Abstract
Background:
One of the potential benefits of insurance reform is greater stability of insurance and reduced coverage disparities by race and ethnicity.
Objectives:
We examined the temporal trends in insurance coverage by racial/ethnic group before and after Massachusetts Insurance Reform by abstracting records across two urban safety net hospital systems.
Research Design:
We examined adjusted odds of being uninsured and incident rate ratios of gaining and losing insurance over time by race and ethnicity. We used billing records to capture the payer for each episode of care.
Subjects:
We included data from January 2005 through December 2013 on patients with hypertension between the ages of 21 and 64 years. We compared four racial and ethnic groups: non-Hispanic White, non-Hispanic Black, non-Hispanic Asian and Hispanic.
Measures:
We examined individual patients’ insurance coverage status in 6 month intervals. We compared odds of being uninsured in the transition and post insurance reform period to the pre reform period, adjusting for age, sex, comorbidities practice location and education and income by Census tract.
Results:
Among 48,291 patients with hypertension, reduction in rates of uninsurance with insurance reform was greater for Hispanic (29.7%), non-Hispanic Black (24.8%) and non-Hispanic Asian (26.8%) than non-Hispanic White (14.9%) patients. The odds of becoming uninsured were reduced in all racial and ethnic groups (OR 0.27–0.41).
Conclusions:
Massachusetts Insurance Reform resulted in stable insurance coverage and a reduction in disparities in insurance instability by race and ethnicity.
Keywords: insurance coverage, health reform, disparities
Introduction
Racial and ethnic health disparities are pervasive, well documented, and consistently linked to health insurance coverage.1,2 Health insurance coverage leads to better disease outcomes by facilitating access to care.3–5 Thus, insurance instability (the frequency of switches in insurance coverage or gaps without coverage) may contribute to disparities in access and quality of care.6,7 With the explicit goal of reducing care disparities, Massachusetts (MA) Health Insurance Reform in 2006–7 extended comprehensive health insurance coverage to 95% of the state’s residents, with disproportionately greater gains in coverage among racial/ethnic minorities and the poor.8 With the increase in insurance options and coverage, however, comes the potential for increased instability, that is, increased switches or loss of insurance.9 With insurance coverage still tied to employment or to income thresholds, there may be a population of patients whose insurance coverage is unstable as their employment or income varies across the eligibility criteria for coverage. Studies have not examined longitudinally whether extending health insurance coverage results in greater stability or instability of such new coverage, and which populations are at greatest likelihood of increased instability.1
Using data from safety net hospital systems that provide a disproportionate share of care for low-income communities, we looked longitudinally at the impact of insurance reform policy on health insurance instability. We hypothesized that before insurance reform, racial and ethnic minority groups would have more insurance instability than whites, that the odds of being uninsured would decrease overall with the implementation of insurance reform, and racial/ethnic minority groups would benefit the most in reduced insurance instability after insurance reform.
Methods
We abstracted data from the electronic health and billing records of patients receiving primary care at two major safety net health care systems, which included two hospitals and six affiliated community health centers in the greater Boston area, all organizations providing a disproportionate share of care to underserved populations. We focused our analyses on patients with a diagnosis of hypertension, a chronic medical condition that requires ongoing management, which would thus allow us to monitor their care and associated insurance coverage over short (six month) time intervals. Hypertension is a common chronic condition, present in women and men, and all racial and ethnic groups, and present as an isolated medical problem, as well as with additional mild, moderate and severe complex comorbidities, such as diabetes, heart disease, pulmonary disease, and renal disease. We used primary care visit data from the electronic health records and the associated registration data, problem list codes, and billing codes to capture clinical and demographic data for each episode of care. Hypertension was defined as patients with the following ICD-9 codes on either a problem list or billing codes 401.0, 401.1, 401.9, 405.01, 405.09, 405.11, 405.19, 405.91, or, 405.99. For insurance coverage, we utilized billing records for each visit for the expected payor of each episode of care. We looked only at primary care visits, as other visit types, including mental health, specialty, pharmacy or dental, may have insurance carve-outs which might appear to be health insurance coverage changes.
