Abstract
Coronary artery disease (CAD) is a life-threatening condition that, unless treated at an early stage, can lead to congestive heart failure, ischemic heart disease, and myocardial infarction. Early detection of diagnostic features underlying electrocardiography signals is crucial for the identification and treatment of CAD. In the present work, we proposed novel entropy called Renyi Distribution Entropy (RdisEn) for the analysis of short-term heart rate variability (HRV) signals and the detection of CAD. Our simulation experiment with synthetic, physiological, and pathological signals demonstrated that RdisEn could distinguish effectively among different subject groups. Compared to the values of sample entropy or approximation entropy, the RdisEn value was less affected by the parameter choice, and it remained stable even in short-term HRV. We have developed a combined CAD detection scheme with RdisEn and wavelet packet decomposition (WPD): (1) Normal and CAD HRV beats obtained were divided into two equal parts. (2) Feature acquisition: RdisEn and WPD-based statistical features were calculated from one part of HRV beats, and student’s t-test was performed to select clinically significant features. (3) Classification: selected features were computed from the remaining part of HRV beats and fed into K-nearest neighbor and support vector machine, to separate CAD from normal subjects. The proposed scheme automatically detected CAD with 97.5% accuracy, 100% sensitivity and 95% specificity and performed better than most of the existing schemes.
Keywords: coronary artery disease, heart rate variability, renyi distribution entropy, wavelet packet decomposition, classifier
Introduction
Plaque accumulation (fatty and cholesterol substances) in the inner wall of the coronary arteries causes a blockage in the coronary circulation and the reduction of blood supply to the heart muscles, leading to coronary artery diseases (CAD) (Steinberg and Gotto, 1999). Unless treated early, CAD can result in congestive heart failure, ischemic heart disease, myocardial infarction, ischemia, arrhythmias, angina and sudden death (Grech, 2011). In 2012, 7.4 million CAD-related deaths were reported, which accounted for 10% of total fatalities among female population and 16% among male population that year, respectively (World Health Organization, 2015). By 2030, an estimated 37% increase in CAD-related death is expected in emerging nations (Acharya et al., 2017c). Early CAD detection is therefore the key to prevent further heart function damage and save lives.
The exercise stress test (EST), which monitors various heart status features, is often used for CAD diagnosis. However, not all CAD subjects can achieve the expected heart rate, and many patients may suffer cardiac arrest during EST (Román et al., 1998). Alternatively, measurement of resting ECG signals can be applied as a non-invasive and preferred method for CAD diagnosis. Since no obvious change in the resting ECG signals is detected among ∼70% of CAD subjects, the manual CAD diagnosis is time-consuming and ineffective (Antanavicius et al., 2008). In recent years, computer-aided diagnostic technologies (CADT) for CAD detection have garnered increasing attentions for their ease of operation without the excessive reliance on the personal experience of a doctor, as well as their cost-effectiveness.
Heart rate variability (HRV) extracted from the ECG depicts the variation in time interval between adjacent heartbeats and is vital for autonomic modulation of the heart. CADT-based HRV analyses have been proposed in recent years for CAD diagnosis. Reduced values in the frequency-domain feature of HRV signals is closely related to the severity of CAD (Hayano et al., 1990). For instance, compared to normal subjects, CAD patients exhibit lower circadian rhythms (Huikuri et al., 1994). Power spectral analysis also reveals that the low/high frequency ratio of HRV signals is significantly lower in CAD-affected subjects with panic disorder than in normal subjects (Lavoie et al., 2004). Moreover, CAD patients exhibit lower values in the time domain features of HRV signals, such as NN50 (number of adjacent NNs, which are greater than 50 ms) and pNN50 (NN50 divided by total number of NNs, which is expressed as a percentage), than normal subjects (Acharya et al., 2014). Due to its non-linear and non-stationary nature, the non-linear methods perform better at decoding the invisible complexities and extracting valuable information from HRV signals, compared to the frequency- and time-domain analyses of HRV signals. Applying non-linear methods can also minimize variation and background noise problems that are often associated with the frequency- and time- domain analyses. Many non-linear parameters, including the fractal dimension (Rajendra et al., 2005), the Lyapunov exponents (Acharya et al., 2004), the detrended fluctuation analysis (Peng et al., 1995), and the recurrence quantification analysis (RQA) (Acharya et al., 2014), are calculated from HRV signals in order to separate CAD from normal subjects.
Entropy, the main method of non-linear analysis that measures randomness and complexity of signals, is widely used for HRV signal analyses to detect cardiac abnormalities (Acharya et al., 2014, 2015b; Elias et al., 2014; Rajendra Acharya et al., 2015). Acharya et al. (2014) showed that Approximate Entropy (ApEn) and Sample Entropy (SamEn) are higher in normal subjects than in CAD subjects. Entropy evaluations are highly reliant upon the selection of parameters, including N (data length), r (distance tolerance), and m (embedding dimension) (Pincus, 1991; Mayer et al., 2014). Among these parameters, r has the largest impact on results, as even a small change in its value significantly alters the complexity measurement of a given data set, potentially causing mis-diagnosis (Castiglioni and Rienzo, 2008; Lu et al., 2008; Liu et al., 2011). Li et al. (2015) proposed a new entropy named the Distribution Entropy (DisEn) to measure the distribution property existing in data sets by computing Shannon entropy of the empirical probability density of inter-vector distances. Compared to the effect of r on ApEn and SamEn computations, the parameters M (the number of bins) and m (embedding dimension) have less impact on the stability and consistency of DisEn’s performance (Udhayakumar et al., 2016). DisEn excels in analyzing HRV signals with a shorter length (Karmakar et al., 2017). In contrast to the computation of ApEn and SamEn, which requires reconstruction of two adjacent dimension vector spaces, the computation of DisEn only requires reconstruction of the m-dimension vector space. As a result, the amount of DisEn computation is only half that of ApEn or SamEn. Renyi entropy (RenEn) is a generalization and reduction of Shannon entropy as the order parameter q closes to 1. RenEn, highlighting characteristics of multifractality or long-range interactions occurring in biomedical systems, is more sensitive to frequent occurrences when q increases (Liang et al., 2015). RenEn calculated from HRV signals is often used as an important clinical indicator of early cardiac autonomic neuropathy (Cornforth et al., 2013, 2014). Recently, RenEn has also been combined with non-linear decompositions, such as discrete wavelet transform (DWT) (Acharya et al., 2016), wavelet packet decomposition (WPD) (Li and Zhou, 2016), empirical mode decomposition (EMD) (Acharya et al., 2017b; Sridhar et al., 2017) for automated diagnosis of CAD, myocardial infarction, and congestive heart failure.
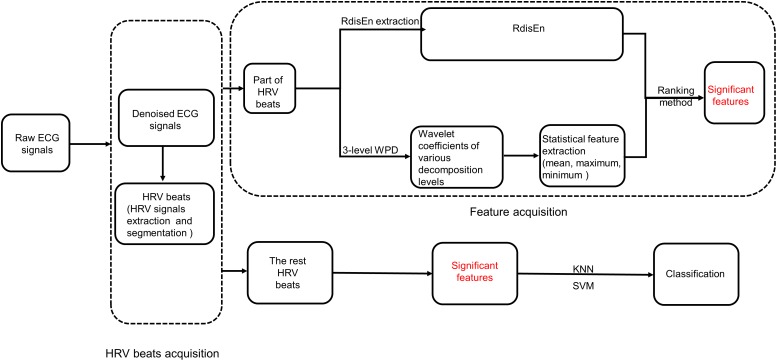
In our current studies, we propose a new entropy named Renyi Distribution Entropy (RdisEn), which integrates Renyi entropy and distribution entropy. In addition, we have developed an automatic CAD detection scheme (Figure 1): CAD and normal HRV beats are each divided into two parts. One part of HRV beats is used to extract features with important clinical information, while the other is used to evaluate classification performance of the CAD detection scheme. The feature extraction consists three steps: (1) CAD and normal HRV beats are subjected to three levels of WPD (2) Statistical features (mean, maximum, and minimum values) are computed from the obtained coefficients of the third decomposition levels, and RdisEn is computed from the HRV beats (3) The resulting WPD-based statistical features and RdisEn are then ranked to extract features with significant information for distinguishing those subjects with CAD from those without. Finally, the extracted features computed from the remaining part of HRV beats are fed into K-nearest neighbor (KNN) and support vector machine (SVM) for automatic CAD detection.
