%+ of Residents on Parole/Probation* | 0.23 | 0.11 | 0.002 | 0.49 | 0.26 | 0.177 | 0.46 | 0.18 | 0.044 | 1.71 | 0.57 | 0.108 | 1.11 | 0.46 | 0.809 |
| 30+ Required Days Sober* | 1.47 | 0.72 | 0.432 | 0.93 | 0.45 | 0.875 | 1.05 | 0.45 | 0.913 | 0.43 | 0.12 | 0.003† | 1.36 | 0.55 | 0.443 |
| Drug Testing at Intake* | 1.00 | 0.60 | 0.997 | 2.23 | 1.37 | 0.192 | 1.00 | 0.51 | 0.992 | 0.92 | 0.35 | 0.837 | 2.52 | 1.20 | 0.052 |
| Mandated AA/NA Attendance* | 2.74 | 1.40 | 0.048 | 3.59 | 1.86 | 0.014 | 2.41 | 1.10 | 0.055 | 2.11 | 0.78 | 0.042 | 1.39 | 0.63 | 0.460 |
| Program Orientation | |||||||||||||||
| SMPS Total Score ≥ 63* | 1.07 | 0.53 | 0.892 | 0.72 | 0.34 | 0.488 | 1.29 | 0.57 | 0.560 | 0.86 | 0.28 | 0.646 | 0.98 | 0.39 | 0.964 |
| Quite a bit/Completely 12-step Oriented* | 2.95 | 1.50 | 0.034 | 2.67 | 1.32 | 0.047 | 2.09 | 0.94 | 0.102 | 0.54 | 0.17 | 0.052 | 2.31 | 0.96 | 0.043 |
Notes. Results from separate multilevel models testing the effect of various housing characteristics on substance use, criminal justice, and employment outcomes parameterize clustering of observations within participants and participants within houses (ICCs ranging from 0.008–0.137). All random intercept models control for time, condition, their interaction, gender, race/ethnicity, age, educational attainment, and number of days in the house. Individual ORs, SEs, and p-values are listed for each category of categorical variables as well as the p-value for Wald test of the overall effect of the categorical variable.
Denotes models with missing data on house characteristics that were subjected to sensitivity analyses employing different multiple imputation techniques. Findings in bold typeface reflect those that were robust across these different techniques.
Reflects findings that remained statistically significant in multivariable multilevel models.
3.1. Resident characteristics
As Table 1 displays, the average age of respondents was 39, and the majority of the sample were men (75%). Close to half of the sample (47%) was Caucasian/White, and a little over a third (36%) had at least some college education. No differences were found on these characteristics between residents recruited from houses assigned to the intervention condition.
3.2. Residence characteristics
Table 2 displays characteristics of the SLHs by treatment condition. As this table shows, the majority of houses (74%) were part of a larger group of houses owned/operated by the same entity. Slightly more than a quarter (27%) of houses were affiliated with a treatment program. The majority of the houses had 11 or more beds; nearly a third had 21 or more beds. We primarily recruited houses belonging to one of four Sober Living Network chapters, the largest percentage (37%) belonging to the South Bay/Long Beach Chapter. As mentioned earlier, we specifically recruited houses charging fees less than $1500/month, but 47% charged less than $600/month. While most houses were single-gender (with men’s houses accounting for 51% of the sampled houses), 31% of the houses were co-ed. Houses in the intervention condition were more likely to charge less than $600/month and be a member of the LA Metro SLN Chapter but less likely to be affiliated with a treatment program.
Table 2 also displays houses characteristics collected from the house managers. Among houses with these data, nearly half (48%) had some sort of referral arrangements with parole/probation, with an average of 32% of residents estimated to be on parole/probation. The majority of houses (74%) had a manager who lived on site, but less than a third (30%) provided residents with meals. The majority also mandated that residents attend AA/NA meetings (77%) and reported drug testing residents upon intake (77%); the average number of days required to be sober upon entry was 41 (SD=117). Scores on the Social Model Philosophy scale ranged from 48–75. Although the average score was lower than what has been identified as the cut-point for true social model programs (e.g., >=75; Kaskutas et al., 1998; Kaskutas et al., 1999), the majority (69%) were characterized by house managers as being operated quite a bit or completely based on a 12-step orientation. No differences were found between houses assigned to the intervention condition on these characteristics.