We included data from January 2005 through December 2013, starting 18 months prior to implementation of Massachusetts health insurance reform, including the 18-month transition window for implementation of the components of insurance reform, and continuing for six years after implementation but before implementation of the national Affordable Care Act.
We included data on all patients between the ages of 21 and 64 years on the date of the visit. We excluded patients once they reached 65 years, as they were then Medicare eligible, without risk of loss of this eligibility. We defined four racial and ethnic groups with sufficient size for comparisons: non-Hispanic White (white), non-Hispanic Black (Black), non-Hispanic Asian (Asian), and Hispanic. We excluded those whose race/ethnicity was missing (7.4%) or in the “other” category (4.3%).
Measures
We classified individual patients’ insurance coverage at each primary care office visit using five categories: 1) privately insured, which included employer based or individual coverage without subsidies, 2) Medicaid, 3) Medicare, 4) insurance products available on the insurance exchange that were subsidized (e.g., Commonwealth Care), and 5) uninsured. For visits with other types of insurance (e.g. coverage by dental plans, worker’s compensation, or automobile insurance coverage of an injury) or nursing and other visits with no associated bill, we carried forward the primary insurance from the past visit. A switch in insurance coverage was defined as moving from one of the five categories to another with insurance loss or gain defined as subsets of switches. Changes in coverage within the same category, such as one private insurance policy to another with change in employment, were not considered an insurance switch. Based upon the individual insurance coverage at each clinical visit, we created six-month intervals per person (January–June, and July–December); switches were calculated by comparing each primary care visit to the previous primary care visit, whether or not the visits were in the same interval; our primary analysis outcome was “ever uninsured” versus “always insured” within each six-month interval. Individuals were included in the analytic data only during those six-month intervals where they had a primary care visit.
We collected the following data for use as covariates in our analyses. Comorbidities were assessed at each visit using the Charlson comorbidity score. We utilized median household income in 2014 dollars and percentage with high school graduation in Census tract of residence as a proxy for socioeconomic status. Other covariates included sex, age, and location of care, stratifying into three groupings, by either of the two medical centers, or one of the community health centers. Age, Charlson score, and median household income and high school graduation by Census tract were included as time dependent covariates measured at the beginning of each interval.
Analysis Plan
We first examined characteristics of the sample, using descriptive statistics. Because the data contained repeated observations from the same patients over time, we used generalized estimating equation regression models to account for correlated measurements over time. For binary outcomes, we used the log link and binomial distribution. For count data, we used the log link and negative binomial distribution. We plotted rates of insurance over time, stratified by four racial/ethnic groups (white, Black, Hispanic, Asian) and adjusted by covariates. We modeled time in these analyses as “piece-wise linear” (a series of six 18-month time segments from 1/1/05 to 12/31/13). We examined the odds of being uninsured using a categorical approach, representing the pre-reform (1/1/05 to 6/30/06), transition (7/1/06–12/31/07), and post-reform (1/1/08–6/30/09) periods. We calculated the incidence rate ratios (IRR) of all insurance switches, and the subsets of loss and gain of insurance, to examine whether insurance loss or gain varied by race/ethnicity, after adjusting for possible confounders. In analyses of number of insurance switches, we modeled time as categorical, and calculated the incidence rate ratios (IRR) of all insurance switches, and the subtypes of loss and gain of insurance, to examine whether there were changes after insurance reform, and whether the changes varied by race/ethnicity. Models were adjusted for possible confounders including age, comorbidities, sex, site of care, and education and income by census tract. In each model, to assess whether there were differences among race/ethnicity categories in changes over time, we used the likelihood ratio test to perform a global test of all race*period terms.
