Abstract
Background.
Sexual minorities (experience significant health disparities across a variety of mental, behavioral, and physical health indicators. Yet, an understanding of the etiology and progression of sexual minority health disparities across the lifespan is limited.
Methods.
We used the US National Epidemiologic Survey of Alcohol and Related Conditions III to evaluate the association between sexual minority status and seven past-year health outcomes (alcohol use disorder, tobacco use disorder, drug use disorder, major depressive episode, generalized anxiety disorder, sexually transmitted infection, and cardiovascular conditions). To do this, we used unadjusted and adjusted logistic regression among our study sample (n=30,999; aged 18–65) and time-varying effect models to evaluate how sexual orientation differences in these outcomes vary across adulthood.
Results.
Relative to heterosexuals, sexual minorities had elevated odds of past-year alcohol use disorder and drug use disorder across all ages (18 to 65 years), though the magnitude of the disparity varies by age. Sexual minorities were also more likely to experience higher rates of major depressive episode, generalized anxiety disorder, tobacco use disorder, sexually transmitted infection, and cardiovascular disease, but only at specific ages.
Conclusion.
Sexual minority health disparities vary appreciably across the adult lifespan, thus elucidating critical periods for focused prevention efforts.
Keywords: LGB, sexual minority, public health, health inequalities, epidemiology, public health, sexually transmitted diseases, substance abuse
INTRODUCTION
Sexual minorities (SMs) are disproportionately vulnerable to a variety of poor health outcomes. In 2016, the National Institute on Minority Health and Health Disparities at the US National Institutes of Health formally recognized sexual and gender minorities as a population for health disparities research [1]. Sexual-orientation-related disparities span the spectrum of health outcomes, including physical health, mental health, and substance use [2–4]. Compared to heterosexual adults, for example, sexual minorities are 2–5 times as likely to have substance use disorders [5], 2 times as likely to indicate mood or anxiety disorders [6], and 2.5 times as likely to report lifetime suicide attempts [7]. A recent review documented greater cardiovascular disease risk among SM men and women [8], largely attributed to health conditions such as poor mental health and substance use. SM men are also at increased risk for both sexually transmitted infections (STI) and Human Immunodeficiency Virus (HIV) [2] and SM women are more likely to test positive for Hepatitis C [2].
A growing body of evidence suggests that sexual-orientation-related health disparities are largely driven by internal (e.g., internalized homophobia; expectations of rejection) and external (e.g., discrimination, victimization) stressors that uniquely impact sexual minorities across the life span -often referred to as minority stress [9–11]. Studies that utilize quasi-natural experimental designs, for example, highlight the deleterious effects of enacting anti-LGB policy for the health and well-being of SMs [12].There are, however, unique developmental considerations that must be taken into account when considering risk factors that contribute to the timing of sexual-orientation-related disparities. Schools, for example, are finite contexts that confer risk for victimization and bullying of SM youth [13], which can have lasting, but diminishing effects for mental health as adolescence age into adulthood [14]. SMs also have to navigate “coming out” – or disclosing their sexual identity to family and friends which is oftentimes stressful [15] – which may lead to rejection and consequent mental and behavioral health risk [16]. Despite evidence on the existence of sexual-orientation-related health disparities and the developmental nature of the associated risk factors, the progression of these health inequities across the lifespan is not completely understood.
Even with increased attention to SM health, significant research gaps remain [17]. Little is known, for example, about how health disparities [2,3,7] vary across the lifespan for sexual minorities, despite evidence that mental, behavioral, and physical health conditions vary in their onset and course over the life course [18–21]. Alcohol use disorder, for example, increases during late adolescence into young adulthood, peaks during the mid- twenties, and steadily declines across subsequent ages [21]. Considering that theoretical mechanisms of sexual orientation-related health disparities also vary by age [22], might the degree to which heterosexuals and SMs differ in these health-related outcomes change across the life course? Importantly, because there are developmental differences in the onset and prevalence of specific health conditions, researchers who aggregate data across broad age ranges (e.g., 18–65) may be over- or underestimating the degree to which SMs may be at risk for poor mental, behavioral, and physical health. Understanding how health conditions fluctuate across the lifespan would allow research efforts to more accurately examine developmentally-sensitive mechanisms that contribute to SMs’ increased vulnerability, and inform the development of tailored prevention and intervention strategies.
