Abstract
Background:
Behavioral intervention with parent participation is effective in reducing symptoms of Autism Spectrum Disorder (ASD), but access to intervention is limited. The current study explored whether a video-enriched parent-training program would (a) be comprehensible and acceptable to parents in the Republic of Albania, (b) increase parental knowledge of behavioral strategies and (c) increase parental self-efficacy.
Methods:
Twenty-nine parents of children with ASD aged 18-70 months completed the Early Intervention Parenting Self-Efficacy Scale (EIPSES, Guimond, Wilcox, & Lamorey, 2008) and a quiz to assess their knowledge of behavioral strategies. Parents in the Treatment Group then received access to a parent-training (PT) program on evidence-based teaching and behavior management techniques. The program was based on empirical research, but considered Albanian cultural norms and included topics Albanian parents requested. Parents in the Treatment Group rated the program using the Treatment Evaluation Inventory Short Form (TEI-SF; Kelley, Heffer, Gresham, & Elliott, 1989). Change in parents’ quiz scores and EIPSES ratings from baseline to post-treatment were compared by group.
Results:
Parents rated this video training program as comprehensible and valuable. The program modestly increased aspects of self-efficacy as well as parents’ knowledge of effective teaching strategies.
Conclusion:
Remote PT may be useful in low-resource settings to help parents develop techniques for teaching skills and forestalling problem behavior in children with ASD. Additional research, with a larger sample size, that observes the effect of the program on child behavior is warranted.
Keywords: Autism spectrum disorders, Parent training, Intervention, Distance learning
Introduction
Although ASD is generally considered a lifelong disorder, symptoms can diminish and individuals with ASD can demonstrate life-enhancing improvements in their communication skills and adaptive behavior (e.g., Anderson, Liang, & Lord, 2014; Bal, Kim, Cheong, & Lord, 2015; Rogers & Vismara, 2008). Yet owing to sociodemographic and logistical factors, access to early intervention programs that can improve outcome remains limited for many families (Chiri & Warfield, 2012; Sharpe, & Baker, 2007; Thomas, Ellis, McLaurin, Daniels, & Morrissey, 2007).
Intensive intervention that takes advantage of the plasticity in early development (Dawson, 2008) is one of the most important predictors of progress in communication and in reductions of restricted, repetitive behaviors (e.g., Anderson et al., 2014; MacDonald, Parry-Cruwys, Dupere, & Ahearn, 2014; Orinstein et al., 2014; Rogers & Vismara, 2008). Participation in early intervention also predicts increases in skills of daily living, which are necessary for independent living (Bal et al., 2015). There are a variety of interventions for children with ASD, but behaviorally based teaching is the most evidence-based method for optimizing outcome (Rogers & Vismara, 2008), especially when parents participate in delivery of the intervention (Ozonoff & Cathcart, 1998; Rogers & Vismara, 2008; Tonge, Brereton, Kiomall, Mackinnon, & Rinehart, 2014). Indeed, reviews of early intervention for ASD have cited family involvement as one of the crucial elements of effective treatment (Hurtb, Shaw, Izeman, Whaley, & Rogers, 1999; Rogers & Vismara, 2008). For example, children’s joint attention, joint engagement, intellectual development, adaptive behavior, compliance, and dyadic communication with parents have all been shown to increase in response to parent training (Bahadourian & Greer, 2005; Bal et al., 2015; Green et al., 2010; Kasari, Gulsrud, Paparella, Hellemann, & Berry, 2015; Rocha, Schreibman, & Stahmer, 2007; Vismara, Young, & Rogers, 2012). Some treatment for very young children, as in the Infant Start Denver Model (Rogers et al, 2014), relies entirely on parent training.
Parents also experience personal advantages as a result of participation in their children’s treatment. For example, parents reported reduced stress levels after they were taught how they could participate in their children’s intervention (Kasari et al., 2015; Keen, Couzens, Muspratt, & Rodger, 2010). In another study that provided parents of young children with ASD with access to a telehealth-based parent-mediated intervention, parents demonstrated reduced stress and greater self-efficacy postintervention, in comparison to their baseline assessments (Ingersoll, Wainer, Berger, Pickard, & Bonter, 2016). Indeed, Hume, Bellini, and Pratt (2005) found that parents judged their own training to confer the greatest impact on their children’s growth of all the services they received.
Parents are especially appropriate agents for helping their children with ASD learn new skills and reduce maladaptive behaviors. Parents are usually children’s earliest teachers and are often in a unique position to notice the emergence of the skill deficits and maladaptive behaviors that signal developmental delay (CDC, 2017; Glascoe, 1999). Parents are also able to practice skills with their children across a variety of contexts, thereby enhancing generalization (Sachse & Von Suchodoletz, 2008). Moreover, children may be more motivated to interact with parents than with intervention providers. Finally, teaching parents to provide intervention can dramatically increase the hours of intervention a child receives.
Barriers to Intervention
Taken together, the literature on ASD suggests that children should ideally receive between 25 and 40 hours of intervention per week (AAP, 2007), and some portion of the intervention should involve parent participation. However, multiple barriers prohibit many children and families from obtaining this level of services. First, parental perceptions of some interventions as not being of high quality diminish their enthusiasm about participation; indeed, some families judge providers’ inability to adequately treat their child as a major obstacle (Chiri & Warfield, 2012).
Second, even if families are enthusiastic about intervention, practical barriers can limit access to services. Intervention can be expensive and geographical locations vary in the amount of free or subsidized support offered for children with ASD (Latifi et al., 2015; Sharpe, & Baker, 2007). Accordingly, poverty and being uninsured are significantly associated with greater unmet need for medical and psychological services (Chiri & Warfield, 2012). Additionally, transportation to and from intervention may be costly and time-consuming. Given the inequitable geographic distribution of health-related resources, this is particularly the case for families living in rural areas (Latifi et al., 2015; Thomas et al., 2007). Moreover, intervention services are frequently offered during standard business hours that overlap with working parents’ schedules. Therefore, bringing a child to a facility to receive intervention, or clearing their schedule in order to participate in their children’s intervention, presents challenges for working parents. If the child with ASD has siblings, parents must arrange for alternative childcare while they travel to a treatment facility and if the older sibling is also affected with ASD, parents may be using resources to facilitate this treatment. In the event that parents are able to overcome these challenges, they often continue to face additional barriers to services due to a scarcity of providers. Specifically variable waitlists in different regions often prevent timely access to intervention, a particularly frustrating limitation for eager parents who have been encouraged to begin treatment as early as possible (Mansell & Morris, 2004; Young, Ruble, & McGrew, 2009).
All of these impediments coalesce to create a substantial gap between available evidence-based ASD intervention services and their utilization. Intervention access is particularly disproportionate across families of different sociodemographic backgrounds, including race/ethnicity, education, and occupation (Kohler, 1999; Liptak et al., 2008; Thomas et al., 2007; Zablotsky, Pringle, Colpe, Kogan, Rice, & Blumberg, 2015). Survey-based studies in the United States suggest that approximately one-third of children with ASD have problems accessing desired services (Kohler, 1999; Krauss, Gulley, Sciegaj, & Wells, 2003; Zablotsky et al., 2015). Twenty-nine percent of parents of children with comorbid ASD, intellectual disability, and an additional psychiatric disorder reported unmet needs for their children’s treatment (Zablotsky et al., 2015).
In addition to the discrepancy within countries, access to intervention varies among countries. While therapists are lacking in developed countries, they are even scarcer in low-resource countries (Fairburn & Patel, 2014). Indeed, over 90 percent of global mental health resources are located in wealthy countries (Fairburn & Patel, 2014). Accordingly, between 76 and 85 percent of people with mental disorders in low and middle income countries reported receiving no treatment in the past year (Fairburn & Patel, 2014).
ASD Services in the Republic of Albania
The Republic of Albania lies in the southeastern region of Europe. Albania’s health care system is primarily public, with the state providing a majority of the health services, including diagnosis and treatment of ASD (Institute of Statistics, Institute of Public Health [Albania] and ICF Macro 2010). Although it was upgraded from a lower- to an upper-middle-income country (the latter denoting gross national income per capita between about $4,000 and $12,000) in 2013 (The World Bank, 2015), Statistics Times lists the per capita GDP in 2016 as $3,946, ranking 40th among the 45 countries in Europe. Services for children with ASD are particularly limited in Albania due to a lack of trained providers and inadequate resources (Daniels, Como, Hergüner, Kostadinova, Stosic, & Shih, 2017; Latifi et al., 2015). Indeed, the first early intervention center for children with ASD in Albania was established in 2009 (Wallace et al., 2012).