We conducted a sensitivity analysis, censoring individuals after the first 6 month interval with no primary care visits, in the event that these intervals are more likely to be associated with losing insurance and therefore not seeking care. We repeated the adjusted analyses calculating odds of being uninsured, and the incidence rate ratios of switches.
Results
We included in our analyses data from 48,291 unique patients and 305,268 6-month person-intervals (Table 1). Of the subjects, 52.8% were women, 56.9% Black, 28.9% white, 7.8% Hispanic, and 6.3% were Asian. Mean age at the first visit within the dataset was 46.9 years (standard deviation (SD) 11.1 years). Mean of the median Census tract income was $57,667 (SD $25,654). Mean Census tract percentage of residents with high school graduation was 82.3% (SD, 10.3%). The Charlson score was 0 for 56.2% of subjects; 24.8% had a score of 1, and 18.9% had a score of 2 or greater at their first included visit. Overall within the dataset, of the 18 possible six-month intervals, the average number of intervals per individual was 6.3 (or just over 3 years) of time with visits within the clinical practice, with average number of six-month intervals by racial/ethnic group ranging from 4.6 for Hispanics to 6.6.for Asian subjects. We found that Hispanic and Black groups had more comorbidities, and were more likely to be in Census tracts with lower education and income.
Table 1.
Demographic Characteristics of Patients from Two Massachusetts Urban Safety Net Hospital Systems*, 2005–2013
| Variable | n | Non-Hispanic White n = 13,969 (28.9) | Hispanic n = 3,763 (7.8) | Black/African American n = 27,499 (56.9) | Asian/Asian Pacific Islander n = 3,060 (6.3) | |
|---|---|---|---|---|---|---|
| Age (years) (mean (SD)) | 48,291 | 46.9 (11.1) | 48.41 (10.7) | 46.16 (11.1) | 45.94 (11.2) | 49.89 (10.5) |
| Male | 48,289 | 22,795 (47.2) | 7637 (54.7) | 1944 (51.7) | 11811 (42.9) | 1403 (45.8) |
| Race | 48,291 | |||||
| Charlson Comorbidity Score | 48,284 | |||||
| 0 | 27,151 (56.2) | 7960 (57.0) | 1998 (53.1) | 15300 (55.6) | 1893 (61.9) | |
| 1 | 11,986 (24.8) | 3358(24.0) | 1012 (26.9) | 6852 (24.9) | 764 (25.0) | |
| ≥2 | 9,147 (18.9) | 2646 (18.9) | 752 (20.0) | 5346 (19.4) | 403 (13.2) | |
| Census Tract High School Graduate or Higher (%) (mean (SD)) | 44,259 | 82.3 (10.3) | 87.76 (9.5) | 78.95 (10.9) | 79.97 (9.5) | 83.00 (10.5) |
| Census Tract Income (mean (SD)) | 44,259 | $57,667 ($25,654) | $72245.29 (28033.9) | $50527.88 (23087.8) | $50743.03 (21151.4) | $62528.06 (25404.3) |
| Site | ||||||
| Academic Center A | 26,551 (55.0) | 6711 (48.1) | 2155 (57.4) | 16796 (61.2) | 889 (29.1) | |
| Community Health Centers | 17,348 (36.0) | 4863 (34.9) | 1378 (36.7) | 9569 (34.8) | 1538 (50.3) | |
| Academic Center B | 4,320 (9.0) | 2378 (17.0) | 219 (5.8) | 1091 (4.0) | 632 (20.7) |
Data from patients receiving primary care at two urban safety net hospitals and six community health centers.
Results are frequency (%) unless otherwise indicated.
The mean number of 6 month intervals per individual in the data was 6.3, ranging from 4.6 for Hispanic to 6.6 for Asian patients.