We hypothesize that health disparities between heterosexual and SM adults will vary by age, such that there are age ranges of greater vulnerability for specific health outcomes among SMs. To evaluate these hypotheses, we used nationally representative cross-sectional data and an innovative analytic method, the time-varying effect model (TVEM) [23], to examine whether SM and heterosexual differences in seven well-established sexual orientation related disparities differ across ages 18–65 [2–8]: Outcomes include past-year alcohol, tobacco, and drug use disorders, major depressive episode, generalized anxiety disorder, cardiovascular problems, and STIs.
METHODS
Participants and Procedure
Data are from the National Epidemiologic Survey of Alcohol and Related Conditions–III (NESARC-III), a nationally representative, cross-sectional study of the non-institutionalized adult population in the US collected in 2012–2013 [24]. To ensure an adequate sample size at all ages, we restricted our analytic sample to participants aged 18–65 resulting in a final unweighted sample size of 30,999 participants.
Measures
Our primary predictor was SM status. SM status is complex, comprised of identity, behavior, and attraction. Despite significant research [25], there is not strong scientific consensus on how to best classify sexual minorities. Because we hypothesize that the disparities examined are related to minority stress, and because it is likely having same-sex attraction, behavior, or SM identity could result in experiences of internal and external stigma, we used broad criteria to identify sexual minorities. We identified SMs using an inclusive classification strategy, where any endorsement of same-sex attraction, same-sex behavior, or SM identity (i.e., lesbian/gay or bisexual) resulted in classification as SM.
Given the paucity of research documenting developmental differences in sexual-orientation-related health disparities, we assessed age-specific differences in the prevalence of seven health outcomes that have been shown to systematically vary across sexual orientation [2–8]. These included three measures of past-year substance use disorders (i.e., alcohol [AUD], tobacco [TUD], and drug use disorder [DUD]) and two measures of mental health disorders (i.e., major depressive episode [MDE] and generalized anxiety disorder [GAD]). Substance use and mental health disorders were classified using the Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5) [16], which aligns with the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V) (American Psychiatric Association, 2013) diagnostic criteria [24]. For each substance, participants were asked if they had experienced 11 symptoms, and were coded as having specific substance use disorders if they experienced at least 2 symptoms within the past year. For AUD, questions referred to whether symptoms were caused by drinking alcohol. For TUD, the questions referred to “tobacco and nicotine, including cigarettes, cigars, pipes, snuff, chewing tobacco, or e-cigarettes.” DUD indicated disorder associated with the use of sedatives, cannabis, opioids, cocaine, stimulants, hallucinogen, inhalant/solvent, club drugs, heroin, or other drugs. We also examined two measures of past-year physical health: self-reported diagnoses of sexually transmitted infections (STI) and cardiovascular health via self-reported heart attack or any other form of heart disease.
Analysis
First, we used weighted logistic regression to calculate the unadjusted and adjusted associations between SM status and each health outcome. Adjusted models controlled for biological sex (male or female), race/ethnicity (White, Black, Hispanic, Other race), education (high school diploma or less, some college or more), household income (<$20,000; $20,000 – $34,999; $35,000 – $69,999; $70,000+), and region of country (Northeast, Midwest, South, West). Finally, we used weighted logistic time-varying effect models (TVEM) [27] to estimate age-specific associations between SM status and each health outcomes from ages 18 to 65. The weighted TVEM macro applies normalized weights [27,28]. TVEM is a flexible, semi- parametric model that estimates rates and associations as a flexible function of age This method allows associations between predictors and outcomes to be modeled flexibly across continuous age, providing precise age ranges during which associations are the strongest [23,27]. We ran seven independent models with SM status predicting each outcome across age. For each model the best-fitting number of knots (which define the complexity of each age function) for the intercept and SM status parameters were selected using AIC and BIC criteria. Models included biological sex, race/ethnicity, education, income, and US region as time-invariant effects to account for potential confounding. Results are presented as figures to best display age-specific estimates and time-varying shape of associations. Thus, for each outcome we present a figure showing adjusted odds ratios (OR) and 95% confidence intervals (CI) corresponding to the age- specific associations between SM status and health outcomes.
This study utilized a limited access dataset obtained from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and was approved by the Pennsylvania State University Institutional Review Board (IRB #4463).