FIGURE 1.
Block diagram of the scheme for CAD detection.
Materials and Methods
Data Acquisition
In this study, normal and CAD ECG recordings were downloaded from Fantasia open-access database1 and St. Petersburg Institute of Cardiological Technics 12-lead Arrhythmia Database2, respectively. Only the lead-II ECG recordings were used for this study. We employed a total of 57 ECG recordings, among which 40 were from normal subjects (20 old: 68 to 85 years, 20 young: 21 to 34 years) and 17 were from 7 CAD patients.
Renyi Distribution Entropy
For a discrete time series {x(i), i = 1, 2,…, N}, B and m denote bin number and embedding dimension, the RdisEn is computed as follows:
(1) Reconstruction of state space: (N−m)vectors U (i) byU (i) = {x (i), x(i+1),…, x(i+m−1)}, 1 ≤ i ≤ N-m.
(2) Construction of the distance matrix: M = {di,j} between vectors U (i) and U (j) for 1 ≤ i, j ≤ N-m, where
(3) Estimation of probability density: the distances in the matrix M are divided into B bins with equal space, and thus the probability of each bin (t) of the histogram is calculated as
(4) Calculation: the normalized RdisEn of x (i) is defined as
From the algorithm of RdisEn, it is not difficult to conclude that RdisEn will degenerate to DisEn when q → 1 (Cornforth et al., 2014).
Proposed CAD Detection Scheme
In our present study, we developed a combination scheme to separate CAD patients and normal subjects. It consisted of three steps: (1) HRV beats acquisition, (2) RdisEn and WPD-based feature acquisition (3) classification through K-NN and SVM.
HRV Beats Acquisition
The downloaded ECG signals were sampled at 250 HZ for normal group and 257 HZ for CAD group. The normal ECG signals were up-sampled to 257 HZ to maintain uniformity between the two groups. Daubechies wavelet 6 (db6) was used to eliminate unwanted noise (Martis et al., 2013). The ECG signals were subjected to Pan-Tompkin to detect R-peaks (Pan and Tompkins, 2007), and then HRV signals were obtained by calculating the time duration of two consecutive R-peaks (Constant et al., 1999). Finally, each CAD HRV signal was divided into beats (each beat is a segment containing 500 samples), and as a result, 80 HRV beats were acquired from 17 normal ECG signals. In order to keep the dataset balance between the two groups, two normal HRV beats were extracted from each normal HRV signals, and consequently a total of 80 beats were acquired from 40 normal ECG signals.
Feature Acquisition
One hunderd and sixty HRV beats obtained from normal and CAD HRV signals were randomly divided into two parts before feature acquisition, with each part consisting of equal number of beats from the two classes. One part of beats (40 beats for each type of signals) was used for feature acquisition, while the other was utilized to evaluate classification performance.
Feature extraction
As shown in Figure 1, RdisEn and WPD-based statistical features were extracted from the HRV beats of the two classes. RdisEn was computed based on the distribution characteristics of inter-vector distances, and parameters on RdisEn evaluation were fixed at B = 512, m = 2, q = 0.4 for CAD detection in our proposed scheme (the rationale for the chosen combined parameter is detailed in section “Performance on CAD Detection”). RdisEn was used to extract significant features from each HRV beat to distinguish CAD patients from normal subjects, and WPD-based statistical features were also computed. Briefly, a 3-level WPD was performed on every segmented HRV beat with 500 samples to divide it into a set of sub-bands. WPD, a popular methodology of multiresolution analysis for non-stationary and non-linear signals (Acharya et al., 2015a), can exploit properties of the studied signals in frequency and time domains simultaneously. WPD provides better frequency resolution for the sub-bands than DWT, and it possesses more wavelet sub-bands on the 3rd level WPD of each HRV beat than DWT (8 for WPD and 4 for DWT). Since the obtained wavelet coefficients in each sub-band are related to the wavelet basis selected (Zhang et al., 2018), Daubechies (orders 1–5), Harr, Coiflets (orders 1–3) wavelet function with 3-level decomposition were considered to capture significantly discriminable features for the best classification accuracy for CAD detection. Subsequently, three statistical features, namely mean [M(k)], minimum [Mi(k)], and maximum [Ma(k)] (k = 1, 2…8,) were evaluated from the wavelet coefficients of the 3rd level wavelet sub-bands.
Feature selection
Not all of the features obtained from the HRV beats exhibited great separation between the two groups, redundant and insignificant features would raise computation cost and impede classification performance. To maximize classification accuracy, feature selection was applied to the original features from extraction, with the least number of features. Student’s t-test was used as a method of feature selection in our current study (Box, 1987), and features with a p-value less than 0.05 were deemed to have significant differences. RdisEn and the top four ranked statistical features were selected.
Classification
Top four ranked statistical features were computed from the remaining part of HRV beats using RdisEN, and fed into classifiers one by one to obtain the highest accuracy with minimum number of features. The two classifiers used in our work are described below.
K-nearest neighbor (KNN)
K-nearest neighbor is a supervised machine learning method widely used in classification, and the class of a testing data is determined by the majority of votes for k training samples with the closest Euclidean distance (González et al., 2016). In this work, k = 10 was used.
Support vector machine (SVM)
The SVM classifier divides the training set into two parts by constructing a hyper-plane in the feature space. Features in non-linear separation may be change into linear separation, using kernel functions to map the original data to a feature space with higher dimension (Duda et al., 2012). In this work, an order 1 function kernel was used.
Three evaluation indicators, Accuracy (Acc), Sensitivity (Sen), and Specificity (Spe) were calculated to evaluate the classifiers performance. To ensure unbiasedness and credibility of the classification results, 10 × 10-fold cross validation methodology was implemented, and overall evaluation indicators were calculated.
Feature Assessment
Three statistics methods were used to test the CAD detection performance of these features. The open source R package was used for all the analysis and calculation. First, univariate binary logistic regression method was used to access the statistically significant correlations between CAD and each feature (p-value < 0.05). Second, the correlation between the extracted features was evaluated by using Pearson test (p-value < 0.05, correlation coefficient >0.5). Finally, multivariate binary logistic regression model without redundant features was established to determine statistically significant feature associated with CAD detection (p-value < 0.05).
Results
Performance of RdisEn on Various Signals
To test the consistency and stability of the RdisEn measurement, we studied the impact of the changing parameter combinations on the RdisEn measurement, using synthetic, physiologic and pathological signals. DisEn was originally introduced to eliminate ApEn and SamEn’s excessive dependence on tolerance r. RdisEn proposed in this work was based on DisEn. We therefore compared the performance of RdisEn to that of ApEn, SamEn and DisEn.
