ABSTRACT
In November 2017, it was announced that the new dengue vaccine (“Dengvaxia”) had risks for those not previously exposed to dengue. While some countries proceeded with adjusting guidance accordingly, the Philippines reacted with outrage and political turmoil with naming and shaming of government officials involved in purchasing the vaccine, as well as scientists involved in the vaccine trials and assessment. The result was broken public trust around the dengue vaccine as well heightened anxiety around vaccines in general. The Vaccine Confidence ProjectTM measured the impact of this crisis, comparing confidence levels in 2015, before the incident, with levels in 2018. The findings reflect a dramatic drop in vaccine confidence from 93% “strongly agreeing” that vaccines are important in 2015 to 32% in 2018. There was a drop in confidence in those strongly agreeing that vaccines are safe from 82% in 2015 to only 21% in 2018; similarly confidence in the effectiveness of vaccines dropped from 82% in 2015 to only 22%. This article highlights the importance of routinely identifying gaps or breakdowns in public confidence in order to rebuild trust, before a pandemic threat, when societal and political cooperation with be key to an effective response.
KEYWORDS: Vaccine confidence, dengue vaccine, Dengvaxia, Philippines, pandemic preparedness, risk perception, public trust, vaccine confidence index
Marking its 100th anniversary, there have been numerous articles and books reflecting on the 1918 “Spanish” flu from scientific, public health, historical and social science perspectives. The common thread is the acknowledgement that it was the biggest killer in recorded pandemic history, killing more people than the battles of the First World War. Estimates for the number of people who died range between 50 to 100 million. It was, as one article framed it, the “Mother of all Pandemics”.1
While anniversaries beg “lessons learned”, and response efforts around the 2009 A/H1N1 pandemic – a descendent of the original 1918 strain – regularly referred to the Spanish flu to alert politicians and the public that this was not “just the flu”, the public seemed unconcerned.
Furthermore, while there was no vaccine available to counter the 1918 scourge, the one made available in 2009 had less than optimal uptake, if any.2–4
Perhaps the 1918 episode is deemed just too long ago to have relevance. A tragic history tale, but we’ve come a long way since then. Indeed, from many perspectives, there have been tremendous scientific and public health advances. But, when it comes to public emotion, we have hardly evolved. In fact, with the advent of the internet and social media, the viral spread of anxieties, beliefs and rumours has reached unprecedented levels of speed and spread around the world. Social media platforms like Facebook have been used as to propagate fake news and unsubstantiated allegations, viciously damaging programs, institutions and individuals without checks and balance. Critical thinking has become increasingly challenged by belief in conspiracy and false narratives.5
Historic experiences, personal narratives and community memories are not forgotten, particularly when they have triggered past anxiety and concern.6 In the context of acute uncertainty and risk, trust becomes key. Reflecting on where episodes of vaccine reluctance and refusal have exposed underlying distrust, political tensions and underlying hostilities can help anticipate where trust building is needed most. We cannot wait until pandemics strike, we must prepare for the next “big one”, when trust and cooperation will be key to containing the spread of disease and mitigating its health and societal impacts.
The example of political drama, public outcry and breakdown of trust in the Philippines, following a newly reported risk identified in a recently introduced dengue vaccine, is a poignant tale. It reveals the cost of broken trust in the context of high risk. Trust which needs to be rebuilt soon, before a pandemic strikes. Not only has the current dengue vaccine panic undermined trust in the dengue vaccine, but also in vaccines more broadly, as well as other interventions provided by health clinics, such as deworming medication. The Philippines story reveals the implications for broader public trust in government health interventions and strategies should a pandemic strike.
The Philippines dengue vaccine panic
On the 29th November 2017, Sanofi announced a new finding that their new dengue vaccine posed a risk when given to people not previously exposed to dengue.7,8 Unfortunately, unlike the other countries that have used this novel vaccine, and dealt with the new warning by advising relevant local authorities, changing the guidance and amending the label, the Philippines reacted with a dramatic public and political outcry. There was biased media hype; social media was driven by false narratives aiming to vilify authorities, scientists and regulators; separate senate and congress inquiries that resembled the inquisition; a Public Attorney Office exhuming bodies and concluding that the dengue vaccine caused the deaths despite no solid evidence; and a handful of health professionals distorting scientific and regulatory information. All of these fuelled a highly political controversy and provoked public panic.