In an attempt to increase ASD awareness and improve services, the Albanian Children’s Foundation established the Regional Center for Autism in 2011. While this center has provided intervention access for some families (Brennan, Fein, Como, Carcani Rathwell, & Chen, 2016), overall access to treatment remains limited in the Albanian capital of Tirana and particularly outside Tirana (Daniels et al., 2017; Latifi et al., 2015). In a survey of parents of children with ASD who were evaluated and treated in health care centers and clinics in Albania, 73 percent reported frustration related to obtaining services for their children (Daniels et al., 2017). These parents cited a lack of intervention programs (especially empirically supported behavioral intervention programs), limited knowledge about the existing programs, long waitlists, and financial barriers as impediments to accessing intervention for their children. A majority of parents reported that they rely on easily accessible information on the Internet to learn about ASD (Daniels et al., 2017). It seems likely that the percentage of parents expressing frustration would be even higher in families whose children were not yet evaluated or receiving treatment. Furthermore, nearly half of the parents surveyed in Albania who have children on the autism spectrum over five years of age report that their children are not enrolled in school (Daniels et al., 2017).
Use of Telehealth to Facilitate Intervention Dissemination
In an attempt to facilitate access to healthcare for underserved populations, researchers have explored the potential of remote service delivery to families via DVDs, the Internet, and related technologies. While remote parent training (PT) programs for ASD are relatively novel, a large body of literature supports the use of such programs to treat a variety of mental health conditions. For example, remote parent training has been successfully implemented to treat children’s behavioral disorders, attention-deficit/hyperactivity disorder, and mental health more broadly. These programs have improved parent outcome (e.g., self-efficacy) and child outcome (e.g., symptoms of the diagnosis) (Deitz, Cook, Billings, & Hendrickson, 2008; Nieuwboer, Fukkink, & Hermanns, 2013; Sanders, Calam, Durand, Liversidge, & Carmont, 2008; Taylor, Webster-Stratton, Feil, Broadbent, Widdop, Severson, 2006).
Most published research on telehealth services for ASD has been conducted in the past eight years and is based on pilot studies with small sample sizes and an absence of control groups. However, initial findings suggest that remote parent-training interventions can increase parents’ knowledge of best practices for facilitating their children’s learning (Hamad, Serna, Morrison, & Fleming, 2010; Ingersoll & Berger, 2015; Kobak, Stone, Wallace, Warren, Swanson, & Robson, 2011; Vismara et al., 2012; Wainer & Ingersoll, 2013; Wainer & Ingersoll, 2015), increase parents’ self-efficacy (Ingersoll et al., 2016; Nefdt, Koegel, Singer, & Gerber, 2010), and reduce parents’ stress (Ingersoll et al., 2016). As well, parent-mediated telehealth interventions have demonstrated the potential to increase children’s social communication (Vismara et al., 2012) and reduce their problem behavior (Lindgren et al., 2016; Wacker et al., 2013). Indeed, such improvements were observed following both self-directed and therapist-assisted telehealth interventions (Ingersoll et al., 2016). To date, there have not been any studies evaluating the acceptability or efficacy of a remote parent-training intervention for children with ASD in Albania. However, based on telehealth research in other countries, it is believed that telemedicine services can increase intervention access in middle-income countries and in rural regions, including in Albania (Latifi et al., 2015).
Limitations of Past Research
This emerging body of literature offers a promising way to capitalize on the growing popularity of technology worldwide in order to provide services to more families of children with ASD. While these initial studies have multiple strengths, they warrant replication and exploration of numerous other factors. Specifically, most of these studies have been conducted in high-resource countries, such as the United States and those in western Europe, and therefore we do not know whether these treatment practices are generalizable to other cultures and countries where parents may have less experience with technology and less prior exposure to information about ASD. Additionally, many online programs deliver intervention through real-time discussions between providers and parents (e.g., telehealth via videoconferencing) or provide therapist feedback based on video recordings of parent/child interactions. Therefore, many interventions to date have enabled parents to receive coaching from a trained professional and adapt their behavior accordingly. Additional research is necessary to understand the extent to which families are capable of understanding and implementing behavioral intervention based on text-based information and video demonstrations, without direct feedback following observation of parent-child interactions, or with only minimal communication with a trained provider. Finally, few parent-training studies included a control group. In the absence of such design rigor, numerous interpretive problems arise. Implicit and explicit demand characteristics associated with parental expectations of treatment effectiveness cannot be ruled out. In addition, pre- and post-treatment administration of assessments in the absence of control comparisons could mean that improvements after treatment reflect practice effects on the assessment measures or the effects of maturation.
Program Development
The current study is the first assessment of a home-based video PT program in Albania. The American Academy of Pediatrics suggests that intervention should include elements of accessibility, comprehensiveness, family centeredness, compassion, coordination, and affordability (AAP, 2002). Accordingly, the investigators created a free DVD program with supporting written materials that were designed to educate caregivers in basic behavioral and naturalistic teaching principles, and to enhance their use of these principles with their young children who have ASD.
The program incorporated successful elements from the broader PT literature, including the use of training modules, videos that demonstrate positive parenting behaviors, and video vignettes (Nieuwboer et al., 2013). The program also incorporated elements similar to some of those from among the most comprehensive ASD PT programs (e.g., enhancing communication, teaching pretend play, prompting and prompt fading, and contingent consequences; Ingersoll & Berger, 2015; Vismara, McCormick, Young, Nadhan, & Monlux, 2013). However, we expanded our program to review typical development in social, communication, and cognitive functioning from age one to age five, a review of concerning behaviors, Applied Behavior Analysis (ABA) strategies in greater depth, and fundamentals of the Picture Exchange Communication system (PECS; text approved by Dr. Andy Bondy). Finally, the program included modules based on skills that Albanian parents wanted to learn. Specifically, a Board Certified Behavioral Analyst (BCBA) held several meetings with parents, in which she asked for suggestions about aspects of child behavior would be most helpful to include in PT programs (none of these parents were included in the current study). The consensus was that toilet training, picky eating, and problem behavior would be particularly valuable.
The program was translated into Albanian and back-translated to English, with collaboration from Albanian co-investigators who were psychologists and psychiatrists with expertise in ASD. At the time of program development, there was no extant literature on Albanian parents’ preferences for content of PT programs, so we relied on the information collected from the parents and from our Albanian collaborators’ clinical experience. Interestingly, a recent paper reports on preferences of 148 parents of children with ASD living in South-East Europe. Findings demonstrated that parents sought PT programs that would provide general information about typical development and ASD, as well as strategies for enhancing communication in their children, toilet training, and handling problem behavior (Preece, Symeou, Stošić, Troshanska, Mavrou, Theodorou, & Škrinjar, 2017). Moreover, a majority of parents expressed the desire to learn about structured approaches, including ABA and PECS. Finally, almost all parents reported a desire for greater family involvement that extended beyond solely teaching parents, but instead allowed multiple caregivers (e.g., grandparents) to participate in learning strategies (Preece et al., 2017). Although this paper was not published at the time of our program development, these requests are consistent with the approaches taken in the PT program.
The PT program development began in 2014; at that time, less than 20 percent of the Albanian population had household access to the Internet (United Nations Statistics Division, 2018). The study staff in Albania felt that DVDs would be most appropriate in order to enable the greatest number of parents to access the training materials. A pediatrician and a psychiatrist narrated the video program text; video clips were interspersed to demonstrate the behaviors being taught. The video program was supplemented with several chapters of written text.
The program was based on both naturalistic and behavioral principles and instructed parents in evidence-based skill teaching and behavior management techniques. Initial modules taught parents to identify developmental concerns in their children and to apply ABA principles (e.g., contingent reinforcement, prompting, prompt fading, etc.). Subsequent modules provided guidance about ways to apply these behavioral principles to address target behaviors in their children (e.g., teaching language, facilitating pretend play, addressing problem behavior, etc.). Specific evidence-based training components are detailed in Table 1 and in the Measures section below.
Table 1.
Program Modules
| Module | Details | Format |
|---|---|---|
| 1. Expected Development | Expected language development, social interaction and thinking and self-help for children ages 12 to 60 months | Video – English videos with introductions in Albanian |
| 2. Basic Principles of Teaching | Principles of ABA, including reinforcement, how to choose rewards prompts, and prompt fading | Video – Primarily Albanian |
| 3. Choosing Skills To Teach and Breaking Skills into Smaller Parts | Eye contact, making requests, selection of functional and socially significant targets for teaching | Video – Primarily Albanian |
| 4. Picture Exchange Communication System (PECS) | Introduction to PECS, initiating communication and expanding the use of pictures | Video – Primarily Albanian |
| 5A. Teaching Children In The Context of Daily Routines | Teaching language, imitation, play, eye contact, social interaction during daily routines | Video – Primarily English, with introductions in Albanian |
| 5B. Teaching Games and Activities | Additional specific activities for waking up and going to sleep, diaper changing and dressing, meal time, learning during errands, chore time, bath time, indoor play, outdoor play, and music-themed play | Manual |
| 6A. Setting Up Special Learning Sessions | Learning to sit in the learning place and comply with simple instructions, imitating, matching, following instructions | Video – Primarily Albanian |
| 6B. Importance of Using Clear Instructions and the Concepts of Mastery and Generalization | Importance of giving clear instructions using simple language, how to measure mastery, and how to facilitate maintenance and generalization | Manual |
| 7. Teaching Pretend Play | Knowing when the child is ready to begin pretend play, choosing toys that encourage pretend play, one-step and multi-step play with your child, simple pretend play with an object as an actor | Manual |
| 8. Prevention and Handling of Problem Behavior | Crying and fussing as forms of communication, recognizing problem behavior, strategies for preventing problem behaviors, increasing cooperation, choosing battles wisely | Manual |
| 9. Picky Eating | When is picky eating a problem, how to handle normal picky eating, selecting new foods to introduce, a program to increase child's food repertoire, teaching children to use utensils | Manual |
| 10. Toilet Training | When is your child ready for toilet training?, toilet training during the day, planned "sitting", responding to accidents during training sessions, fading prompts | Manual |
As will be described below, the Albanian Children’s Center provided therapists who contacted families in the Treatment Group each week for brief phone calls, in order to respond to questions parents had about the program.