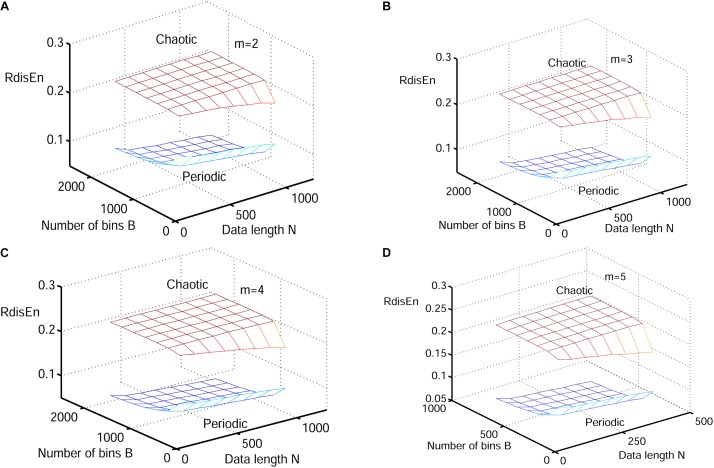
Performance of RdisEn on Synthetic Signals by Varying Parameters
The synthetic signals were generated by the Logistic attractor xn+1 = wxn (1−xn). The constant w was set at 3.5 and 3.8 to obtain periodic and chaotic signals (Pincus, 1991) respectively, which has been widely applied to describe variations of entropy level (Xie et al., 2008; Chen et al., 2009; Karmakar et al., 2017). Twenty realizations were generated from 1000 samples of both signal types, and initial values of the realizations were selected randomly between 0.1 and 0.2 to eliminate the random factors. The mean values of RdisEn with the changing parameter combinations of N (N = 50, 200, 350, 500, 650, 800, 1000), B (B = 100,250,350,500,650,1000,1300,2000) and m (m = 2,3,4,5) for chaotic and periodic signals, as well as the fixed parameter q (q = 0.5), are shown in Figure 2. A significant separation between the two signal types was observed, while the traits of the RdisEn values were similar for m = 2, 3, 4, 5 (Figure 2).
FIGURE 2.
Variation of mean RdisEn values chaotic and periodic signals of with varying parameter combinations N and B for (A) m = 2, (B) m = 3, (C) m = 4, and (D) m = 5.
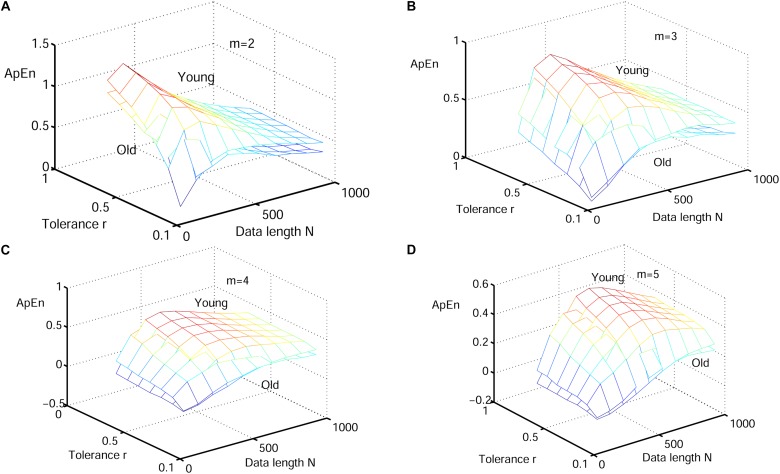
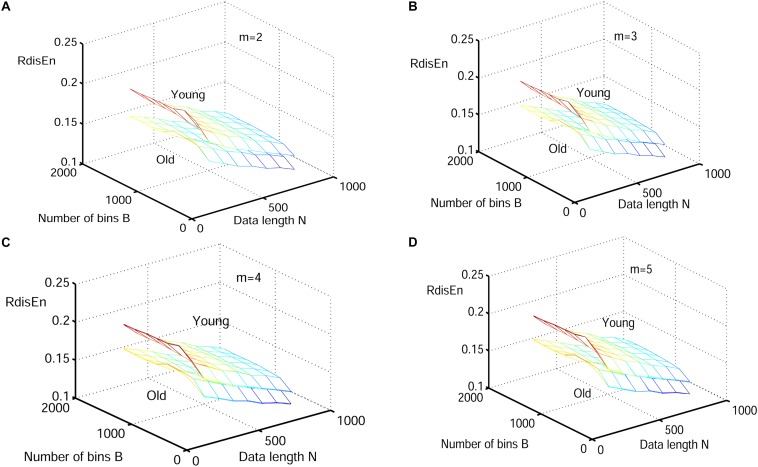
Performance of RdisEn on Physiologic Signals by Varying Parameters
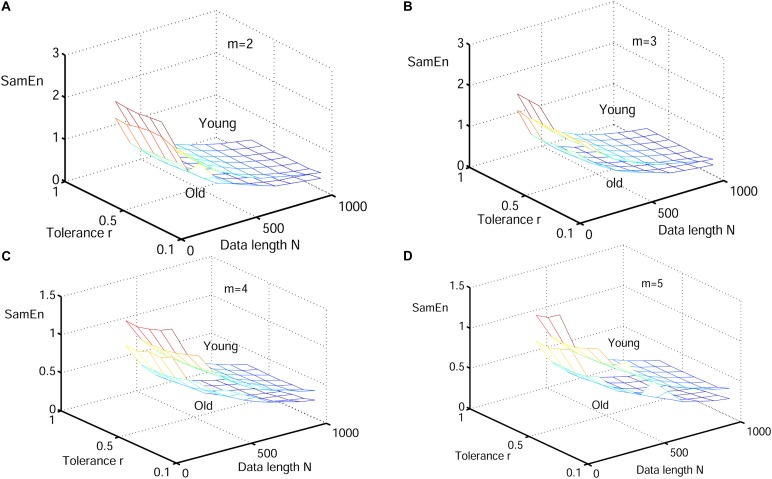
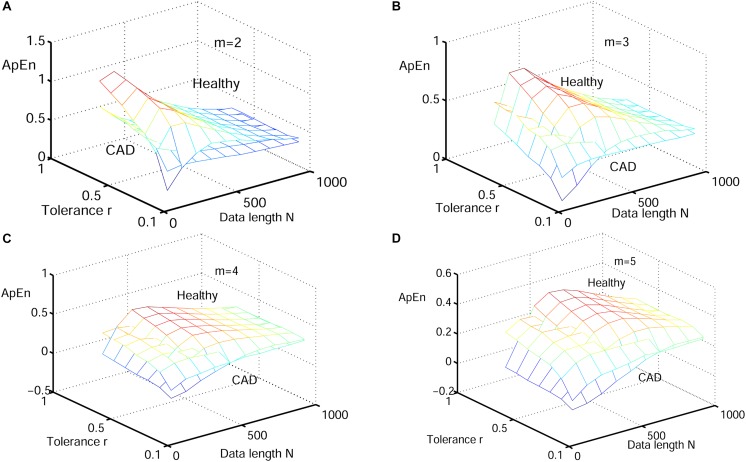
Next, physiological features were extrapolated from the HRV signals of 20 elderly and 20 young healthy subjects as described in section “HRV Beats Acquisition.” For each subject, a HRV signal was selected with varying length (50, 200, 350, 500, 650, 800, and 1000) for RdisEn calculation using the following parameters: N = 50, 200, 350, 500, 650, 800, and 1,000; B = 100, 250, 350, 500, 650, 1,000, 1,300, and 2,000; m = 2, 3, 4, and 5; q = 0.5. As comparison, ApEn and SamEn were also calculated with the following parameters: N = 50, 200, 350, 500, 650, 800, and 1,000; r = 0.1∗SD, 0.2∗SD,…,1∗SD; m = 2, 3, 4, and 5. The results are shown in Figure 3–5. The values of ApEn fluctuated widely with different combinations of N, r, and m, especially for a small data length (Figure 3). There was a crossover in ApEn meshes between the HRV signals from the elderly and young subjects, suggesting that ApEn failed to effectively separate the two age groups. The SamEn mesh was sparse in comparison with the ApEn and RdisEn mesh (Figure 4), most likely due to the fact that SamEn was not defined for smaller data length, resulting in invalid values. As shown in Figure 5, RdisEn could effectively differentiate HRV signals between the two age groups, even for smaller data lengths. In addition, the variation of RdisEn values was small with diverse parameter m. The effects of different parameters N and B or r on entropy measurements (ApEn and RdisEn) for embedding dimension m ∈ [2, 5] were quantified by the means of the standard deviation across N and B or r (Table 1). It was not difficult to find that the change of ApEn measurement with a variation of N was less than that with the change of r. The variation of RdiEn measurement with varying B was higher than that with varying of N for old vs. young subjects. More importantly, compared to ApEn, the variations of RdisEn values with changing parameters B and M were relatively small (Table 1).
