Abstract
Minimally invasive approaches are safe, feasible, and often recommended as the initial choice in the surgical management of Crohn's disease. However, a consensus has not been reached as the ideal approach in the surgical treatment of complex and recurrent Crohn's disease. Laparoscopy may provide advantages such as shorter length of stay and decreased postoperative pain and result in less adhesion formation in patients with complex disease. Robotic techniques may be beneficial in selected patients for completion proctectomy, providing better visualization in the narrow pelvis and increased dexterity. Decision of surgical technique should be made on a case-by-case basis.
Keywords: robotic completion proctectomy, laparoscopic ileocecal resection, fistulizing Crohn's disease
Definitions and History
Management of Crohn's disease begins with medical treatment. However, regardless of the advancements in medical therapy and newly introduced agents, during the course of the disease, surgery may be required in up to 80% of the patients. 1 Besides refractory medical treatment, indications for surgery in Crohn's disease may range from complications due to medical therapy to complications from the disease itself such as abscesses, perforation, and fistulas.
Penetrating disease is described as a behavioral subtype by the Montreal Classification. 2 Description of complex and penetrating Crohn's disease may include perforating disease with fistulas, intra-abdominal abscesses, and even free perforations. Behavioral pattern of disease may progress over time and this may lead to a requirement of surgery. Management of complex Crohn's disease remains to be a challenging topic for the practicing surgeon.
Guidelines and Recommendations
Practice guidelines from Europe and United States have looked into the surgical management of complex Crohn's disease and discussed the evidence regarding minimally invasive approaches. According to clinical practice guidelines published by American College of Colon and Rectal Surgeons in 2007, laparoscopic surgery was equivalent to open approach. 3 It is also stated that if penetrating ileocolonic disease was not complicated, resection can either be performed with laparoscopic approach or open surgery.
Clinical Practice Guidelines published by ASCRS in 2015 state that laparoscopic approach can be safely used when the adequate surgical expertise and experience is available with a level 1B recommendation (strong recommendation based on moderate-quality evidence). 4
Additionally, according to 2016 European Crohn's and Colitis Organization, laparoscopy can be preferred for ileocolonic resections in Crohn's disease where appropriate expertise is available; however, the role of laparoscopy can be considered for more complex disease. In more complex cases or for recurrent resection, sufficient evidence does not exist recommending laparoscopic surgery. 5 Thus, consensus is formed for implementing laparoscopy in straightforward Crohn's disease, but application in more complex disease is still debated.
Laparoscopic Approach
Laparoscopic surgery for Crohn's disease was first described by Milsom et al in 1993 in nine patients. 6 Since that time, laparoscopy has gradually increased in patients with Crohn's disease. Application for complex disease remains a controversial topic because complicated anatomy with fistulas or abscesses might make the laparoscopic approach challenging especially for novice laparoscopist. 7
Laparoscopic surgery is favored because it provides benefits such as shorter operative time and better cosmetic results when compared with open surgery. Lower degree of adhesion formation after laparoscopic surgery compared with open surgery 8 could be another beneficial property for complex Crohn's disease patients in the short and long term. It may be possible that as we see further advancements in medical therapy for Crohn's disease, time of surgery could be delayed. Subsequently, this may lead to more and more patients presenting with more complex disease.
Studies looking at feasibility of laparoscopic surgery in patients with complex Crohn's disease are mostly limited by small numbers. 9 10 11 12 13 A summary of literature reporting use of laparoscopic surgery in complex Crohn's disease is given in Table 1 . 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 One of the reported series with large case series is by Bellolio et al, reporting a total of 293 patients with perforating disease, 251 of who had a fistula and were included only if it was the initial surgery. Most common site of fistula was sigmoid colon along with fistulas to bladder and enterocutaneous fistulas. The group with the perforating disease reported longer operative times ( p < 0.001) and higher conversion rates ( p < 0.001). They also reported higher incidence of temporary ileostomy creation rates ( p = 0.002). 24
Table 1. Studies reporting results with laparoscopic approach for complex Crohn's disease.