Current Study Aims
Since this was the first attempt to deliver such materials to parents in Albania, the primary purpose of the current study was to examine whether this video parent-training program would be judged as comprehensible and acceptable by parents. Secondary outcomes included exploration of whether the program would (1) increase parent knowledge from baseline to post-treatment (i.e., four months after baseline) in the Treatment Group, relative to the wait-list Control Group, as shown on a multiple-choice quiz, and (2) increase parental self-efficacy from baseline to post-treatment in the Treatment Group relative to the Control Group. The current study is the first, to our knowledge, to assess whether an electronic parent-training program, with limited guidance from a professional, can be rated as valuable by parents, and can increase knowledge and self-efficacy in parents of children with ASD who live in Albania.
Methods
Participants
Participants were recruited from three clinics located in the capital of Tirana and outside of Tirana. Parents were invited to participate in the current study if they had a child who was 18 to 70 months of age and had recently received a diagnosis of ASD or a provisional diagnosis of ASD based on an evaluation that included administration of the Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2000). Although ASD can be diagnosed earlier than 18 months, this was selected as the earliest eligible enrollment age to ensure that all program modules would be developmental appropriate for all children. This study was part of a larger study on screening and diagnosis in Albania (Brennan et al., 2016) funded by Autism Speaks.
Initial participants were 38 parent/child dyads (see Table 2). Parents of children with ASD or a provisional diagnosis of ASD were invited to participate in the current study. Participants were assigned to the Treatment Group or the wait-list Control Group by a U.S. researcher, who did not know any of the families. She was provided with each family’s child age and gender, recruitment site (three clinics), and maternal education. The Albanian collaborators informed the U.S. team that maternal age is a sensitive variable in Albania, and enough forms were missing maternal age that it was not possible to match on this variable. Families were assigned to the Treatment or Control Group in order to achieve the best match as follows: The first two clinics were in rural areas, while the third was in Tirana, and the three clinics tended to serve different socioeconomic strata. We therefore started by dividing the sample into the three clinic sources, and matched within clinics. We next matched on child’s age, then gender, and following that, on maternal education. As can be seen in Table 2, age was consistent across the three clinics, and as expected, the levels of maternal education were indeed higher in Tirana.
Table 2.
Initial Participant Characteristics
| Clinic 1 N=12 |
Clinic 2 N=8 |
Clinic 3 N=18 |
Total | |||||
|---|---|---|---|---|---|---|---|---|
| Control | Treatment | Control | Treatment | Control | Treatment | Control | Treatment | |
| Child Age (months): M (SD) | 49.83 | 50 | 48 | 47.25 | 48.56 | 46.33 | 48.84 | 47.68 |
| (8.11) | (8.76) | (11.40) | (23.92) | (12.36) | (11.30) | (10.41) | (13.43) | |
| Child Gender (% male) | 67% | 83% | 100% | 75% | 100% | 100% | 89% | 89% |
| Mother’s Education (%) | ||||||||
| Did not complete high school | 67% | 66% | 25% | 25% | 22% | 22% | 37% | 37% |
| Completed high school | 0% | 17% | 25% | 25% | 12% | 0% | 11% | 11% |
| Completed College | 33% | 0% | 25% | 25% | 44% | 56% | 37% | 32% |
| Advanced Degree | 0% | 17% | 25% | 25% | 22% | 22% | 15% | 20% |
Twenty-nine dyads completed the study. Children were 26 males and three females who were on average 47 months of age. Subsets of parents provided information about their age (n=25, M=33 years) and highest education level (n=29). Nine parents did not complete high school, three parents completed high school, and 17 earned a college or an advanced degree (See Table 3).
Table 3.
Demographics and Intervention History for Parents Who Completed the Study
| Control Group N=16 |
Treatment Group N=13 |
p | |
|---|---|---|---|
| Mother's Education (%) | .23 | ||
| Did not complete high school | 31% | 31% | |
| Completed high school | 0% | 23% | |
| Completed College | 44% | 23% | |
| Advanced Degree | 25% | 23% | |
| Mother's Age (years): M (SD) | 30.21 (3.79) | 35.91 (4.28) | <.01 |
| Child Age (months): M (SD) | 42.25 (11.05) | 48.77 (14.35) | .46 |
| Child Gender (%) | 85% male | 94% male | .57 |
| Intervention Hours Per Week at Baseline: M (SD) | 4.38 (1.70) | 4.46 (4.63) | .95 |
Note: Maternal education is presented as a percentage; Maternal age is presented in years; child’s age is presented in months; gender represents the percentage of males per group (treatment/control group); and intervention represents the average number of hours of intervention per group at baseline.
Of the nine participants who did not complete the study, six were in the Treatment group and three in the Control group, with one girl and eight boys. Three dyads moved and therefore could not complete the post-treatment measures (n=1 in the Treatment Group and n=2 in the Control Group), two children were felt by parents to be too high functioning to benefit from the intervention, (both in the Treatment Group), one parent “lost interest” in participating (Treatment Group), one mother experienced health concerns that prevented her from participating (Treatment Group), and two were lost to contact (n=1 in the Treatment Group and n=1 in the Control Group). We compared non-completers to those who completed the PT program and the post-treatment measures. Children’s age and gender did not differ. Of the non-completers, four mothers had not completed high school, two had completed high school, three had a Bachelor’s Degree and one had a Master’s Degree. Participants who completed the study were more educated, χ2 = 11.92, p < .05 (59% college graduates compared to 11% college graduates in the participants who did not complete the study) and had higher baseline quiz scores, t (36) = 2.20, p < .05, (Completed Participants M(SD) = 51.34% (11.79%); Dropped Participants M(SD) = 40.33% (16.88%)).
Procedure
A research assistant in Albania traveled to families’ homes at baseline, at which time parents completed three measures: the Early Intervention Parenting Self-Efficacy Scale (EIPSES, Guimond, Wilcox, & Lamorey, 2008), a quiz developed for this study to assess their knowledge of behavioral principles and teaching strategies, and a demographic form, which included information about the child’s therapy history and other family information including mother’s education and age.
The Treatment Group then received access to the DVD PT program. The research coordinators ensured that participants could access a DVD player at least a few times per week. Parents’ feedback about the program was elicited with the Treatment Evaluation Inventory Short Form (TEI-SF; Kelley, Heffer, Gresham, & Elliott, 1989). Specifically, parents were asked to complete the TEI-SF after they completed each module and to mail this form to the research coordinator.
A therapist trained in behavioral principles contacted the parents in the Treatment Group each week for a brief phone interview (up to 15 minutes). The ultimate goal of the program development is for the material to be usable without professional support when such support is not available, but without knowing how comprehensible the concepts were, we decided that this initial trial had to provide some telephone support, for ethical reasons. Therapists (a) asked whether parents reviewed a new PT module that week, (b) inquired about whether parents practiced newly learned intervention techniques during the week, and asked which ones they felt worked and which did not, (c) asked about any outside additional services the child received, and (d) confirmed that parents completed the TEI-SF that week; if they did not, therapists reminded parents to complete the form and mail it to the research coordinator. These calls were designed to be no more than 15 minutes, and in fact, the modules resulted in average length of calls that ranged from 6.8 to 10.5 minutes (M = 8.56 minutes, SD = 1.24 minutes). The Control Group did not engage in these calls, as they did not receive the training material and therefore would not have material to ask questions about. However, parents in the Control Group received brochures containing basic information about ASD and were told that they would be given access to instructional materials at the end of the waitlist period of four months. Children in both groups continued all other established treatment as usual.
Post-treatment (14-16 weeks after baseline), parents in both groups completed the EIPSES and the quiz a second time. After the second assessment, the parents in the Control Group were provided with access to all of the training material that the Treatment Group previously received. They also received a therapists’ contact information to address any questions about the training materials.
Measures
Video Program.
The video program comprised of six DVD modules, each 30 to 60 minutes long, and six chapters of written material (See Table 1). The videos included illustrative clips of ABA-based intervention. The DVDs and written material instructed parents in evidence-based teaching and behavior management techniques. Specifically, the training modules explained typical developmental milestones in cognition, language, and social interaction from birth to five years, and when to be concerned about their child’s development, basic principles of ABA (including prompting, contingent reinforcement, and prompt fading), picking functional targets such as eye contact and requesting, using pictures when needed for communication, embedding teaching into specific daily routines, preventing problem behavior, handling picky eating, and toilet training. The program integrated aspects of generalization in natural settings, focus on the child’s interests to increase motivation, joint attention, positive affect, natural consequences of behavior, communication, and the importance of the parent-child relationship.