FIGURE 3.
Variation of the mean ApEn value for HRV signals of old and young subjects with varying parameter combinations N and r for (A) m = 2, (B) m = 3, (C) m = 4, and (D) m = 5.
FIGURE 5.
Variation of the mean RdisEn value for HRV signals of old and young subjects with varying parameter combinations N and B for (A) m = 2, (B) m = 3, (C) m = 4, and (D) m = 5.
FIGURE 4.
Variation of the mean value for HRV signals of old and young subjects with varying parameter combinations N and r for (A) m = 2, (B) m = 3, (C) m = 4, and (D) m = 5.
Table 1.
Mean of the standard deviation across data length N and bin number B for RdisEn or tolerance r for ApEn.
| Entropy | Embedding dimension m | Young | Old | Healthy | CAD | Healthy | Arrhythmia | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RdisEn | 2 | 0.0043 | 0.0242 | 0.0043 | 0.0217 | 0.0043 | 0.0217 | 0.0067 | 0.0226 | 0.004 | 0.0192 | 0.0074 | 0.0196 |
| 3 | 0.0048 | 0.0244 | 0.0049 | 0.0219 | 0.0049 | 0.0219 | 0.0079 | 0.0229 | 0.0051 | 0.0195 | 0.0084 | 0.0199 | |
| 4 | 0.0054 | 0.0245 | 0.0054 | 0.0220 | 0.0054 | 0.0220 | 0.0087 | 0.0231 | 0.0057 | 0.0196 | 0.0093 | 0.0200 | |
| 5 | 0.0060 | 0.0245 | 0.0060 | 0.0221 | 0.0060 | 0.0221 | 0.0096 | 0.0221 | 0.0062 | 0.0197 | 0.0101 | 0.0201 | |
| ApEn | 2 | 0.1302 | 0.2641 | 0.0982 | 0.2527 | 0.0982 | 0.2527 | 0.0404 | 0.1225 | 0.0829 | 0.2481 | 0.1063 | 0.2322 |
| 3 | 0.1114 | 0.1893 | 0.0859 | 0.1599 | 0.0859 | 0.1599 | 0.0401 | 0.0698 | 0.0741 | 0.1487 | 0.0995 | 0.1357 | |
| 4 | 0.0983 | 0.1687 | 0.0770 | 0.1314 | 0.0770 | 0.1314 | 0.0447 | 0.0419 | 0.0657 | 0.1122 | 0.0867 | 0.11104 | |
| 5 | 0.0875 | 0.1545 | 0.0707 | 0.1172 | 0.0707 | 0.1172 | 0.0447 | 0.0316 | 0.0578 | 0.0941 | 0.0748 | 0.0995 | |
Performance of RdisEn on Pathological Signals by Varying Parameters
In this work, CAD signals and arrhythmia short-term HRV signals were compared to healthy signals. 40 healthy and 17 CAD short-term HRV signals were acquired from 40 normal and 7 CAD subjects, as described in section “HRV Beats Acquisition.” Using the Pan-Tompkin algorithm, 48 arrhythmia short-term HRV signals were obtained from MIT-BIH Arrhythmia Database3, which contains 48 ECG signals from 47 subjects (25 men: 32 to 89 years, 22 women: 23 to 89 years) (Pan and Tompkins, 2007).
The HRV signals of varying lengths (50, 200, 350, 500, 650, 800, and 1,000) were selected to test ability of RdisEn to separate the two types of pathological signals with changing parameters. ApEn and SampEn were also calculated as references, and the parameters corresponding to the three entropies (RdisEn, ApEn, and SamEn) were set as described in section “Performance of RdisEn on Physiologic Signals by Varying Parameters.”
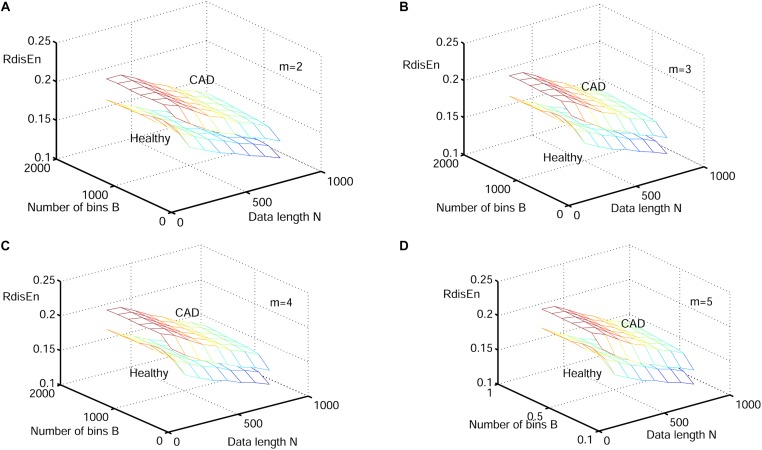
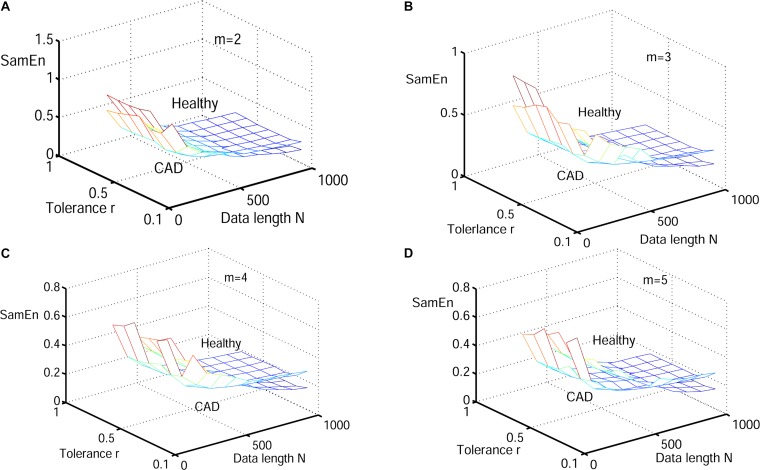
Figure 6–8 show the change of mean ApEn, SamEn and RdisEn values with varying parameter combinations for normal and CAD HRV signals. In contrast to ApEn and SamEn, the mean value of RdisEn for CAD HRV signals was higher than that for normal HRV signals, demonstrating the superiority of RdisEn in differentiating CAD and normal subjects. Quantification results on the effect of parameter selections for entropy values (ApEn and RdisEn) for embedding dimension m ∈ [2, 5], in terms of the means of standard deviation across N and B or r, are shown in Table 1. Our results demonstrated that RdisEn measurement remained relatively stable to parameter selection for very short lengths of HRV signals (Figure 3–8 and Table 1), most likely due to its inherited merits from DisEn (Karmakar et al., 2017). In contrast, a large amount of invalid values was generated in ApEn and SamEn calculation (Figure 6, 7). Moreover, remarkable separation between normal and CAD RdisEn meshes was observed (Figure 8). Taken together, these results demonstrated that the RdisEn analysis is the best method to generate stable values with clear separation between normal and CAD groups.