| Study year | Authors | Number of patient population | Study design | Results |
|---|---|---|---|---|
| 1997 | Wu et al 14 | 116 (46 lap with 24 complex vs. 70 open) | Prospective |
Longer operative time in open (
p
< 0.05), higher blood loss in open (
p
< 0.05)
LOS shorter in lap ( p < 0.01) |
| 2003 | Hasegawa et al 15 | 52 (61 lap, 45 primary vs. 16 recurrent, -7 lap vs. 9 open) | Retrospective |
Shorter operative time in open group (
p
= 0.042)
Shorter operative time in primary group ( p = 0.012) |
| 2004 | Uchikoshi et al 16 | 43 for recurrent disease (17 lap vs. 6 HALS vs. 20 open) | Retrospective |
Flatus earliest in HALS (
p
< 0.05)
LOS shortest in HALS ( p < 0.01) |
| 2004 | Moorthy et al 17 | 48 (57 lap procedures, 26 recurrent vs. 31 primary) | Retrospective |
Conversion higher in recurrent (
p
= 0.02)
Days to soft diet shorter in primary ( p = 0.03) |
| 2007 | Okabayashi et al 12 | 107 (124 procedures, 91 lap, 67 initial, and 24 recurrence vs. 33 open) | Retrospective | Complications comparable Recurrence of CD more in laparoscopy group ( p = 0.001) Stricturing disease more commonly underwent laparoscopy ( p = 0.035) |
| 2009 | Goyer et al 11 | 124 (all lap, 54 complex vs. 70 simple) | Prospective |
Conversion rate higher in complex disease group (
p
< 0.01)
Mean operative time longer in complex disease group ( p < 0.05) |
| 2009 | Melton et al 13 | 104 with ISF (29 lap vs. 75 open) | Retrospective |
Lap group had lower rates of stoma creation (
p
= 0.04)
LOS, complications comparable |
| 2010 | Holubar et al 18 | 40 (30 lap-completed vs. 10 lap-converted) | Retrospective |
LOS shorter in lap (
p
= 0.002)
Days to soft diet shorter in lap ( p = 0.03) |
| 2010 | Brouquet et al 19 | 57 (62 reoperations, 29 lap vs. 33 open) | Retrospective |
Need for associated procedures more often in open (
p
= 0.003)
Intraoperative intestinal injuries more in lap ( p = 0.01) |
| 2011 | Chaudhary et al 20 | 59 lap (30 recurrent vs. 29 primary) | Retrospective |
Operative time longer in recurrent (
p
< 0.01)
Postoperative complication rates comparable |
| 2011 | Pinto et al 21 | 130 lap (80 primary resection vs. 50 for recurrent disease) | Retrospective | LOS comparable Postoperative complication rates comparable |
| 2012 | Aytac et al 9 | 52 with prior midline incisions (26 lap vs. 26 open) | Retrospective Case-match |
Operative time, LOS, overall morbidity comparable |
| 2012 | Huang et al 22 | 130 lap (48 with prior surgery vs. 82 without prior surgery) | Retrospective | Rate of conversion to open surgery comparable Postoperative complication rates comparable |
| 2013 | Beyer-Berjot et al 10 | 33 lap (11 fistulizing vs. 22 control nonfistulizing) | Retrospective Case-match |
LOS, rate of conversion and major complications comparable |
| 2016 | Manabe et al 23 | 56 lap (25 simple CD vs. 31 complex CD) | Retrospective |
Longer incision length in complex CD (
p
= 0.004)
Incidence of severe postoperative complications higher in complex CD ( p = 0.026) |
Abbreviations: CD, Crohn's disease; HALS, hand-assisted laparoscopic surgery; ISF, ileosigmoid fistula; lap, laparoscopic; LOS, length of stay.