The language of the text and video was kept as simple and non-technical as possible. For example, in places, “reward” was used instead of or alongside “reinforcement”, and “hints” instead of “prompts”. The training program was originally created by a licensed clinical psychologists with several decades of experience specializing in assessment and recommendations for children with ASD, a Board Certified Behavior Analyst Doctoral level with 25 years of experience in designing and supervising ABA programs and parent coaching for children with ASD, and a developmental-behavioral pediatrician. The program employed treatments that are most firmly based in empirical evidence. The innovation of the program lay in the comprehensibility of the content covered through use of non-technical language, the illustration of ABA and naturalistic techniques through illustrative videos, the translation of material to Albanian, and the adaptation of materials to be appropriate for Albanian culture. In addition, some existing remote PT programs focus on teaching or increasing the frequency of a specific skill (e.g., imitation or reinforcement and prompting). Valuable as are these specific foundational skills for children with ASD, the current program was designed to be comprehensive enough to teach parents the basic principles of ABA so that they could apply these techniques to help their children learn across a variety of skill areas.
A majority of the videos were filmed at the Albanian Children’s Foundation to maximize comprehensibility to the Albanian speaking populations in Eastern Europe; therapists at the Foundation had undergone several years of training in basic ABA by two American BCBAs who made multiple trips to Albania and continued training by Skype supervision. The remaining video segments were created in the United States; these included nonverbal videos or videos with little communication (e.g., a video to demonstrate gestures, such as pointing). An Albanian explanation preceded each video demonstration that included parent/child exchanges in English. Parents were encouraged to spend between two and three hours reviewing each section of the training and to implement the learned behavioral techniques in their everyday interactions with their children.
Demographic Form.
Parents completed a demographic form at baseline to indicate their age and level of education, and to report the child’s age, gender, and history of intervention for ASD.
Treatment Evaluation Inventory Short Form (TEI-SF; Kelly et al., 1989).
A 9-item version of the TEI-SF provided five-point Likert-scale items (1= strongly disagree, 2= disagree, 3= neutral, 4= agree, 5= strongly agree) to determine how useful parents perceived the training materials to be after each program module, and for the material as a whole. In addition, means were calculated by averaging parents’ ratings of all criteria for each module and by averaging responses across modules for each criteria (e.g., the likeability rating across all program modules) (see Table 4).
Table 4.
Mean TEI-SF Ratings for Each Item and Each Module
| Module | Acceptable (1) |
Willing to use (2) |
Child responded well (3) |
Like (4) |
Considered Effective (5) |
Long term improvement (6) |
Able to try out (7) |
Clear (8) | Overall Positive (9) |
Numeric Average of Module (criteria 1-8) |
|---|---|---|---|---|---|---|---|---|---|---|
| Basic Principles | 4.54 | 4.46 | 4.23 | 4.46 | 4.62 | 4.08 | 4.31 | 4.62 | 4.54 | 4.42 |
| Teaching Skills | 4.23 | 4.31 | 4.33 | 4.46 | 4.46 | 4.08 | 4.00 | 4.31 | 4.46 | 4.27 |
| PECS | 3.91 | 3.91 | 3.70 | 3.82 | 3.91 | 3.64 | 3.55 | 4.09 | 4.00 | 3.82 |
| Day In The Life | 4.69 | 4.54 | 4.38 | 4.62 | 4.46 | 4.31 | 4.31 | 4.50 | 4.62 | 4.48 |
| Learning Sessions | 4.54 | 4.38 | 4.46 | 4.38 | 4.54 | 4.54 | 4.23 | 4.69 | 4.62 | 4.47 |
| Pretend Play | 4.46 | 4.38 | 4.23 | 4.38 | 4.31 | 4.15 | 4.15 | 4.23 | 4.31 | 4.29 |
| Problem Behavior | 4.38 | 4.38 | 4.38 | 4.46 | 4.23 | 4.15 | 4.31 | 4.38 | 4.38 | 4.33 |
| Picky Eating | 4.27 | 4.36 | 4.00 | 4.45 | 4.36 | 4.36 | 4.09 | 4.36 | 4.27 | 4.28 |
| Toilet Training | 4.50 | 4.30 | 4.30 | 4.40 | 4.50 | 4.10 | 4.10 | 4.60 | 4.60 | 4.35 |
| Overall Program Rating | 4.25 | 4.42 | 4.42 | 4.58 | 4.42 | 4.33 | 4.25 | 4.67 | 4.50 | 4.42 |
| Numeric average of each TEI-SF Criteria | 4.38 | 4.34 | 4.24 | 4.40 | 4.38 | 4.17 | 4.13 | 4.45 | 4.43 | 4.31 |
Parent Quiz.
The study investigators created a multiple choice, 31-item quiz to assess mastery of the instructional material (as in Hamad et al., 2010, Kobak et al., 2011, and Wainer and Ingersoll, 2015), with four answer choices for each question, one of them being correct. Items were based directly on the PT program (i.e., the video and textual material). The aim was to create a quiz with a spread of easy to difficult items, with greater than chance baseline responding, but low enough to leave room for significant improvement with learning. The quiz was created by an author who has extensive experience creating quizzes, including for a professional board certification program. The quiz was pretested on 20 adult females, of whom 8 were ABA supervisees with the remaining naïve to ABA. The overall score on the quiz was 64 percent correct. The ABA supervisees had an average score of 84 percent correct, while the naive participants had an average score of 51 percent. Of individual items, there were eight difficult (35-55 percent correct), 12 medium (60-75 percent correct) and 11 easy (80-95 percent correct). Following are two examples of quiz items:
1. You have just started to teach your child how to request things. You are in the grocery store, and your child wants a cookie from the box you just put in the shopping cart. He is starting to get upset and cry. What is the best thing to do?
Place the cookie box back on in the shelf and tell him he cannot have any.
Give him a cookie to prevent him from getting more upset.
Help him point to the box then explain that he can have one when you leave the store.
Help him to point at the box, and then give him a little piece of a cookie.
2. Your child is lying on the floor spinning the wheels of a toy car and staring at them. A good thing to do might be to:
allow the child to continue since he is happy with the toy.
scold him for not playing nicely.
take the toy car away.
bring another toy car and help him race his car with yours.
Parents completed the quiz at baseline and post program. The investigators calculated each parent’s score as a percent correct of all 31 items.
Early Intervention Parenting Self-Efficacy Scale (EIPSES; Guimond et al., 2008).
The EIPSES is a brief self-efficacy measure, with adequate convergent and discriminant validity. The EIPSES assessed individuals’ perceptions of their competence as parents and of the modifiability of child outcomes, at baseline and post-treatment. We used a revised version of the EIPSES, which included 10 items on a five-point Likert Scale (1= strongly disagree, 2= disagree, 3= neutral, 4= agree, 5= strongly agree). Items four, five, and eight were reverse coded. Responses were averaged across items to produce a single self-efficacy score at baseline, and post-treatment.
All materials were written in English, and adapted by first being translated into Albanian, followed by back-translation into English, at which point the two English versions were compared. The translation of the original English material into Albanian was carried out by two bilingual, Albanian ABA therapists and then back-translated by a professional translator. The back-translation was then reviewed by a bilingual child psychiatrist. A highly experienced Board Certified Behavioral Analyst reviewed the back-translation in consultation with the bilingual child psychiatrist and Albanian ABA therapists via Skype to resolve any discrepancies.
Analytic Plan
Demographics.
The groups were well matched at the beginning of the study. In order to see whether parents who completed the study differed by group, Treatment and Control groups were compared on demographic factors at the conclusion of their participation, including child’s age, child’s gender, mother’s level of education, and mother’s age. Groups were also compared on the number of intervention hours the child had been receiving at baseline. Independent t-tests were performed to analyze continuous variables and Fisher’s Exact tests and chi-square tests of independence were used to examine categorical data.
Primary Outcome
TEI-SF.
Treatment Group parents rated each module based on eight items and an overall rating. Averages were derived for each module, and for each item to assess the overall acceptability of the material and the parents’judgments of various aspects of the material.
Secondary Outcomes
Parent Quiz.
To determine whether group membership influenced parents’ knowledge about teaching and behavior management techniques, we conducted a repeated measures ANOVA. Assumptions about repeated measures ANOVA were satisfied. Histograms revealed that parents’ quiz scores at baseline and post-treatment were normally distributed.
EIPSES.
Similarly, in accordance with the paper that describes the development of the EIPSES (Guimond et al., 2008), we explored participants’ mean responses. A repeated measures ANOVA assessed whether groups differed in self-efficacy at baseline and post-treatment. Histograms revealed that parents’ self-efficacy scores were normally distributed at baseline and post-treatment. As this was an exploratory analysis, we also looked at each EIPSES item to evaluate whether the parent-training program influenced certain self-efficacy items more than others. Change scores were calculated for each item and then compared by group. A Bonferroni correction was used for item level analyses to reduce the potential for Type I errors due to multiple comparisons; a cut-off of α = .0025 (i.e., p = .005/10 EIPSES items) was set for these analyses.
Statistical analyses were performed using IBM SPSS Statistics for Windows, Version 22.0 (IBM Corp., 2013).