FIGURE 6.
Variation of the mean ApEn value for HRV signals of normal and CAD subjects with varying parameter combinations N and r for (A) m = 2, (B) m = 3, (C) m = 4, and (D) m = 5.
FIGURE 8.
Variation of the mean RdisEn value for HRV signals of normal and CAD subjects with varying parameter combinations N and B for (A) m = 2, (B) m = 3, (C) m = 4, and (D) m = 5.
FIGURE 7.
Variation of the mean SamEn value for HRV signals of normal and CAD subjects with varying parameter combinations N and r for (A) m = 2, (B) m = 3, (C) m = 4, and (D) m = 5.
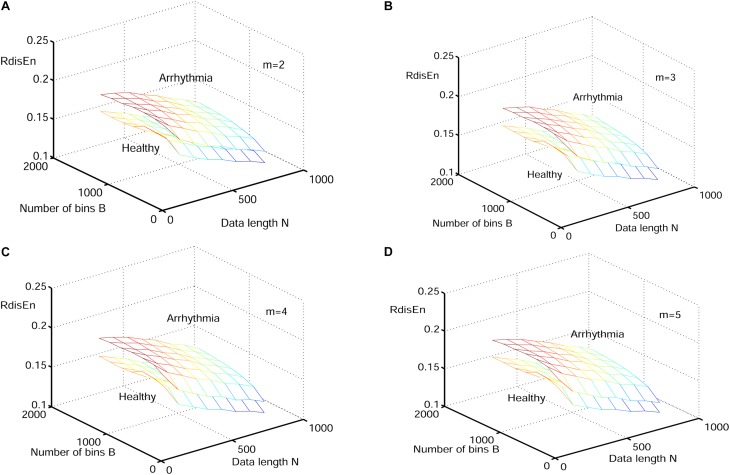
The change of mean RdisEn values with varying parameter combinations for normal and arrhythmia HRV signals was shown in Figure 9. The parameter combinations of RdisEn were the same as that described in section “Performance of RdisEn on Physiologic Signals by Varying Parameters.” Significant separation between normal and arrhythmia RdisEn meshes can be observed (Figure 9). In addition, area under the ROC curve (AUC) was used to examine the performance of RdisEn (B = 512, m = 2, q = 0.9) with varying length (500, 800, and 1000) to separate healthy from arrhythmia short-term HRV signals. ApEn (r = 0.2 × SD, m = 2), SamEn (r = 0.2 × SD, m = 2), DisEn (B = 512, m = 2), and RenEn (q = 0.9) were used as references. When AUC equals to 1, the feature distributions belonging to the two classes are completely separated; when AUC equals to 0.5, the feature distributions are similar, suggesting that the closer to 1 the AUC value, the better the discriminatory power of RdisEn (Hanley and McNeil, 1982). RisEn out-performed ApEn, SamEn, DisEn, and RenEn in distinguishing healthy from arrhythmia short-term HRV signals (Table 2 and Figure 9). RdiEn also exhibited good computing stability with varying length, as shown by the SD values (Table 2).
FIGURE 9.
Variation of the mean RdisEn value for HRV signals of normal and arrhythmia subjects with varying parameter combinations N and B for (A) m = 2, (B) m = 3, (C) m = 4, and (D) m = 5.
Table 2.
AUC values of the five entropy measurements with varying lengths for separating healthy from arrhythmia HRV signals.
| Entropy | 500 | 800 | 1000 | Mean | SD |
|---|---|---|---|---|---|
| ApEn | 0.4427 | 0.4552 | 0.4583 | 0.4521 | 0.0083 |
| SampEn | 0.5833 | 0.5729 | 0.551 | 0.5691 | 0.0165 |
| DisEn | 0.7719 | 0.7677 | 0.7604 | 0.7667 | 0.0058 |
| RenEn | 0.5208 | 0.5104 | 0.45 | 0.4937 | 0.0382 |
| RdisEn | 0.7698 | 0.7698 | 0.7656 | 0.7684 | 0.0024 |
Performance on CAD Detection
We repeated the RdisEn analyses using HRV beats obtained via the automated CAD detection scheme from normal and CAD subjects. B = 512 was frequently employed in the analysis of HRV signals with respect to DisEn (Li et al., 2015; Yang et al., 2015), and the selection of m had little effect upon the RdisEn evaluation on the basis of the aforementioned study. Consequently, the related parameters on the RdisEn evaluation were fixed to B = 512 and m = 2 for CAD detection. In addition to the parameter B and m on the DisEn evaluation, another parameter q, which enhances differentiation between normal and CAD HRV beats, requires to be fixed for the RdisEn measurement. To optimize q, we adopted the Student’s t-test to assess the performance of RdisEn calculated from one part of normal and CAD HRV beats with varying parameter q (q ∈ [0.1, 2]). As shown in Table 3, the two groups exhibited significantly different RdisEn values, regardless of the q parameter variations. The p-value was lowest when q = 0.4, indicative of the optimal condition to differentiate the two groups (RdisEn degenerated into DisEn, as mentioned in section “Renyi Distribution Entropy”). As a result, we computed RdisEn with parameters N = 500, B = 512, m = 2, and q = 0.4. Table 4 shows the means and SD of RdisEn, as well as the top four statistical features based on WPD with the db1, computed from one part of normal and CAD HRV beats, and their p-values generated by Student’s t-test, significant differences were observed between the two groups (Table 4).
Table 3.
p-Values of RdisEn computed from normal and CAD HRV beats with varying parameter q.
| q | 0.1 | 0.2 | 0.3 | 0.4 | 0.5 | 0.6 | 0.7 | 0.8 | 0.9 | 1 |
| p-Value | 9.68E-5 | 5.08E-5 | 3.55E-5 | 3.15E-5 | 3.32E-5 | 3.85E-5 | 4.68E-5 | 5.60E-5 | 7.1E-5 | 8.86E-5 |
| q | 1.1 | 1.2 | 1.3 | 1.4 | 1.5 | 1.6 | 1.7 | 1.8 | 1.9 | 2 |
| p-Value | 1.08E-4 | 1.30E-4 | 1.54E-4 | 1.81E-4 | 2.09E-4 | 2.39E-4 | 2.71E-4 | 3.05E-4 | 3.39E-4 | 3.74E-4 |
Table 4.
Mean and SD values of RdisEn and the top five WPD (db1 basis) based statistical features for normal and CAD HRV beats.