3.3. Outcome prevalence by interview time point
Figure 1 displays unadjusted prevalence of various 6-month substance use, arrest, and employment outcomes by interview time point. In general, from one interview to the next, rates of abstinence increase, rates of arrests decrease, and employment rates increase. As mentioned earlier, we found no evidence to suggest differential attrition by characteristics measured at baseline or by treatment condition. Among those completing interviews at each time point, there were no demographic differences by treatment condition, and the only difference in outcomes found by condition pertained to arrests among those participating in the 6-month interview. Significantly fewer of those in the intervention condition compared to those in the control condition reported any arrests in the prior 6 months (12% vs. 25%, p<0.01).
3.4. Findings from separate multilevel models
Results from multilevel models testing the effects of various organizational, residence/operational, and programming characteristics adjusting for demographics, length of stay, treatment condition, and time are presented in Table 3.
3.4.1. Organizational characteristics.
Being recruited from a house that was part of an organization or a larger group of houses was associated with increased odds of total abstinence (aOR=3.98, p<0.001), alcohol abstinence (aOR=3.04, p=0.006), and drug abstinence (aOR=3.19, p<0.001); being recruited from a house that was affiliated with a treatment program was associated with increased odds of total abstinence (aOR=2.56, p=0.045) and being employed (aOR=2.92, p=0.003). Referral agreements with parole probation were associated with decreased odds of arrest (aOR=0.55, p=0.025) and increased odds of employment (aOR=2.43, p=0.006). While capacity of 21 or residents was associated with decreased odds of employment (aOR=0.33, p=0.039) relative to houses with 10 or fewer residents, the overall effect of residence capacity was only marginally associated with employment outcomes.
3.4.2. Residence and operational characteristics.
Alcohol abstinence outcomes varied significantly by Sober Living Network chapter, and so did employment outcomes. Relative to being recruited from a house belonging to the LA Metro Chapter, being recruited from a house belonging to the San Fernando Valley/San Gabriel Valley Chapter was associated with increased odds of alcohol abstinence (aOR=4.39, p=0.006), as was being recruited from a house belonging to the West LA Chapter (aOR=8.54, p<0.001). Being recruited from a house belonging to the West LA Chapter was also associated with increased odds of employment (aOR=5.04, p=0.003). Factors pertaining to the type of residents that houses served were associated with increased odds of alcohol abstinence, specifically being recruited from houses that charges monthly fees greater than $600 (aOR=3.18, p=0.036) and being recruited from men’s houses (aOR=2.90, p=0.031) relative to co-ed houses. There was also indication that, as the estimated percentage of residents on parole/probation increased, the odds of abstinence decreased and the odds of arrest increased. House rules and policies were also found to be associated with outcomes. Being recruited from a house that required prospective residents to have 30 or more days of sobriety was associated with decreased odds of arrest (aOR=0.43, p=0.003). While drug testing at intake was not associated with outcomes, there was an indication that mandated AA/NA attendance was associated with increased odds of both total and alcohol abstinence as well as arrests.
3.4.3. Program orientation.
SMPS scores were not associated with outcomes. However, there was some indication that houses being more (quite a bit or completely) 12-step oriented was associated with increased odds of total and alcohol abstinence as well as increased odds of employment.
3.5. Missing data sensitivity analyses
To ensure that estimates from models that implemented listwise deletion when house-level data was missing were bias-free, we reran the models with imputed data generated from non-missing house-level data. To reflect the potential effect of resident characteristics on the imputations, we also created imputed datasets in Mplus and reanalyzed the data as multilevel, random intercept-only latent growth models. Variables with missing house-level data are denoted with an asterisk (*) in Table 3. Effects that were consistently significant across these analyses are reflected in the table with boldface font. It is important to note that we also reran models without missing house-level data in Mplus to examine potential changes that might be due to analytic approach. While some variation might be expected, results from the three-level random intercept models and the multilevel growth models were largely the same when analyzing the effect of house characteristics without missing data. In general, estimates from models with imputed data were similar in magnitude and direction, but standard errors increased resulting in fewer findings reaching statistical significance. In fact, the only finding that was robust across imputation models was the finding regarding rules requiring residents to be sober a minimum of 30 days prior to entry.