Results
The following results are presented for parent/child dyads who completed the program. Groups did not differ on child gender (p = .57, Fisher’s Exact test) child age, t (27) = −.75, p = .46, or maternal education (p = .23, Fisher’s Exact test) (69% of Control parents and 46% of the Treatment parents had completed college). Children in both groups received a similar number of intervention hours at baseline, t (27) = −.07, p = .95 (Control Group M = 4.38, SD = 1.70, hours per week; Treatment Group M = 4.46, SD = 4.63, hours per week) (See Table 3.) None of the parents had received training in ABA at baseline.
Primary Outcome
On the TEI-SF, parents in the Treatment Group valued the video intervention and rated the overall program highly (M = 4.43 on 5-point scale). Overall, parents felt that the intervention was acceptable, clear, effective, and led to long-term improvement. Parents also reported that they were willing to use the intervention and that their children responded well (see Table 4). When asked about specific modules, parents rated all modules highly (see Table 4). The only module that received an average score lower than 4.0 was the module on Picture Exchange Communication System (PECS). Comments indicated that parents felt that creating the necessary pictures for PECS, and carrying them everywhere, was too time consuming and difficult. Additionally, some parents reported that their children communicated with gestures or words and parents felt that communication facilitated by pictures would hinder their children’s progress and disrupt their more effective communication strategies, despite information to the contrary that was included in the PT material. Modules with the highest ratings (overall rating > 4.5) were basic principles of teaching, day in the life (incorporating teaching into daily routines), how to set up learning sessions, and toilet training.
Secondary Outcomes
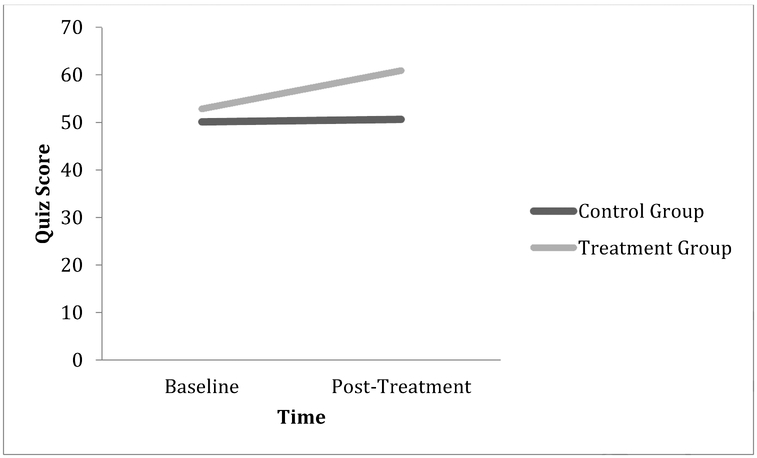
With regard to parental knowledge, the two groups’ quiz scores were very similar at baseline (Control Group M = 50.13, Treatment Group M = 50.63). Post-treatment, parent scores in the Treatment Group increased by eight points, on average, and Control Group parents’ mean score remained as they were at baseline (See Table 5 and Figure 1). Although the Group by quiz interaction, (F(1,27) = 2.12, p = .16, ηp2 = .07), did not reach significance, there was a medium effect size, suggesting that the change in quiz score from baseline to post-treatment differed for parents in the Treatment and Control Groups and significance was limited by the small sample.
Table 5.
Average quiz percent correct and self-efficacy scores by group and time point
| Control Group | Treatment Group | p | ||
|---|---|---|---|---|
| M (SD) | M (SD) | |||
| Quiz | Baseline | 50.13 (13.95) | 52.85 (8.74) | 0.16 |
| Post-Treatment | 50.63 (13.73) | 60.87 (15.98) | ||
| Self-Efficacy | Baseline | 3.57 (.40) | 3.79 (.54) | 0.77 |
| Post-Treatment | 3.89 (.45) | 3.97 (.45) |
Figure 1.
Quiz Scores by Group and Time
To explore whether Group influenced the change in parents’ self-efficacy ratings from baseline to post-treatment, a repeated-measures ANOVA was conducted with the overall EIPSES rating as a within-subjects factor and Group as a between-subjects factor. As shown in Table 5, there was no interaction between Group and EIPSES scores, (F(1,27) = .09, p = .77, ηp2 = .003), suggesting that groups did not significantly differ in their change in EIPSES scores from baseline to post-treatment.
Item-level data were also examined, and suggest that parents in the Treatment Group became more confident in their parenting abilities post-intervention, while the Control Group became less confident over time F(1,26) = 9.48, p = .005, ηp2 = .27), with a large effect size (see Table 6).
Table 6.
EIPSES item-level average change scores by group
| Item | Control Group |
Treatment Group |
p |
|---|---|---|---|
| 1. If my child is having problems, I would be able to think of some ways to help my child | −0.07 | 0.69 | 0.13 |
| 2. When my child shows improvement, it is because I am able to make a difference in my child's development | 0.38 | 0.54 | 0.75 |
| 3. If a professional working with my child had difficulty, I would be able to offer some useful suggestions | 0.25 | 0.62 | 0.33 |
| 4. Children will make the most progress if a professional rather than a parent works with them | 0.13 | 0 | 0.76 |
| 5. Even a good parent may not have much impact on whether children make progress in their development | 0.19 | 0.15 | 0.96 |
| 6. If my child learns something quickly, it would probably be because I've done a good job teaching him | 0.31 | 0.23 | 0.84 |
| 7. On most days, I can handle most of the ups and downs of being a parent | 0.38 | 0.67 | 0.46 |
| 8. I worry that I am not a good enough parent due to outside demands placed upon my time and energy | −1 | 0.54 | .005 |
| 9. Over the past six months, I can see the progress that I have made in becoming a better parent | −0.07 | 0.62 | 0.09 |
| 10. Whether a child is born with a disability or not, the child's parents can still do a lot to help him/her | 0.25 | 0.15 | 0.73 |
Note: Items 4, 5, and 8 are reverse coded.
Discussion
The current study aimed to evaluate a video parent-training program for families of children with ASD in Albania. Specifically, we assessed whether parents in the Treatment Group understood and valued the program. In addition, we compared the Treatment Group to a Control Group (matched on child gender, child age, and parental education) on knowledge about teaching principles for children with ASD and on parenting self-efficacy to determine whether the PT program influenced these outcomes.
Participants in the Treatment Group appraised the program very highly. This result was comparable to other studies that have evaluated video parent-training programs (e.g., Nefdt et al., 2010). Interestingly, many remote intervention studies for parents of children with ASD demonstrate that although parents value the interventions, the technological component (e.g., operational and connectivity difficulties, lack of required equipment/software, and discomfort with technology) cause frustrations for parents (Ashburner, Vickerstaff, Beetge, & Copley, 2016; Baharav& Reiser, 2010; Vismara et al., 2012) and in some cases lead parents to decline participation (Salomone, & Maurizio Arduino, 2017). Parents in the present study did not express such technological reservations, owing perhaps to the relative simplicity and familiarity of the study’s DVD and text-based format, and the support by telephone. Since remote intervention has been presented as a promising way to reduce the burden of treatment and provide support to families with limited intervention access, it is important that remote programs are accessible to all parents and rely on technology that is readily available or can be easily and affordably provided to families. This is particularly important for future research to consider because necessary technology for remote programs, and comfort with such equipment, is likely to be particularly limited in low-resource areas. Unmet, this challenge has the potential to perpetuate the current inequitable access to services.
Parents in the present study especially valued the material on basic principles, day in the life (incorporating teaching into daily routines), how to set up learning sessions, and toilet training modules. These modules delivered strategies for reinforcing and scaffolding skills, as well as helping children develop language, social interaction, compliance, and toilet training. Overall, parents reported that children were most compliant with instructions from these modules. Parents least appreciated the PECS, pretend play, and picky eating modules, which emphasized using pictures to facilitate communication, choosing toys to encourage pretend play, and handling picky eating. Parents reported that the preparation of pictures necessary for PECS was too time consuming and in certain cases, parents felt that it was not relevant to their children who were already communicating in a different way.
Although we received Dr. Bondy’s approval to include the basics of PECS in the training program, the decision to only incorporate part of the manualised treatment may have compromised fidelity and contributed to parents’ reduced enthusiasm for this module. The PECS module was included as a relevant resource for non-verbal children and parents were provided with resources (books and websites) so that they could access the remainder of the PECS material post-program, if they chose to learn more. Regarding pretend play, some parents were not able to effectively implement recommended strategies because their children were not interested in play or “did not understand” the play prompts. Finally, although some parents liked the suggestions for managing their children’s picky eating, others reported that their children did not adapt to the new strategies and continued to cry or refuse to eat specific foods.
In response to parent reservations about these modules, we plan to emphasize that: (a) using PECS is an optional component, and should be used if the child does not have another effective means of communication, (b) pretend play requires a minimum level of cognitive and social skills, and that if the child is not yet interested in play, it should be returned to at a later time, and (c) children with ASD can find trying new foods very frightening or unpleasant (Provost, Crowe, Osbourn, McClain, & Skipper, 2010; Williams, Dalrymple, & Neal, 2000) and parents should return to this module at a later date if their child continues to show distress at being encouraged to try new foods. The item with the highest overall rating was that the material was “clear”, suggesting that the attempt to describe behavioral techniques in non-technical language was successful.
