ABSTRACT
Currently, many countries are dealing with groups refusing available recommended vaccinations. Despite several studies having demonstrated the efficacy of mandatory vaccinations in ensuring herd immunity, opposition is widespread. The aim of our study was to systematically review published studies evaluating attitudes towards mandatory vaccination programs. PubMed and Scopus scientific databases were searched and 4,198 results were returned, of these 29 met the inclusion criteria. Twenty-two studies assessed attitudes towards mandatory vaccination programs in general, while 9 papers focused specifically on the Human Papilloma Virus (HPV) vaccine. Most of the studies were performed in Europe and North America. According to the assessed studies, the majority of the population seems to be in favour of compulsory vaccinations, although attitudes differed among studies. The results presented in this review could be an important starting point to further understand the issue of vaccine hesitancy and support the implementation of effective vaccination strategies.
KEYWORDS: Vaccination, attitude, mandatory, review
Introduction
Vaccines have proven to be effective tools for controlling and eliminating life-threatening infectious diseases and are estimated to avoid between 2 and 3 million deaths each year. With clearly defined target groups, they are among the most cost-effective health investments, and evidence-based strategies allow them to be accessible to even the most hard-to-reach and vulnerable populations.1,2 Vaccination programs can concern the population in general (children, adolescents and adults in good health), but they are usually targeted towards specific groups such as pregnant women, travellers and individuals with specific diseases/conditions.3
Despite their proven effectiveness, some parents continue to have multiple concerns and misperceptions regarding childhood vaccinations, even in communities with high vaccination rates.4,5 Similarly, healthcare workers (HCW) have lingering misconceptions of vaccines and vaccine-preventable diseases and are one of the major causes for reduced uptake of recommended vaccines.6 This lack of confidence contributes to the occurrence of vaccine hesitancy, threatening the effectiveness of vaccination programs.7
In order to maintain vaccine-acquired herd immunity, it is essential that the vaccination coverage of the population remains above specific threshold values.8 Adopted vaccination policies differ greatly around the world: some countries focus on educating the population, giving individuals freedom of choice, while others have implemented mandatory vaccinations to ensure high coverage rates.9
The introduction of mandatory vaccination policies remains strongly debated: among healthcare workers, some mandatory vaccinations, such as Hepatitis B, are generally accepted,10,11 although their benefits and the ethical issues they pose are still widely discussed, as in the case of influenza vaccination.12-14
In many countries, routine immunization efforts are hindered by groups of people refusing vaccination for themselves and their children and no intervention has yet proven to be decisive in eliminating this issue.15,16
Mandatory vaccination strategies may represent a viable solution, as their effectiveness has been demonstrated in several contexts. In Italy, compulsory vaccinations for ten infectious diseases were introduced on the 31 of July 2017, following a decline in immunization levels below the coverage targets defined by the Italian national plan for prevention through vaccines, PNPV (Piano Nazionale Prevenzione Vaccinale).17 The implementation of this strategy has led to an increase in vaccine coverage from June to October 2017 of 1.0% for the hexavalent vaccine against diphtheria, tetanus, pertussis, poliomyelitis, Haemophilus Influenzae type b and hepatitis B and of 2.9% for the measles, mumps, and rubella vaccine, according to preliminary data.18 However, despite their proven effectiveness,19-21 mandatory vaccinations are not universally accepted.
According to the WHO SAGE Working Group on Vaccine Hesitancy, poor communication is an important factor in undermining acceptance. This can be a problem in any setting: in high-income countries, with well-resourced vaccination programs, inadequate or poor immunization program communication can increase vaccine hesitancy and outright refusal; in low and middle-income countries, scarce communication resources limit the capacity to counter negative information on vaccines and to achieve community support for vaccination programs.16
Evaluating attitudes towards mandatory vaccination could lead to better understand these issues and allow to plan suitable strategies to improve immunization coverage. Although attitudes towards mandatory vaccination have been investigated by a number of studies,22-25 to our knowledge the degree of consent has not yet been systematically reviewed. Therefore, the aim of this study was to systematically review published studies evaluating attitudes towards mandatory vaccination programs to promote awareness on this issue, which could benefit the implementation of such policies and help develop strategies to increase general approval and compliance.
Results
Our search strategy returned 4,198 records to be evaluated. After removing duplicates and irrelevant results, we obtained 230 articles for full text review. The final selection consisted of 29 studies (see Figure 1).
Figure 1.
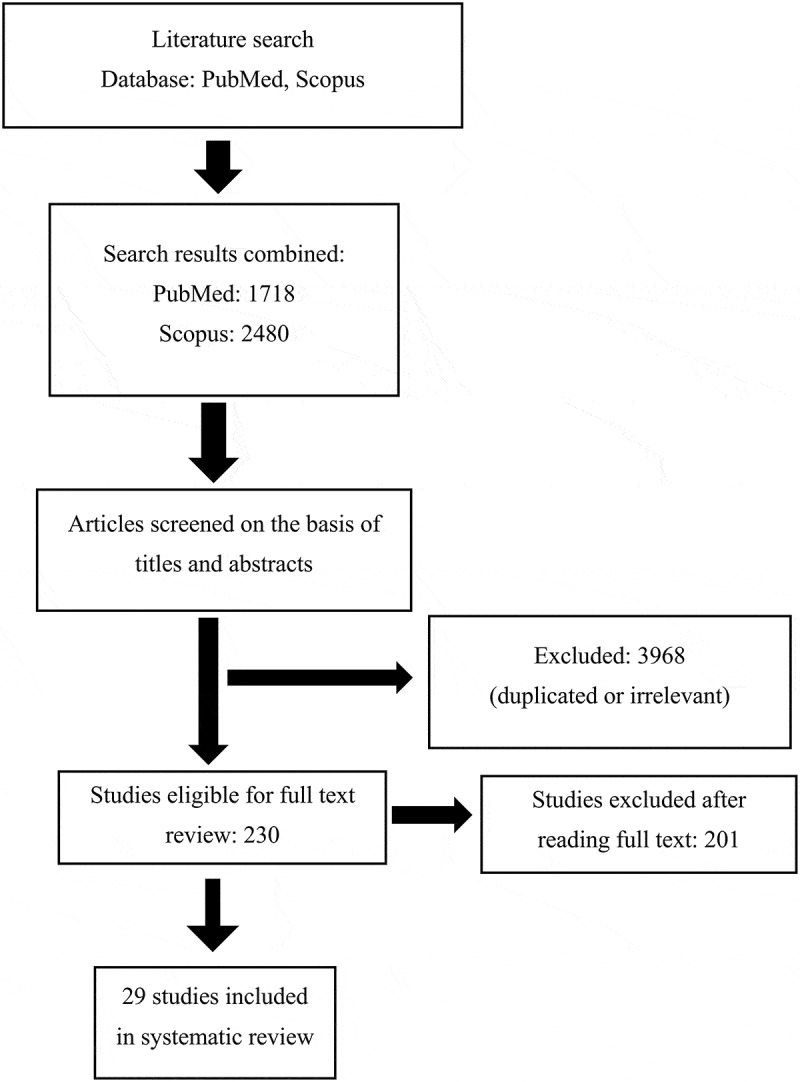
Articles research flow-chart following PRISMA guidelines.
A total of 22 studies assessed knowledge, attitudes and beliefs towards vaccination programs26-43 (Table 1), while 9 papers, two of which presented results obtained from the same study, assessed attitudes towards the Human Papilloma Virus (HPV) vaccine in young girls specifically (Table 2).25,26,38,44-47
Table 1.