| Feature | CAD | Normal | p-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| RdisEn | 0.2690 | 0.0363 | 0.2345 | 0.0316 | 3.15E-5 |
| Mi(1) | 1.6203 | 0.3024 | 2.4613 | 0.4826 | 2.37E-14 |
| M(1) | 1.9249 | 0.3958 | 2.8147 | 0.5110 | 3.55E-13 |
| Mi(5) | 2.2415 | 0.4469 | 3.0369 | 0.5778 | 1.29E-9 |
| Ma(6) | 0.3315 | 0.2148 | 0.0992 | 0.0995 | 2.45E-8 |
Five selected features were calculated from the remaining part of normal and CAD HRV beats and then fed into classifiers KNN or SVM one by one to maximize the accuracy with minimal features. As shown in Table 5, the proposed scheme for CAD detection achieved the highest mean accuracy of 96.34% with five features (RdisEn and four WPD with db1 d statistical features) in 10 × 10-fold cross validation using KNN. We repeated the CAD detection scheme (Figure 1) using RdisEn and WPD with other wavelet-based statistical features, and the results were shown in Table 5. We computed the p-values for the correlations between CAD detection with five features, i.e., RdisEn and the top ranked four WPD with coif2 based statistical features [Mi(1), M(1), Ma(1), and Mi(6)] by univariate binary logistic regression method, the corresponding p-values for the five features are 2.5e-6, 0.01, 3.3e-6, 4.6e-6, and 0.02, respectively, which demonstrated that these features statistically significant correlated with CAD detection. As presented in Table 5, when the fifth feature was added into the KNN classifier, the CAD detection performed with 97.5% accuracy, 100% sensitivity, 95% specificity, respectively, with no significant improvement compared with the performance of the 4-feature based model (97.37 ± 0.41% accuracy, 99.75 ± 0.79% sensitivity, 95% specificity). This indicated that the fifth feature [Mi(6)] is correlated with the other four features [RdisEn, Mi(1), M(1), and Ma(1)] and therefore includes redundant information. A Pearson test was performed to calculate the correlations between the fifth feature and other four, the correlation coefficient for Mi(6) and RdisEn, fMi(1), M(1), and Ma(1) are -0.26 (p-value = 0.020), -0.073 (p-value = 0.518), 0.218 (p-value = 0.052), and 0.953 (p-value = 4.3e-42), respectively, indicating a significant correlation between the fifth feature [Mi(6)] and Ma(1). At last, the multivariate binary logistic regression model was used to test the relationship between the features and the CAD detection, in which RdisEn and the other three features were entered and their p-values are 0.033, 0.563, 0.089, and 0.501, respectively; it is obvious that RdisEn improved the CAD detection statistically significant.
Table 5.
Classification performance of RdisEn and WPD (various basis) based statistical features by using KNN and SVM classifiers.
| Wavelet basis | NoF | KNN | SVM | ||||
|---|---|---|---|---|---|---|---|
| Acc(%) | Sen(%) | Spe(%) | Acc(%) | Sen(%) | Spec(%) | ||
| db1 | 3 | 96.08 ± 0.38 | 97.5 | 94.75 ± 0.79 | 96.08 ± 0.38 | 97.25 ± 0.79 | 95 |
| 4 | 96.08 ± 0.38 | 97.5 | 94.75 ± 0.79 | 96.06 ± 0.59 | 97.5 ± 1.79 | 95.24 ± 0.77 | |
| 5 | 96.34 ± 0.72 | 97.5 | 95.25 ± 1.42 | 95.6 ± 0.85 | 97.25 ± 0.79 | 94 ± 1.29 | |
| db2 | 3 | 96.08 ± 0.38 | 97.5 | 94.75 ± 0.79 | 97.12 ± 0.84 | 99.25 ± 1.69 | 95 |
| 4 | 97.25 ± 0.79 | 100 | 94.5 ± 1.58 | 97.37 ± 0.41 | 99.75 ± 0.79 | 95 | |
| 5 | 96.48 ± 0.99 | 98 ± 1.97 | 95 | 96.6 ± 0.86 | 98.25 ± 1.69 | 95 | |
| db3 | 3 | 96.33 ± 0.41 | 97.75 ± 0.79 | 95 | 95.6 ± 0.85 | 96.5 ± 1.75 | 94.75 ± 0.79 |
| 4 | 97.37 ± 0.41 | 99.75 ± 0.79 | 95 | 96.6 ± 0.86 | 98.5 ± 1.75 | 94.75 ± 0.79 | |
| 5 | 95.72 ± 0.62 | 96.5 ± 1.29 | 95 | 96.46 ± 0.54 | 98 ± 1.05 | 95 | |
| db4 | 3 | 95.96 ± 0.51 | 97 ± 1.05 | 95 | 95.38 ± 1.31 | 95.75 ± 2.65 | 95 |
| 4 | 97.37 ± 0.41 | 99.75 ± 0.79 | 95 | 96.23 ± 1.17 | 97.5 ± 2.36 | 95 | |
| 5 | 97.37 ± 0.41 | 99.75 ± 0.79 | 95 | 95.24 ± 0.95 | 95.5 ± 1.97 | 95 | |
| db5 | 3 | 95.84 ± 0.58 | 97 ± 1.05 | 94.75 ± 0.79 | 95 ± 1.26 | 95 ± 2.63 | 95 |
| 4 | 96.23 ± 1.02 | 97.75 ± 0.79 | 94.75 ± 1.84 | 95.85 ± 0.83 | 97 ± 1.05 | 94.75 ± 1.42 | |
| 5 | 96.74 ± 1.22 | 98.75 ± 1.32 | 94.75 ± 1.84 | 95.60 ± 1.34 | 96.75 ± 1.69 | 94.50 ± 1.58 | |
| db6 | 3 | 95.96 ± 0.51 | 97.50 | 94.50 ± 1.05 | 95.97 ± 0.78 | 97 ± 1.58 | 95 |
| 4 | 97.24 ± 0.55 | 100 | 94.5 ± 1.05 | 96.73 ± 0.89 | 98.50 ± 1.75 | 95 | |
| 5 | 95.85 ± 0.83 | 97.50 ± 1.18 | 94.25 ± 1.21 | 95.48 ± 0.84 | 96.50 ± 1.75 | 94.50 ± 1.05 | |
| harr | 3 | 96.08 ± 0.38 | 97.50 | 94.75 ± 0.79 | 96.08 ± 0.38 | 97.25 ± 0.79 | 95 |
| 4 | 96.08 ± 0.38 | 97.50 | 94.75 ± 0.79 | 96.21 ± 0.59 | 97.50 ± 1.18 | 95.24 ± 0.77 | |
| 5 | 96.34 ± 0.71 | 97.50 | 95.25 ± 1.42 | 95.60 ± 0.85 | 97.25 ± 0.79 | 94 ± 1.23 | |
| coif1 | 3 | 96.08 ± 0.38 | 97.50 | 94.75 ± 0.79 | 95.84 ± 0.81 | 97 ± 1.05 | 94.75 ± 0.79 |
| 4 | 95.96 ± 0.51 | 97.50 | 94.50 ± 1.05 | 95.85 ± 1.01 | 97.25 ± 1.42 | 94.50 ± 1.05 | |
| 5 | 97.24 ± 0.55 | 99.75 ± 0.79 | 94.75 ± 0.79 | 96.24 ± 1.31 | 98 ± 1.97 | 94.50 ± 1.05 | |
| coif2 | 3 | 96.33 ± 0.41 | 97.75 ± 0.79 | 95 | 97.11 ± 0.63 | 99.25 ± 1.21 | 95 |
| 4 | 97.37 ± 0.41 | 99.75 ± 0.79 | 95 | 97.24 ± 0.55 | 99.5 ± 1.05 | 95 | |
| 5 | 97.50 | 100 | 95 | 97.24 ± 0.55 | 100 | 94.50 ± 1.05 | |
| coif3 | 3 | 95.96 ± 0.51 | 97.25 ± 0.79 | 94.75 ± 0.79 | 96.98 ± 0.98 | 97 ± 1.97 | 95 |
| 4 | 96.98 ± 0.67 | 99.25 ± 1.21 | 94.75 ± 0.79 | 96.99 ± 0.88 | 99 ± 1.75 | 95 | |
| 5 | 95.84 ± 0.58 | 96.75 ± 1.21 | 95 | 95.36 ± 0.58 | 95.75 ± 1.21 | 95 | |
NoF, number of features.
