Abstract
A 34-year-old multipara presented 72 hours postpartum with acute right-sided abdominal pain. The investigation revealed mild leucocytosis with positive D-dimer and elevated C reactive protein. Abdominal ultrasound and abdominopelvic CT demonstrated an enlarged right ovarian vein with endoluminal thrombus, representing postpartum ovarian vein thrombosis. The patient became asymptomatic 48 hours after starting broad-spectrum antibiotic treatment and anticoagulant therapy. She completed the treatment in ambulatory regimen and control abdominopelvic CT imaging was performed and revealed a duplicated right ovarian vein and a small residual subacute thrombus in the lumen of the distal right ovarian vein. The patient remained asymptomatic in the clinical follow-up.
Keywords: radiology, pregnancy, gynecology
Background
The present case refers to a rare clinical case of postpartum ovarian vein thrombosis in a patient with duplicated right ovarian vein. This entity carries an important risk of significant morbidity and mortality if inadequately managed, and our case was successful in the treatment undertaken and adequate follow-up.
Case presentation
A 34-year-old multipara, presented 72 hours postpartum at our emergency department with severe, acute right-sided abdominal and flank pain, and constipation with 3 days of evolution. She had no vomiting, nausea, anorexia or fever. Abdominal examination revealed intense right lower quadrant pain with rebound tenderness. Gynaecological evaluation was within the normal for the puerperal period.
She had an uncomplicated spontaneous vaginal delivery of a live full-term female; the antenatal and immediate postpartum period were unremarkable.
Neither of her three previous vaginal deliveries was followed by complications.
There was no relevant medical, surgical or family history.
Investigations
Laboratory studies showed mild leukocytosis (white cell count: 13.0×109/ L), with positive D-dimer result (2032 ng/mL; cut-off value:<500 ng/mL) and elevated C reactive protein (115.1 mg/L; cut-off value:<5 mg/L). Blood and urine cultures were negative.
The remainder of the laboratory studies were within normal values.
A diagnosis of acute appendicitis was suspected, and abdominopelvic ultrasound (US) examination was performed immediately.
On US, the right iliac fossa evaluation was limited by overlying bowel gas and the appendix vermiformis could not be visualised.
The right ovary size was minimally increased (62×46 mm) and an enlarged (42×53 mm), hypoechoic, tortuous noncompressible tubular structure was seen extending superiorly from the right adnexa, lateral to the inferior vena cava (IVC), representing the thrombosed right ovarian vein (figure 1).
Figure 1.
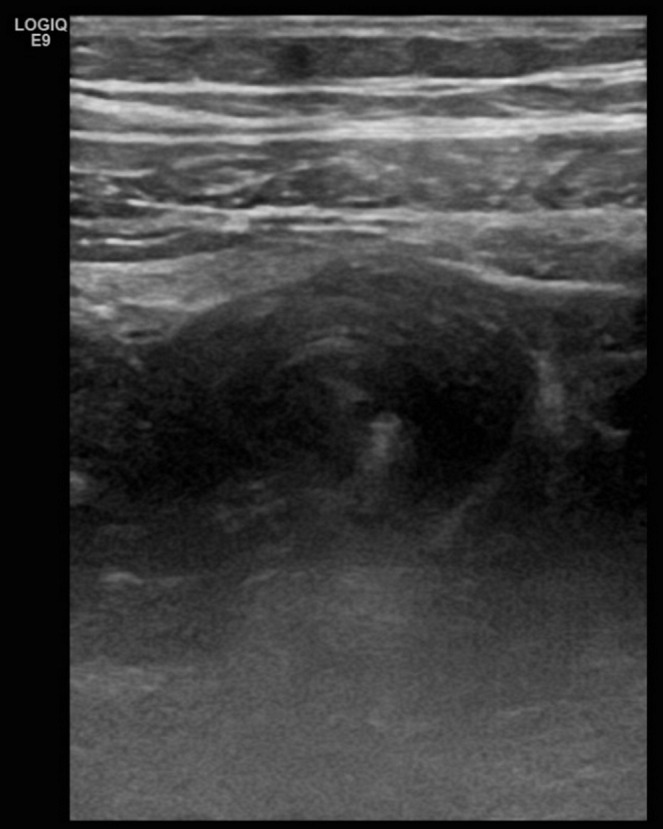
Ultrasound image of the right adnexal region depicting a hypoechoic tubular structure representing the thrombosed right ovarian vein.
