Abstract
Influenza myocarditis is an underappreciated and severe complication of influenza infection, estimated to be present in about 10% of all influenza cases. We present a case of a woman who precipitously died of fulminant influenza myocarditis and then review the historical data, literature and expert recommendations for suspecting and managing influenza myocarditis.
Keywords: influenza, cardiovascular medicine
Background
Influenza myocarditis is an underappreciated and severe complication of influenza infection, estimated to be present in about 10% of all influenza cases. Symptoms vary from asymptomatic to arrhythmias and sudden cardiac death. Early diagnosis and management is critical to preventing fatal cardiac and pulmonary outcomes, but still may not eliminate all deaths associated with this disease.
Case presentation
A middle-aged woman, generally well-appearing but with medical history of asthma, hypertension and morbid obesity, came to our emergency department with worsening shortness of breath, wheezing, cough, fever, chills, headache, chest pain and arthralgias for 2–3 days. She visited a family member with influenza earlier that week, but revealed that she did not obtain influenza vaccination for the current influenza season. Physical examination of lungs revealed moderate respiratory distress with bilateral rhonchi. On initial workup, her influenza A H3 PCR was positive, echocardiogram (ECG) showed normal sinus rhythm at 93 bpm with non-specific ST segment depression in leads V4-6 and inverted T wave on lead III, and chest X-ray showed clear lungs with no pulmonary oedema. Laboratory findings were unremarkable, including normal electrolytes, normal creatine kinase of 71 U/L and three sets of negative troponin T enzymes (<0.01 ng/mL) over 13 hours. She was admitted to the telemetry unit for continued monitoring of the ST segment changes and severe asthma exacerbation and given albuterol, methylprednisolone and oseltamivir.
The next morning, she was found unresponsive with cardiac monitoring showing ventricular fibrillation. Creatine kinase increased to 897 U/L and a fifth set of troponin T enzymes drawn 19 hours after the first set was elevated at 0.95 ng/mL. She was initiated on amiodarone and later esmolol, lidocaine and procainamide were added, but procainamide was discontinued to corrected QT (QTc) interval prolongation. She was sedated, intubated, placed on mechanical ventilation and given norepinephrine and phenylephrine to manage new-onset hypotension. A multiplex respiratory PCR panel for 15 viral and 2 bacterial respiratory pathogens was positive only for influenza H3, but given the progression into severe sepsis, oseltamivir was switched to peramivir and vancomycin and piperacillin-tazobactam were added.
Despite all these interventions, the patient was shocked over 50 times and persisted with incessant ventricular tachycardia. ECG now showed ST and T wave abnormalities with frequent and consecutive ventricular complexes and prolonged QRS complex duration of 72 ms. Repeat chest X-ray showed new onset mild congestive heart failure, which was confirmed by an echocardiogram revealing a left ejection fraction of 45% with normal ventricle size but moderate lateral wall hypokinesis. She was initiated on extracorporeal membrane oxygenation (ECMO) for emergent circulatory support. More cardiac diagnostic tests were performed including a coronary angiogram, which showed normal coronary arteries and an endomyocardial biopsy of the right ventricle, which revealed normal myocardium. But in light of the severe and acute nature of the patient’s cardiac dysfunction, the cardiology team diagnosed the patient with influenza myocarditis with focal involvement.
Differential diagnosis
Asthma exacerbation
Outcome and follow-up
By day 4, the patient had absent corneal reflexes and oculocephalic reflexes. Brain death was confirmed by negative cerebral perfusion scan, as she could not perform an apnea test. On day 6, she was pronounced dead. Autopsy was not performed.