The results of the various parliamentary investigations seem to demonstrate that tolerance for vaccine risk is low and that a zero-risk vaccine is the only one that would be acceptable. Even World Health Organisation (WHO) was questioned in the course of the investigation. The reaction led to public anxiety and fear around the dengue vaccine (and vaccines more broadly) as well as other health interventions, such as deworming medicine, in both public health programs and private clinics.
Accusations of impropriety were directed at health authorities who had launched the vaccination campaign in three regions of the country with the highest burden of disease in 2016 in an effort to help arrest a debilitating, and in some cases, fatal dengue epidemic.9 Dengue cases were very high from 2012–2015, filling hospital emergency rooms and resembling a “war zone”. Between 2014 and 2015, there had been a 65 percent increase in the number of dengue cases in the Philippines. By the end of 2015, 200,415 suspected cases of dengue and 598 deaths were reported, compared to 121,000 cases reported in 2014.10 Some local governments declared a state of calamity. The opportunity to introduce a new dengue vaccine, endorsed by the WHO, seemed like a panacea for the public health crisis.
Dengue cases did drop in 2017; but, in the Philippines, the news of the potential vaccine risk in certain circumstances, overwhelmed any perception of vaccine benefit, and instead became a spark fueling the flames of underlying political ferment.
Measuring vaccine confidence
In an effort to measure the impact of the fears and anxiety on broader vaccine confidence, the Philippines was re-surveyed by the Vaccine Confidence ProjectTM with their Vaccine Confidence IndexTM, using the same representative sampling approach used for the 2015 data reported in “The State of Vaccine Confidence 2016” study (in which the methods are fully described).11 The 2018 study surveyed a further 1500 participants to the 1000 surveyed in 2015.
The findings reflect a dramatic drop in overall vaccine confidence from 93% “strongly agreeing” that vaccines are important to only 32% in the 2018 study. With regards to vaccine safety perceptions, there was a drop in those strongly agreeing that vaccines are safe from 82% in 2015 to 21% in 2018 (Figure 1); and the response on confidence in the effectiveness of vaccines similarly dropped from 82% strongly agreeing to only 22%. Even the question inquiring whether vaccines are compatible with the respondents’ religious beliefs decreased significantly from 63% agreeing to only 21% agreeing.
Figure 1.
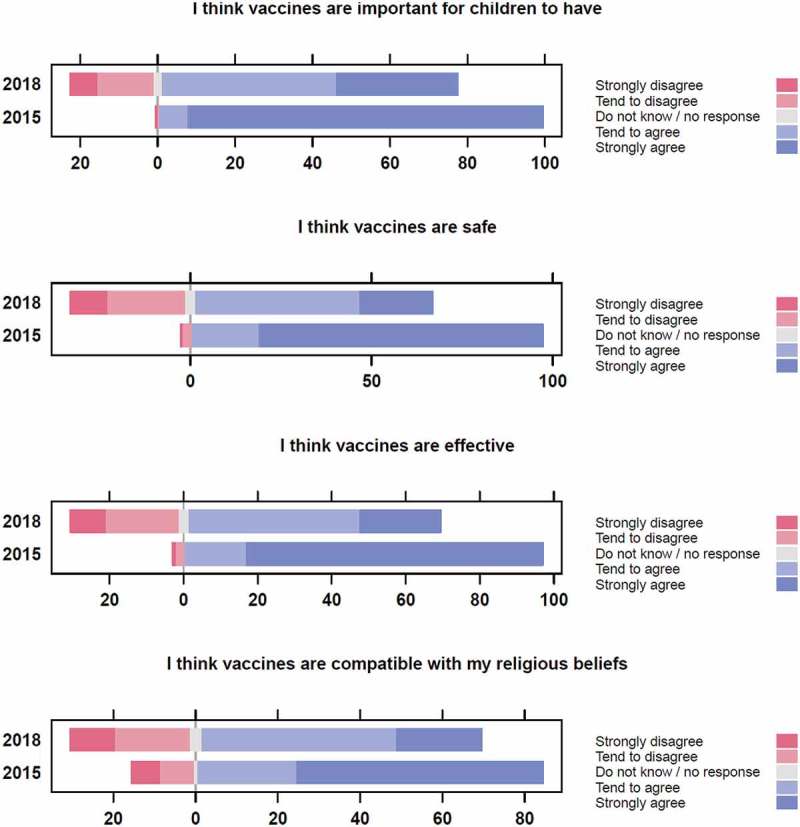
Confidence in vaccines has declined substantially in the Philippines between 2015 and 2018.