Rates of Uninsurance
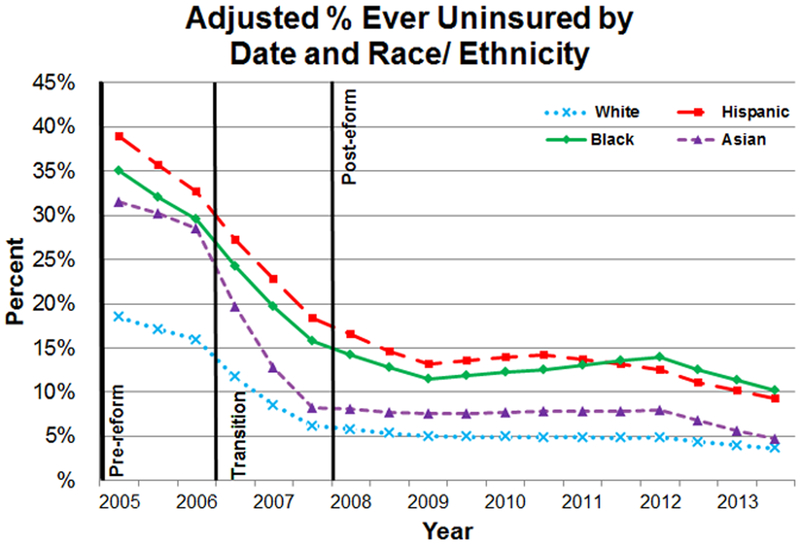
Rates of patients in our cohort who were ever uninsured declined from 30.2% in the period before insurance reform, to 18.8% in the transition period and 12.4% in the post reform period. Figure 1 gives the adjusted percentages of individuals in our sample who were uninsured during at least some part of each six-month interval. During the first half of 2005, the adjusted percentage of individuals without insurance was 18.5% for whites, lower than the rates of 38.9%, 35.0% and 31.6% for Hispanic, Black and Asian groups, respectively. These rates had already declined to 11.7% for whites, and 27.2%, 24.3%, and 19.7% for Hispanic, Black and Asian groups by mid-2006 before the initiation of 2007 Massachusetts Health Insurance Reform. These numbers further decreased sharply during the transitional implementation period and were 5.8%, 16.6%, 14.2% and 8.1% for white, Hispanic, Black and Asian groups, respectively, by the beginning of 2008. By the end of the post-reform observation period in 2013, adjusted rates of those uninsured continued to be lower for whites (3.6%) and Asians (4.8%), than for Hispanic (9.2%) and Black (10.2%) patients. The absolute decline from 2005 through 2013 in those uninsured was 26.8% for Asians, 24.8% for Blacks, 29.7% for Hispanics, and 14.9% for whites.
Figure 1.
Adjusted percentage of Ever Uninsured by Date and Race/Ethnicity Time was modeled as piece-wise linear, adjusting for sex, age, Charlson comorbidity score, practice location, and income and education by census tract.
Table 2 gives the adjusted odds ratios (ORs) for being ever uninsured versus never uninsured in a six-month interval during the transition and post reform period, as compared with pre-reform, overall and by race/ethnicity, with ORs less than one indicating more stable health insurance. These models were adjusted for patient age, sex, Charlson comorbidity score, clinical practice location, and Census tract education and income level. In comparison to the pre-reform period, the odds of ever being uninsured were reduced in the transition period, with ORs of 0.58–0.64 across all racial and ethnic groups. In the post-reform period, the odds of being ever uninsured decreased even further, with ORs in the 0.27–0.41 range. The interaction term between race/ethnicity and time period was significant (p=0.004), with the greatest decline in odds of ever being uninsured among the Asian patients. Sensitivity analyses censoring observations for any patient with a 6 month interval with no primary care visits did not change the direction or significance of the findings. (Appendix A)
Table 2.