3.6. Multivariable multilevel findings
House characteristics that were robustly associated with outcomes in separate models (across analytic approach and imputation techniques) were run in multivariable multilevel models. Results from these models are also denoted (†) in Table 3. Some findings that were significantly associated with outcomes in separate models were no longer statistically significant in multivariable models; these were findings that generally would have been considered non-significant had we implemented Bonferroni-type adjustments in the separate models. However, using that approach would have masked the effect of Sober Living Network chapter on employment.
4. Discussion
Despite growing evidence for their effectiveness and manuals and standards guiding operations based on a wealth of experience operating recovery housing, there is still little empirical evidence to guide the field and other stakeholders (including prospective residents and their loved ones) regarding best practices for recovery housing. We found evidence that points to salience of organizational and some operational factors as well.
4.1. Organizational characteristics
Because recovery housing is rooted in the traditions of mutual aid (National Association for Recovery Residences, 2012), it may seem counter-intuitive to apply organizational and other management theories to the understanding of it. However, all Oxford Houses have charters from Oxford House, Inc which currently consists of 2,287 chartered houses in 44 states (Oxford House Inc., 2018). And while most recovery housing operators would be dwarfed in scale in comparison, it is not uncommon for operators to have multiple houses (Mericle et al., 2015). Even operators with just one house must balance revenue and expenses and make decisions about how to maintain the residence and address resident recovery needs. Further, although experiential knowledge is central to recovery housing models and some models are democratically-run (National Association for Recovery Residences, 2012), all recovery housing must be managed in some way, and questions about the background and training of those managing houses and how this is done are still germane. In fact, this may become increasing relevant as roles and requirements for peers providing recovery support services continue to expand and evolve (Salzer, Schwenk, & Brusilovskiy, 2010; White, 2010).
In this study, hypotheses regarding organization characteristics were largely confirmed, particularly with respect to organizations with multiple houses and relationships with treatment programs being associated with improved outcomes. It is important to note that although we did our best to limit the number of houses that were recruited into study belonging to the same organization, as this could potentially create another level of clustering, we sometimes did have multiple houses from the same organization. To ensure that these houses did not artificially restrict house-level variance, we ran post-hoc sensitivity analyses specifying robust estimation of variance at the house-level. While these analyses did sometimes cause some attenuation in the level of significance (e.g., changing from p<0.01 to p<0.05), they did not meaningfully change the overall findings. This observed heterogeneity could reflect operators’ attempts to use different houses to address different populations, or it may simply reflect how different physical structures and location factors may influence recovery housing characteristics even when houses are operated by the same organization.
Findings pertaining to staffing and house capacity were less clear, but there was some indication that larger capacity may be inversely related to positive employment outcomes. However, this may reflect larger houses being able to charge lower monthly fees, thereby decreasing the necessity of residents to work. These findings, as well as those which were stronger, require more detailed analyses, as the relationships between these characteristics and outcomes are likely quite nuanced and related to a number of other factors. For example, a resident’s experience of house capacity is likely not only influenced by things such as resident-to-staff ratio, but also by overall square footage and space configuration.
The factors behind and the effects of organizational integration, expansion, and linkages also require additional study. It is possible that having multiple houses improves outcomes through increased quality because it forces operators to codify and standardize procedures; it may also allow them to better match residents to environments that might be optimally conductive to recovery. Alternately, it may reflect economies of scale where cost savings can be reinvested into house improvements as well as more or better-trained managers. Further, it is unclear whether having an affiliation with a treatment program simply helps reduce resource scarcity by ensuring referrals to the residence, or whether it does indeed translate into better addressing emergent needs of residents. It may also induce operators to more clearly define the service they provide and operate more similarly to the organizations with whom they are affiliated. This would may be particularly important to study further with respect to linkages with organizations in different service delivery sectors (e.g., criminal justice and mental health) that may operate under different guidelines and mandates.
4.2. Residence, operational, and program orientation factors
SLHs, like most other models of recovery housing, do not provide treatment, so decisions about where they are located, how environments in the house are structured, who they serve, expectations for residents, and their overall orientation to recovery constitute the service provided, as all these characteristics contribute to the therapeutic nature of the residence. Although we did not find strong evidence supporting program orientation, we did find differences by the geographic region, as indicated by Sober Living Network chapter membership. Although we cannot rule out that there might be something about these chapters contributing to outcomes other than their geographic purview, community-level factors are notably related to substance use and relapse (Boardman, Finch, Ellison, Williams, & Jackson, 2001; Karriker-Jaffe, Au, Frendo, & Mericle, 2017), and it likely that community resources, like proximity to 12-step meetings and other services, could also have a positive influence on recovery outcomes (Jacobson, 2004). Additional research more specifically analyzing these factors is needed.