Another series reported by Goyer et al described laparoscopic ileocolonic resection to be safe and feasible for complex Crohn's disease in 54 patients compared with 70 patients without complex disease. It is advocated that complexity of the disease is not necessarily a contraindication for laparoscopy. 11
A recent study by Manabe et al compared laparoscopic surgery in simple and complex Crohn's disease patients. Twenty-two patients among the 31 in the complex disease group had penetrating disease. There was no difference between the groups in terms of operative time, estimated blood loss, and length of stay. However, in the complex Crohn's group, Clavien-Dindo grade 3 and 4 complications were seen more often (12.9 vs. 0.0%, p = 0.026). 23 Beyer-Berjot et al also reported 11 patients with complex fistulizing disease who underwent laparoscopic surgery and perioperative outcomes were compared with the nonfistulizing disease group and found comparable, supporting use of laparoscopic surgery in fistulizing complex Crohn's disease. 10
In most patients, Crohn's disease has a progressive course and it is very likely that these patients may develop fibrostenotic or penetrating disease during the course of disease that requires surgery. Patients with complex disease may require reoperation after the initial resection. Preferring the minimally invasive approach with careful patient selection may help decrease adhesions and possible complications and allow easier reoperations in the following operations. These patients may have a midline incision which could affect the outcomes of the second surgery. In a study from our institution by Aytac et al, laparoscopy was compared with open approach in patients with previous midline incisions. A total of 29 patients with penetrating disease were included, 12 in laparoscopy and 17 in open group. Compared with the open surgery group, patients who underwent laparoscopy and had a previous midline incision were comparable in terms of operative time, estimated blood loss, overall morbidity, length of stay, reoperation, and readmission rates. 9 The laparoscopy group had less wound infections, which should be highlighted as an advantage for patients with Crohn's colitis.
Immunologic responses in Crohn's disease are altered 25 due the pathophysiology of the disease itself and also as a result of medical treatment with immunosuppressive and/or biologic agents prior to surgery. This altered response may also negatively affect the physiology of wound healing. Laparoscopic surgery may be beneficial in avoiding morbidity such as wound infections in these patients. Also overall low body mass indexes and poor nutritional status, 26 especially in younger patients, may be associated with delayed wound healing. This population may benefit from minimal tissue trauma as in minimally invasive approaches.
Laparoscopic Approach in Complex Crohn's Disease
Recent studies report favorable outcomes with laparoscopic approach for complex Crohn's disease. It is important to note that when managing patients with complex disease, their condition should be stabilized before proceeding with laparoscopic surgical resection. 23 This may aid the surgeon in clear visualization of the surgical field and minimize conversions. Studies show that during the course of disease, 70% of patients may fall into the category of complex disease in 10 years of follow-up. 27 As the optimal conditions for surgical treatment are rarely reached in patients with complex disease, decision of surgical method should be done on a case-by-case basis and minimally invasive surgery can be the preferred decision in selected cases. Although published literature shows favorable results comparable with open surgery in complex disease, 10 11 23 the decision to proceed with laparoscopy should be made carefully and the experience of the surgeon should be one of the main factors to consider in addition to the individual characteristics of the patient and the indications for surgery.
Finding the best method of treatment for fistulizing disease is difficult in the sense that it has many variables that need to be considered such as patients' age, nutritional status, and any previous surgery, which will affect the surgical approach. Despite the favorable properties of laparoscopic approach, there are certain limitations such as necessity for a large incision and extensive adhesions that make laparoscopic approach nonapplicable. Although laparoscopic approach is promising, it should be carefully utilized by highly experienced laparoscopists.
Single Incision Laparoscopic Surgery
Single incision laparoscopic surgery (SILS) can be considered a subtype of laparoscopic surgery in which the laparoscopic instruments are introduced from a single incision site, umbilicus or stoma site. 28 It allows the entire operation to be completed through one incision which is also used as the extraction site. 29 Mizushima et al reported 24 patients with structuring and perforating disease who underwent SILS for ileal resection, ileocecal resection, stoma closure, and stricturoplasty. Perioperative outcomes were found to be comparable besides blood loss, which was higher in the perforating disease group. 28
According to other studies comparing SILS with conventional laparoscopy, it is safe and feasible in patients with complex Crohn's disease, resulting in less need for pain medication, 29 shorter operative time, 30 and with technical advantages over multiport technique. 31
Single incision technique can be the procedure of choice especially in pediatric population and adolescent patients who have an indication for diverting ileostomy. Safe use of SILS was advocated with comparable perioperative outcomes with open surgery. 32
Role of Robotic Technique
The robotic platform enables the surgeon to have better visualization, enhanced control of the surgical field, and improved dexterity. 33 These benefits of the robotic approach is highly advantageous for operating in the narrow pelvis, such as proctectomy. Better viewing angles may help, particularly in complex disease, in removing adhesions or resection of fistulizing disease without damaging adjacent anatomical structures. This will help avoid nerve injury and related functional and sexual complications with the close-up visuals provided by the robotic camera. As the robotic approach is gaining popularity, the question of feasibility for patients with complex Crohn's disease remains to be answered.