Regarding the secondary outcome variables, while participants in both groups had almost identical scores on the quiz about teaching principles at baseline, the Treatment Group improved by eight points, on average, while the Control Group’s scores were unchanged post-treatment. Although this difference was not statistically significant, the medium effect size suggests that the lack of significance may reflect the compromised power associated with the small sample size. In addition, the quiz was administered post-treatment (i.e., 4 months after baseline), so parents were required to remember some of the learned information (i.e., from initial modules) for four months. It is possible that larger effects would have been observed if quizzes were administered immediately following the conclusion of each intervention module. Given that other remote intervention outcome studies have found significant increases in parents’ knowledge post-treatment (Hamad et al., 2010; Kobak et al., 2011; Wainer & Ingersoll, 2013), it will be useful to evaluate the present approach with a larger sample.
Finally, Group did not differentially influence parent’s reported overall self-efficacy. Item-level analyses demonstrate that parents in the Treatment Group felt that they were better parents posttreatment than parents in the Control Group. Specifically, Control Group parents’ confidence diminished post-treatment, while Treatment Group parents’ confidence increased, with a large effect. The result for this item is consistent with other video parent-training programs that have been shown to increase parents’ self-efficacy (Nefdt et al., 2010). It is possible that parents in the Control Group attempted alternative teaching strategies with their children and became increasingly discouraged when their children did not progress in a developmental appropriate pace. Overall, the medium-to-large effect sizes observed, even on some items that did not significantly differ significantly between groups (e.g., item 1, ηp2 = .08 and item 9, ηp2 = .10; see Table 6) suggest that such PT programs, with very limited time and input from clinicians, may increase aspects of self-efficacy and knowledge of optimal teaching strategies in parents of children with ASD.
The current study expands upon previous studies investigating video parent-training programs for parents of children with ASD in several ways. This is the first remote intervention study for parents of children with ASD who live in Albania. Most of the video and telehealth PT studies for families of children with ASD have been conducted in the United States and in Western Europe, which limits generalizability to low- and middle-income countries (Fairburn & Patel, 2014). It is crucial to expand this work to settings with a demonstrated gap in ASD intervention, such as other low-resource countries internationally as well as low-resource areas within the U.S. Additionally, most remote parent-training studies deliver intervention through real-time interaction with parents (e.g., telehealth) or provide therapist feedback based on video recordings of parent/child interactions (e.g. Green et al., 2010; Poslawsky, Naber, Bakermans-Kranenburg, van Daalen, van Engeland, & van IJzendoorn, 2015). Therefore, many remote parent-training interventions to date that use technology have enabled parents to receive coaching from a trained professional and to adapt their behavior accordingly. Since remote intervention is often proposed as a way to reduce the cost of therapy and to overcome the barrier of a shortage of providers, additional research is needed to understand the efficacy of parent-training programs that include brief contact with a therapist. This is particularly warranted since initial data suggests that parents can achieve fidelity and increase knowledge after self-directed telehealth and video programs (Hamad et al., 2010; Kobak et al., 2011; Nefdt et al., 2010; Wainer & Ingersoll, 2013). Some studies that compared self-directed and therapist-assisted programs found that change in parents’ knowledge was comparable in the two groups (Ingersoll & Berger, 2015). Others reported that parents who interacted with therapists remotely achieved greater fidelity than the self-directed group (Ingersoll et al., 2016). Additional research is necessary to understand the extent to which families are capable of understanding and implementing behavioral intervention based exclusively on text-based materials and video demonstrations, without direct feedback from a trained provider about their implementation of learned techniques. We included the brief weekly contact with therapists mainly for ethical reasons, so that parents would have someone to consult with before trying to implement a strategy that they may not understand. However, many parent-mediated intervention programs rely on weekly meetings with therapists of up to several hours; it may be that even if brief contact with therapists is needed, this will be more economically feasible than more intense supervision. Finally, few prior studies of remote parent training have included a control group.
Limitations and Future Directions
Several limitations of the present study merit consideration. First, parents in the Treatment Group engaged in weekly 15-minute debriefing interviews with a therapist. Although the video intervention was designed as a self-directed PT program, we elected to have support available, in the form of brief phone calls, when the intervention was first tried, in order to avoid possible harm to children if parents did not comprehend the material. These phone calls were structured and were brief, as noted above. Still, it is possible that the high appraisal of the training program and the benefits derived by the Treatment Group were influenced by these phone calls, as caregivers in the Control Group did not receive weekly phone calls from therapists. Future work should determine whether parents are able to successfully complete this program without any interaction with a professional.
Second, given the nature of this pilot study, the sample size was small, which limits both power and generalizability. Relatedly, the current study had a high dropout rate, which may have influenced results. This dropout rate is consistent with some other self-directed PT studies for ASD (e.g., Hamad et al., 2010). Participants who dropped out had lower levels of education and lower quiz scores at baseline. This suggests that interventions that are predominantly self-directed have to be designed with input from parents of lower education levels in order to maximize their utility to parents of different backgrounds. It also suggests that predominately self-directed interventions may be better suited for parents with higher education levels. However, additional information is needed to characterize the sample of parents who are not completing such interventions. Future studies with larger sample sizes should build a follow-up process such as an exit interview into consent, as this can be a valuable method of obtaining additional information from families who dropped out of the intervention in order to understand ways to improve future programs.
Third, our sample is more educated than the typical population in Albania, which could limit generalizability. Although 97 percent of adults in Albania are literate, and 82 percent complete secondary education, only 21 percent obtain a higher degree (UNICEF, 2013), relative to the 59 percent in our sample. As aforementioned, the education attainment in our sample was partially inflated because majority of the individuals who withdrew from the study did not have a college degree. Additionally, caregivers with higher socioeconomic status were more likely to live in or near Tirana and therefore had higher changes of participating in the present study.
Fourth, we did not include a measure of time parents spent reviewing each program module. An important next step is to evaluate how much time parents are willing and able to devote to reviewing training materials and practicing these strategies with their children. In a current study, parents are provided with a diary and are asked to track engagement with the material.
Fifth, like many remote parent-training interventions, this feasibility study did not include assessments to determine whether changes in parent training corresponded to any changes in children’s abilities or reduction of ASD symptoms. As remote self-directed PT for ASD remains a clinically significant but underdeveloped area of research, future studies should assess to what extent parent training influences child outcomes, and whether this is related to parents’ perceptions of the quality of the program, the amount of time they invest in the program, and their own improvement in variables such as self-efficacy and knowledge about teaching strategies.
Finally, the program text stressed that if a skill seems too difficult or children are distressed when parents practice program strategies, parents should return to the module at a later time. However, there are several factors that could contribute to children not responding positively to the intervention strategies (e.g., parents implementing strategies incorrectly (Wainer & Ingersoll, 2013), children requiring more intensive services, or parents lacking engagement with the intervention (Axford, Lehtonen, Kaoukji, Tobin, & Berry, 2012). Although self-directed interventions are less time consuming for therapists, and are therefore more accessible for families, a weakness of such programs is that parents do not benefit from feedback from a trained observer. Without knowing how parents were implementing strategies, we decided to include program text that encouraged parents to skip modules that were causing their children distress, rather than suggesting that parents persist and risk causing harm to their children.
The study investigators are currently building upon this study to conduct larger-scale PT studies that will observe the effect of a web-based program (content will be the same as the content described in the current program) on parent knowledge and self-efficacy, directly observed parent ability to teach the child, and child behavior and skill acquisition. These studies will also explore they way that child and family characteristics may influence the success of remote parent-training programs. Such work would eventually enable us to tailor programs to families and to help caregivers decide which modules are currently appropriate and which they should revisit at a future date. Future research on such PT programs is necessary both in Albania and in other geographical regions.
Conclusion
Overall, these findings suggest that the video program, with a minimal therapist assisted component, had high value and acceptability to parents of children with ASD in Albania. As well, the program increased parent’s knowledge from baseline to post-treatment more than treatment as usual received by the wait-list Control Group. This difference was not significant, however it may be clinically meaningful and the medium effect size suggests that it may have approached significance with greater power.
While the program did not influence parents’ overall self-efficacy, it led to increases in parents’ confidence in their own knowledge and parenting abilities, while the wait-list control parents experienced a decline in their confidence over time. This positive result is consistent with previous literature.
Overall, initial results of this program are promising and suggest that future research with a larger sample size is warranted. In light of the importance of early intervention that includes parents, and the profound scarcity of available resources, particularly in low-resource areas, this program may provide a promising means of increasing access to intervention for underserved families in Albania. If future research continues to demonstrate the efficacy of this PT program, this program could also be useful for Albanian-speaking families in other countries. This video training may be used by parents who are on waitlists for traditional services or by parents who wish to supplement traditional concurrent intervention. Finally, since parents are often concerned that they do not have any helpful resources before their child receives a formal diagnosis (Pickard, Wainer, Bailey, & Ingersoll, 2016), this video PT could be accessed by parents at the time of their first concern about their child. This would have the potential to reduce parental frustration with barriers to services, and to lead to positive changes in parent outcomes.