In terms of other operational factors, requiring that prospective residents be sober for at least 30 days prior to entry was consistently associated with decreased odds of arrest. The relationships between other operational factors and outcomes were less consistent, but it is important to note some important limitations with respect to measuring these characteristics. First, information about many of these factors were collected within the context of a semi-structured interview conducted to determine suitability of houses as recruitment sites rather than to systematically gather data on housing characteristics per se. This has implications for the quality of the data collected and for the type of data collected, as a number of potentially important contributors to the nature house environment, like architectural features (Wittman, Jee, Polcin, & Henderson, 2014), were not assessed during this interview. In an attempt to gather information more systematically about the nature of the environment, an augmented version of the SMPS was administered toward the end of the study. By that time, however, many of the participating houses had closed or were not interested in completing this interview, again compromising the quality of the data collected. Further, despite contributions of measures developed to assess the characteristics of Oxford Houses (Ferrari, Groh, & Jason, 2009; Ferrari, Jason, Davis, Olson, & Alvarez, 2004; Ferrari et al., 2006), substance use treatment programs more generally (Carise, McLellan, & Gifford, 2000; D’Aunno & Price, 2009; Institute of Behavioral Research, 2006), and those based on them (Mericle et al., 2015; Mericle et al., 2017; Miles et al., 2017), the field is lacking a comprehensive assessment tool to adequately capture characteristics of recovery residences across organizational, operational, and programmatic domains which would be needed to more rigorously study recovery housing and how these factors may affect resident outcomes.
4.3. Limitations and directions for research
In addition to aforementioned measurement and missing data issues, other study limitations should also be noted. The generalizability of these findings may be limited because this study focused on SLHs (one type of recovery housing) in southern California (one geographic region). Further, the study did not draw a random sample of these houses, and many houses meeting study eligibility criteria declined participation. Finally, the study recruited only those residents involved in the criminal justice system at high risk for HIV/AIDS and may best generalize to this subpopulation. Despite these limitations, this study is the first to examine a range of recovery residence characteristics in relationship to resident outcomes.
It should also be noted that this work is currently being expanded to focus more specifically on how neighborhood characteristics and resources, architectural features, and the social environment within the SLHs affect resident outcomes in a more diverse sample of SLHs. Future studies are also needed that include a broader range of outcomes, like income from employment and gains health and wellbeing, to better understand how recovery housing can be leveraged to maximize outcomes across of variety of domains. It should also be expanded to examine how these factors may influence outcomes in other types of recovery housing (such as those that provide recovery support and other clinical services) and other housing models, such as Housing First models (Tsemberis, Gulcur, & Nakae, 2004; Watson, Wagner, & Rivers, 2013).
4.4. Conclusions
Recovery housing helps contribute to improved outcomes, but we lack an evidence base on which and how residence characteristics contribute to these outcomes. Drawing from organizational theory and findings from studies examining organizational and management factors in the delivery of substance use treatment, this study used a multilevel analytic framework to explore the effects of organizational, operational, and program orientation on substance use, employment, and criminal justice outcomes among residents recruited from SLHs in California. Findings regarding the salience of being part of larger group of houses and being affiliated with a treatment program, as well as findings regarding differences by geographic location invite future research to investigate what these factors represent and precisely how they may affect recovery outcomes. This work would be facilitated with a comprehensive recovery housing assessment tool to monitor and study recovery housing similar to those developed for substance use treatment programs as well as specific measures characterizing the therapeutic nature of the environment.
Disclosures and acknowledgements
Work on this manuscript was funded by the National Institute on Drug Abuse (R01DA034973; R01DA042938). The funding agencies had no role in study design; in the collection, analysis, or interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIDA or the National Institutes of Health. In addition to our funders, the authors would like to thank the Sober Living Network for their support of the study as well as Dave Sheridan of the National Alliance for Recovery Residences for his comments on early drafts of this manuscript.
Contributor Information
Amy A. Mericle, Alcohol Research Group at the Public Health Institute, Emeryville, CA 94608, USA.
Elizabeth Mahoney, Alcohol Research Group at the Public Health Institute, Emeryville, CA 94608, USA.
Rachael Korcha, Alcohol Research Group at the Public Health Institute, Emeryville, CA 94608, USA.