RESULTS
Sample Characteristics
Ten percent of the sample indicated same-sex attraction, same-sex behavior, and/or a gay/lesbian or bisexual identity, and thus 3,349 individuals were classified as SM. Among the SM participants, 31% endorsed same-sex attraction, same-sex behavior, or a SM identity. Two percent of the SM sample endorsed same-sex behavior and SM identity (but not same-sex attraction), 20% endorsed same-sex attraction and same-sex behavior (but not SM identity), 5% endorsed same-sex attraction and a SM identity (but not same-sex behavior). Finally, 30% of the SM sample endorsed only same-sex attraction, 12% endorsed only same-sex behavior, and 1% exclusively endorsed a SM identity.
With respect to demographic variables, SMs were similar to heterosexuals. All health outcomes were more prevalent among the SMs. A quarter (24%) of SMs met the criteria for a past-year AUD, compared to 15% of heterosexuals. Past-year anxiety disorders, major depressive episodes, and STIs were both approximately twice as prevalent among SMs. with respective prevalences of 10% and 22%, compared to 5% and 12% among heterosexuals. . STDs affected 2% of SM in the past year, compared to <1% of heterosexuals. Five percent of SMs reported negative cardiovascular outcomes in the past year, compared to 4% of heterosexuals (Table 1).
Table 1.
Weighted Sample Characteristics (Unweighted N=36,309)
| Sexual Minority n=3,349 |
Heterosexual n=27,650 |
|
|---|---|---|
| Age | ||
| 18–24 | 20.7% | 15.0% |
| 25–34 | 24.4% | 20.1% |
| 35–44 | 18.0% | 20.7% |
| 45–54 | 18.8% | 22.5% |
| 55–65 | 18.1% | 21.8% |
| Biological Sex | ||
| Male | 40.1% | 50.1% |
| Female | 59.9% | 49.9% |
| Race/Ethnicity | ||
| White | 63.7% | 63.5% |
| Black | 13.4% | 12.4% |
| Hispanic | 14.9% | 16.3% |
| Other | 8.0% | 7.7% |
| Education | ||
| High School diploma or less | 35.1% | 37.2% |
| Some College or more | 64.9% | 62.8% |
| Household Income (Annual) | ||
| Less than $20,000 | 26.6% | 18.8% |
| $20,000 – 34,999 | 19.1% | 17.5% |
| $35,000 – 69,999 | 26.5% | 28.1% |
| $70,000 or more | 27.8% | 35.6% |
| Region of Country | ||
| Northeast | 19.1% | 18.0% |
| Midwest | 19.9% | 21.5% |
| South | 33.3% | 37.4% |
| West | 27.7% | 23.0% |
| Alcohol Use Disorder | ||
| Yes | 24.2% | 15.2% |
| No | 75.9% | 84.8% |
| Tobacco Use Disorder | ||
| Yes | 28.9% | 21.6% |
| No | 71.1% | 78.4% |
| Drug Use Disorder | ||
| Yes | 8.8% | 4.0% |
| No | 91.2% | 96.0% |
| Major Depressive Episode | ||
| Yes | 21.7% | 11.7% |
| No | 78.3% | 88.3% |
| Generalized Anxiety Disorder | ||
| Yes | 9.9% | 5.2% |
| No | 90.1% | 94.8% |
| Cardiovascular Outcome | ||
| Yes | 4.5% | 3.6% |
| No | 95.4% | 96.1% |
| Sexually Transmitted Infection | ||
| Yes | 2.3% | 0.7% |
| No | 97.4% | 98.9% |
Substance Use Disorders
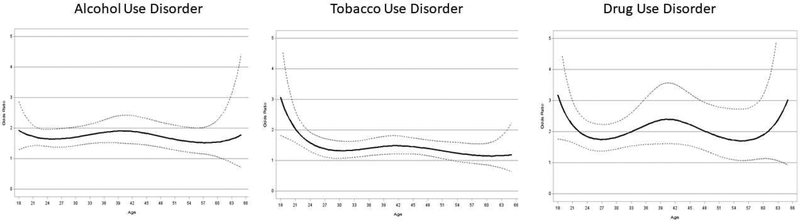
The unadjusted weighted odds ratio (OR) for the association between SM status and AUD was 1.78 (95% confidence interval (CI):1.61,1.96). The adjusted odds ratio (aOR) indicated that SMs were 1.83 (95% CI: 1.65,2.03) times as likely to indicate a past-year AUD. TVEM analyses revealed that the adjusted association did not vary appreciably by age (Figure 1a). SM adults generally had 2 times greater adjusted odds of meeting the criteria for a past-year AUD compared to heterosexuals, and this association was significant until age 63.