Changes in Insurance Stability with Massachusetts Insurance Reform Adjusted Odds Ratios of Ever Versus Never Uninsured By Race/ Ethnicity and Time Period Two Massachusetts Urban Safety Net Health Systems*, 2005–2009
| Ever Uninsured in a 6 month interval during transition and post-reform periods compared with pre- reform period (01/05–06/06) | |||
|---|---|---|---|
| Transition Period (07/06–12/07) | Post-Reform Period (01/08–06/09) | ||
| Race | Number of 6 month study intervals | OR (95% CI) | OR (95% CI) |
| Overall | 128,635 | 0.64(0.63,0.66) | 0.38(0.37,0.39) |
| Non-Hispanic White | 38,945 | 0.64(0.61,0.68) | 0.38(0.35,0.41) |
| Hispanic | 7,285 | 0.63(0.57,0.69) | 0.41(0.36,0.47) |
| Non-Hispanic Black | 74,247 | 0.64(0.62,0.66) | 0.37(0.36,0.39) |
| Non-Hispanic Asian | 8,158 | 0.58(0.53,0.64) | 0.27(0.23,0.32) |
| Interaction Race* Period p-value: 0.004 | |||
Data from patients receiving primary care at two urban safety net hospitals and six community health centers.
Models adjusted for sex, age, Charlson comorbidity score, practice location, and income and education by Census tract. 12,809 Non-Hispanic White, 3,335 Hispanic, 25,406 Non-Hispanic Black and 2,706 Non-Hispanic Asian patients were included in the analysis. Adjusted results were similar to unadjusted analyses.
Table 3 provides the incident rate ratios of number of any insurance switches and the subset of insurance losses and insurance gains per six-month interval, comparing the transition and post-reform period to the pre-reform period for each racial/ethnic group. The number of insurance switches per six-month interval (any switch among the five insurance categories) increased in all racial/ethnic groups in the transition and the post reform period, with IRRs between 1.17 and 1.96. Hispanic and Black patients had similar IRRs to White patients. Asian patients had greater rates of switches (higher IRRs) in both the transition and post-reform compared with White. The interaction term between race and time period was significant at p = 0.0005.
Table 3.
Number of Insurance Switches and Insurance Losses per 6 month interval by Race/ Ethnicity in Two Massachusetts Urban Safety Net Hospital Systems* , 2005–2009
| Incidence Rate Ratios of Any Insurance Switches, Losses or Gains per 6 month interval | Incidence Rate Ratios of Losses of Insurance per 6 month interval | Incidence Rate Ratios of Gains of Insurance per 6 month interval | |||||
|---|---|---|---|---|---|---|---|
| Transition Period (07/06–12/07) | Post-Reform Period (01/08–06/09) | Transition Period (07/06–12/07) | Post-Reform Period (01/08–06/09) | Transition Period (07/06–12/07) | Post-Reform Period (01/08–06/09) | ||
| Number of 6 month study intervals | IRR (95% CI) p-value | IRR (95% CI) p-value | IRR (95% CI) p-value | IRR (95% CI) p-value | IRR (95% CI) p-value | IRR (95% CI) p-value | |
| Overall | 120,962 | 1.20 (1.15,1.26) | 1.22 (1.17,1.28) | 0.86 (0.79,0.94) | 1.05 (0.96,1.14) | 1.21 (1.14,1.27) | 0.83 (0.78,0.88) |
| By Race/Ethnicity | |||||||
| Non-Hispanic White | 36,561 | 1.19 (1.07,1.32) | 1.24 (1.10,1.38) | 0.74 (0.6,0.92) | 1.07 (0.86,1.33) | 1.23 (1.09,1.40) | 0.77 (0.67,0.89) |
| Hispanic | 6,694 | 1.29 (1.08,1.54) | 1.33 (1.11,1.59) | 1.01 (0.72,1.42) | 1.06 (0.75,1.50) | 1.31 (1.05,1.63) | 1.02 (0.81,1.28) |
| Non-Hispanic Black | 69,991 | 1.17 (1.11,1.24) | 1.18 (1.11,1.25) | 0.89 (0.80,0.99) | 1.01 (0.91,1.11) | 1.14 (1.07,1.22) | 0.82 (0.76,0.88) |
| Non-Hispanic Asian | 7,716 | 1.87 (1.50,2.33) | 1.96 (1.56,2.46) | 0.67 (0.39,1.16) | 1.88 (1.22,2.90) | 2.22 (1.71,2.88) | 1.03 (0.77,1.38) |
| Interaction race* period p-value=0.0005. | Interaction race* period p-value=0.001. | Interaction race* period p-value<0.001. | |||||
Data from patients receiving primary care at two urban safety net hospitals and six community health centers.