Robotic platform could be useful in performing proctectomy in patients with complex disease. Completion proctectomy is indicated in Crohn's patients who have resistant perianal disease with penetrating behavior. 33 34 It is a technically challenging procedure requiring expertise. Robotic approach may help overcome the ergonomical and visual shortcomings of laparoscopic surgery especially in the deep and narrow pelvis. 33 35
Treatment of choice in these patients with anorectal involvement is generally proctocolectomy with permanent ileostomy. 34 Performing robotic completion proctectomy consists of similar steps as the laparoscopic approach. Port placement takes place under direct vision with the robotic camera. Five to six ports are usually inserted that include the camera and the assistant ports ( Fig. 1 ). Docking from the left side of the patient is performed for the pelvic portion of the surgery. If all steps of the operation are performed with the robotic platform, multiple dockings can be necessary.
Fig. 1.
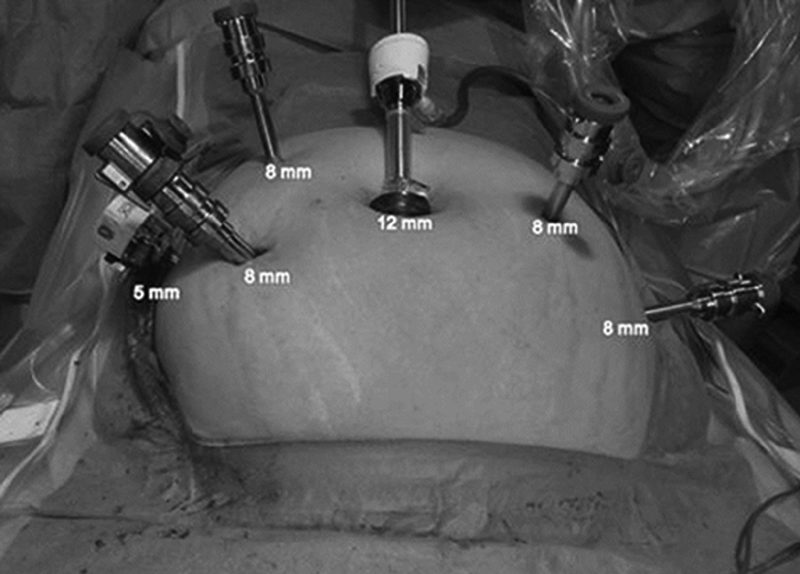
Port placement for robotic completion proctectomy.
Current literature is scant about application of robotic surgery in patients with complex Crohn's disease. In a study comparing 30-day morbidity between robotic and laparoscopic groups in rectal resection, only 2 patients had Crohn's disease among 79 patients of robotic approach group. 36 In a previous study from our institution, 21 patients undergoing laparoscopic proctectomy were matched with robotic proctectomy group and 4 patients in each group had a diagnosis of Crohn's disease. Operative time was longer ( p = 0.008) and estimated blood loss was higher ( p = 0.02) in the robotic proctectomy group. Rate of conversion, return of bowel movements, and hospital stay were found to be similar between robotic and laparoscopy groups. 33
During completion proctectomy for these patients, intramesorectal or total mesorectal excision can be performed based on existing dysplasia. Another advantage of robotic approach for performing completion proctectomy in these patients could be the possible better preservation of nerves adjacent to the surgical plane when performing intramesorectal or total mesorectal excision. 33
Certain disadvantages of robotic approach for completion proctectomy are that single docking is usually not sufficient and multiple docking is necessary which can be time consuming. However, it should be noted that these disadvantages should not push the surgeon away from this approach, as new innovations allow multiquadrant docking and may help overcome some of these issues. 33
Another disadvantage as shown in our previous study was the longer operative time with the robotic approach. As the learning curve is reached and robotic surgical training becomes more available, this disadvantage may disappear. Using laparoscopy and robot together to compensate for each other's limitations may shorten the operative time by avoiding multiple docking and provide the surgeon with the advantages of robot when working in the narrow pelvis.