Figure 1.
Age-varying associations between sexual minority status and past-year alcohol use disorder, tobacco use disorder, and drug use disorder, controlling for biological sex, race/ethnicity, education, household income, and region of country. Dashed lines indicate 95% confidence intervals.
Unadjusted and adjusted weighted logistic regression models indicated that SMs had a greater likelihood of past-year TUD relative to heterosexuals (OR:1.47, 95% CI:1.32,1.64; aOR:1.48, 95% CI:1.34,1.64). TVEM analyses indicated that SM status was most strongly associated with having a past-year TUD at earlier ages, and this disparity declined over age – remaining significant until age 54 (Figure 1b). For example, SMs had 3 times greater odds of meeting the criteria for a past-year TUD at age 18 and 1.5 times greater adjusted odds at age 27.
Generally, SMs had about 2–2.5 times the odds of meeting criteria for past-year DUD (OR:2.32, 95% CI: 1.94,2.79; aOR:2.22, 95% CI: 1.84,2.68). TVEM models indicated that SM status was significantly associated with DUD across all adult ages, with some fluctuation in effect size (Figure 1c). SM young adults had approximately 3 times greater adjusted odds of past-year DUD, but declined sharply until age 25.
Mental Health Disorders
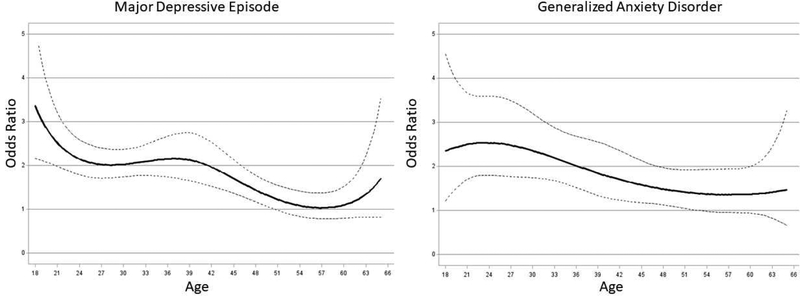
The crude association between SM status and MDE was 2.09 (95% CI:1.89, 2.31); an association that was slightly attenuated after adjustment (aOR:2.00, 95% CI:1.81,2.19). TVEM analyses revealed that the association between SM status and MDE was strongest at younger ages, and declined with age (Figure 2a). At age 18, SM status was associated with approximately 3 times greater adjusted odds of having an MDE in the past year, compared to 1.5 times greater odds at age 25 through 40, and was no longer significant by age 52.
Figure 2.
Age-varying associations between sexual minority status and past-year major depressive episode and generalized anxiety disorder, controlling for biological sex, race/ethnicity, education, household income, and region of country. Dashed lines indicate 95% confidence intervals.
Logistic regression models revealed significant sexual orientation differences in past-year GAD (OR:2.02, 95% CI:1.73,2.36; aOR:1.81, 95% CI:1.56,2.10), but the disparity varied by age. The relationship was strongest in the late twenties with an aOR of approximately 2.5, before declining and plateauing around age 40. The association was non-significant by age 53 (Figure 2b).
Physical Health
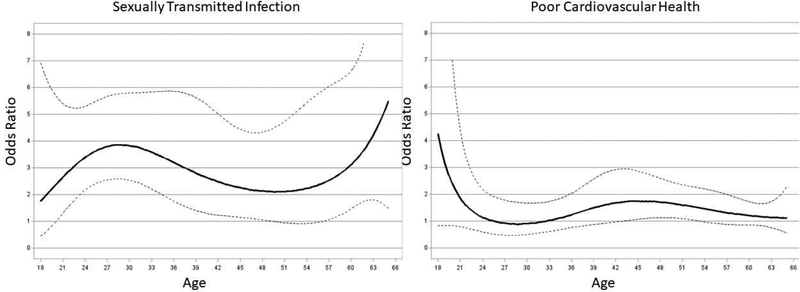
SMs had more than three times the odds of reporting a STI in the past year in both unadjusted (OR:3.57, 95% CI:2.72,4.67) and adjusted (aOR:3.19, 95% CI:2.42,4.22) models.. TVEM analyses indicated that SM status was significantly associated with STI between ages 20 and 49 (Figure 3a), but most strongly in the late twenties. SMs were 4 times as likely to report STI in their late twenties, but only two times as likely at age 18 and at age 45. .
Figure 3.