The case was discussed with the referring doctor and the patient. Given the lack of timely access to MRI in the emergency setting and the need to exclude the presence of pathology requiring surgical management, the decision was taken to perform a CT study.
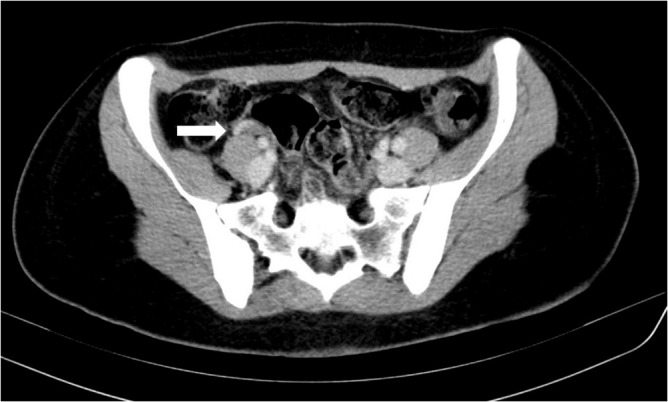
Abdominopelvic CT scan demonstrated an enlarged right ovarian vein, with spontaneously hyperdense endoluminal material in the pre-contrast acquisition phase, and lack of central enhancement after iodine contrast material injection, extending up to the IVC. Inflammatory changes in retroperitoneal fat around right ovarian vein were also present (figure 2).
Figure 2.

Abdominopelvic CT scan with iodine contrast illustrating the marked dilatation and tortuosity of the right ovarian vein (solid arrows), with lack of endoluminal enhancement, representing acute ovarian vein thrombosis.
There was no thrombus in the IVC or in the right renal vein, and the left ovarian vein was also normal. Normal appearing appendix vermiformis was visualised. No evidence of abscess, diverticulitis, bowel perforation, hydronephrosis or ureteral obstruction was found.
Differential diagnosis
The differential diagnosis of ovarian vein thrombosis (OVT) in postpartum period includes acute nephrolithiasis, endometritis, pelvic inflammatory disease, pyelonephritis, appendicitis, tubo-ovarian abscess and torsion of the ovary/pedunculated uterine fibroid.
Treatment
On admission antibiotic therapy was started (Ceftriaxone 1 g every 24 hours plus metronidazole 500 mg every 8 hours) and continued for 10 days.
In addition to antibiotic therapy, therapeutic systemic anticoagulation was administered for 21 days (enoxaparin sodium 60 mg, subcutaneously, every 12 hours).
Outcome and follow-up
The patient became asymptomatic 48 hours after starting broad-spectrum antibiotic treatment and anticoagulant therapy, and was discharged home 4 days after the admission.
She completed the treatment in ambulatory regimen and the clinical follow-up after 2 weeks was uneventful, with laboratory findings within the normal limit.
On the 30th day after the patient was discharged from the hospital, abdominopelvic CT imaging was performed and showed a small remaining subacute thrombus in the lumen of the distal right ovarian vein (figure 3).
Figure 3.
Follow-up abdominopelvic CT scan with iodine contrast detailing the residual endoluminal thrombus (solid arrow) in the inferior segment of the right ovarian vein.
Duplicated right ovarian vein was noted, with adequate patency and drainage of the duplicated vessels into the IVC (figure 4).
Figure 4.

Maximum intensity projection coronal view of follow-up abdominopelvic CT scan with iodine contrast portraying the duplication (solid and open arrows) of the right ovarian vein.
Clinical follow-up was done in 3 months and the patient remained asymptomatic.