Conclusion
Minimally invasive approach in the management of complex Crohn's disease is gaining popularity. Guidelines and published studies support the use of laparoscopic surgery in Crohn's disease, but full adoption of this technique in complex disease remains to be investigated. Robotic surgery may provide the surgeon and the patient with certain benefits, but extended research is necessary to clearly evaluate the benefits and feasibility of this technique. A multidisciplinary discussion for the patients with complex disease to select the right approach is necessary.
Footnotes
Conflict of Interest None declared.
References
- 1.Neumann P A, Rijcken E. Minimally invasive surgery for inflammatory bowel disease: Review of current developments and future perspectives. World J Gastrointest Pharmacol Ther. 2016;7(02):217–226. doi: 10.4292/wjgpt.v7.i2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silverberg M S, Satsangi J, Ahmad Tet al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology Can J Gastroenterol 200519(Suppl A):5A–36A. [DOI] [PubMed] [Google Scholar]
- 3.Strong S A, Koltun W A, Hyman N H, Buie W D; Standards Practice Task Force of The American Society of Colon and Rectal Surgeons.Practice parameters for the surgical management of Crohn's disease Dis Colon Rectum 200750111735–1746. [DOI] [PubMed] [Google Scholar]
- 4.Strong S, Steele S R, Boutrous M et al. Clinical practice guideline for the surgical management of Crohn's disease. Dis Colon Rectum. 2015;58(11):1021–1036. doi: 10.1097/DCR.0000000000000450. [DOI] [PubMed] [Google Scholar]
- 5.Gomollón F, Dignass A, Annese V et al. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn's Disease 2016: Part 1: Diagnosis and medical management. J Crohn's Colitis. 2017;11(01):3–25. doi: 10.1093/ecco-jcc/jjw168. [DOI] [PubMed] [Google Scholar]
- 6.Milsom J W, Lavery I C, Böhm B, Fazio V W. Laparoscopically assisted ileocolectomy in Crohn's disease. Surg Laparosc Endosc. 1993;3(02):77–80. [PubMed] [Google Scholar]
- 7.Neumann P A, Rijcken E J, Bruewer M. Current status of laparoscopic surgery for patients with Crohn's disease. Int J Colorectal Dis. 2013;28(05):599–610. doi: 10.1007/s00384-013-1684-y. [DOI] [PubMed] [Google Scholar]
- 8.Dowson H M, Bong J J, Lovell D P, Worthington T R, Karanjia N D, Rockall T A. Reduced adhesion formation following laparoscopic versus open colorectal surgery. Br J Surg. 2008;95(07):909–914. doi: 10.1002/bjs.6211. [DOI] [PubMed] [Google Scholar]
- 9.Aytac E, Stocchi L, Remzi F H, Kiran R P. Is laparoscopic surgery for recurrent Crohn's disease beneficial in patients with previous primary resection through midline laparotomy? A case-matched study. Surg Endosc. 2012;26(12):3552–3556. doi: 10.1007/s00464-012-2361-x. [DOI] [PubMed] [Google Scholar]
- 10.Beyer-Berjot L, Mancini J, Bege T et al. Laparoscopic approach is feasible in Crohn's complex enterovisceral fistulas: a case-match review. Dis Colon Rectum. 2013;56(02):191–197. doi: 10.1097/DCR.0b013e31826fedeb. [DOI] [PubMed] [Google Scholar]
- 11.Goyer P, Alves A, Bretagnol F, Bouhnik Y, Valleur P, Panis Y. Impact of complex Crohn's disease on the outcome of laparoscopic ileocecal resection: a comparative clinical study in 124 patients. Dis Colon Rectum. 2009;52(02):205–210. doi: 10.1007/DCR.0b013e31819c9c08. [DOI] [PubMed] [Google Scholar]