Highlights.
-
-
A novel, video-based parent-training program was developed in Albanian for parents of young children with ASD.
-
-
The program incorporated elements similar to some of those from among the most comprehensive parent-training programs (e.g., enhancing communication, teaching pretend play, prompting and prompt fading, contingent consequences) but was expanded to review typical development and when to be concerned, Applied Behavior Analysis strategies in greater depth and detail, Picture Exchange Communication System (approved by Dr. Andy Bondy), and to include specific techniques addressing additional areas of development, such as toilet training, picky eating, and problem behavior.
-
-
Parents of children with ASD in Albania rated this training program as enjoyable and valuable.
-
-
The program modestly increased an aspect of self-efficacy as well as parents’ knowledge of effective teaching strategies. Although the change in quiz score from baseline to post-program did not significantly differ by group (i.e., Treatment and Control groups), the medium effect size and average difference of eight points suggests that the program may be effective. Additional research with larger sample sizes is warranted.
Acknowledgements
The authors wish to extend our deep appreciation to the children and families who participated in the filming and in the pilot trial of this material, as well as the highly committed staff of the Albanian Children’s Foundation. We express special gratitude to Dr. Liri Berisha, who founded and led the Albanian Children’s Foundation and who made the study possible. The authors also acknowledge the following funding sources: the National Institute of Mental Health R34 “Teaching Skills to Toddlers: a Program for Caregivers” R34MH091208 (D. Fein, PI) for development of the PT material, and a grant from the Autism Speaks Global Autism Public Health Initiative (Screening, Diagnosis and Parent Training for Young Children with ASD in Albania), of which this study was a part, with leadership by Andy Shih, which supported the translation, adaptation, and production of DVDs in Albania.
Footnotes
Conflicts of Interest
Ariel Como and Iris Rathwell received consulting fees from this grant. All authors declare that they have no potential or competing conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants in the study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Academy of Pediatrics (2007). Management of children with autism spectrum disorder. Pediatrics, 120, 1162–1182. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics, Policy Statement (2002). The Medical Home. Pediatrics, 110(1), 184–187.12093969 [Google Scholar]
- Anderson DK, Liang JW, & Lord C (2014). Predicting young adult outcome among more and less cognitively able individuals with autism spectrum disorders. Journal of Child Psychology and Psychiatry, 55(5), 485–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashburner J, Vickerstaff S, Beetge J, & Copley J (2016). Remote versus face-to-face delivery of early intervention programs for children with autism spectrum disorders: Perceptions of rural families and service providers. Research in Autism Spectrum Disorders, 23, 1–14. doi: 10.1016/j.rasd.2015.11.011 [DOI] [Google Scholar]
- Axford N, Lehtonen M, Kaoukji D, Tobin K, & Berry V (2012). Engaging parents in parenting programs: Lessons from research and practice. Children and Youth Services Review, 34(10), 2061–2071. [Google Scholar]
- Bahadourian AJ, & Greer RD (2005). CABAS parent education: Increasing child compliance via parental emission of unflawed commands and contingent consequations during play. Journal of Early and Intensive Behavior Intervention, 2(3), 213. [Google Scholar]
- Baharav E, & Reiser C (2010). Using telepractice in parent training in early autism. Telemedicine and E-Health, 16(6), 727–731. doi: 10.1089/tmj.2010.0029 [DOI] [PubMed] [Google Scholar]
- Bal VH, Kim S, Cheong D, & Lord C (2015). Daily living skills in individuals with autism spectrum disorder from 2 to 21 years of age. Autism, 19(7), 774–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan L, Fein D, Como A, Rathwell IC, & Chen CM (2016). Use of the Modified Checklist for Autism, Revised with Follow Up-Albanian to Screen for ASD in Albania. Journal of autism and developmental disorders, 46(11), 3392–3407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2017). Autism Spectrum Disorder. Retrieved from https://wwwi.cdc.gov/ncbddd/autism/data.html
- Chiri G, & Warfield ME (2012). Unmet need and problems accessing core health care services for children with autism spectrum disorder. Maternal and Child Health Journal, 16(5), 1081–1091. [DOI] [PubMed] [Google Scholar]
- Daniels AM, Como A, Hergüner S, Kostadinova K, Stosic J, & Shih A (2017). Autism in southeast Europe: A survey of caregivers of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 1–12. [DOI] [PubMed] [Google Scholar]
- Dawson G (2008). Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Development and Psychopathology, 20(3), 775–803. [DOI] [PubMed] [Google Scholar]
- Deitz DK, Cook RF, Billings DW, & Hendrickson A (2008). Brief report: a web-based mental health program: reaching parents at work. Journal of Pediatric Psychology, 34(5), 488–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, & Patel V (2014). The global dissemination of psychological treatments: a road map for research and practice. American Journal of Psychiatry, 171(5), 495–498. [DOI] [PubMed] [Google Scholar]
- Glascoe F (1999). The value of parents’ concerns to detect and address developmental and behavioural problems. Journal of Paediatrics and Child Health, 35(1), 1–8. [Google Scholar]
- Green J, Charman T, McConachie H, Aldred C, Slonims V, Howlin P, … Byford S (2010). Parent-mediated communication-focused treatment in children with autism (PACT): A randomized controlled trial. The Lancet, 375(9732), 2152–2160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guimond AB, Wilcox MJ, & Lamorey SG (2008). The Early Intervention Parenting Self-Efficacy Scale (EIPSES) scale construction and initial psychometric evidence. Journal of Early Intervention, 30(4), 295–320. [Google Scholar]
- Hamad CD, Serna RW, Morrison L, & Fleming R (2010). Extending the reach of early intervention training for practitioners: A preliminary investigation of an online curriculum for teaching behavioral intervention knowledge in autism to families and service providers. Infants & Young Children, 23(3), 195–208. doi: 10.1097/IYC.0b013e3181e32d5e [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hume K, Bellini S, & Pratt C (2005). The usage and perceived outcomes of early intervention and early childhood programs for young children with autism spectrum disorder. Topics in Early Childhood Special Education, 25(4), 195–207. [Google Scholar]
- Hurtb J, Shaw E, Izeman SG, Whaley K, & Rogers SJ (1999). Areas of agreement about effective practices among programs serving young children with autism spectrum disorders. Infants & Young Children, 12(2), 17–26. [Google Scholar]
- Ingersoll B, & Berger NI (2015). Parent engagement with a telehealth-based parent-mediated intervention program for children with autism spectrum disorders: Predictors of program use and parent outcomes. Journal of Medical Internet Research, 17(10) doi: 10.2196/jmir.4913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll B, Wainer AL, Berger NI, Pickard KE, & Bonter N (2016). Comparison of a self-directed and therapist-assisted telehealth parent-mediated intervention for children with ASD: A pilot RCT. Journal of Autism and Developmental Disorders, 46(7), 2275–2284. doi: 10.1007/s10803-016-2755-z [DOI] [PubMed] [Google Scholar]
- Institute of Statistics, Institute of Public Health [Albania] and ICF Macro. (2010). Albania Demographic and Health Survey 2008-09. Tirana, Albania: Institute of Statistics, Institute of Public Health and ICF Macro. [Google Scholar]
- Kasari C, Gulsrud A, Paparella T, Hellemann G, & Berry K (2015). Randomized comparative efficacy study of parent-mediated interventions for toddlers with autism. Journal of consulting and clinical psychology, 83(3), 554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keen D, Couzens D, Muspratt S, & Rodger S (2010). The effects of a parent-focused intervention for children with a recent diagnosis of autism spectrum disorder on parenting stress and competence. Research in Autism Spectrum Disorders, 4(2), 229–241. [Google Scholar]
- Kelley ML, Heffer RW, Gresham FM, & Elliott SN (1989). Development of a modified treatment evaluation inventory. Journal of Psychopathology and Behavioral Assessment, 11(3), 235–247. [Google Scholar]
- Kobak KA, Stone WL, Wallace E, Warren Z, Swanson A, & Robson K (2011). A web-based tutorial for parents of young children with autism: Results from a pilot study. Telemedicine and E-Health, 17(10), 804–808. doi: 10.1089/tmj.2011.0060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohler FW (1999). Examining the services received by young children with autism and their families: A survey of parent responses. Focus on Autism and Other Developmental Disabilities, 14(3), 150–158. [Google Scholar]
- Krauss MW, Gulley S, Sciegaj M, & Wells N (2003). Access to specialty medical care for children with mental retardation, autism, and other special health care needs. Mental Retardation, 41(5), 329–339. [DOI] [PubMed] [Google Scholar]