Papers assessing knowledge, attitudes and believes towards vaccination programs.
| Country | Vaccine | Population Target | Sample | Evaluation Tool | Findings | |
|---|---|---|---|---|---|---|
| Akmatov 2009 50 | Kyrgyzstan | Childhood vaccinations | Children | Parents of first-year school children in the capital of Kyrgyzstan. N = 934 | A questionnaire was developed for the purpose of the study and focused on the child’s vaccination status, attitudes and beliefs towards vaccinations, and source of information about vaccines. | 15% of respondents were opposed to mandatory vaccination. |
| Akmatov 2018 22 | Germany | Adult vaccinations | Adult population | Males and females between 15 and 69 years of age selected from the population registries. N = 1,698 | Web- or paper-based questionnaire. The questionnaire on adult vaccinations was designed as a knowledge-attitude-practice (KAP) survey. | 82% of the study participants supported mandatory vaccinations for specific population groups such as health care workers and 40% for all adults. |
| Greenberg 2017 24 | Canada | Childhood vaccinations | Children 5 years old or younger | Parents with young children (5 and younger) regarding. N = 1,000 | An online survey included 25 questions organized into 4 major categories: perceptions about vaccines and vaccination; views on the public debate about vaccines and vaccine-preventable disease; information seeking needs and practices, including media usage and trust in institutional sources; and communication strategies |
44% agreed that vaccination should still be a matter of parental choice (49% disagreed, and 7% were unsure). When asked whether schools and day-care facilities should refuse children who are not vaccinated, except for those with medical exemptions, approximately 65% answered this question affirmatively. |
| Gualano 2018 23 | Italy | Childhood Vaccination | Children | Pregnant women from 15 Italian cities. N = 1,820 | A non-self-compiling paper questionnaire was used during the 25-minutes interview. The questionnaire was composed of seven sections for a total of 63 items. | Most women of the sample (81.6%) declared to be in favour of mandatory vaccinations, 13.8% were against them and 4.5% did not answer to the question. |
| Horn 2010 26 | USA | Childhood vaccination (focusing on HPV) | Children | Parents with children 9 to 17 years old. N = 325 | The survey was designed to be an anonymous self-administered survey. The 53-question survey was divided into 3 sections: demographic information, opinions on vaccines in general, and attitudes about the HPV vaccine. | The majority (89%) of parents support a mandatory vaccine program for their children. A minority of parents (43%) thought the HPV vaccine should be mandatory for their children. |
| Karageorgou 2014 27 | Greece | Vaccine Preventable Disease (VPD). As of 2013, in Greece the Ministry of Health recommends the vaccination of HCWs against the following diseases: seasonal influenza, hepatitis A, hepatitis B, measles, mumps, rubella, varicella, tetanus, diphtheria, acellular pertussis (for HCWs in contact with patients), and the tetravalent meningococcal (A,C,W135,Y) vaccine for microbiologists only. | HCWs | Students of the Faculty of Healthcare Professions, Department of Nursing and Department of Medical Laboratories. N = 165 |
A standardized, self-reported, anonymous paper questionnaire. | Mandatory vaccination of HCWs was supported by 96.7% of the students. |
| Kennedy 2005 28 | USA | Childhood Vaccination | Children | Parents with children aged <18 years living in the household. N = 1,540 | Data from the 2002 HealthStyles survey was used for analysis. HealthStyles is an annual, mail panel survey of adults in the contiguous United States, as well as the District of Columbia | Parents who strongly agreed or agreed that children should be allowed to go to public school even if they are not vaccinated were categorized as opposed to compulsory vaccination (opposed parents). Parents who were neutral, disagreed, or strongly disagreed with the statement were considered supportive of compulsory vaccination (supportive parents). 12% of this weighted subsample was classified as opposed to compulsory vaccinations for school entry |
| Krok-Schoen 2018 29 | USA | According to current recommendations by the Advisory Committee on Immunization Practices, adolescents should receive the tetanus, diphtheria toxoid, acellular pertussis, meningococcal vaccine, and human papillomavirus (HPV) vaccine at 11–12 years old. |
Children | Parents of girls aged 9–17 from 12 counties in rural Ohio Appalachia enrolled in the Community Awareness, Resources and Education Project. N = 337 | Telephone survey. During the initial phone call, the study was described, questions were answered, informed consent was obtained, and the baseline survey was administered. To assess beliefs about mandatory school vaccinations, participants were asked to respond to the statement, “Parents should have the right to refuse vaccines that are required for school for any reason.” |
47% agreed with the statement that parents should have the right to refuse vaccines that are required for schools for any reason. |
| Kubli 2017 30 | USA | Hepatitis B, influenza, measles, mumps, rubella (MMR), varicella, tetanus, diphtheria, pertussis (Tdap), meningococcal and human papilloma virus (HPV) | General Population | First year pharmacy students at the University of California San Diego Skaggs School of Pharmacy and Pharmaceutical Sciences. N = 85 | A pre- and post-immunization course questionnaire. The questionnaire had forty-eight items. | The proportion of students believing immunizations should be a personal choice, not mandatory, did not change significantly from prior to taking the course (41.5%) and following the course (37.4%, p = 0.5572). |
| Little 2015 31 | United Kingdom | Occupational Vaccination (annual flu and MMR) | HCWs | Clinical and non-clinical staff from eight randomly selected wards. N = 133 | The survey comprised of twelve questions, eleven required simple multiple choice tick box responses and one required numerical ranking. | 70% supported the routine use of compulsory vaccination for staff working with vulnerable patients. |
| Macintosh 2014 32 | USA | Occupational Vaccination (annual flu and MMR) | School Employees | A convenience sample of school district employees was invited to participate in the study. Both full- and part-time individuals employed by the rural school district were eligible. N = 835 | The questionnaire was two pages and included 10 yes/no, 7 multiple choice, 2 open-ended, and 7 demographic questions. | Of those who responded about their beliefs regarding vaccination mandates for all school employees, 24.2% replied “no,” although almost half of participants believed school employees should have mandatory vaccination requirements. Another 30.1% were undecided about vaccination mandates for school employees. |
| Maltezou 2012 33 | Greece | VPD: Completed and up-to-date vaccination was defined as follows: one shot for rubella, two shots for measles, mumps, varicella, or hepatitis A, and three shots for hepatitis B (all shots within the appropriate time schedule for each disease), and one booster shot against tetanus-diphtheria within the last 10 years. |
HCWs | HCWs regardless of demographic or professional characteristics in four tertiary-care hospitals. N = 505 |
A standardized printed form to assess demographic and professional data, knowledge about recommended vaccines, attitudes towards mandatory vaccinations, and self-reported immunity against vaccine-preventable diseases. |
63% stated that vaccination should be mandatory in general for all HCWs indiscriminately compared to 100% who stated that vaccination should be mandatory for HCWs who care for immunocompromised patients. Acceptance of a mandatory policy ranged significantly per disease, from 10.6% for mumps to 85.6% for hepatitis B. |
| Maltezou 2013 34 | Greece | Mandatory occupational vaccinations. In Greece, the Ministry of Health recommends annual vaccination of all HCWs against hepatitis B and seasonal influenza and vaccination of paediatricians and infectious disease specialists against hepatitis A. |
HCWs | HCWs were defined as all persons employed in a health care facility with or without involvement in direct patient care and regardless of employment status. They were selected in 185 primary health care centres in Greece. N = 2,055 | A standardized, self-answered, anonymous questionnaire. The questionnaire elicited demographic and professional data, data on immunity against vaccine-preventable diseases, knowledge regarding recommended vaccines, and attitudes regarding mandatory vaccination for HCWs. | 65.1% indicated that vaccinations should be mandatory; acceptance rates of mandatory vaccination differed by disease, ranging from 12.8% for pertussis to 87.3% for hepatitis B |