Kevin Delucchi, University of California San Francisco, San Francisco, CA 94143, USA.
Douglas L. Polcin, Alcohol Research Group at the Public Health Institute, Emeryville, CA 94608, USA.
References
- Allison PD (2001). Missing Data. Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- American Society of Addiction Medicine. (2018). Public Policy Statement on the Role of Recovery in Addiction Care. Rockville, MD. [Google Scholar]
- Asparouhov T, & Muthen B (2010). Multiple Imputation with Mplus [accessed online 6/26/18 https://www.statmodel.com/download/Imputations7.pdf] (pp. 25).
- Boardman JD, Finch BK, Ellison CG, Williams DR, & Jackson JS (2001). Neighborhood disadvantage, stress, and drug use among adults. Journal of Health and Social Behavior, 42(2), 151–165. [PubMed] [Google Scholar]
- Borkman T (1999). Understanding Self-help/Mutual Aid: Experiential learning in the commons. New Brunswick, NJ: Rutgers University Press. [Google Scholar]
- Borkman TJ, Kaskutas LA, Room J, Bryan K, & Barrows D (1998). An historical and developmental analysis of social model programs. Journal of Substance Abuse Treatment, 15(1), 7–17. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, McLellan AT, Lin Y-T, & Lynch KG (2007). Initial evidence for the reliability and validity of a “Lite” version of the Addiction Severity Index. Drug and Alcohol Dependence, 87(2–3), 297–302. [DOI] [PubMed] [Google Scholar]
- Carise D, McLellan AT, & Gifford LS (2000). Development of a “treatment program” descriptor: the Addiction Treatment Inventory. Substance Use and Misuse, 35(12–14), 1797–1818. [DOI] [PubMed] [Google Scholar]
- Cloud W, & Granfield R (2008). Conceptualizing recovery capital: expansion of a theoretical construct. Substance Use and Misuse, 43(12–13), 1971–1986. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Obeidat K, & Losardo D (2010). Twelve frequently asked questions about growth curve modeling. Journal of Cognition and Development, 11(2), 121–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Aunno T (2006). The role of organization and management in substance abuse treatment: review and roadmap. Journal of Substance Abuse Treatment, 31(3), 221–233. [DOI] [PubMed] [Google Scholar]
- D’Aunno T, & Price R (2009). National Drug Abuse Treatment System Survey, Waves II-IV. ICPSR 4146 [Accessed: 2016-05-27 Archived by WebCite® at http://www.webcitation.org/6hp4NHX5h]. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]. [Google Scholar]
- De Leon G (2000). The Therapeutic Community: Theory, model, and method. New York: Springer Publishing Company. [Google Scholar]
- Dennis ML, & Scott CK (2007). Managing addiction as a chronic condition. Addiction Science and Clinical Practice, 4(1), 45–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy P, & Baldwin H (2013). Recovery post treatment: plans, barriers and motivators. Substance Abuse Treatment, Prevention, and Policy, 8, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyrich-Garg KM, Cacciola JS, Carise D, Lynch KG, & McLellan AT (2008). Individual characteristics of the literally homeless, marginally housed, and impoverished in a US substance abuse treatment-seeking sample. Social Psychiatry and Psychiatric Epidemiology, 43(10), 831–842. [DOI] [PubMed] [Google Scholar]
- Ferrari JR, Groh DR, & Jason LA (2009). The neighborhood environments of mutual-help recovery houses: comparisons by perceived socio-economic status. Journal of Groups in Addiction and Recovery, 4(1–2), 100–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari JR, Jason LA, Davis MI, Olson BD, & Alvarez J (2004). Similarities and differences in governance among residents in drug and/or alcohol misuse recovery: self vs. staff rules and regulations. Therapeutic Communities, 25(3), 185–198. [Google Scholar]
- Ferrari JR, Jason LA, Olson BD, Davis MI, & Alvarez J (2002). Sense of community among Oxford House residents recovering from substance abuse: Making a house a home In Fischer A (Ed.), Psychological Sense of Community. New York, NY: Kluger/Plenum Inc. [Google Scholar]
- Ferrari JR, Jason LA, Sasser KC, Davis MI, & Olson BD (2006). Creating a home to promote recovery: the physical environments of Oxford House. Journal of Prevention and Intervention in the Community, 31(1–2), 27–39. [DOI] [PubMed] [Google Scholar]
- Gerstein DR, Johnson RA, Foote M, Suter N, Jack K, Merker G, … Fountain D (1994). Evaluating Recovery Services: The California Drug and Alcohol Treatment Assessment (CALDATA): Methodology Report. Sacramento, CA: State of California Department of Alcohol and Drug Programs. [Google Scholar]