Age-varying associations between sexual minority status and past-year sexually transmitted infections and poor cardiovascular health, controlling for biological sex, race/ethnicity, education, household income, and region of country. Dashed lines indicate 95% confidence intervals.
SM status was significantly associated with poor cardiovascular health in unadjusted (OR:1.26, 95% CI:1.00,1.59), but not in adjusted (aOR:1.23, 95% CI:0.97,1.56) logistic regression models. Results from adjusted TVEM revealed that the disparity was significant at some ages: heterosexual and sexual minorities aged 43–53 (Figure 3b) statistically differed, with the largest difference at age 45.
DISCUSSION
Consistent with a large and growing body of evidence, we find that SMs experience striking health disparities across a variety of mental, behavioral, and physical health conditions. Our findings, however, demonstrate that the degree to which SMs are more likely to experience poor health varies by age. Findings identify critical periods of vulnerability for the development of these disparities and suggest potential ages to target for prevention and intervention.
Similar to prior research [5–7], we found that SMs have significantly higher odds of AUD and DUD throughout adulthood with slight variation across ages. Yet, our results from TVEM analyses also indicate that the odds of a major depressive episode, anxiety disorder, TUD, STI, and cardiovascular disease among sexual minorities vary by age.
The associations between SM status and depression and anxiety are strongest around age 20 and age 24, respectively. Elevated risk in the early twenties may be related to experience of “coming out” which, for many, occurs in the late teens and early twenties. Furthermore, these youth may still be dealing with the residual effects of school-based victimization, which is more common for SM youth [13] and the effect of which last (at least) into the early 20s [14]. . The decreasing disparity in mental health across adulthood may reflect SMs exiting hostile school and family environments, while simultaneously seeking out supportive networks and communities [14,29,30].SMs have significantly higher odds of TUD in early adulthood (ages 18–28) and the disparity narrows with age. One possible explanation for this narrowing disparity may be that smoking rates among SMs may decline after early adulthood. A key driver of smoking among SMs may be sexual minority stressors, including discrimination [31], which is reported at highest rates in early adulthood [32]. It could also be that the narrowing disparity is not due to decreased tobacco use among SMs as they age, but instead due to elevated rates of tobacco use among older heterosexuals. A recent report from the Centers for Disease Control and Prevention (CDC) indicates that 13% of adults aged 18–24, 18% of adults aged 25–44, and 18% of adults aged 45–64 smoke cigarettes [33]. Notably, this mimics the shape of the trajectories we found for the examined mental health outcomes (GAD and MDE). We hypothesize that these similar trajectories reflect the well-documented relationship between smoking and mental health [34], where persons with mental illness are approximately two times as likely to smoke [23], perhaps as a form of self-medication [35], although smoking may increase the risk of certain mental disorders [36]. We also noted unique patterns for AUD and DUD whereby disparities were largest during 18–20 and then again around the age of 40. Generally, rates of alcohol and drug use peak in early adulthood and decline as people age [21]. It is possible that the sexual-orientation-related disparities in early adulthood are, in part, due to unique milestones for SM adolescents and young adults (e.g., “coming out”), coinciding with normative increases in substance use. Elevated risk for AUD and DUD during midlife, however, is counter to what we might expect and encourage future research attention in to its predictors. This may, for example, be an instance where the explanation may be more related to cohort, rather than a developmental, differences [37].
Finally, cardiovascular disparities were smaller in magnitude and age-specific. The odds of cardiovascular disease were significantly higher for SMs, relative to heterosexuals, from the mid-40s to early 50s. This likely reflects the natural trajectory of cardiovascular disease, where risk of cardiovascular disease increases with age. Thus, the relationship between SM status and cardiovascular health maps on to an age period of heightened risk in the overall population. Given previous findings of significant associations between stress and cardiometabolic risk among SM groups [8], but not among heterosexuals [38], as well as lifelong experiences of sexual-minority-specific discrimination [39], disparities in cardiovascular heath may reflect the effect of chronic stress for SM populations or other health-related behaviors linked to stress (e.g., substance use). Future research should investigate the role of minority stress on the significant cardiovascular health disparity, such that future programs might intervene on that link.