- 12.Okabayashi K, Hasegawa H, Watanabe M et al. Indications for laparoscopic surgery for Crohn's disease using the Vienna Classification. Colorectal Dis. 2007;9(09):825–829. doi: 10.1111/j.1463-1318.2007.01294.x. [DOI] [PubMed] [Google Scholar]
- 13.Melton G B, Stocchi L, Wick E C, Appau K A, Fazio V W. Contemporary surgical management for ileosigmoid fistulas in Crohn's disease. J Gastrointest Surg. 2009;13(05):839–845. doi: 10.1007/s11605-009-0817-7. [DOI] [PubMed] [Google Scholar]
- 14.Wu J S, Birnbaum E H, Kodner I J, Fry R D, Read T E, Fleshman J W.Laparoscopic-assisted ileocolic resections in patients with Crohn's disease: are abscesses, phlegmons, or recurrent disease contraindications? Surgery 199712204682–688., discussion 688–689 [DOI] [PubMed] [Google Scholar]
- 15.Hasegawa H, Watanabe M, Nishibori H, Okabayashi K, Hibi T, Kitajima M. Laparoscopic surgery for recurrent Crohn's disease. Br J Surg. 2003;90(08):970–973. doi: 10.1002/bjs.4136. [DOI] [PubMed] [Google Scholar]
- 16.Uchikoshi F, Ito T, Nezu R et al. Advantages of laparoscope-assisted surgery for recurrent Crohn's disease. Surg Endosc. 2004;18(11):1675–1679. doi: 10.1007/s00464-004-8802-4. [DOI] [PubMed] [Google Scholar]
- 17.Moorthy K, Shaul T, Foley R J. Factors that predict conversion in patients undergoing laparoscopic surgery for Crohn's disease. Am J Surg. 2004;187(01):47–51. doi: 10.1016/j.amjsurg.2002.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Holubar S D, Dozois E J, Privitera A et al. Laparoscopic surgery for recurrent ileocolic Crohn's disease. Inflamm Bowel Dis. 2010;16(08):1382–1386. doi: 10.1002/ibd.21186. [DOI] [PubMed] [Google Scholar]
- 19.Brouquet A, Bretagnol F, Soprani A, Valleur P, Bouhnik Y, Panis Y. A laparoscopic approach to iterative ileocolonic resection for the recurrence of Crohn's disease. Surg Endosc. 2010;24(04):879–887. doi: 10.1007/s00464-009-0682-1. [DOI] [PubMed] [Google Scholar]
- 20.Chaudhary B, Glancy D, Dixon A R. Laparoscopic surgery for recurrent ileocolic Crohn's disease is as safe and effective as primary resection. Colorectal Dis. 2011;13(12):1413–1416. doi: 10.1111/j.1463-1318.2010.02511.x. [DOI] [PubMed] [Google Scholar]
- 21.Pinto R A, Shawki S, Narita K, Weiss E G, Wexner S D. Laparoscopy for recurrent Crohn's disease: how do the results compare with the results for primary Crohn's disease? Colorectal Dis. 2011;13(03):302–307. doi: 10.1111/j.1463-1318.2009.02133.x. [DOI] [PubMed] [Google Scholar]
- 22.Huang R, Valerian B T, Lee E C. Laparoscopic approach in patients with recurrent Crohn's disease. Am Surg. 2012;78(05):595–599. [PubMed] [Google Scholar]
- 23.Manabe T, Ueki T, Nagayoshi K et al. Feasibility of laparoscopic surgery for complex Crohn's disease of the small intestine. Asian J Endosc Surg. 2016;9(04):265–269. doi: 10.1111/ases.12287. [DOI] [PubMed] [Google Scholar]
- 24.Bellolio F, Cohen Z, Macrae H M et al. Outcomes following surgery for perforating Crohn's disease. Br J Surg. 2013;100(10):1344–1348. doi: 10.1002/bjs.9212. [DOI] [PubMed] [Google Scholar]