Discussion
Seasonal influenza leads to 140 000–710 000 hospitalisations and 12 000–56 000 deaths in the USA annually. Complications of influenza infections include asthma exacerbations, decompensation from chronic cardiac disease, ear and sinus infections, encephalitis, myocarditis, myositis and rhabdomyolysis, pneumonia and sepsis. Although complications can present in anyone with influenza infection, people who are aged ≤5 years or ≥65 years, have certain chronic medical conditions (such as asthma, cardiac disease, diabetes or obesity), or are pregnant are at higher risk.1
Influenza is generally considered a less common cause of viral myocarditis compared with cardiotropic viruses such as adenovirus, cytomegalovirus, enterovirus (particularly coxsackievirus), Epstein-Barr virus, human herpes virus 6 and parvovirus B19.2 However it is estimated that influenza infection has myocardial involvement in about 10% of all cases, and those rates may be even higher during severe seasons. During the pandemic influenza seasons of 1918, 1957, 1968, rates of influenza myocarditis from 15% to 33% were reported.3–5 In 2009, a review of 58 case reports of H1N1pdm2009 influenza myocarditis found that 62% of those patients had fulminant myocarditis.4
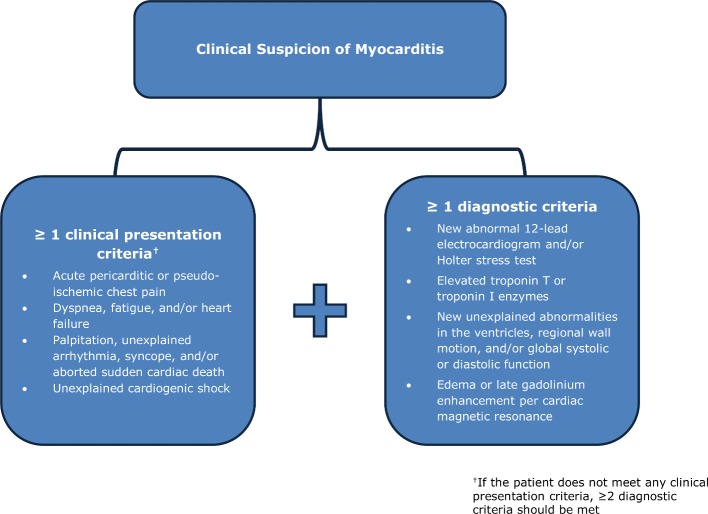
Influenza myocarditis can be difficult to diagnose as the clinical presentation can vary from asymptomatic to sudden cardiac death. Additionally, cardiac MRI (cMRI) and/or endomyocardial biopsy are preferred diagnostic tools for myocarditis and should be obtained as soon as possible, but their sensitivity can be poor. A large European epidemiological study of patients with acute or chronic myocarditis found that 72% had dyspnoea, 32% had chest pain, and only 18% had arrhythmias. Of the 3055 endomyocardial biopsies obtained in the study, only 17.2% of were positive for inflammation and 11.8% were positive for viral pathogens.6 7 Given these diagnostic challenges, the American Heart Association recommends to clinically suspect myocarditis if ≥1 clinical presentation and ≥1 diagnostic criteria are found (see figure 1).8
Figure 1.
American Heart Association diagnostic criteria for clinically suspected myocarditis.
Treatments for myocarditis include heart failure management, immunosuppressants, antiarrhythmics, ECMO and even cardiac transplant depending on the symptoms, severity and cause. Prolonged aerobic activity can increase risk of cardiac death, so competitive sports should be avoided for 3–6 months after diagnosis. Non-steroidal anti-inflammatory drugs should also be avoided due to increased risk of inflammation and death.8 9
Neuraminidase inhibitors may have limited utility in influenza myocarditis as patients can present days to weeks after initial influenza infection, well outside the optimal treatment initiation period of 48 hours after symptom onset. But a study of H1N1pdm2009-infected mice showed significantly improved survival as well as improved histological exams and decreased viral genome in cardiac and pulmonary tissues in peramivir-treated mice versus the control group.10 Larger clinical trials are still ongoing to assess the role of neuraminidase inhibitors and other antivirals in acute and chronic viral myocarditis.
Influenza vaccination remains a key intervention in preventing complications such as influenza myocarditis by curbing the virus’s ability to replicate and mutate. Influenza vaccine has been shown to reduce the risk of recurrent myocardial infarction in patients with documented coronary artery disease. A meta-analysis of 6735 patients with varying degrees of cardiovascular disease found a significantly lower risk of major adverse cardiovascular events in patients who received influenza vaccination versus those who did not. The greatest benefit was seen among high-risk patients with active coronary disease.11
It is worth noting that rare cases of influenza vaccination-associated myocarditis have been reported, including with inactivated vaccine.12 Nonetheless, a prospective cohort study found no cases of confirmed or possible myocarditis in 189 patients who received a trivalent inactivated influenza vaccine.13 Thus while providers should be aware of this rare adverse event from influenza vaccination, it should not deter them from recommending influenza vaccination to all eligible patients.
In our patient, initial acute dyspnoea, chest tightness and non-specific ST segment changes on ECG prompted admission for cardiac monitoring. By day 2, it was clear that she had fulminant myocarditis despite a negative endomyocardial biopsy due to the new onset of incessant arrhythmias, cardiogenic shock and congestive heart failure plus the newly elevated creatine kinase and troponin T enzymes. Despite no known history of cardiac disease, our patient’s history of asthma, hypertension and morbid obesity put her at high risk for cardiac disease and severe complications from influenza, to which she ultimately succumbed.