Vaccine confidence in the Philippines has declined across all four measures of confidence measured by the Vaccine Confidence ProjectTM: the percentage of respondents agreeing that vaccines are important for children to have has decreased from 99.5% in 2015 to 76.2% in 2018. Similar drops are observed for vaccine safety (97.3% to 65.2%), effectiveness (97.0% to 67.9%), and compatibility with religious beliefs (83.8% to 67.9%).
Conclusion
Episodes such as the Philippines response to the dengue vaccine risk, despite it benefits, are signals of deep dissent and distrust that needs to be considered in advance of a pandemic. While health authorities and immunization programmes cannot resolve broader political tensions and societal polarization, two steps can be taken. Firstly, to re-establish credibility for a damaged reputation of and confidence in the Philippines Department of Health and in the immunization programme, but secondly for the global players involved to examine this experience and consider its handling of risk in times of uncertainty.
Disclosure of potential conflicts of interest
In accordance with Taylor & Francis policy and ICMJE policy regarding Conflicts of Interest, I, Kenneth Hartigan-Go, am reporting that I was one of the undersecretaries of health at the time the Dengvaxia immunization program was initiated in April 2016; I left the Philippine Department of Health (DOH) in June of the same year. At the time of the publication of this commentary, I was not connected to, nor representing, DOH. I have no affiliation with the industry. Neither the DOH nor the industry has provided any assistance or funds for this commentary. I have declared my current affiliation with the Asian Institute of Management, where my position is Head of the Stephen Zuellig School of Development Management, which is not connected to any Zuellig company.
Acknowledgments
We would like to thank PSRC, the Philippines partner in the Worldwide Independent Network of Market Research, WIN/Gallup, who contributed the data for the survey.
References
- 1.Taubenberger JK, Morens DM.. 1918 influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12(1):15–22. doi: 10.3201/eid1201.050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Black S, Rappuoli R. A crisis of public confidence in vaccines. Sci Translational Med. 2010;2(61):61. doi: 10.1126/scitranslmed.3001738. [DOI] [PubMed] [Google Scholar]
- 3.Ofri D. The emotional epidemiology of H1N1 influenza vaccination. New England J Med. 2009;361(27):2594–2595. doi: 10.1056/NEJMp0911047. [DOI] [PubMed] [Google Scholar]
- 4.Bish A, Yardley L, Nicoll A, Michie S. Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine. 2011;29:6472–6484. doi: 10.1016/j.vaccine.2011.06.107. [DOI] [PubMed] [Google Scholar]
- 5.Atlani-Duault L, Kendall C. Influenza, anthropology, and global uncertainties. Med Anthropol. 2009;28(3):207–211. doi: 10.1080/01459740903070519. [DOI] [PubMed] [Google Scholar]
- 6.Larson HJ, Heymann D. Public health response to influenza A (H1N1) as an opportunity to build public trust. JAMA. 2010;303(3):271–272. doi: 10.1001/jama.2009.2023. [DOI] [PubMed] [Google Scholar]
- 7.Pang T, Gubler D, Goh DYT, Ismail Z. Asia Dengue Vaccine Advocacy Group. Dengue vaccination: a more balanced approach is needed. The Lancet. 2018;391:654. doi: 10.1016/S0140-6736(18)30245-9. [DOI] [PubMed] [Google Scholar]
- 8.Rosenbaum L. Trolleyology and the dengue vaccine dilemma. New England J Med. 2018;379(4). doi: 10.1056/NEJMp1804094. [DOI] [PubMed] [Google Scholar]
- 9.Vannice K, Chocarro L, Pfleiderer M, Bellah A, Ward M, Yoon I-K, Hombach J. The value of multi-country joint regulatory reviews: the experience of a WHO joint technical consultation on the CYD-TDV (Dengvaxia®) dossier. Vaccine. 2017. October 13;35(43):5731–5733. doi: 10.1016/j.vaccine.2017.07.044. [DOI] [PubMed] [Google Scholar]
- 10.Herriman R. Philippines reports more than 200,000 dengue cases in 2015. Outbreak News Today. 2016. February 10 [accessed 2018 Aug 02]. http://outbreaknewstoday.com/philippines-reports-more-than-200000-dengue-cases-in-2015/
- 11.Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IJ, Cook AR, Jones NS. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]