| Martinelli 2015 35 | Italy | Mandatory childhood vaccination: diphtheria, tetanus, polio and hepatitis B. | Children | Family paediatrician working in Puglia. N = 502 | A standardised, ad hoc and piloted phone questionnaire. The questionnaire included demographic and job information (gender, age, duration of professional career, number of children cared) and opinion on mandatory vaccinations. | 14.3% would agree with the hypothesis of abrogation of mandatory vaccination. |
| Nicolay 2008 36 | France | Adult Vaccination | General population | French population aged between 18 and 79 years. N = 4,112. General practitioners and paediatricians working or living in continental France. N = 1,285 General Practitioners and 742 paediatricians |
National telephone survey. Two different questionnaires were administered by experienced interviewers. Common topics included immunization, practices and perceptions related to infectious risk in general, nosocomial infections, travellers’ tropical diseases, hygiene, hepatitis and zoonosis; the practitioners’ questionnaire also include questions on their patients’ perceptions. Eighteen questions referred either directly or indirectly to immunization in the practitioner questionnaire, and 16 in the general population questionnaire. | 56.5% of the general population is in favour of mandatory vaccination. The percentage of GPs and paediatricians in favour of mandatory immunization is 42%. |
| Pelullo 2014 37 | Italy | Mandatory childhood vaccination: diphtheria, tetanus, polio and hepatitis B. | Children | One parent of each child brought for the first, second or third dose of the hexavalent vaccine. When both parents were present at the centre, the workers interviewed only the mother. N = 1,039 | A questionnaire was developed, aiming to investigate parents’ vaccination intentions. | 955 (91.9%) stated that they would certainly (n = 721; 69.4%) or probably (n = 234; 22.5%) vaccinate their children if vaccination were not mandatory. On the other hand, 84 parents (8.1%) stated that they would certainly (n = 30; 2.9%) or probably not (n = 35; 3.4%) vaccinate their children or that they did not know what they would do (n = 19; 1.8%). |
| Perkins 2010 38 | USA | HPV and Childhood vaccination | Vaccine-eligible girls aged 11–18 years | Parents or legal guardians of vaccine-eligible girls aged 11–18 years. N = 73 | Interviews. Interview guides were designed to elicit demographic information, parental intention to vaccinate against HPV, and parents’ opinions about mandating routine childhood vaccines and HPV vaccine. | 97.3% supported mandating childhood vaccinations for school entry. |
| Rebmann 2016 39 | USA | A staff mandatory vaccination policy was defined as a policy requiring all staff except those with a medical contraindication to receive all Centers for Disease Control and Prevention (CDC) recommended vaccines. |
Staff from children day-care agencies | Parents of children in day-care and childcare agency staff in the St Louis city and county region. In all, 23 childcare agencies assisted with subject recruitment. N = 354 | The questionnaire was available online and in paper format. The questionnaire assessed attitudes regarding a proposed staff mandatory vaccination policy and/or agency certification program, including which exemptions should be allowed (18 items); perceptions related to staff vaccination (2 items); immunization status related to pertussis, hepatitis A, and seasonal influenza vaccine (3 items); and agency vaccine exemption policies (5 items). | 80.0% reported that they would support a staff mandatory vaccination policy, and all groups (parents, staff, and administrators) were equally likely to support such a policy |
| Riccò 2017 40 | Italy | Tetanus | Agricultural Workers | The target population included Aws. The sampling was performed through convenience, involving all consecutive participants to qualification courses and focusing on the occupational use of pesticides. The following excluding criteria were applied: an inadequate ability to understand the Italian language and age < 18 years. N = 707 | The instrument used was a specifically designed structured questionnaire including a total of 22 items divided into four areas of inquiry: (1) Information about the interviewee. (2) Knowledge about vaccines. (3) Attitudes. (4) Practices | Attitude towards tetanus vaccination was somehow favourable in 79.5% of participants, and 72.7% correctly identified tetanus vaccination as mandatory for Agricultural Workers. |
| Seale 2009 41 | Australia | Mandatory Occupational Vaccination. Vaccines encompassed within the directive include measles–mumps–rubella vaccine (MMR), varicella, hepatitis B vaccine, and diphtheria–tetanus- (acellular) pertussis vaccine (Tdap). | HCWs | Four groups were surveyed: Medical (staff specialists, registrars, medical students), Nursing (registered nurses, nurse unit managers, and enrolled nurses), Allied Health Personnel (physiotherapists, occupational therapists, psychologists) and Ancillary staff (domestic services, administration, computer specialists). N = 1,079 | 6 page survey that assessed: (1) demographic characteristics, professional designation; (2) awareness and understanding of the policy directive; (3) knowledge of specific vaccine inclusion; and (4) level/reasons for support/opposition. 894 paper survey were collected and further 185 questionnaires were submitted electronically. | After a brief description of the policy directive, 78% of staff supported it, 13.0% neither supported nor opposed it and 3.6% of staff opposed the directive. Only one ancillary staff member stated that they opposed the directive. |
| Seale 2011 42 | Australia | Mandatory Occupational Vaccination. Vaccines encompassed within the directive include measles–mumps–rubella vaccine (MMR), varicella, hepatitis B vaccine, and diphtheria–tetanus- (acellular) pertussis vaccine (Tdap). | HCWs | 10 wards from the original 40 (which had been included in Seale 2009) to contact for this second study, which included all the high risk wards (intensive care, neonatal, and emergency). The survey was sent to every staff member on the ward. N = 256 | An anonymous self-completed paper-based questionnaire. We developed a four page survey that assessed (1) demographic characteristics and professional designation; (2) awareness and understanding of the policy directive; (3) level/reasons for support/opposition of the directive and how it was implemented; and (4) reasons for support/opposition for the possible inclusion of the influenza vaccine in the directive. | Eighty-five percent of respondents stated they were aware of a policy about staff vaccination. There was a significant change between the two surveys in regards to this question (OR: 0.27, 95%CI: 0.18–0.41, p = <0.001). The majority of respondents supported the directive, while four staff members were opposed to it. There was a significant increase in the number of respondents who supported the policy between the two surveys (OR: 0.47, 95% CI: 0.25–0.90, p = 0.01). |
| Tafuri 2009 43 | Italy | Mandatory childhood vaccination: diphtheria, tetanus, polio and hepatitis B. | Children | All the employees of the Apulian Vaccination Services immediately before each employee began a 10-day training course on the updated management system of the vaccination registers. N = 302 | A self-administered anonymous questionnaire. It reported demographic information, occupation, length of service in the vaccine clinic, the opinion on mandatory vaccination, the procedures for calling the parents to the clinic for the primary appointment and for the issuing of subsequent reminders, the conduct of the health worker when faced with parents who refuse vaccination for their child, and the importance the health worker gave to the computerisation of the vaccination registers. | Of those questioned, 4.4% (95% CI = 2–6.7) thought that mandatory vaccination should be abolished now, 21.2% (95% CI = 16.6–25.9) that it should be abolished gradually, while the majority of respondents, 74.4% (95% CI = 69.4–79.4), declared that it should be retained. The opinion that mandatory vaccination should be abolished was held by a higher proportion of doctors than by other health staff. |
KAP: Kwnoledge, attitudes and practice; HPV: Human Papilloma Virus; VPD: Vaccine Preventable Disease; HCWs: Healthcare Workers; MMR: measles, mumps, rubella; Tdap: tetanus, diphtheria, pertussis; Aws: Agricultural Workers;
Table 2.