Discussion
The CAD diagnostic signals can be divided into three major categories: heart sound signals (HSS), ECG signals, and HRV signals. The detailed methods of CAD detection are described in Table 6. HRV signals are essential tools widely used for cardiac abnormality detection and CAD diagnosis (Lee et al., 2007, 2008; Dua et al., 2012; Giri et al., 2013; Patidar et al., 2015; Kumar et al., 2016). Lee et al. (2007, 2008) employed linear and non-linear features extracted from HRV signals as indices to distinguish normal subjects from CAD patients, and they achieved a ∼90% accuracy using the SVM classifier. The automatic CAD detection algorithm was proposed by Dua et al. (2012), based on non-linear features (recurrence plots, detrended fluctuation, and three types of entropy) and a principal component analysis method, and achieved an accuracy of 89.5% using multilayer perceptron (MLP) methodology. Giri et al. (2013) used DWT to divide HRV signals into frequency sub-bands. They also applied dimensionality reduction methods such as PCA, independent component analysis (ICA), and linear discriminant analysis (LDA) to the coefficients from the obtained sub-bands to lower the data dimension. With the additional combined method of ICA and Gaussian mixture model (GMM), Giri et al. (2013) reported the highest accuracy for automatically identifying CAD of 96.8%. Patidar et al. (2015) applied a combination of tunable-Q wavelet transform (TQWT), centered correntropy, and the PCA method to achieved an accuracy of 99.72% with HRV signals from the automated diagnosis of CAD. Kumar et al. (2016) developed a CAD detection technique, which consists of the flexible analytic wavelet transform (FAWT) and ranking methods, including receiver operating characteristics (ROC), entropy and Bhattacharya space algorithm, with a classification accuracy of 100%.
Table 6.
Studies conducted to distinguish normal from CAD subjects using various signals.
| Author | Data used | Method/features | Classifiers | Cross validation | Accuracy |
|---|---|---|---|---|---|
| using HSS signals | |||||
| Karimi et al., 2005 | 5 CAD and 5 normal | DWT, WPD (some statistical features) | ANN | No | 90% |
| Zhao and Ma, 2008 | 40 CAD and 40 normal | EMD, TEO (some statistical features) | BPNN | No | 85% |
| using ECG signals | |||||
| Lewenstein, 2001 | 479 CAD and 297 normal | (slope of an ST segment, blood pressure, load during the test) | Radial basis function neural networks | No | 97% |
| Babaoǧlu et al., 2010a | 480 CAD | principle component analysis | SVM | 5-fold | 79.1% |
| Babaoglu et al., 2010b | 480 CAD | binary particle swarm optimization and genetic algorithm | SVM | 5-fold | 81.46% |
| Acharya et al., 2017c | 7 CAD and 40 normal | Higher-Order Statistics and Spectra (HOS) | KNN,DT | 10-fold | 98.99% |
| Kumar et al., 2017 | 7 CAD and 40 normal | Flexible analytic wavelet transform (cross information potential) | LS-SVM | 10-fold | 99.6% |
| Normal and CAD using HRV signals | |||||
| Lee et al., 2007 | 99 CAD, 94 Normal | Linear (time domain, frequency domain) and non-linear methods (Poincare plot, approximation entropy) | Support vector machine (SVM) | 10-fold | 90% |
| Lee et al., 2008 | 99 CAD, 94 Normal | Linear (time domain, frequency domain) and non-linear methods (Poincare plot, the hurst exponent, Detrended fluctuation analysis) | CPAR & SVM: | 10-fold | 85–90% |
| Dua et al., 2012 | 10 CAD and 10 normal subjects | Non-linear methods (recurrence plots, Shannon entropy) and principal component analysis (PCA) | multilayer perceptron (MLP) | 5-fold | 89.5% |
| Giri et al., 2013 | 10 CAD and 15 normal subjects | DWT and Independent Component Analysis (ICA) | Gaussian Mixture Model (GMM) | 3-fold | 96.8% |
| Patidar et al., 2015 | 10 CAD and 10 normal subjects | TQWT and PCA (correntropy) | LS-SVM | 3-fold | 99.72% |
| Kumar et al., 2016 | 10 CAD and 10 normal subjects | FAWT and entropy | LS-SVM | 10-fold | 100% |
| In this work | 40 normal and 7 CAD subjects | RdisEn and WPD (statistical features) | KNN and SVM | 10 times 10-fold | 97.5% |
In the current study, we proposed a new entropy called RdisEn based on DisEn. Our simulation experiments with three types of signals showed that RdisEn, as an indicator of the randomness and complexities occurring in the signals, was not overly reliant on parameter selection and remained stable for even very short sequences (Figure 5, 8). It out-performed ApEn and SamEn in separating physiological (old from young) and pathological (healthy from CAD and healthy from arrhythmia) signals (Figure 3–8). The results indicate that RdisEn is a promising measure to characterize physiological and pathological condition of subjects with short-term HRV signals.
We developed an automatic CAD detection scheme combining RdisEn and WPD-based statistical features to analyze short-term HRV signals. Since the HRV signals used in this work were extracted from standard ECG signals obtained during the rest period instead of exercise, the ECG signal acquisition were harmless to the test subjects. Using only five features with KNN and the 10 × 10-fold cross validation method, the proposed scheme can differentiate normal and CAD affected HRV with 97.5% accuracy, demonstrating that our scheme outperformed other algorithms in automatic CAD detection (Table 5). It was worth mentioning that, in feature acquisition, features were extracted from a data set, which was independent of that used for the subsequent evaluation of the classifier in our work. Compared with other CAD detection schemes shown in Table 6, our scheme using RdisEn and WPD-based statistical features is more stable, rigorous and efficient. The classification accuracy achieved was significantly higher than that using WPD-based statistical features alone (97.5% vs. 90%) (Karimi et al., 2005). The p-values of 2.5e-6 and 0.033 for RdisEn by univariate and multivariable binary logistic regression method, respectively, were obtained in the process of testing the ability of RdisEn as a feature for CAD detection in this work. These indicated that RdisEn made a great contribution in distinguishing normal and CAD affected HRV signals. In the future, RdisEn can be utilized as a quantification index of irregularity within non-linear signals for the diagnosis of other diseases such as fibrillation, myocardial infarction and congestive heart failure (Acharya et al., 2017a, 2018a,b; Fujita and Cimr, 2019).
Conclusion and Future Work
Coronary artery disease is a serious cardiac abnormality, leading to high fatality. Early diagnosis and treatment of CAD can prevent progression. In this work, we proposed a new important entropy named RdisEn. It can effectively reveal the irregularity and randomness in HRV beats. A scheme for the automated differentiation between HRV signals from normal and CAD affected people has been developed, using WPD- and RdisEn-based computation, Student’s t-test selection, and classifiers to yield a classification accuracy of 97.5%, sensitivity of 100% and specificity of 95%. This novel scheme for CAD detection is reproducible, cost-effective, non-invasive, and more accessible than physical examinations such as coronary angiography and cardiac catheterization. In future works, we will apply the proposed scheme for the diagnosis of CAD and test this model in big population samples for future application.
Data Availability
Publicly available datasets were analyzed in this study. This data can be found here: https://www.physionet.org/physiobank/database/incartdb/.
Author Contributions
MS and CZ contributed to the majority of writing and conducted major parts of the experiments. YJ, HH, RW, and YS conducted some experiments and contributed to the methodology and writing. BS supervised the project and revised the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding. This study was supported by the National Key Research and Development Program of China (Grant No. 2016YFC1306605), the National Natural Science Foundation of China (Grant No. 31670851), and the Postgraduate Research and Practice Innovation Program of Jiangsu Province (KYCX18_2488), and Natural Science Foundation of Anhui Province (No. 1508085MC55).