This study had several limitations. First, it is widely recognized that there is heterogeneity in the SM population. Health disparities, for example, have been shown to differ by sexual identity (i.e. gay vs. bisexual) [5, 44] and by biological sex [2,7]. Others have applied an intersectionality framework to examine how SM health disparities differ across racial/ethnic groups [40]. In this analysis, we did not examine the differences within sexual minorities, but instead call attention to developmental differences in sexual orientation health disparities more broadly. Thus, the degree to which disparities vary by age may also significantly differ across subpopulations within the larger SM community is an important focus for future research. Second, we used an inclusive definition of SM status by including those who report any same-sex attraction, behavior, or SM identity [41]. This is a conservative approach, and thus may yield an underestimate of SM health disparities. Future research should explore whether these disparities may be stronger among particular subgroups of SMs. Third, the interpretation of these analyses is limited by our inability to separate age effects from cohort effects. Future longitudinal studies that explicitly collect measures of sexual orientation and related experiences (e.g., discrimination) are needed to better untangle these potentially related and confounding effects. Fourth, our substance abuse measures combine all drug use disorders in to a single item. Although useful in providing the overall prevalence of drug use disorder among SM adults, drug disorders have varying etiologies, prevalence, and contributing factors. Thus, future research examining specific drug abuse prevalence by age is needed to make more directly claims for this population. Finally, the NESARC-III does not include measures of gender identity; we were therefore unable to examine disparities by gender-identity. The absence of gender identity measures in national data have stymied scientific understanding of this population; the measurement of gender identity in future national studies would provide an unprecedented opportunity to address these knowledge gaps.
Future research should continue to explore the etiology of these disparities and, specifically, addressable social factors that contribute to them. The minority stress theory [11, 42], for example, posits that health disparities affecting SMs may be explained by minority specific stress unique to SMs (e.g., internalized stigma, discrimination) [11,43]. It is likely that exposure to SM-related stressors vary as people age, potentially leading to different health outcomes across the life course. Future work should also explore how age-specific disparities vary across other sociodemographic factors known to affect the health of sexual minorities. Furthermore, many of these health factors are co-occurring and interrelated (e.g., smoking and mental health) [34]. Although this analysis focused on addressing each health condition as an independent outcome, future research focused on the developmental timing of risk may aim to understand the co-occurrence of outcomes.
Sexual-orientation-related health disparities persist in most cases across adulthood, but vary in strength by age. These findings inform the timing and targeting of prevention and intervention efforts, suggest focused research efforts on developmental periods where disparities are most salient for SMs, and highlight the need for investigations into developmentally-situated mechanisms that contribute to SM health.
ACKNOWLEDGEMENTS & CONFLICT OF INTEREST STATEMENT:
This study was funded in part by award P50DA039838 and award DA039854 from the National Institute on Drug Abuse. This research was further supported by the National Institute on Alcohol Abuse and Alcoholism grant number F32AA023138. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This manuscript was prepared using a limited access dataset obtained from the National Institute on Alcohol Abuse and Alcoholism and does not reflect the opinions or views of NIAAA or the U.S. Government.
The authors have no conflicts of interest to report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
ETHICS APPROVAL:
This study was approved by The Pennsylvania State University Institutional Review Board (#4463).
Contributor Information
Cara Exten Rice, The Methodology Center, Pennsylvania State University, 404 HHD Building, University Park, PA 16802.
Sara A. Vasilenko, Human Development and Family Science, David B. Falk College of Sport and Human Dynamics, Syracuse University, Syracuse, NY, USA.
Jessica N. Fish, Department of Family Science, School of Public Health, University of Maryland, Austin, TX, USA.
Stephanie T. Lanza, Department of Biobehavioral Health, The Methodology Center, The Pennsylvania State University, University Park, PA, USA.