- Latifi R, Dasho E, Shatri Z, Tilley E, Osmani KL, Doarn CR, Dogjani A, Olldashi F, Kociraj A, & Merrell RC (2015). Telemedicine as an innovative model for rebuilding medical systems in developing countries through multipartnership collaboration: The case of Albania. Telemedicine and e-Health, 21(6), 503–509 [DOI] [PubMed] [Google Scholar]
- Lindgren S, Wacker D, Suess A, Schieltz K, Pelzel K, Kopelman T, … Waldron D (2016). Telehealth and autism: Treating challenging behavior at lower cost. Pediatrics, 137 Suppl 2, S167–75. doi: 10.1542/peds.2015-2851O [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liptak GS, Benzoni LB, Mruzek DW, Nolan KW, Thingvoll MA, Wade CM, & Fryer GE (2008). Disparities in diagnosis and access to health services for children with autism: data from the National Survey of Children's Health. Journal of Developmental & Behavioral Pediatrics, 29(3), 152–160. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, DiLavore PC, … & Rutter M (2000). The Autism Diagnostic Observation Schedule—Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of autism and developmental disorders, 30(3), 205–223. [PubMed] [Google Scholar]
- MacDonald R, Parry-Cruwys D, Dupere S, & Ahearn W (2014). Assessing progress and outcome of early intensive behavioral intervention for toddlers with autism. Research in Developmental Disabilities, 35(12), 3632–3644. [DOI] [PubMed] [Google Scholar]
- Mansell W, & Morris K (2004). A survey of parents’ reactions to the diagnosis of an autistic spectrum disorder by a local service: Access to information and use of services. Autism, 8(4), 387–407. [DOI] [PubMed] [Google Scholar]
- Nefdt N, Koegel R, Singer G, & Gerber M (2010). The use of a self-directed learning program to provide introductory training in pivotal response treatment to parents of children with autism. Journal of Positive Behavior Interventions, 12(1), 23–32. doi: 10.1177/1098300709334796 [DOI] [Google Scholar]
- Nieuwboer CC, Fukkink RG, & Hermanns JM (2013). Online programs as tools to improve parenting: A meta-analytic review. Children and Youth Services Review, 35(11), 1823–1829. [Google Scholar]
- Orinstein AJ, Helt M, Troyb E, Tyson KE, Barton ML, Eigsti IM, … Fein DA (2014). Intervention for optimal outcome in children and adolescents with a history of autism. Journal of Developmental and Behavioral Pediatrics: JDBP, 35(4), 247–256. doi: 10.1097/DBP.0000000000000037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozonoff S, & Cathcart K (1998). Effectiveness of a home program intervention for young children with autism. Journal of Autism and Developmental Disorders, 28(1), 25–32. [DOI] [PubMed] [Google Scholar]
- Pickard KE, Wainer AL, Bailey KM, & Ingersoll BR (2016). A mixed-method evaluation of the feasibility and acceptability of a telehealth-based parent-mediated intervention for children with autism spectrum disorder. Autism, 20(7), 845–855. doi: 10.1177/1362361315614496 [DOI] [PubMed] [Google Scholar]
- Poslawsky IE, Naber FB, Bakermans-Kranenburg MJ, van Daalen E, van Engeland H, & van IJzendoorn MH (2015). Video-feedback intervention to promote positive parenting adapted to autism (VIPP-AUTI): A randomized controlled trial. Autism, 19(5), 588–603. [DOI] [PubMed] [Google Scholar]
- Preece D, Symeou L, Stošić J, Troshanska J, Mavrou K, Theodorou E, & Frey Škrinjar J (2017). Accessing parental perspectives to inform the development of parent training in autism in southeastern Europe. European Journal of Special Needs Education, 32(2), 252–269. [Google Scholar]
- Provost B, Crowe TK, Osbourn PL, McClain C, & Skipper BJ (2010). Mealtime behaviors of preschool children: Comparison of children with autism spectrum disorder and children with typical development. Physical & Occupational Therapy in Pediatrics, 30(3), 220–233. [DOI] [PubMed] [Google Scholar]
- Rocha ML, Schreibman L, & Stahmer AC (2007). Effectiveness of training parents to teach joint attention in children with autism. Journal of Early Intervention, 29(2), 154–172. [Google Scholar]
- Rogers SJ, & Vismara LA (2008). Evidence-based comprehensive treatments for early autism. Journal of Clinical Child & Adolescent Psychology, 37(1), 8–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers SJ, Vismara L, Wagner AL, McCormick C, Young G, & Ozonoff S (2014). Autism treatment in the first year of life: a pilot study of infant start, a parent-implemented intervention for symptomatic infants. Journal of Autism and Developmental Disorders, 44(12), 2981–2995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachse S, & Von Suchodoletz W (2008). Early identification of language delay by direct language assessment or parent report? Journal of Developmental and Behavioral Pediatrics : JDBP, 29(1), 34–41. doi: 10.1097/DBP.0b013e318146902a [DOI] [PubMed] [Google Scholar]
- Salomone E, & Maurizio Arduino G (2017). Parental attitudes to a telehealth parent coaching intervention for autism spectrum disorder. Journal of Telemedicine and Telecare, 23(3), 416–420. [DOI] [PubMed] [Google Scholar]
- Sanders M, Calam R, Durand M, Liversidge T, & Carmont SA (2008). Does self-directed and web-based support for parents enhance the effects of viewing a reality television series based on the Triple P–Positive Parenting Programme?. Journal of Child Psychology and Psychiatry, 49(9), 924–932. [DOI] [PubMed] [Google Scholar]
- Sharpe DL, & Baker DL (2007). Financial issues associated with having a child with autism. Journal of Family and Economic Issues, 28(2), 247–264. [Google Scholar]
- Statistics Times (2017, February 22). List of European Countries by GDP. Retrieved from http://statisticstimes.com/economy/european-countries-by-gdp.php.
- Taylor TK, Webster-Stratton C, Feil EG, Broadbent B, Widdop CS, & Severson HH (2008). Computer-based intervention with coaching: An example using the incredible years program. Cognitive Behaviour Therapy, 37(4), 233–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank (2015). How We Classify Countries. Retrieved from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519. Accessed 28 June 2017.
- Thomas KC, Ellis AR, McLaurin C, Daniels J, & Morrissey JP (2007). Access to care for autism-related services. Journal of Autism and Developmental Disorders, 37(10), 1902–1912. [DOI] [PubMed] [Google Scholar]
- Tonge B, Brereton A, Kiomall M, Mackinnon A, & Rinehart NJ (2014). A randomised group comparison controlled trial of ‘preschoolers with autism’: A parent education and skills training intervention for young children with autistic disorder. Autism, 18(2), 166–177. [DOI] [PubMed] [Google Scholar]
- UNESCO (2018). Retrieved from http://uis.unesco.org/country/AL
- UNICEF (2013, November 12). Statistics. Retrieved from https://www.unicef.org/infobycountry/albania_statistics.html
- United Nations Statistics Division. (2018, May 7). Households in housing units by type of housing until and availability of communication technology devices/access to Internet for selected cities. Retrieved from http://data.un.org/Data.aspx?d=POP&f=tableCode%3A307.
- Vismara LA, McCormick C, Young GS, Nadhan A, & Monlux K (2013). Preliminary findings of a telehealth approach to parent training in autism. Journal of Autism and Developmental Disorders, 43(12), 2953–2969. [DOI] [PubMed] [Google Scholar]
- Vismara LA, Young GS, & Rogers SJ (2012). Telehealth for expanding the reach of early autism training to parents. Autism Research and Treatment, 2012, 121878. doi: 10.1155/2012/121878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacker DP, Lee JF, Padilla Dalmau YC, Kopelman TG, Lindgren SD, Kuhle J, … & Waldron DB (2013). Conducting functional communication training via telehealth to reduce the problem behavior of young children with autism. Journal of Developmental and Physical Disabilities, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wainer AL, & Ingersoll BR (2013). Disseminating ASD interventions: A pilot study of a distance learning program for parents and professionals. Journal of Autism and Developmental Disorders, 43(1), 11–24. doi: 10.1007/s10803-012-1538-4 [DOI] [PubMed] [Google Scholar]
- Wainer AL, & Ingersoll BR (2015). Increasing access to an ASD imitation intervention via a telehealth parent training program. Journal of Autism and Developmental Disorders, 45(12), 3877–3890. doi: 10.1007/s10803-014-2186-7 [DOI] [PubMed] [Google Scholar]
- Wallace S, Fein D, Rosanoff M, Dawson G, Hossain S, Brennan L, Como A, & Shih A (2012). A global public health strategy for autism spectrum disorders. Autism Research, 5(3), 211–217. [DOI] [PubMed] [Google Scholar]
- Williams PG, Dalrymple N, & Neal J (2000). Eating habits of children with autism. Pediatric nursing, 26(3), 259. [PubMed] [Google Scholar]
- Young A, Ruble L, & McGrew J (2009). Public vs. private insurance: Cost, use, accessibility, and outcomes of services for children with autism spectrum disorders. Research in Autism Spectrum Disorders, 3(4), 1023–1033. [Google Scholar]
- Zablotsky B, Pringle BA, Colpe LJ, Kogan MD, Rice C, & Blumberg SJ (2015). Service and treatment use among children diagnosed with autism spectrum disorders. Journal of Developmental and Behavioral Pediatrics:JDBP, 36(2), 98–105. doi: 10.1097/DBP.0000000000000127 [DOI] [PMC free article] [PubMed] [Google Scholar]