Papers assessing knowledge, attitudes and believes towards Human Papilloma Virus (HPV) vaccine.
| Country | Vaccine | Population Target | Sample | Evaluation Tool | Findings | |
|---|---|---|---|---|---|---|
| Balla 2016 25 | Hungary | HPV | Children | Students aged ≥18 years in 19 high school. N = 1,022 | An anonymous questionnaire divided into 4 sections: 26 matrix questions concerned basic demographic, socio-economic, and lifestyle factors; 13 questions assessed knowledge about HPV infection and cervical cancer; 11 examined the attitude toward the HPV vaccine; 4 focused on cervical cancer screening. |
35.7% of the sample would make the vaccine compulsory |
| Carlos 2011 44 | USA | HPV | Girls ages 11–12 | Women attending breast and cervical cancer screening, mothers or primary caretakers of adolescent females aged 9–17. N = 232 |
A mail-based self-administered written survey assessed several constructs potentially related to HPV uptake (including demographics, knowledge of and experience with HPV and HPV-related diseases), individual-level perceptions such as perceived benefits, barriers and safety concerns about adolescent HPV vaccination, and intention to comply with an hypothetical mandate for adolescent HPV vaccination. |
Intent to follow a hypothetical law mandating adolescent HPV vaccination (11-point scale). All population: low intent (22.2%, representing 0–3 on the scale), undecided (14.3%, 4–6 on the scale) and high intent (63.5%, 7–10 on the scale). Only women with daughters ages 11–12: 29.3% low intent, 12.0% were undecided, 58.7% high intent. |
| Chapman 2010 48 | USA | HPV | Children | Women between the ages of 18 and 60. N = 186 | An anonymous questionnaire divided into sections: a 32-question initial assessment addressing general knowledge and beliefs about HPV, a section on demographic information and sections addressing both parental and individual vaccine acceptability. Subjects were then asked to watch an eight-minute video about HPV and the vaccine and to complete an additional 11-question post survey assessment. Five questions were extracted from pre- and post-video questionnaires to evaluate HPV vaccine acceptability. |
54.8% of respondents would make the vaccine required for all children |
| Ferris 2010 49 | USA | HPV | Children | Parents with children 9 to 17 years old. N = 325 | The survey was designed to be an anonymous self-administered survey. The 53-question survey was divided into 3 sections: demographic information, opinions on vaccines in general, and attitudes about the HPV vaccine. | A minority of parents (43%) thought the HPV vaccine should be mandatory for their children |
| Horn 2010 26 | USA | Childhood vaccination (focusing on HPV) | Children | Parents with children 9 to 17 years old. N = 325 | The survey was designed to be an anonymous self-administered survey. The 53-question survey was divided into 3 sections: demographic information, opinions on vaccines in general, and attitudes about the HPV vaccine. | A minority of parents (43%) thought the HPV vaccine should be mandatory for their children |
| Morhason-Bello 2015 45 | Nigeria | HPV | Children | Reproductive-aged women (18–49 years). N = 1,002 | A pretested self-administered tool was used to seek information. The main dependent variable in the analysis was willingness to have the HPV vaccine administered to their children, together with opinions and concerns regarding the HPV vaccine policy and program. | 64.3% strongly agreed that HPV vaccination should be made mandatory to all female children, and 52.9% also strongly agreed that the evidence of vaccine uptake should be a precondition for junior secondary school admission in Nigeria |
| Perkins 2010 38 | USA | HPV | Vaccine-eligible girls aged 11–18 years | Parents or legal guardians of vaccine-eligible girls aged 11–18 years. N = 73 | Interviews. Interview guides were designed to elicit demographic information, parental intention to vaccinate against HPV, and parents’ opinions about mandating routine childhood vaccines and HPV vaccine. | 62% of parents (n = 45) were in favour of requiring HPV vaccination for school entry. |
| Rashwan 2013 46 | Malaysia | HPV | Female students | Only female students in 8 government schools in Kuala Lumpur, from form 4 and lower form 6, with age range from 15–20 years old. N = 550 | Pre-tested and validated self-administered questionnaire. The questionnaire was divided into 4 parts. Part A: demographic data of respondents, part B: knowledge of cervical cancer, part C: knowledge of prevention of cervical cancer and part D: questions about vaccination. | The majority of respondents (82.2%) agreed that vaccination should be compulsory for school students in Malaysia. |
| Tyrell 2015 47 | Guyana | HPV | Young females | Two different study populations: 11-year old girls from five primary schools in Georgetown and their guardians. N1 = 87, N2 = 74 | Questionnaires were used to collect the data. One questionnaire was used for the girls first and included questions about HPV, the vaccine, cervical cancer and access to health information. A similar questionnaire was utilized for the guardians but also incorporated questions about level of education, gender and home address. Each questionnaire took approximately 15 minutes to complete. | 40% of girls and 27% of guardians thought that the vaccine should be made mandatory. |
HPV: Human Papilloma Virus
Vaccination programs
Knowledge, attitudes, and beliefs towards vaccination were assessed by 22 studies, published between 2005 28 and 2018.22,23 Eleven of these studies were performed in Europe,22,23,27,31,33-37,40,43 eight in North America24,26,28-30,32,38,39 and three in other countries.41,42,50 Most of these studies concerned childhood vaccinations.23,24,26-37,39,41-43,50 The sample size ranged from 7338 to more than 4,000 interviewed subjects.36
A first group of studies consisted of surveys conducted among parents to assess their attitude towards mandatory childhood vaccination.23,24,26,28,29,37,38,50 In particular, the first study performed in 2005 showed how 12% of the 1,527 interviewed parents was opposed to compulsory vaccination. Survey results indicated that parent’s opinions on compulsory vaccination for school admission were significantly associated with believing in the safety and usefulness of vaccines.28 Similarly, a study from Central Asia performed in 2006 revealed that in the specific area about 15% of interviewed parents were opposed to mandatory vaccination.50 Lower percentages were recorded in two studies performed in the USA in 2010.26,38 In the first one, 10.8% of the parents that were questioned refused to support government-mandated vaccine requirements.49 In the second one, only two parents out of 73 (3%) did not support requiring childhood vaccinations for school entry.38 On the other hand, a higher level of refusal was recorded in the rural Ohio Appalachia area, where 47% of interviewed parents agreed with the statement that parents should have the right to refuse vaccines required for school admission for any reason.29 Most recently, more than 1,800 pregnant women were interviewed in an Italian study and results showed that 13.8% were against mandatory vaccination for school admission, while 81.6% supported mandatory vaccination.23 Greenber at al. performed an in-deep focus in 2017. In their paper the issue of mandatory vaccination was particularly contentious: parents were split when asked, “should parents be able to choose whether their children are vaccinated?”; even though more than 90% of parents chose to vaccinate their children, 44% agreed that vaccination should be a matter of parental choice. Furthermore, approximately 65% of respondents agreed that schools and day-care facilities should refuse children who are not vaccinated, except those with medical exemptions.24 Pelullo et al. evaluated in 2013 whether it is reasonable to abandon compulsory vaccinations in Italy. Most respondents (91.9%) said that they would certainly (69.4%) or probably (22.5%) vaccinate their children if vaccinations were not mandatory.37
Two Italian studies assessed knowledge, attitudes and beliefs towards mandatory childhood vaccination among healthcare workers.35,43 The first, published in 2009, was conducted through a self-administered anonymous questionnaire given to all the employees of the Vaccination Service of Apulia, a southern region of Italy. In total, 302 health care workers participated in the survey, representing 100% of the Vaccination Service personnel. Of those questioned, 4.4% (95% CI = 2–6.7) thought that mandatory vaccination should be abolished immediately, 21.2% (95% CI = 16.6–25.9) that it should be abolished gradually, while the majority of respondents, 74.4% (95% CI = 69.4–79.4), declared that it should be maintained. The opinion that mandatory vaccination should be abolished was more frequent among doctors than other health care workers.43 in the second Italian study, published in 2015, 502 family paediatricians were interviewed. Among them, only 72 (14.3%) agreed with abolishing mandatory vaccination, and 46.6% (n = 234) of the respondents considered mandatory vaccinations to be more effective than recommended vaccinations.35