Discussion
OVT occurs in 0.02%–0.18% of pregnancies.1 The risk is higher in caesarean delivery (1%–2%) compared with vaginal delivery (0.05%).2 3 Eighty per cent to 90% occur in the right side and multiple factors can contribute to this lateral predisposition, which can be explained by the increased length of the right ovarian vein, lack of retrograde flow and the presence of multiple incompetent valves. Compression of the IVC and right-ovarian vein as they cross the pelvic rim, due to dextrorotation of the uterus during pregnancy, can also be an important feature to this right-sided predominance.4 5
This condition presents usually in the puerperal stage, due to the increased risk of intrapartum endothelial trauma, in addition to a relatively hypercoagulable state and blood flow stasis that occur during pregnancy, which predispose women to postpartum ovarian vein thrombosis.1 3 It may also occur in the prepartum period, after ruptured ectopic pregnancy, abortion and in patients with hydatidiform mole. OVT can also arise in non-puerperal settings such as endometritis, pelvic inflammatory disease, thrombophilia, inflammatory bowel disease, malignancy and pelvic and gynaecological surgeries.6 7
The influence of the IVC vascular malformations as a major risk factor for deep vein thrombosis, by influence on the vascular flow dynamics and contributing to a reduced venous flow velocity, has been confirmed in previous studies, and the same mechanism can be a contributing factor in the present case.8 9
OVT can cause serious complications such as sepsis, IVC thrombosis, renal vein thrombosis and pulmonary thromboembolism which develops in 13% of cases, with a 4% mortality risk.10 11
The ovarian veins are frequently used to identify the ovaries, and are a useful landmark to determine the origin of a pelvic mass (ovarian vascular pedicle sign).12
The gonadal veins are anatomically asymmetric, and this anatomical variations have been shown in about 11% of cases, with preponderance on the left side, aspects suggesting the rarity of the present case.13
The clinical presentation is variable and vague, requiring a high index of suspicion to make the diagnosis. The majority of cases arise in the first 7 days postpartum and fever is present in 80% of the patients. Half of the patients have right lower quadrant abdominal pain and other non-specific symptoms are frequent, such as diffuse abdominal pain, malaise, shortness of breath and ileus.7 14 15
Diagnostic workup of suspected OVT can include US examination, CT and MRI, which can provide non-invasive and sensitive methods to make an accurate diagnosis, avoiding unnecessary surgery. Several studies evaluated the sensitivity and specificity of the three imaging techniques, ranging from 50% to 55.6% and 41.2% to 99% for US, 77.8% to 100% and 62.5% to 99% for CT and 92% to 100% and 100% for MRI, respectively.7 16 17
When OVT is suspected, the initial investigation should be an ultrasound examination, which has no ionising radiation and is vastly available. This imaging modality may confirm the diagnosis, although it has several known limitations, such as, being operator-dependent and frequently limited by overlying bowel gas. The high sensitivity and specificity of abdominopelvic CT scan with intravenous contrast to the diagnosis of this condition makes this study an adequate next investigative step, as it is readily obtainable and is more cost-effective than MRI.18
On sonography, the appearance of a thrombosed ovarian vein is of a tortuous tubular structure with echogenic endoluminal content, extending superiorly from the adnexal region lateral to the lumbar aorta or IVC. Additional information can be provided by Doppler US such as the absence of colour-flow filling and spectral waveform.19
Ovarian thrombosis is visualised on contrast-enhanced CT scans as an enlarged tubular retroperitoneal structure, usually with peripheral enhancement of the vein and lack of endoluminal thrombus enhancement, and follows the characteristic path along the retroperitoneum from the adnexal region to the level of the renal veins. The use of multiplanar reconstructed images (mainly coronal) helps the visualisation of the vein and IVC in its entire length and evaluation of the total thrombotic extent. This cross-sectional technic is also useful to assess for other secondary signs, such as inflammatory fat stranding, uterine enlargement and hematometra/hydrometra, and can exclude other differential diagnosis.20
MRI has a great potential value in the diagnosis and follow-up of OVT cases, being capable of imaging in various planes, having angiographic non-contrast sequences and presenting with great sensitivity to signal alterations in blood flow.11 Usually the angiographic aspect of the thrombus is of a flow void in the vessel, with a T1-weighted low or high intensity (due to methaemoglobin) and T2-weighted intermediate-high signal with a dark peripheral rim.21 22 The capability to identify the paramagnetic effects of iron (in the form of methaemoglobin), leads to the possibility of differentiation between acute (less than 1 week old) and subacute (between 1 week and 1 month) thrombotic material.23
The mainstay of the treatment for OVT is the use of broad-spectrum antibiotics and anticoagulation. The preferable route of administration is the intravenous and agents such as clindamycin, gentamicin, imipenem, cilastatin, ampicillin, sulbactam or the use of second or third-generation cephalosporin in a single-agent therapy or in combination with metronidazole (if concomitant anaerobic infection is suspected), are appropriate to treat this process.8 24 The current consensus states that antibiotic therapy should be continued until the patient has clinically improved (lack of fever for at least 48 hours, resolution of leukocytosis), which usually takes several days to a week.3
There is no clear consensus in the literature regarding optimal dose, length and type of anticoagulation therapy for postpartum OVT. Some authors consider that there are currently no indications to continue the anticoagulation therapy in an outpatient setting in the absence of complications such as pulmonary embolism. Several reports describe a favourable outcome with low-molecular-weight heparin use, but an evidence-based treatment protocol for patients with OVT is not currently available.7 25 26 Surgery and IVC filter placement, are reserved for women with recurrent pulmonary embolism or in whom anticoagulation is contraindicated.2
Currently, there are no generally accepted guidelines about the need of routine thrombophilia testing after ovarian vein thrombosis in postpartum patients.2 3 However some authors recommend that it is usually unnecessary when the thrombosis is located only in the ovarian vein.3 23
The recurrence rate of OVT is unknown, but apparently is similar to that of deep venous thrombosis, thus antenatal prophylactic doses of anticoagulants, continued until 6 weeks postpartum, are recommended in future pregnancies.2 3
Learning points.