- Ghose T (2008). Organizational and individual-level correlates of post-treatment substance use: A multilevel analysis. Journal of Substance Abuse Treatment, 34(2), 249–262. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Hedeker D, & DuToit S (2010). Advances in analysis of longitudinal data. Annual Review of Clinical Psychology, 6, 79–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson NM, & Olejnik S (2003). Treatment of missing data at the second level of hierarchical linear models. Educational and Psychological Measurement, 63(2), 204–238. [Google Scholar]
- Granfield R, & Cloud W (1999). Coming Clean: Overcoming addiction without treatment. New York: New York University Press. [Google Scholar]
- Grella CE, & Stein JA (2006). Impact of program services on treatment outcomes of patients with comorbid mental and substance use disorders. Psychiatric Services, 57(7), 1007–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grund S, Lüdtke O, & Robitzsch A (2018). Multiple imputation of missing data for multilevel models: simulations and recommendations. Organizational Research Methods, 21(1), 111–149. [Google Scholar]
- Hasenfeld Y (2010). Human Services as Complex Organizations, 2nd edition (2nd ed.). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Heslin KC, Singzon TK, Farmer M, Dobalian A, Tsoa J, & Hamilton AB (2013). Therapy or threat? Inadvertent exposure to alcohol and illicit drug cues in the neighbourhoods of sober living homes. Health & Social Care in the Community, 21(5), 500–508. [DOI] [PubMed] [Google Scholar]
- Hillman AJ, Withers MC, & Collins BJ (2009). Resource dependence theory: A review. Journal of Management, 35(6), 1404–1427. [Google Scholar]
- Hser Y-I, Joshi V, Maglione M, Chou C-P, & Anglin MD (2001). Effects of program and patient characteristics on retention of drug treatment patients. Evaluation and Program Planning, 24(4), 331–341. [Google Scholar]
- Institute of Behavioral Research. (2006). TCU Survey of Structure and Operations (TCU SSO) [Accessed: 2016-05-27 Archived by WebCite® at http://www.webcitation.org/6hp61rhhl]. Fort Worth, TX: Texas Christian University, Institute of Behavioral Research. [Google Scholar]
- Jacobson JO (2004). Place and attrition from substance abuse treatment. Journal of Drug Issues, 34(1), 23–50. [Google Scholar]
- Jason LA, Davis MI, Ferrari JR, Anderson E (2007). The need for substance abuse after-care: Longitudinal analysis of Oxford House. Addictive Behaviors, 32, 803–818. [DOI] [PubMed] [Google Scholar]
- Jason LA, Groh DR, Durocher M, Alvarez J, Aase DM, & Ferrari JR (2008). Counteracting “Not in My Backyard”: the positive effects of greater occupancy within mutual-help recovery homes. Journal of Community Psychology, 36(7), 947–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Light JM, Stevens EB, & Beers K (2014). Dynamic social networks in recovery homes. American Journal of Community Psychology, 53(3–4), 324–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Luna RD, Alvarez J, & Stevens E (2016). Collectivism and individualism in Latino recovery homes [Published online April 26: https://www.tandfonline.com/doi/abs/10.1080/15332640.2016.1138267?journalCode=wesa20 Journal of Ethnicity in Substance Abuse. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Mericle AA, Polcin DL, & White WL (2013). The role of recovery residences in promoting long-term addiction recovery. American Journal of Community Psychology, 52(3–4), 406–411. [DOI] [PubMed] [Google Scholar]
- Jason LA, Stevens E, & Light JM (2016). The relationship of sense of community and trust to hope. Journal of Community Psychology, 44(3), 334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe KJ, Au V, Frendo M, & Mericle AA (2017). Offsetting the effects of neighborhood disadvantage on problem drinking. Journal of Community Psychology, 45(5), 678–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Greenfield TK, Borkman TJ, & Room JA (1998). Measuring treatment philosophy: a scale for substance abuse recovery programs. Journal of Substance Abuse Treatment, 15(1), 27–36. [DOI] [PubMed] [Google Scholar]
- Laird NM, & Ware JH (1982). Random effects models for longitudinal data. Biometrics, 38(4), 963–974. [PubMed] [Google Scholar]