Three studies considered knowledge, attitudes and beliefs concerning mandatory vaccination targeted towards the general population.22,30,36 The first of these, performed in France between 2005 and 2006, involved 4,112 individuals between 18 and 79 years that were interviewed using a telephone survey. Of the interviewed subjects, 56.5% were in favour of mandatory vaccination. In the same study, general practitioners and paediatricians were asked if they were in favour of mandatory immunization programs and 42% among the 1285 GPs and the 742 paediatricians involved responded affirmatively.36 A second study was performed in Germany in 2014, through the HaBIDS study (Hygiene and Behaviour Infectious Diseases Survey), an online panel. Of the 2,379 panel members, 1,698 (71%) completed the knowledge-attitude-practice (KAP) questionnaire on vaccinations. Overall, 82% of participants agreed that adult vaccinations should be mandatory for selected groups such as health care workers, and 40% stated that vaccinations should be mandatory for all adults.22 A third study evaluated pharmacy students’ perceptions of immunizations using a pre- and post-immunization course questionnaire. Among the 85 students interviewed, the proportion of students believing immunizations should be a personal choice, not mandatory, did not change significantly before (n = 41, 49%) and after taking the course (n = 37, 44%, p = 0.5572).30
Finally, nine studies assessed attitudes towards specific mandatory occupational vaccination protocols for different types of workers.27,31-34,39-42 The first study was performed in 2009 in Australia, and aimed to assess knowledge, attitudes and beliefs concerning a policy directive which requires all staff in certain patient care areas to prove protection against certain infectious diseases or to be vaccinated against measles, mumps, rubella, diphtheria, tetanus, pertussis, hepatitis B and varicella. A total of 1,200 paper surveys were distributed and 894 collected, and 185 questionnaires were submitted electronically, resulting in a total of 1,079 completed questionnaires. The results showed that 78% of staff supported the directive, 13.0% neither supported nor opposed it and 3.6% were opposed.41 Two years after the implementation of the policy directive, another survey was performed. Eighty-five percent of respondents stated they were aware of the policy and the majority of respondents (91.3%, n = 198) supported the directive, while four staff members were opposed to it. There was a significant increase in the number of respondents who supported the policy between the two surveys (OR: 0.47, 95%CI: 0.25–0.90, p = 0.01).42 Two other similar studies were performed in Greece to evaluate healthcare workers’ opinions on mandatory vaccinations.33,34 In the first study, a questionnaire was distributed to healthcare workers of four tertiary-care hospitals; 63% stated that vaccinations should be mandatory in general for all healthcare workers indiscriminately and 100% stated that vaccinations should be mandatory only for those caring for immunocompromised patients. Acceptance of a mandatory policy ranged significantly per disease, from 10.6% for mumps to 85.6% for hepatitis B33. In the second study, a questionnaire was distributed to the personnel working in all primary health care centres in Greece. A total of 2,055 healthcare workers (36.4% response rate) from 152 primary health care centres participated: 65.1% indicated that vaccinations should be mandatory for HCWs; however, acceptance rates differed by disease, ranging from 12.8% for pertussis to 87.3% for hepatitis B.34 The third study, performed in Athens among 165 healthcare students, showed how healthcare workers’ mandatory vaccination was supported by 145 (96.7%) students.27 Similar results emerged from an English study where 133 clinical and non-clinical staff were interviewed: There was substantial support (nearly 70%) for the routine use of compulsory vaccination for staff working with vulnerable patients.31 Rebmann et al. assessed the support for a childcare agency staff mandatory vaccination policy, defined as a policy requiring all staff except those with a medical contraindication to receive all Centres for Disease Control and Prevention (CDC)-recommended vaccines. Overall, 354 parents, staff and agency administrators from 23 childcare agencies participated in the survey. Most respondents (80%) reported that they would support a mandatory staff vaccination policy and all groups were equally likely to support such a policy.39 In another American study, 835 school employees were interviewed on their opinion regarding mandatory vaccination for all school employees; 24.2% were opposed, although almost half of participants (45.7%) believed school employees should have mandatory vaccination requirements, and another 30.1% were undecided.32 An Italian study published in 2017 assessed the attitudes towards mandatory tetanus vaccination for agricultural workers: 79.5% of participants were favourable to some degree and 72.7% were aware that tetanus vaccination is mandatory for agricultural workers in Italy.40
HPV vaccination
There were 8 studies (9 papers) focusing on HPV vaccination, published between 201026,38,48,49 and 2016.25 Half of the studies were performed in the USA,26,38,44,48,49 one in Malaysia,46 one in Guyana,47 one in Nigeria45 and one in Hungary.25 Samples consisted of parents and caretakers of adolescents in a first group of studies,26,38,44,49 students from high school in two studies,25,46 both parents and children in one study,47 and women over 18 years old in the two final studies.45,48 The majority of the studies collected data through questionnaires (web- or paper-based), while only one study used qualitative interviews.38 Sample sizes ranged from 73 38 to 1,022 interviewed subjects.25
Four studies assessed knowledge, attitudes and beliefs about HPV vaccination in parents or caretakers of adolescents.26,38,44,47,49 The percentage of agreement with mandatory vaccination ranged from 27% 47 to 63.5%.44 The study with the lowest percentage of agreement was a cross-sectional survey performed in Guyana in 201547 on two different study populations, which examined the level of knowledge on HPV vaccination in a sample of 11-year old girls (N = 87) and their guardians (N = 74 parents or schoolteachers who had 11-year old daughters). Only 27% of guardians thought the vaccine should be made mandatory. Most guardians who were against mandatory vaccination stated that information was limited and that it should be a personal choice. The other three studies were conducted in the USA. A first survey, performed in Georgia in 2010, involved 325 parents of 9- to 17-year-olds;49 43% of the sample agreed with adding the HPV vaccine to school entry requirements. A second study,38 performed in Massachusetts and published in 2010, interviewed parents or legal guardians of vaccine-eligible girls aged 11–18 years who accessed Paediatric, Adolescent, or Obstetrics and Gynaecology practices for preventive care or problem-related visits. Qualitative interviews were used to explore parents’ attitudes about school-related mandatory HPV vaccination. Despite 89% intending their daughters to receive the HPV vaccine, only 62% of parents (n = 45) were in favour of requiring HPV vaccination for school entry. Parents’ arguments opposing compulsory HPV vaccination were: that they considered vaccination a personal choice and that HPV is not transmissible by routine social contact. In 2011, in Michigan, Carlos et al. interviewed women attending breast and cervical cancer screening, mothers or primary caretakers of adolescent females aged 9–17 years old.44 The primary outcome measured in the study was whether mothers intended to comply to a hypothetical law requiring HPV vaccination for their eldest adolescent daughter. Based on the results, the sample was divided in two groups: low intent and undecided (36.5%, representing 0–6 on the Likert scale) and high intent (63.5%, representing 7–10 on the scale). High safety concern scores (adjusted OR 0.4, 95% CI 0.25–0.77) and a perception that their daughter was too young for vaccination (adjusted OR 0.72, 95% CI 0.54–0.98) were associated with lower probability of intent to comply on the mothers’ part. High vaccine benefits scale scores (adjusted OR 2.98, 95% CI 1.62–5.49) were associated with higher intent to comply.
Three more recent studies analysed the knowledge of young adults on HPV-induced diseases and assessed their attitudes towards HPV vaccination. The percentage of agreement with mandatory vaccination were respectively 35.7% in Hungary,25 40% in Guyana47 and 82.2% in Malaysia.46 The Hungarian sample was the largest: Balla et al. interviewed 1022 students aged ≥18 years in 19 high schools in Budapest 25. Their aim was to assess knowledge on HPV infection and cervical cancer and to examine the attitude towards the HPV vaccine and cervical cancer screening: 35.7% of the sample favoured compulsory vaccination, 31.4% was undecided and 32.9% was against it. In the above-mentioned study by Tyrell et al., the sample consisted of 87 11-year old girls from five primary schools in Georgetown and their guardians.47 Forty per cent of the girls involved thought that the vaccine should be made mandatory. Most of the girls that were against mandatory vaccination indicated that information was limited and that vaccination should be a personal choice. Finally, Rashwan et al. interviewed 550 female 15 to 20 year old students in 8 government schools in Kuala Lumpur.46 The majority of respondents (82.2%) agreed that vaccination should be compulsory for secondary school students in Malaysia.