Clinicians should be aware to include ovarian vein thrombosis (OVT) in the differential diagnosis of acute abdominal pain and fever in postpartum women, because a delay in diagnosis may lead to significant morbidity.
The symptoms of OVT can mimic other more frequent conditions, and a high index of suspicion is required for the diagnosis of this condition.
Adequate imaging studies are crucial for the adequate evaluation of OVT.
Footnotes
Contributors: JA performed the patient’s ultrasound and CT, and drafted the manuscript. ET helped on the bibliographic research and edited the manuscript. FG and CF critically reviewed the manuscript. All authors approved the final manuscript and agree to be accountable for all aspects of the work.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Dunnihoo DR, Gallaspy JW, Wise RB, et al. . Postpartum ovarian vein thrombophlebitis: a review. Obstet Gynecol Surv 1991;46:415–27. 10.1097/00006254-199107000-00002 [DOI] [PubMed] [Google Scholar]
- 2. Klima DA, Snyder TE. Postpartum ovarian vein thrombosis. Obstet Gynecol 2008;111:431–5. 10.1097/AOG.0b013e318162f6c0 [DOI] [PubMed] [Google Scholar]
- 3. Dougan C, Phillips R, Harley I, et al. . Postpartum ovarian vein thrombosis. The Obstetrician & Gynaecologist 2016;18:291–9. 10.1111/tog.12295 [DOI] [Google Scholar]
- 4. Kearon C. Diagnosis of pulmonary embolism. CMAJ 2003;168:183–94. [PMC free article] [PubMed] [Google Scholar]
- 5. Sinha D, Yasmin H, Samra JS. Postpartum inferior vena cava and ovarian vein thrombosis-a case report and literature review. J Obstet Gynaecol 2005;25:312–3. 10.1080/01443610500106835 [DOI] [PubMed] [Google Scholar]
- 6. Deneux-Tharaux C, Carmona E, Bouvier-Colle MH, et al. . Postpartum maternal mortality and cesarean delivery. Obstet Gynecol 2006;108(3 Pt 1):541–8. 10.1097/01.AOG.0000233154.62729.24 [DOI] [PubMed] [Google Scholar]
- 7. Kominiarek MA, Hibbard JU. Postpartum ovarian vein thrombosis: an update. Obstet Gynecol Surv 2006;61:337–42. 10.1097/01.ogx.0000216564.53044.f1 [DOI] [PubMed] [Google Scholar]
- 8. Bilgin M, Sevket O, Yildiz S, et al. . Imaging of postpartum ovarian vein thrombosis. Case Rep Obstet Gynecol 2012;2012:1–4. 10.1155/2012/134603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chee YL, Culligan DJ, Watson HG. Inferior vena cava malformation as a risk factor for deep venous thrombosis in the young. Br J Haematol 2001;114:878–80. 10.1046/j.1365-2141.2001.03025.x [DOI] [PubMed] [Google Scholar]
- 10. Ruggeri M, Tosetto A, Castaman G, et al. . Congenital absence of the inferior vena cava: a rare risk factor for idiopathic deep-vein thrombosis. Lancet 2001;357:441 10.1016/S0140-6736(00)04010-1 [DOI] [PubMed] [Google Scholar]
- 11. Mintz MC, Levy DW, Axel L, et al. . Puerperal ovarian vein thrombosis: MR diagnosis. AJR Am J Roentgenol 1987;149:1273–4. 10.2214/ajr.149.6.1273 [DOI] [PubMed] [Google Scholar]
- 12. Karaosmanoglu D, Karcaaltincaba M, Karcaaltincaba D, et al. . MDCT of the ovarian vein: normal anatomy and pathology. AJR Am J Roentgenol 2009;192:295–9. 10.2214/AJR.08.1015 [DOI] [PubMed] [Google Scholar]