- Laudet AB, Stanick V, & Sands B (2009). What could the program have done differently? A qualitative examination of reasons for leaving outpatient treatment. Journal of Substance Abuse Treatment, 37(2), 182–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, & White W (2010). What are your priorities right now? Identifying service needs across recovery stages to inform service development. Journal of Substance Abuse Treatment, 38(1), 51–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majer JM, Jason LA, Aase DM, Droege JR, & Ferrari JR (2013). Categorical 12-Step involvement and continuous abstinence at two-years. Journal of Substance Abuse Treatment, 44(1), 46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, … Argeriou M (1992). The Fifth Edition of the Addiction Severity Index. Journal of Substance Abuse Treatment, 9(3), 199–213. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, & Kleber HD (2000). Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA, 284(13), 1689–1695. [DOI] [PubMed] [Google Scholar]
- Mericle AA, Carrico AW, Hemberg JL, & de Guzman R (2017). Intersecting identities among MSM in recovery residences. Alcoholism: Clinical and Experimental Research, 41(S1), 287A. [Google Scholar]
- Mericle AA, Karriker-Jaffe KJ, Gupta S, Sheridan DM, & Polcin DL (2016). Distribution and neighborhood correlates of sober living house locations in Los Angeles. American Journal of Community Psychology, 58(1–2), 89–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mericle AA, Miles J, & Cacciola J (2015). A critical component of the substance abuse continuum of care: recovery homes in Philadelphia. Journal of Psychoactive Drugs, 47(1), 80–90. [DOI] [PubMed] [Google Scholar]
- Mericle AA, Polcin DL, Hemberg J, & Miles J (2017). Recovery housing: evolving models to address resident needs. Journal of Psychoactive Drugs, 49(4), 352–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles J, Reif S, & Mericle AA (2017). Program features and provider challenges of licensed recovery residences in Massachusetts: Preliminary results Annual Addiction Health Services Research Conference. Madison, WI. [Google Scholar]
- Muthén B, & Asparouhov T (2011). Beyond multilevel regression modeling: Multilevel analysis in a general latent variable framework In Hox JJ & Roberts JK (Eds.), European Association for Methodology series: Handbook of Advanced Multilevel Analysis (pp. 15–40). New York, NY: US: Routledge/Taylor and Francis. [Google Scholar]
- Muthén LK, & Muthén BO (1998–2012). Mplus User’s Guide, Seventh Edition [https://www.statmodel.com/download/usersguide/Mplus%20user%20guide%20Ver_7_r3_web.pdf]. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- National Alliance for Recovery Residences. (2017a). Domains, Core Principles and Standards [https://narronline.org/wp-content/uploads/2017/10/NARR_Standard_V2_rev_07-10-2017.pdf].
- National Alliance for Recovery Residences. (2017b). NARR Code of Ethics [https://narronline.org/wp-content/uploads/2017/10/NARR_ethics_code_amended_10-2017.pdf].
- National Association of Recovery Residences. (2012). A brief primer on recovery residences: FAQ [Accessed: 2014-01-16 Archived by WebCite® at http://www.webcitation.org/6Mg0GCoVM] (pp. 15). Atlanta, GA. [Google Scholar]
- Oxford House Inc. (2015). Oxford House Manual: An idea based on a sound system for recovering alcoholics and drug addicts to help themselves [https://www.oxfordhouse.org/userfiles/file/doc/BasMan.pdf]. Silver Spring, MD. [Google Scholar]
- Oxford House Inc. (2018). Annual Report, Fiscal Year 2017 [https://www.oxfordhouse.org/userfiles/file/doc/ar2017.pdf]. Silver Spring, MD. [Google Scholar]
- Pfeffer J, & Salancik GR (1978). The external control of organizations: A resource dependence perspective. New York, NY: Harper and Row. [Google Scholar]
- Polcin DL (2009). A model for sober housing during outpatient treatment. Journal of Psychoactive Drugs, 41(2), 153–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, & Henderson DM (2008). A clean and sober place to live: philosophy, structure, and purported therapeutic factors in sober living houses. Journal of Psychoactive Drugs, 40(2), 153–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Korcha R, Bond J, & Galloway G (2010a). Eighteen-month outcomes for clients receiving combined outpatient treatment and sober living houses. Journal of Substance Abuse, 15(5), 352–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Korcha R, Bond J, & Galloway G (2010b). What did we learn from our study on sober living houses and where do we go from here? Journal of Psychoactive Drugs, 42(4), 425–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Korcha R, Witbrodt J, Mericle AA, & Mahoney E (in press). Motivational Interviewing Case Management (MICM) for persons on probation or parole entering sober living houses. Criminal Justice and Behavior. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Korcha RA, Bond J, & Galloway G (2010). Sober living houses for alcohol and drug dependence: 18-month outcomes. Journal of Substance Abuse Treatment, 38(4), 356–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Mericle AA, Callahan S, Harvey R, & Jason LA (2016). Challenges and rewards of conducting research on recovery residences for alcohol and drug disorders. Journal of Drug Issues, 46(1), 51–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical Linear Models: Applications and data analysis methods (2nd ed.). Thousand Oaks, CA: SAGE Publications. [Google Scholar]
- Reif S, George P, Braude L, Dougherty RH, Daniels AS, Ghose SS, & Delphin-Rittmon ME (2014). Recovery housing: assessing the evidence. Psychiatric Services, 65(3), 295–300. [DOI] [PubMed] [Google Scholar]
- Room J, & Kaskutas L (2008). Social Model Philosophy Scale (SMPS): Manual. Guidelines for scale administration and interpretation: residential, non-residential & detoxification alcohol and drug programs, revised. Emeryville, CA: Alcohol Research Group. [Google Scholar]
- Room J, Kaskutas LA, & Piroth K (1998). A brief overview of the social model approach. Contemporary Drug Problems, 25(4), 649–664. [Google Scholar]
- Salzer MS, Schwenk E, & Brusilovskiy E (2010). Certified peer speciality roles and activities: Results from a national survey. Psychiatric Services, 61(5), 520–523. doi: 10.1176/ps.2010.61.5.520 [DOI] [PubMed] [Google Scholar]
- Scott WR, & Davis GF (2007). Organizations and organizing: Rational, natural, and open system perspectives. Upper Saddle River, NJ: Pearson Prentice Hall. [Google Scholar]
- Sobell LC, Sobell MB, Buchan G, Cleland PA, Fedoroff IC, & Leo GI (1996). The reliability of the Timeline Followback method applied to drug, cigarette, and cannabis use Association for the Advancement of Behavior Therapy. New York, NY: November 21–24. [Google Scholar]
- StataCorp. (2017). Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC. [Google Scholar]
- Stevens E, Guerrero M, Green A, & Jason LA (2018). Relationship of hope, sense of community, and quality of life [ 10.1002/jcop.21959]. Journal of Community Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens E, Jason LA, Ram D, & Light J (2015). Investigating social support and network relationships in substance use disorder recovery. Substance Abuse, 36(4), 396–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2012). SAMHSA’s Working Definition of Recovery [Accessed: 2015-07-31 Archived by WebCite® at http://www.webcitation.org/6aRHz0R8X] (pp. 7). Rockville, MD. [Google Scholar]
- Tsemberis S, Gulcur L, & Nakae M (2004). Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. American Journal of Public Health, 94(4), 651–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren S (2011). Multiple imputation of multilevel data In Hox JJ (Ed.), Handbook of Advanced Multilevel Analysis (pp. 173–196). New York, NY: Routledge. [Google Scholar]
- Watson DP, Wagner DE, & Rivers M (2013). Understanding the critical ingredients for facilitating consumer change in housing first programming: A case study approach. The Journal of Behavioral Health Services & Research, 40(2), 169–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White WL (2008). Recovery Management and Recovery-oriented Systems of Care: Scientific rationale and promising practices. Pittsburgh, PA: Northeast Addiction Technology Transfer Center, the Great Lakes Addiction Technology Transfer Center, and the Philadelphia Department of Behavioral Health/Mental Retardation Services. [Google Scholar]
- White WL (2010). Nonclinical addiction recovery support services: History, rationale, models, potentials, and pitfalls. Alcoholism Treatment Quarterly, 28(3), 256–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittman FD, Jee B, Polcin DL, & Henderson D (2014). The setting is the service: how the architecture of the sober living residence supports community based recovery. International Journal of Self Help and Self Care, 8(2), 189–225. doi: 10.2190/SH.8.2.d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zins C (2001). Defining human services. The Journal of Sociology and Social Welfare, 28(1), 3–21. [Google Scholar]