REFERENCES
- 1.National Institute of Minority Health and Health Disparities (NIMHD). Sexual and gender minorities formally designated as a health disparity population for research purposes. 2016; Retrieved February 28, 2017, from https://www.nimhd.nih.gov/about/directors-corner/message.html
- 2.Operario D, Gamarel KE, Grin BM, Lee JH, Kahler CW, Marshall BDL, et al. Sexual Minority Health Disparities in Adult Men and Women in the United States: National Health and Nutrition Examination Survey, 2001–2010. Am J Public Health 2015; 105(10):e27–34. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26270288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lick DJ, Durso LE, Johnson KL. Minority Stress and Physical Health Among Sexual Minorities. Perspect Psychol Sci 2013;8(5):521–48. [DOI] [PubMed] [Google Scholar]
- 4.Plöderl M, Tremblay P. Mental health of sexual minorities: a systematic review. Int Rev Psychiatry 2015;27:367–85. [DOI] [PubMed] [Google Scholar]
- 5.McCabe SE, Hughes TL, Bostwick WB, West BT, Boyd CJ. Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction 2009;104(8):1333–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hatzenbuehler ML, Keyes KM, Hasin DS. State-level policies and psychiatric morbidity in lesbian, gay, and bisexual populations. Am J Public Health 2009;99(12):2275–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, et al. A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry 2008;8:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caceres BA, Brody A, Luscombe RE, Primiano JE, Marusca P, Sitts EM, et al. A Systematic Review of Cardiovascular Disease in Sexual Minorities. Am J Public Health 2017;107(4):570–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldberg AE, Smith JZ. Stigma, social context, and mental health: lesbian and gay couples across the transition to adoptive parenthood. J Couns Psychol 2011;58(1):139–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lick DJ, Tornello SL, Riskind RG, Schmidt KM, Patterson CJ. Social Climate for Sexual Minorities Predicts Well-Being Among Heterosexual Offspring of Lesbian and Gay Parents. Sex Res Soc Policy 2012; 9(2):99–112. [Google Scholar]
- 11.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 2003;129(5):674–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hatzenbuehler ML, Mclaughlin KA, Keyes KM, Hasin DS. The Impact of Institutional Discrimination on Psychiatric Disorders in Lesbian, Gay, and Bisexual Populations: A Prospective Study. American Journal of Public Health 2010; 100(3): 452–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Toomey RB, Russell ST, Denny T. The Role of Sexual Orientation in School-Based Victimization: A Meta-Analysis. Youth Soc. 2016;48(2):176–201. doi: 10.1177/0044118X13483778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Russell ST, Toomey RB, Ryan C, Diaz RM. Being out at school: The implications for school victimization and young adult adjustment. Am J Orthopsychiatry 2014;84(6):635–43. [DOI] [PubMed] [Google Scholar]
- 15.Russell ST, Fish JN. Mental Health in Lesbian, Gay, Bisexual, and Transgender (LGBT) Youth. Annu Rev Clin Psychol. 2016;12:465–487. doi: 10.1146/annurev-clinpsy-021815-093153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baams L, Grossman AH, Russell ST. Minority stress and mechanisms of risk for depression and suicidal ideation among lesbian, gay, and bisexual youth. Dev Psychol. 2015;51(5):688–696. doi: 10.1037/a0038994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Institute of Medicine (US) Committee on Lesbian, Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding National Academies Press (US); 2011. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22013611 [PubMed] [Google Scholar]
- 18.Maggs JL, Ph D, Schulenberg JE. Trajectories of alcohol use during the transition to adulthood. Alcohol Resarch Heal. 2005;28(4):195–201. https://pubs.niaaa.nih.gov/publications/arh284/195-201.pdf. [Google Scholar]
- 19.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of Major Depressive Disorder. Arch Gen Psychiatry. 2005;62(10):1097. doi: 10.1001/archpsyc.62.10.1097 [DOI] [PubMed] [Google Scholar]
- 20.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30(1):133–154. doi: 10.1093/epirev/mxn002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vasilenko SA, Evans-Polce RJ, Lanza ST. Age trends in rates of substance use disorders across ages 18–90: Differences by gender and race/ethnicity. Drug Alcohol Depend. 2017;180:260–264. doi: 10.1016/j.drugalcdep.2017.08.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robinson JP, Espelage DL, Rivers I. Developmental trends in peer victimization and emotional distress in LGB and heterosexual youth. Pediatrics. 2013;131(3):423–430. doi: 10.1542/peds.2012-2595 [DOI] [PubMed] [Google Scholar]