- 13. Lalwani R, Athavale SA, Chauhan K, et al. . Cadaveric Study of Mode of Termination of Gonadal Veins: Implications for Procedures Utilizing Terminal Ends of Gonadal Veins as Entry Portals. J Nat Sci Biol Med 2017;8:210–2. 10.4103/0976-9668.210005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Martinelli I. Thromboembolism in women. Semin Thromb Hemost 2006;32:709–15. 10.1055/s-2006-951455 [DOI] [PubMed] [Google Scholar]
- 15. Rodger MA, Avruch LI, Howley HE, et al. . Pelvic magnetic resonance venography reveals high rate of pelvic vein thrombosis after cesarean section. Am J Obstet Gynecol 2006;194:436–7. 10.1016/j.ajog.2005.07.044 [DOI] [PubMed] [Google Scholar]
- 16. Twickler DM, Setiawan AT, Evans RS, et al. . Imaging of puerperal septic thrombophlebitis: prospective comparison of MR imaging, CT, and sonography. AJR Am J Roentgenol 1997;169:1039–43. 10.2214/ajr.169.4.9308461 [DOI] [PubMed] [Google Scholar]
- 17. Kubik-Huch RA, Hebisch G, Huch R, et al. . Role of duplex color Doppler ultrasound, computed tomography, and MR angiography in the diagnosis of septic puerperal ovarian vein thrombosis. Abdom Imaging 1999;24:85–91. 10.1007/s002619900448 [DOI] [PubMed] [Google Scholar]
- 18. Nagayama M, Watanabe Y, Okumura A, et al. . Fast MR imaging in obstetrics. Radiographics 2002;22:563–80. 10.1148/radiographics.22.3.g02ma03563 [DOI] [PubMed] [Google Scholar]
- 19. Savader SJ, Otero RR, Savader BL. Puerperal ovarian vein thrombosis: evaluation with CT, US, and MR imaging. Radiology 1988;167:637–9. 10.1148/radiology.167.3.3283835 [DOI] [PubMed] [Google Scholar]
- 20. Virmani V, Kaza R, Sadaf A, et al. . Ultrasound, computed tomography, and magnetic resonance imaging of ovarian vein thrombosis in obstetrical and nonobstetrical patients. Can Assoc Radiol J 2012;63:109–18. 10.1016/j.carj.2010.08.002 [DOI] [PubMed] [Google Scholar]
- 21. Sharma P, Abdi S. Ovarian vein thrombosis. Clin Radiol 2012;67:893–8. 10.1016/j.crad.2012.01.013 [DOI] [PubMed] [Google Scholar]
- 22. Martin B, Mulopulos GP, Bryan PJ. MRI of puerperal ovarian-vein thrombosis (case report). AJR Am J Roentgenol 1986;147:291–2. 10.2214/ajr.147.2.291 [DOI] [PubMed] [Google Scholar]
- 23. Salomon O, Dulitzky M, Apter S. New observations in postpartum ovarian vein thrombosis: experience of single center. Blood Coagul Fibrinolysis 2010;21:16–19. 10.1097/MBC.0b013e32832f2ada [DOI] [PubMed] [Google Scholar]
- 24. Chen KT. Septic pelvic thrombophlebitis In Bloom A, ed UpToDate, 2018. https://www.uptodate.com/contents/septic-pelvic-thrombophlebitis (Retrieved 9 Oct 2018).
- 25. Beigi RH, Wiensenfeld HC. Enoxaparin for postpartum ovarian vein thrombosis. A case report. J Reprod Med 2004;49:55–7. [PubMed] [Google Scholar]
- 26. Wang IK, Lee CH, Yang BY, et al. . Low-molecular-weight heparin successfully treating a nephrotic patient complicated by renal and ovarian vein thrombosis and pulmonary embolism. Int J Clin Pract Suppl 2005;147:72–5. 10.1111/j.1368-504X.2005.00342.x [DOI] [PubMed] [Google Scholar]