The last two studies involved women over 18 years old.45,48 In both studies, the percentage of agreement to mandatory vaccination was over 50%. In the first study,48 performed in 2010 in Massachusetts, 186 women (between the ages of 18 and 60) completed a 32-question initial assessment addressing HPV knowledge and vaccine acceptability, watched an eight-minute video about HPV and then completed a post-video assessment. Of the 186 subjects, 54.8% (n = 102) agreed that the vaccine should be compulsory for all children in the initial interview; and after watching the video, support for mandatory vaccination increased to 72.6% (p < 0.001). In the second study,45 performed in Nigeria and published in 2015, the sample consisted of 1002 women of reproductive age (18–49 years). The study aimed to determine women’s acceptance for HPV vaccination for their children and their opinions on various vaccination policies. Almost two out of five (38.7%) of the interviewed women had no children. According to the results, 64.3% strongly agreed that HPV vaccination should be mandatory for all female children; moreover, 52.9% strongly agreed that proof of vaccination should be a condition for junior secondary school admission in Nigeria.
Discussion
The purpose of our research was to investigate attitudes towards mandatory vaccination programs, by systematically reviewing the existing literature through the methodology proposed by the PRISMA statement.51 Currently, many countries are dealing with groups refusing available recommended vaccinations for themselves and/or their children.52-54 This issue has created a need for national immunization programs to develop approaches and strategies to address vaccine hesitancy, including the introduction of compulsory vaccination. Investigating attitudes towards mandatory vaccination may help to more effectively implement vaccination programs. An increasing number of studies carried out in different countries address this topic, which emphasizes how this issue is gaining attention, especially in Europe (12 studies) and North America (10 studies).
Parents’ attitudes towards mandatory vaccinations differed among studies, with support ranging from 53% 29 to 97% 38 for different vaccination programs. Stronger resistance emerged for the HPV vaccine: the percentage of agreement for mandatory HPV vaccination ranged from 27%47 to 63.5% .44 Multiple studies analysed parents’ perceptions of the HPV vaccine, concluding that parents are more likely to refuse the HPV vaccine than any other adolescent vaccination.55,56 Among other factors determining vaccine hesitancy in parents, a frequent argument opposing mandatory HPV vaccination was considering HPV not transmissible by routine social contact.38 Moreover, several studies highlighted that knowledge on HPV vaccination is limited.38,47 Higher percentages of agreement were found when assessing young adults’ attitudes towards HPV vaccination (from 35.7 in Hungary to 82.2% in Malaysia),25,46 although in the study by Tyrell et al. most girls opposing mandatory vaccination indicated that information was limited.47
Other studies included in this analysis investigated healthcare workers’ attitudes towards childhood and adult vaccinations. In Italy, according to two studies, the majority of healthcare personnel and doctors thought that mandatory vaccination should be maintained.35,43 Among those opposed, the most common opinions were that refusing childhood vaccination is a parental right and that the public is sufficiently aware of the importance of vaccination to allow an abrogation of the obligation, suggesting that mandatory vaccination may be perceived as an out-dated policy which has served its purpose and is no longer necessary. A French study showed only 42% of GPs and paediatricians were in favour of mandatory immunization,36 although in the same study, 56.5% of the general population was in favour of mandatory vaccination.36 The Authors of this study suggested mandatory immunization may not encourage the information of patients and dialogue with healthcare professionals. The opinion of healthcare workers on mandatory vaccination is crucial, especially considering studies have shown parents and patients rely on them as their main source of information regarding vaccination57 and doctors’ attitudes seem to be a determining factor in convincing patients: one the main reasons stated by parents for refusing vaccines for their children is that their GP did not offer them.58
Furthermore, HCW are more exposed to vaccine-preventable diseases and face an increased risk of spreading them to patients, therefore their attitudes towards mandatory vaccination have a direct impact on patient safety, as in the recent nosocomial-transmitted measles outbreaks in developed countries.59 Studies have demonstrated that among healthcare workers acceptance rates for mandatory vaccination differ by disease.33,34 HCW opposing mandatory vaccinations have stated they feel their rights of choice, liberty and autonomy are not respected and that not enough information is provided to them, while others have voiced safety and efficacy concerns.41 Another study found believing vaccinations are not their professional responsibility and organizational issues such as inconvenient times and locations were also a factor in reduced vaccine uptake among HCW.31
These results highlight the complexity of this topic on multiple levels. In general, it seems that support towards mandatory policies increases after their implementation,42 although other strategies must be implemented to improve attitudes and uptake among HCW, such as increasing staff education and providing proof of the efficacy, benefits and safety of vaccines.31
In conclusion, according to the results of the present review, despite the growing resonance of anti-vaccination movements, the majority of the population seems to be in favour of mandatory vaccination policies.
Nevertheless, our review has some limitations that should be acknowledged. To be as comprehensive as possible, we did not exclude any study on the basis of sample size, which varied considerably among studies. Data were collected using questionnaires and a low response rate in some studies 29,39,44 may have led to selection bias. Moreover, we found few studies published outside of Europe or North America. This could be due to a language limitation, since our research excluded all studies not written in English, Italian or French. Finally, our study focused on a quantitative assessment of the acceptance of mandatory vaccinations and investigated to a lesser extent the reasons for which opinions were held. The results of the present review could serve as a starting point for further studies analysing these aspects.
Methods
The present review followed the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) statement.51
Multiple search strategies were adopted in order to summarize the existing evidence related to attitudes towards compulsory vaccination. We considered all papers reporting data obtained from structured surveys assessing the selected outcomes. Considering the recent cultural changes concerning human compulsory vaccination and the increased attention to the issue of vaccine hesitancy,16 we included studies performed after the year 2000.
We consulted the two following databases: PubMed and Scopus. Three researchers (MC, EO and GV) independently performed a systematic search using the following keywords: “Compulsory AND vaccination” OR “mandatory AND vaccination”.
Studies were considered eligible for inclusion if:
They consisted in structured or semi-structured surveys assessing knowledge, attitudes and beliefs towards compulsory vaccinations
They assessed human vaccines
They were written in English, Italian or French
They were published after 2000
No restrictions were performed based on the sample size or the setting of the survey. All article types were included.
However, studies were excluded if:
They involved a non-structured interview
They assessed vaccination coverage but not the knowledge, attitudes and beliefs towards compulsory vaccination
They concerned only seasonal vaccinations
They were letters to the editor or were published before 2000
The first literature search was independently conducted by MC, EO and GV, sources were sorted by title and abstract, and eligible studies were selected for full text review. During the first screening, irrelevant or duplicated papers were excluded. The search was completed through a reference list screening. Finally, the researchers independently assessed the articles considering the criteria enunciated above.
Data extraction
The investigators, solving any discrepancies by consensus, read each full text and independently extracted data from the selected studies. Each investigator collected information about the country in which the study was performed, the vaccine involved, characteristics of the sample, the questionnaire that was used, the outcomes that were assessed and the results of the study.
Acknowledgments
The authors declare that no funding or grant was received from other organizations for the conduction of this study.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- 1.WHO | Immunization WHO. 2018. [accessed 2018 September 14]. http://www.who.int/topics/immunization/en/.
- 2.Plotkin SA, Plotkin SL.. The development of vaccines: how the past led to the future. Nat Rev Microbiol. 2011;9(12):889–93. doi: 10.1038/nrmicro2668. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Vaccines and Immunizations | home | CDC. [accessed 2018. September 14] https://www.cdc.gov/vaccines/index.html.