- 25.Kim D H, Cheon J H. Pathogenesis of inflammatory bowel disease and recent advances in biologic therapies. Immune Netw. 2017;17(01):25–40. doi: 10.4110/in.2017.17.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burnham J M, Shults J, Semeao E et al. Body-composition alterations consistent with cachexia in children and young adults with Crohn disease. Am J Clin Nutr. 2005;82(02):413–420. doi: 10.1093/ajcn.82.2.413. [DOI] [PubMed] [Google Scholar]
- 27.Louis E, Collard A, Oger A F, Degroote E, Aboul Nasr El Yafi F A, Belaiche J. Behaviour of Crohn's disease according to the Vienna classification: changing pattern over the course of the disease. Gut. 2001;49(06):777–782. doi: 10.1136/gut.49.6.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mizushima T, Nakajima K, Takeyama H et al. Single-incision laparoscopic surgery for stricturing and penetrating Crohn's disease. Surg Today. 2016;46(02):203–208. doi: 10.1007/s00595-015-1145-z. [DOI] [PubMed] [Google Scholar]
- 29.Gardenbroek T J, Verlaan T, Tanis P J et al. Single-port versus multiport laparoscopic ileocecal resection for Crohn's disease. J Crohn's Colitis. 2013;7(10):e443–e448. doi: 10.1016/j.crohns.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 30.Rijcken E, Mennigen R, Argyris I, Senninger N, Bruewer M. Single-incision laparoscopic surgery for ileocolic resection in Crohn's disease. Dis Colon Rectum. 2012;55(02):140–146. doi: 10.1097/DCR.0b013e31823d0e0d. [DOI] [PubMed] [Google Scholar]
- 31.Leo C A, Samaranayake S F, Chandrasinghe P C, Shaikh I A, Hodgkinson J D, Warusavitarne J H. Single port laparoscopic surgery for complex Crohn's disease is safe with a lower conversion rate. J Laparoendosc Adv Surg Tech A. 2017;27(11):1095–1100. doi: 10.1089/lap.2016.0567. [DOI] [PubMed] [Google Scholar]
- 32.Huntington J T, Boomer L A, Pepper V K, Diefenbach K A, Dotson J L, Nwomeh B C. Single-incision laparoscopic surgery (SILS) for children with Crohn's disease. Pediatr Surg Int. 2016;32(05):459–464. doi: 10.1007/s00383-016-3875-4. [DOI] [PubMed] [Google Scholar]
- 33.Rencuzogullari A, Gorgun E, Costedio M et al. Case-matched comparison of robotic versus laparoscopic proctectomy for inflammatory bowel disease. Surg Laparosc Endosc Percutan Tech. 2016;26(03):e37–e40. doi: 10.1097/SLE.0000000000000269. [DOI] [PubMed] [Google Scholar]
- 34.de Buck van Overstraeten A, Wolthuis A M, Vermeire S et al. Intersphincteric proctectomy with end-colostomy for anorectal Crohn's disease results in early and severe proximal colonic recurrence. J Crohn's Colitis. 2013;7(06):e227–e231. doi: 10.1016/j.crohns.2012.07.023. [DOI] [PubMed] [Google Scholar]
- 35.Miller A T, Berian J R, Rubin M, Hurst R D, Fichera A, Umanskiy K. Robotic-assisted proctectomy for inflammatory bowel disease: a case-matched comparison of laparoscopic and robotic technique. J Gastrointest Surg. 2012;16(03):587–594. doi: 10.1007/s11605-011-1692-6. [DOI] [PubMed] [Google Scholar]
- 36.Feinberg A E, Elnahas A, Bashir S, Cleghorn M C, Quereshy F A. Comparison of robotic and laparoscopic colorectal resections with respect to 30-day perioperative morbidity. Can J Surg. 2016;59(04):262–267. doi: 10.1503/cjs.016615. [DOI] [PMC free article] [PubMed] [Google Scholar]