- 23.Lanza ST, Vasilenko SA, Russell MA. Time-varying effect modeling to address new questions in behavioral research: Examples in marijuana use. Psychol Addict Behav 2016;30(8):939–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grant BF, Goldstein RB, Smith SM, Jung J, Zhang H, Chou SP, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): reliability of substance use and psychiatric disorder modules in a general population sample. Drug Alcohol Depend 2015;148:27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gender Identity in U.S. Surveillance (GenIUSS) Group. Best Practices for Asking Questions to Identify Transgender and Other Gender Minority Respondents on Population-Based Surveys. 2014:68 http://williamsinstitute.law.ucla.edu/wp-content/uploads/geniuss-report-sep-2014.pdf. Accessed August 17, 2016. [Google Scholar]
- 26.Hasin DS, Greenstein E, Aivadyan C, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): procedural validity of substance use disorders modules through clinical re-appraisal in a general population sample. Drug and Alcohol Dependence 2015;0:27–33. doi: 10.1016/j.drugalcdep.2014.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dziak JJ, Li R, Wagner AT. WeightedTVEM SAS Macro for Accommodating Survey Weights and Clusters. University Park: The Methodology Center, Penn State; 2017. Retrieved from http://methodology.psu.edu [Google Scholar]
- 28.Kaplan D, Ferguson AJ. On the utilization of sample weights in latent variable models. Struct Equ Model A Multidiscip J. 1999;6(4):305–321. doi: 10.1080/10705519909540138 [DOI] [Google Scholar]
- 29.D’Augelli AR, Hershberger SL, Pilkington NW. Lesbian, gay, and bisexual youth and their families: disclosure of sexual orientation and its consequences. Am J Orthopsychiatry 1998;68(3):361-71-5. [DOI] [PubMed] [Google Scholar]
- 30.Frost DM, Meyer IH, Schwartz S. Social support networks among diverse sexual minority populations. Am J Orthopsychiatry 2016;86(1):91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Youatt EJ, Johns MM, Pingel ES, Soler JH, Bauermeister JA. Exploring Young Adult Sexual Minority Women’s Perspectives on LGBTQ Smoking. J LGBT Youth. 2015;12(3):323–342. doi: 10.1080/19361653.2015.1022242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rice CE, Fish JN, Russell ST, Lanza ST. A Modern Snapshot of Discrimination Experiences among Sexual Minorities in a National Sample of Adults in the United States. J Homosexuality (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jamal A, Phillips E, Gentzke AS, et al. Current Cigarette Smoking Among Adults — United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(2):53–59. doi: 10.15585/mmwr.mm6702a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. JAMA 2000;284(20):2606–10. [DOI] [PubMed] [Google Scholar]
- 35.Carmody TP. Affect Regulation, Tobacco Addiction, and Smoking Cessation. J Psychoactive Drugs. 1989;21(3):331–342. doi: 10.1080/02791072.1989.10472175 [DOI] [PubMed] [Google Scholar]
- 36.Johnson JG, Cohen P, Pine DS, Klein DF, Kasen S, Brook JS. Association Between Cigarette Smoking and Anxiety Disorders During Adolescence and Early Adulthood. JAMA. 2000;284(18):2348. doi: 10.1001/jama.284.18.2348 [DOI] [PubMed] [Google Scholar]
- 37.Hammack PL, Frost DM, Meyer IH, Pletta DR. Gay Men’s Health and Identity: Social Change and the Life Course. Arch Sex Behav. 2018;47(1):59–74. doi: 10.1007/s10508-017-0990-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hatzenbuehler ML, Slopen N, McLaughlin KA, McLaughlin KA. Stressful life events, sexual orientation, and cardiometabolic risk among young adults in the United States. Heal Psychol 2014;33(10):1185–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fish JN, Rice CE, Lanza ST, Russell ST. “ Using TVEM to Explore Social Etiology: Sexual Minority Discrimination and Suicidality Across the Lifespan”. Society for Prevention Research 25th Annual Meeting2017. Washington, D.C. [Google Scholar]
- 40.Mereish EH, Bradford JB. Intersecting identities and substance use problems: sexual orientation, gender, race, and lifetime substance use problems. J Stud Alcohol Drugs 2014;75(1):179–88. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24411810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lindley LL, Walsemann KM, Carter JW. The Association of Sexual Orientation Measures With Young Adults’ Health-Related Outcomes. Am J Public Health [Internet]. 2012. June [cited 2017 Jul 14];102(6):1177–85. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22021310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Meyer IH (2007). Prejudice and discrimination as social stressors In Meyer IH & Northridge ME (Eds.), The health of sexual minorities (pp. 242–267). Washington, DC: APA [Google Scholar]
- 43.Meyer IH, Schwartz S, Frost DM. Social patterning of stress and coping: Does disadvantaged social statuses confer more stress and fewer coping resources? Soc Sci Med 2008;67(3):368–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bostwick WB, Boyd CJ, Hughes TL, McCabe SE. Dimensions of sexual orientation and the prevalence of mood and anxiety disorders in the United States. Am J Public Health. 2010;100(3):468–475. doi: 10.2105/AJPH.2008.152942 [DOI] [PMC free article] [PubMed] [Google Scholar]