- 4.Allan N, Harden J. Parental decision-making in uptake of the MMR vaccination: a systematic review of qualitative literature. J Public Health (Bangkok). 2014;37(4):fdu075. doi: 10.1093/pubmed/fdu075. [DOI] [PubMed] [Google Scholar]
- 5.Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative Analysis of Mothers’ Decision-Making About Vaccines for Infants: the Importance of Trust. Pediatrics. 2006;117(5):1532–41. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- 6.Lytras T, Kopsachilis F, Mouratidou E, Papamichail D, Bonovas S. Interventions to increase seasonal influenza vaccine coverage in healthcare workers: A systematic review and meta-regression analysis. Hum Vaccin Immunother. 2016;12(3):671–81. doi: 10.1080/21645515.2015.1106656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Strategic Advisory Group of Experts (SAGE). Report of the SAGE working group on vaccine hesitancy. World Health Organization 2014, October [accessed 2019 Jen 21]. https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf
- 8.Fine P, Eames K, Heymann DL. “Herd immunity”: A rough guide. Clin Infect Dis. 2011;52(7):911–16. doi: 10.1093/cid/cir007. [DOI] [PubMed] [Google Scholar]
- 9.Walkinshaw E. Mandatory vaccinations: the international landscape. Cmaj. 2011;183(16):E1167–E1168. doi: 10.1503/cmaj.109-3993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bloch AB, Orenstein WA, Stetler HC, Wassilak SG, Amler RW, Bart KJ, Kirby CD, Hinman AR. Health impact of measles vaccination in the United States. Pediatrics. 1985;76:524–32. [PubMed] [Google Scholar]
- 11.Bock HL, Kruppenbacher J, Sänger R, Höbel W, Clemens R, Jilg W. Immunogenicity of a recombinant hepatitis B vaccine in adults. Arch Intern Med. 1996;156(19):2226–31. doi: 10.1001/archinte.1996.00440180088011. [DOI] [PubMed] [Google Scholar]
- 12.Abramson ZH. What, in Fact, Is the Evidence That Vaccinating Healthcare Workers against Seasonal Influenza Protects Their Patients? A Critical Review. Int J Family Med. 2012;2012:1–6. doi: 10.1155/2012/205464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hooper CR, Breathnach A, Iqbal R. Is there a case for mandating influenza vaccination in healthcare workers?. Anaesthesia. 2014;69(2):95–100. doi: 10.1111/anae.12561. [DOI] [PubMed] [Google Scholar]
- 14.Thomas RE, Jefferson T, Lasserson TJ. Influenza vaccination for healthcare workers who care for people aged 60 or older living in long-term care institutions. Cochrane Database Syst Rev. 2016;(6)CD005187. doi: 10.1002/14651858.CD005187.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dubé E, Gagnon D, Nickels E, Jeram S, Schuster M. Mapping vaccine hesitancy-Country-specific characteristics of a global phenomenon. Vaccine. 2014;32:6649–54. doi: 10.1016/j.vaccine.2014.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MacDonald NE. SAGE Working Group on Vaccine Hesitancy T. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–64. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 17.Piano Nazionale Prevenzione Vaccinale.; 2017. [accessed 2018 December 4]. http://www.salute.gov.it/imgs/C_17_pubblicazioni_2571_allegato.pdf.
- 18.Signorelli C, Iannazzo S, Odone A. The imperative of vaccination put into practice. Lancet Infect Dis. 2018;18(1):26–27. doi: 10.1016/S1473-3099(17)30696-5. [DOI] [PubMed] [Google Scholar]
- 19.Babcock HM, Gemeinhart N, Jones M, Dunagan WC, Woeltje KF. Mandatory influenza vaccination of health care workers: translating policy to practice. Clin Infect Dis. 2010;50(4):459–64. doi: 10.1086/650752. [DOI] [PubMed] [Google Scholar]
- 20.Olshen E, Mahon BE, Wang S, Woods ER. The impact of state policies on vaccine coverage by age 13 in an insured population. J Adolesc Heal. 2007;40(5):405–11. doi: 10.1016/j.jadohealth.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 21.Al-Tawfiq JA, AbuKhamsin A, Memish ZA. Epidemiology and impact of varicella vaccination: a longitudinal study 1994-2011. Travel Med Infect Dis. 2013;11(5):310–14. doi: 10.1016/j.tmaid.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Akmatov MK, Rübsamen N, Deyneko IV, Karch A, Mikolajczyk RT. Poor knowledge of vaccination recommendations and negative attitudes towards vaccinations are independently associated with poor vaccination uptake among adults – findings of a population-based panel study in Lower Saxony, Germany. Vaccine. 2018;36(18):2417–26. doi: 10.1016/j.vaccine.2018.03.050. [DOI] [PubMed] [Google Scholar]
- 23.Gualano MR, Bert F, Voglino G, Buttinelli E, D’Errico MM, De Waure C, Di Giovanni P, Fantini MP, Giuliani AR, Marranzano M, et al. Attitudes towards compulsory vaccination in Italy: results from the NAVIDAD multicentre study. Vaccine. 2018;36(23):3368–74. doi: 10.1016/j.vaccine.2018.04.029. [DOI] [PubMed] [Google Scholar]
- 24.Greenberg J, Dubé E, Driedger M. Vaccine hesitancy: in search of the risk communication comfort zone. PLoS Curr. 2017;9:1–11. doi: 10.1371/currents.outbreaks.0561a011117a1d1f9596e24949e8690b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Balla B, Terebessy A, Tóth E, Balázs P. Young hungarian students’ knowledge about HPV and their attitude toward HPV vaccination. Vaccines. 2016;5(1):1. doi: 10.3390/vaccines5010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Horn L, Howard C, Waller J, Ferris DG. Opinions of parents about school-entry mandates for the human papillomavirus vaccine. J Low Genit Tract Dis. 2010;14(1):43–48. doi: 10.1097/LGT.0b013e3181b0fad4. [DOI] [PubMed] [Google Scholar]
- 27.Karageorgou K, Katerelos P, Efstathiou A, Theodoridou M, Maltezou HC. Vaccination coverage and susceptibility against vaccine-preventable diseases of healthcare students in Athens, Greece. Vaccine. 2014;32(39):5083–86. doi: 10.1016/j.vaccine.2014.06.031. [DOI] [PubMed] [Google Scholar]
- 28.Kennedy AM, Brown CJ, Gust DA. Vaccine beliefs of parents who oppose compulsory vaccination. Public Health Rep. 2005;120(3):252–58. doi: 10.1177/003335490512000306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krok-Schoen JL, Bernardo BM, Weier RC, Peng J, Katz ML, Reiter PL, Richardson MS, Pennell ML, Tatum CM, Paskett ED. Belief about mandatory school vaccinations and vaccination refusal among ohio appalachian parents: do demographic and religious factors, general health, and political affiliation play a role? J Rural Heal. 2018;34(3):283–92. doi: 10.1111/jrh.12285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kubli K, McBane S, Hirsch JD, Lorentz S. Student pharmacists’ perceptions of immunizations. Curr Pharm Teach Learn. 2017;9(3):479–85. doi: 10.1016/J.CPTL.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 31.Little KE, Goodridge S, Lewis H, Lingard SW, Din S, Tidley M, Roberts RJ, Williams NS, Hayes S. Occupational vaccination of health care workers: uptake, attitudes and potential solutions. Public Health. 2015;129(6):755–62. doi: 10.1016/J.PUHE.2015.02.031. [DOI] [PubMed] [Google Scholar]