Models adjusted for sex, age, Charlson comorbidity score, practice location, and income and education by Census tract. 7,981 Non-Hispanic White, 1,748 Hispanic, 15,187 Non-Hispanic Black and 1,656 Non-Hispanic Asian patients were included in the analysis. Adjusted results were similar to unadjusted analyses.
In contrast to the increased incidence rates of any insurance switches, the IRRs of losing insurance during any six-month interval remained stable or declined during the transition period. Compared with the pre-reform period, the adjusted rate ratios of losing insurance dropped in the transition period for White patients (IRR 0.74, CI (0.60, 0.92)) and Black patients (IRR 0.89, CI (0.80, 0.99)), but with no statistically significant reduction for Asians or Hispanics. In the post reform period, the IRRs remained similar to pre-reform period rates for whites, Blacks and Hispanics but increased for Asian populations (IRR 1.88, CI(1.22, 2.90)). This difference in the Asian population was significant, with a significant interaction term between race and time period.
The incident rate ratios for any insurance gains among those uninsured increased in the transition period for all groups. The ongoing rates of gaining insurance if still uninsured in the post reform period dropped among white and black populations, and remained stable among Hispanic and Asian groups. Sensitivity analyses censoring observations for any patient with a 6 month interval with no primary care visits did not change the direction or significance of the findings. (Appendix A)
Discussion
One of the stated goals of the Massachusetts Health Insurance Reform was to reduce racial and ethnic disparities in coverage and in health outcomes.10 Our data from two urban safety net hospital systems that provide a disproportionate share of care to minority and uninsured communities demonstrated the benefits of insurance reform on increased insurance coverage for all racial and ethnic groups studied. All racial and ethnic groups demonstrated major reductions in being uninsured, with Hispanic, Black and Asian patients having larger absolute reductions in being uninsured than whites, leading to reduced disparities. Furthermore, most racial/ethnic groups in our population did not demonstrate increased losses of coverage over time. Whites and Blacks were significantly less likely to lose insurance in the transition as compared with the pre-reform period, but in the post-reform period their rates of losing insurance were back to pre-reform levels. Rates for Hispanics did not change over time, whereas Asians had increased rates of insurance loss in the post-reform period. The higher rate of insurance loss among Asians is likely related to their extreme improvement in coverage; a person can only lose insurance coverage after they have it. Adjusted rates of switching across types of insurance increased across all racial/ethnic groups.