Although it is mostly asymptomatic, influenza myocarditis is estimated to be present in about 10% of all influenza cases. Urgent evaluation for influenza myocarditis should be performed in all known or suspected influenza patients with acute or worsening cardiac dysfunction, especially in severe influenza seasons when treatment or vaccination can be less effective. cMRI or endomyocardial biopsy should be obtained as soon as possible, but if unavailable or negative despite positive signs and symptoms, the recommendation of American Heart Association for myocarditis diagnosis can be used. Neuraminidase inhibitors may help if given early in disease progression, but this has not been well-studied in humans. Finally, it is important to make all patients aware that influenza infection can cause fatal complications, such as influenza myocarditis, to increase annual influenza vaccination rates.
Learning points.
Influenza myocarditis is estimated to occur in up to 10% of all influenza cases and can cause severe cardiac dysfunction and death.
In influenza patients with acute or severe cardiac dysfunction, urgent evaluation for myocarditis with continuous cardiac monitoring is strongly suggested.
If cardiac MRI or endomyocardial biopsy cannot be obtained or are negative despite positive cardiac signs and symptoms, the American Heart Association recommends to clinically suspect and treat for myocarditis based on the presence of clinical presentation and diagnostic criteria.
All patients need to be informed of the potentially fatal complications of influenza infection, such as influenza myocarditis, to encourage annual influenza vaccination.
Footnotes
Contributors: NS prepared the discussion and figure and drafted the manuscript for submission. SS prepared the case section. MC advised both writers on writing and content and edited all sections.
Funding: This study was funded by Albert Einstein College of Medicine, Yeshiva University (839345).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not required.
References
- 1. Centers for Disease Control and Prevention [Internet]. About flu. Atlanta: U.S. Department of Health; https://www.cdc.gov/flu/about/index.html [Google Scholar]
- 2. Dennert R, Crijns HJ, Heymans S. Acute viral myocarditis. Eur Heart J 2008;29:2073–82. 10.1093/eurheartj/ehn296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mamas MA, Fraser D, Neyses L. Cardiovascular manifestations associated with influenza virus infection. Int J Cardiol 2008;130:304–9. 10.1016/j.ijcard.2008.04.044 [DOI] [PubMed] [Google Scholar]
- 4. Ukimura A, Satomi H, Ooi Y, et al. Myocarditis associated with influenza A H1N1pdm2009. Influenza Res Treat 2012;2012:1–8. 10.1155/2012/351979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rezkalla SH, Kloner RA. Influenza-related viral myocarditis. WMJ 2010;109:209–13. [PubMed] [Google Scholar]
- 6. Hufnagel G, Pankuweit S, Richter A, et al. The European Study of Epidemiology and Treatment of Cardiac Inflammatory Diseases (ESETCID). First epidemiological results. Herz 2000;25:279–85. 10.1007/s000590050021 [DOI] [PubMed] [Google Scholar]
- 7. Friedrich MG, Marcotte F. Cardiac magnetic resonance assessment of myocarditis. Circ Cardiovasc Imaging 2013;6:833–9. 10.1161/CIRCIMAGING.113.000416 [DOI] [PubMed] [Google Scholar]
- 8. Bozkurt B, Colvin M, Cook J, et al. Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association. Circulation 2016;134:e579–e646. 10.1161/CIR.0000000000000455 [DOI] [PubMed] [Google Scholar]
- 9. Schultz JC, Hilliard AA, Cooper LT, et al. Diagnosis and treatment of viral myocarditis. Mayo Clin Proc 2009;84:1001–9. 10.1016/S0025-6196(11)60670-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ukimura A, Ooi Y, Kanzaki Y. The neuraminidase inhibitor peramivir ameliorates myocarditis induced by influenza a (h1n1pdm) virus in a murine model. Clin Microbiol 2015;4:201. [Google Scholar]
- 11. Udell JA, Zawi R, Bhatt DL, et al. Association between influenza vaccination and cardiovascular outcomes in high-risk patients: a meta-analysis. JAMA 2013;310:1711–20. 10.1001/jama.2013.279206 [DOI] [PubMed] [Google Scholar]
- 12. Kim Y-J, Bae J-I, Ryoo SM, et al. Acute fulminant myocarditis following influenza vaccination requiring extracorporeal membrane oxygenation. Korean J Crit Care Med 2018. https://doi.org/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Engler RJ, Nelson MR, Collins LC, et al. A prospective study of the incidence of myocarditis/pericarditis and new onset cardiac symptoms following smallpox and influenza vaccination. PLoS One 2015;10:e0118283 10.1371/journal.pone.0118283 [DOI] [PMC free article] [PubMed] [Google Scholar]