- 32.Macintosh J, Luthy KE, Beckstrand RL, Eden LM, Orton J. Vaccination perceptions of school employees in a rural school district. Vaccine. 2014;32(37):4766–71. doi: 10.1016/J.VACCINE.2014.06.029. [DOI] [PubMed] [Google Scholar]
- 33.Maltezou HC, Gargalianos P, Nikolaidis P, Katerelos P, Tedoma N, Maltezos E, Lazanas M. Attitudes towards mandatory vaccination and vaccination coverage against vaccine-preventable diseases among health-care workers in tertiary-care hospitals. J Infect. 2012;64(3):319–24. doi: 10.1016/j.jinf.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 34.Maltezou HC, Katerelos P, Poufta S, Pavli A, Maragos A, Theodoridou M. Attitudes toward mandatory occupational vaccinations and vaccination coverage against vaccine-preventable diseases of health care workers in primary health care centers. Am J Infect Control. 2013;41(1):66–70. doi: 10.1016/j.ajic.2012.01.028. [DOI] [PubMed] [Google Scholar]
- 35.Martinelli D, Tafuri S, Fortunato F, Cozza V, Germinario CA, Prato R. Are we ready to abrogate compulsory vaccinations for children?. Hum Vaccin Immunother. 2015;11(1):146–49. doi: 10.4161/hv.34417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nicolay N, Lévy-Bruhl D, Gautier A, Jestin C, Jauffret-Roustide M. Mandatory immunization: the point of view of the French general population and practitioners. Vaccine. 2008;26(43):5484–93. doi: 10.1016/j.vaccine.2008.07.058. [DOI] [PubMed] [Google Scholar]
- 37.Pelullo CP, Marino S, Valdes Abuadili AJ, Signoriello G, Attena F. Is it reasonable to abandon obligatory vaccinations in Italy? A 2013 survey. Eurosurveillance. 2014;19(35):1–7. doi: 10.2807/1560-7917.ES2014.19.35.20889. [DOI] [PubMed] [Google Scholar]
- 38.Perkins RB, Pierre-Joseph N, Marquez C, Iloka S, Clark JA. Parents’ opinions of mandatory human papillomavirus vaccination: does ethnicity matter? Women’s Heal Issues. 2010;20(6):420–26. doi: 10.1016/j.whi.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rebmann T, Wang J, Wilson KD, Gilbertson PG, Wakefield M. Parents’ and staff’s support for a childcare agency employee mandatory vaccination policy or agency certification program. Am J Infect Control. 2016;44(7):799–804. doi: 10.1016/j.ajic.2016.01.033. [DOI] [PubMed] [Google Scholar]
- 40.Riccò M, Razio B, Panato C, Poletti L, Signorelli C. Knowledge, attitudes and practices of agricultural workers towards tetanus vaccine: a field report. Ann Di Ig Med Prev E Di Comunita. 2017;29(4):239–55. doi: 10.7416/ai.2017.2156. [DOI] [PubMed] [Google Scholar]
- 41.Seale H, Leask J, Raina MacIntyre C. Do they accept compulsory vaccination? Awareness, attitudes and behaviour of hospital health care workers following a new vaccination directive. Vaccine. 2009;27(23):3022–25. doi: 10.1016/j.vaccine.2009.03.038. [DOI] [PubMed] [Google Scholar]
- 42.Seale H, Leask J, MacIntyre CR. Awareness, attitudes and behavior of hospital healthcare workers towards a mandatory vaccination directive: two years on. Vaccine. 2011;29(21):3734–37. doi: 10.1016/j.vaccine.2011.03.050. [DOI] [PubMed] [Google Scholar]
- 43.Tafuri SST, Martinelli DDM, Caputi GGC, Arbore AAA, Germinario CCG, Prato RRP. Italian healthcare workers’ views on mandatory vaccination. BMC Health Serv Res. 2009;9:100. doi: 10.1186/1472-6963-9-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carlos RC, Dempsey AF, Resnicow K, Ruffin M, Patel DA, Straus CM, Dalton VK. Maternal characteristics that predict a preference for mandatory adolescent HPV vaccination. Hum Vaccin. 2011;7(2):225–29. doi: 10.4161/hv.7.2.13691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morhason-Bello IO, Wallis S, Adedokun BO, Adewole IF. Willingness of reproductive-aged women in a Nigerian community to accept human papillomavirus vaccination for their children. J Obstet Gynaecol Res. 2015;41(10):1621–29. doi: 10.1111/jog.12775. [DOI] [PubMed] [Google Scholar]
- 46.Rashwan H, Ishak I, Sawalludin N. Knowledge and views of secondary school students in Kuala Lumpur on cervical cancer and its prevention. Asian Pac J Cancer Prev. 2013;14(4):2545–49. doi: 10.7314/APJCP.2013.14.4.2545. [DOI] [PubMed] [Google Scholar]
- 47.Tyrell E, Ramsammy-Boyce K. Knowledge and perceptions of HPV and the HPV vaccine among pre-adolescent girls and their guardians in Georgetown, Guyana. West Indian Med J. 2015;64(1):43–48. doi: 10.7727/wimj.2015.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chapman E, Venkat P, Ko E, Orezzoli JP, Del Carmen M, Garner EIO. Use of multimedia as an educational tool to improve human papillomavirus vaccine acceptability-A pilot study. Gynecol Oncol. 2010;118(2):103–07. doi: 10.1016/j.ygyno.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 49.Ferris D, Horn L, Waller JL. Parental acceptance of a mandatory human papillomavirus (HPV) vaccination program. J Am Board Fam Med. 2010;23(2):220–29. doi: 10.3122/jabfm.2010.02.090091. [DOI] [PubMed] [Google Scholar]
- 50.Akmatov MK, Mikolajczyk RT, Kretzschmar M, Krämer A. Attitudes and beliefs of parents about childhood vaccinations in post-soviet countries: the example of kyrgyzstan. Pediatr Infect Dis J. 2009;28(7):637–40. doi: 10.1097/INF.0b013e3181966401. [DOI] [PubMed] [Google Scholar]
- 51.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nowak GJ, Gellin BG, Macdonald NE, Butler R. Addressing vaccine hesitancy: the potential value of commercial and social marketing principles and practices. Vaccine. 2015;33:4204–11. doi: 10.1016/j.vaccine.2015.04.039. [DOI] [PubMed] [Google Scholar]
- 53.Dubé E, Vivion M, MacDonald NE. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Expert Rev Vaccines. 2015;14(1):99–117. doi: 10.1586/14760584.2015.964212. [DOI] [PubMed] [Google Scholar]
- 54.Larson HJ, Jarrett C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007-2012. Vaccine. 2014;32:2150–59. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 55.Gold R, Naleway A, Riedlinger K. Factors predicting completion of the human papillomavirus vaccine series. J Adolesc Heal. 2013;52(4):427–32. doi: 10.1016/j.jadohealth.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 56.Obulaney PA, Gilliland I, Cassells H. Increasing cervical cancer and human papillomavirus prevention knowledge and hpv vaccine uptake through mother/daughter education. J Community Health Nurs. 2016;33(1):54–67. doi: 10.1080/07370016.2016.1120595. [DOI] [PubMed] [Google Scholar]
- 57.Gust DA, Kennedy A, Shui I, Smith PJ, Nowak G, Pickering LK. Parent attitudes toward immunizations and healthcare providers: the role of information. Am J Prev Med. 2005;29(2):105–12. doi: 10.1016/J.AMEPRE.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 58.Baudier F, Beck F, Bourdessol H, Courouve L, Cytrynowicz J, Escalon H, Gautier A, Guilbert P, Lamboy B Legleye S et al. Baromètre santé 2005, Premiers résultats. Saint-Denis Cedex (France): Institut national de prévention et d’éducation pour la santé; 2006. Ed. INPES 2006-85.
- 59.Botelho-Nevers E, Gautret P, Biellik R, Brouqui P. Nosocomial transmission of measles: an updated review. Vaccine. 2012;30(27):3996–4001. doi: 10.1016/J.VACCINE.2012.04.023. [DOI] [PubMed] [Google Scholar]