In 2005, white populations had the lowest rates of being uninsured (20%), compared with Asian, Black and Hispanic groups (33–43%). By 2013, white and Asian patients had similar low rates of being uninsured (4–6%); although rates among Black and Hispanic patients dropped dramatically, they continued to have higher rates of being uninsured (12%). We noted a decrease in those uninsured even before the implementation of the 2006–2007 insurance reform transition period. Even before 2006, Massachusetts had extended Medicaid eligibility, provided insurance premium support to low income workers with employer-based coverage, and conducted an outreach strategy to inform potential beneficiaries of these opportunities.11 However, the 2006–7 insurance reform was associated with a rapid and sustained reduction in individuals being uninsured. Despite the major reductions in patients who were uninsured, these safety net institutions continued to provide care for a higher proportion of the uninsured : overall rates of uninsurance in Massachusetts were lower at 4.0% than our sample by 2008 and remained under 5% through 2013.8,12
One of the concerns about insurance reform was the risk of increased instability, with either increases in switches in types of coverage, or cycles where patients come on and off insurance coverage. Both of these are potentially detrimental to the management of chronic diseases such as hypertension, as patients may not have coverage for chronic disease medications, or may need to switch types of medication or primary providers who oversee their hypertension care. We did see an increase in the number of switches across insurance types. This is in part the goal of insurance reform, where we expected to initially see patients switch from being uninsured to being insured. However, the higher adjusted IRRs of insurance switches continued in the post-reform period, and were present in all racial/ethnic groups, suggesting that consistency in the type of insurance coverage for many individuals remained unstable. Some of these changes may also reflect the economic downturn beginning in 2008 and more individuals subsequently losing employer-based coverage.13 Critically during this period, with the exception of the Asian population, we did not see an increase in gaps in coverage.
There are limitations to our analysis. Our work does not represent the impact of the insurance reform on the entire state or among rural residents, but focused on the impact on patients of two major urban health care systems. However, these two systems provide a large proportion of care to vulnerable populations in Boston, and are likely to care for the communities for whom the changes were intended. One limitation to our understanding of the impact of insurance reform on minority groups was the combining of numerous subpopulations within these categories. For example, the Asian group contains mostly Chinese and Vietnamese communities, the Black group contains both American-born African Americans and populations from a number of African and Caribbean countries, and the Hispanic group includes primarily Puerto Rican and Dominican communities. We have limited our analysis to a subpopulation of patients seeking care for hypertension. Those with a chronic health condition may be more likely to strive to maintain insurance coverage and thus this focus may underestimate the number of losses of insurance across the broader population. We assessed insurance status based on the billing data. Although this was collected retrospectively, it may still include the expected and not actual payor in some cases. We are only able to assess insurance status when patients seek care; we may underestimate rates of insurance loss if patients do not return for care during gaps in insurance. We attempted to assess the potential magnitude of this underestimation. When we performed a sensitivity analysis which only included intervals where patients have care in consecutive 6-month intervals, we found no differences in the overall effect sizes. Due to the de-identified nature of our databases, we were unable to link individual patient visits for patients who moved their care across our health systems or community health centers. Another limitation is the potential of patients leaving the safety net for care once they become insured. Data from 2004–09 in Massachusetts indicates that most patients remained with their care providers in the safety net when they gained insurance.14
Prior research examined insurance coverage through serial cross sectional analyses, whereas our data spanned nine years, with an average of more than three years of data per patient. One cross sectional survey of beneficiaries in Kentucky reported 25% of individuals with insurance switches, mainly due to employment changes or change in eligibility for Medicaid or subsidized coverage.15 Survey data from MEPS 2000–2002 indicated that among adults covered under Medicaid, 7.8% switched to another insurer and 13.6% lost insurance within one year.16
Strengths of our analyses include our focus on two large safety-net institutions, while including a significant stable privately insurance population for comparison. The use of the two systems allows comparison of a number of racial and ethnic communities. Patients within our sample had an average of over three years of continuity with their care provider, allowing us to conduct a longitudinal analysis. A major strength is the large sample with diverse patients, with sufficient Black, Hispanic, and Asian patients to make estimates, and diversity of income and education. Note that Massachusetts insurance reform explicitly aimed to reduce disparities, so this is an ideal sample in which to examine whether the policy had the intended effect.
Our data demonstrated that the Massachusetts insurance reform resulted in increased and sustained insurance coverage for patients from racially/ethnically diverse communities and a reduction in the disparities in insurance coverage by race/ethnicity. The complexity of the system of subsidized and employer-based coverage has resulted in increased instability in the type of coverage; however, it did not result in increased gaps or losses in coverage.
Supplementary Material
Acknowledgments
Disclosure of Funding: The project described was supported by the National Center for Advancing Translational Sciences and National Institute on Minority Health and Health Disparities, National Institutes of Health (UL1TR001064 and R01MD007735, respectively). Dr. Nancy Kressin is supported in part by a Senior VA Health Services Research & Development Service Research Career Scientist award (#02-066-1). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Department of Veterans Affairs.
Footnotes
Disclosure of Conflicts of Interest: Authors have no conflicts of interest to disclose.
References
- 1.Freeman JD, Kadiyala S, Bell JF, Martin DP. The causal effect of health insurance on utilization and outcomes in adults: a systematic review of US studies. Medical care. 2008:1023–1032. [DOI] [PubMed] [Google Scholar]
- 2.Smedley BD, Stith AY, Nelson AR. Institute of Medicine, Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care Unequal treatment: confronting racial and ethnic disparities in healthcare. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 3.Sommers BD, Gawande AA, Baicker K. Health insurance coverage and health—what the recent evidence tells us. Mass Medical Soc; 2017. [DOI] [PubMed] [Google Scholar]
- 4.Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. Hypertension, diabetes, and elevated cholesterol among insured and uninsured US adults. Health Affairs. 2009;28(6):w1151–w1159. [DOI] [PubMed] [Google Scholar]
- 5.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: US trends from 1999 to 2006 and effects of medicare coverage. Annals of Internal Medicine. 2009;150(8):505–515. [DOI] [PubMed] [Google Scholar]
- 6.Schoen C, DesRoches C. Uninsured and unstably insured: the importance of continuous insurance coverage. Health services research. 2000;35(1 Pt 2):187. [PMC free article] [PubMed] [Google Scholar]
- 7.Kapoor A, Battaglia TA, Isabelle AP, et al. The impact of insurance coverage during insurance reform on diagnostic resolution of cancer screening abnormalities. Journal of health care for the poor and underserved. 2014;25(1 0):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Long SK, Skopec L, Shelto A, Nordahl K, Walsh KK. Massachusetts health reform at ten years: great progress, but coverage gaps remain. Health Affairs. 2016;35(9):1633–1637. [DOI] [PubMed] [Google Scholar]
- 9.Sommers BD, Rosenbaum S. Issues in health reform: how changes in eligibility may move millions back and forth between Medicaid and insurance exchanges. Health Affairs. 2011;30(2):228–236. [DOI] [PubMed] [Google Scholar]
- 10.McDonough JE, Rosman B, Butt M, Tucker L, Howe LK. Massachusetts health reform implementation: major progress and future challenges. Health Affairs. 2008;27(4):w285–w297. [DOI] [PubMed] [Google Scholar]
- 11.McDonough JE, Rosman B, Phelps F, Shannon M. The third wave of Massachusetts health care access reform. Health Affairs. 2006;25(6):w420–w431. [DOI] [PubMed] [Google Scholar]
- 12.Long SK, Stockley K. Sustaining health reform in a recession: an update on Massachusetts as of fall 2009. Health Affairs. 2010;29(6):1234–1241. [DOI] [PubMed] [Google Scholar]
- 13.Margerison-Zilko C, Goldman-Mellor S, Falconi A, Downing J. Health impacts of the great recession: a critical review. Current epidemiology reports. 2016;3(1):81–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lasser KE, Hanchate AD, McCormick D, Chu C, Xuan Z, Kressin NR. Massachusetts health reform’s effect on hospitals’ racial mix of patients and on patients’ use of safety-net hospitals. Medical care. 2016;54(9):827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sommers BD, Gourevitch R, Maylone B, Blendon RJ, Epstein AM. Insurance churning rates for low-income adults under health reform: lower than expected but still harmful for many. Health Affairs. 2016;35(10):1816–1824. [DOI] [PubMed] [Google Scholar]
- 16.Sommers BD. Loss of health insurance among non-elderly adults in Medicaid. Journal of general internal medicine. 2009;24(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.