References
- Acharya U. R., Faust O., Sree V., Swapna G., Martis R. J., Kadri N. A., et al. (2014). Linear and nonlinear analysis of normal and CAD-affected heart rate signals. Comput. Methods Programs Biomed. 113 55–68. 10.1016/j.cmpb.2013.08.017 [DOI] [PubMed] [Google Scholar]
- Acharya U. R., Fujita H., Oh S. L., Hagiwara Y., Tan J. H., Adam M. (2017a). Application of deep convolutional neural network for automated detection of myocardial infarction using ECG signals. Inf. Sci. 41 190–198. 10.1016/j.ins.2017.06.027 [DOI] [Google Scholar]
- Acharya U. R., Fujita H., Oh S. L., Hagiwara Y., Tan J. H., Adam M., et al. (2018a). Deep convolutional neural network for the automated diagnosis of congestive heart failure using ECG signals. Appl. Intell. 49 16–27. 10.1007/s10489-018-1179-1 [DOI] [Google Scholar]
- Acharya U. R., Fujita H., Oh S. L., Raghavendra U., Tan J. H., Adam M., et al. (2018b). Automated identification of shockable and non-shockable life-threatening ventricular arrhythmias using convolutional neural network. Future Gener. Comput. Syst. 79 952–959. 10.1016/j.future.2017.08.039 [DOI] [Google Scholar]
- Acharya U. R., Fujita H., Sudarshan V. K., Bhat S., Koh J. E. W. (2015a). Application of entropies for automated diagnosis of epilepsy using EEG signals: a review. Knowl. Based Syst. 88 85–96. 10.1016/j.knosys.2015.08.004 [DOI] [Google Scholar]
- Acharya U. R., Fujita H., Sudarshan V. K., Ghista D. N., Lim W. J. E., Koh J. E. W. (2015b). “Automated prediction of sudden cardiac death risk using kolmogorov complexity and recurrence quantification analysis features extracted from HRV signals,” in Proceeding of the 2015 IEEE International Conference on Systems, Man, and Cybernetics, IEEE, Kowloon. [Google Scholar]
- Acharya U. R., Fujita H., Sudarshan V. K., Shu L. O., Adam M., Koh J. E. W., et al. (2016). Automated detection and localization of myocardial infarction using electrocardiogram: a comparative study of different leads. Knowl. Based Syst. 99 146–156. 10.1016/j.knosys.2016.01.040 [DOI] [Google Scholar]
- Acharya U. R., Kannathal N., Krishnan S. M. (2004). Comprehensive analysis of cardiac health using heart rate signals. Physiol. Meas. 25 1139–1151. 10.1088/0967-3334/25/5/005 [DOI] [PubMed] [Google Scholar]
- Acharya U. R., Oh S. L., Chua C. K., Fujita H., Muhammad A., Chua K. P., et al. (2017b). Application of empirical mode decomposition (EMD) for automated identification of congestive heart failure using heart rate signals. Neural Comput. Appl. 28 3073–3094. 10.1007/s00521-016-2612-1 [DOI] [Google Scholar]
- Acharya U. R., Sudarshan V. K., Koh J. E. W., Martis R. J., Tan J. H., Oh S. L., et al. (2017c). Application of higher-order spectra for the characterization of coronary artery disease using electrocardiogram signals. Biomed. Signal Process. Control 31 31–43. 10.1016/j.bspc.2016.07.003 [DOI] [Google Scholar]
- Antanavicius K., Bastys A., Bluzas J., Gargasas L., Kaminskiene S., Urbonaviciene G., et al. (2008). Nonlinear dynamics analysis of electrocardiograms for detection of coronary artery disease. Comput. Methods Programs Biomed. 92 198–204. 10.1016/j.cmpb.2008.07.002 [DOI] [PubMed] [Google Scholar]
- Babaoǧlu I., Fındık O., Bayrak M. (2010a). Effects of principle component analysis on assessment of coronary artery diseases using support vector machine. Expert Syst. Appl. 37 2182–2185. 10.1016/j.eswa.2009.07.055 [DOI] [Google Scholar]
- Babaoglu İ, Findik O., Ülker E. (2010b). A comparison of feature selection models utilizing binary particle swarm optimization and genetic algorithm in determining coronary artery disease using support vector machine. Expert Syst. Appl. 37 3177–3183. 10.1016/j.eswa.2009.09.064 [DOI] [Google Scholar]
- Box J. F. (1987). Guinness, gosset, fisher, and small samples. Stat. Sci. 2 45–52. 10.1214/ss/1177013437 [DOI] [Google Scholar]
- Castiglioni P., Rienzo M. D. (2008). How the threshold “r” influences approximate entropy analysis of heart-rate variability”. Comput. Cardiol. 35 561–564. [Google Scholar]
- Chen W., Zhuang J., Yu W., Wang Z. (2009). Measuring complexity using FuzzyEn, ApEn, and SampEn. Med. Eng. Phy. 31 61–68. 10.1016/j.medengphy.2008.04.005 [DOI] [PubMed] [Google Scholar]
- Constant I., Laude D., Murat I., Elghozi J. L. (1999). Pulse rate variability is not a surrogate for heart rate variability. Clin. Sci. 97 391–397. 10.1042/cs0970391 [DOI] [PubMed] [Google Scholar]
- Cornforth D. J., Tarvainen M. P., Jelinek H. F. (2013). Using renyi entropy to detect early cardiac autonomic neuropathy. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2013 5562–5565. 10.1109/embc.2013.6610810 [DOI] [PubMed] [Google Scholar]
- Cornforth D. J., Tarvainen M. P., Jelinek H. F. (2014). How to calculate renyi entropy from heart rate variability, and why it matters for detecting cardiac autonomic neuropathy. Front. Bioeng. Biotechnol. 2:34. 10.3389/fbioe.2014.00034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dua S., Du X., Sree S. V., Thajudin Ahamed V. I. (2012). Novel classification of coronary artery disease using heart rate variability analysis. J. Mech. Med. Biol. 12 1240017-1-19 10.1142/s0219519412400179 [DOI] [Google Scholar]
- Duda R. O., Peter E. H., David G. S. (2012). Pattern Classification. Hoboken, NJ: Wiley-Interscience. [Google Scholar]
- Elias E., Mohammad P., Ahmad B. (2014). A novel approach to predict sudden cardiac death (SCD) using nonlinear and time-frequency analyses from HRV signals. PLoS One 9:e81896. 10.1371/journal.pone.0081896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita H., Cimr D. (2019). Computer aided detection for fibrillations and flutters using deep convolutional neural network. Inf. Sci. 486 231–239. 10.1016/j.ins.2019.02.065 [DOI] [Google Scholar]
- Giri D., Rajendra Acharya U., Martis R. J., Vinitha Sree S., Lim T.-C., Ahamed T., et al. (2013). Automated diagnosis of coronary artery disease affected patients using LDA, PCA, ICA and discrete wavelet transform. Knowl. Based Syst. 37 274–282. 10.1016/j.knosys.2012.08.011 [DOI] [Google Scholar]
- González M., Bergmeir C., Triguero I., Rodríguez Y., Benítez J. M. (2016). On the stopping criteria for k-nearest neighbor in positive unlabeled time series classification problems. Inf. Sci. 328 42–59. 10.1016/j.ins.2015.07.061 [DOI] [Google Scholar]
- Grech E. D. (2011). ABC of Interventional Cardiology. London: BMJ books. [Google Scholar]
- Hanley J. A., McNeil B. J. (1982). The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143 29–36. 10.1148/radiology.143.1.7063747 [DOI] [PubMed] [Google Scholar]
- Hayano J., Sakakibara Y., Yamada M., Ohte N., Fujinami T., Yokoyama K., et al. (1990). Decreased magnitude of heart rate spectral components in coronary artery disease. Its relation to angiographic severity. Circulation 81 1217–1224. 10.1161/01.cir.81.4.1217 [DOI] [PubMed] [Google Scholar]
- Huikuri H. V., Niemela M. J., Ojala S., Rantala A., Ikaheimo M. J., Airaksinen K. E. (1994). Circadian rhythms of frequency domain measures of heart rate variability in healthy subjects and patients with coronary artery disease. Circulation 90 121–126. 10.1161/01.cir.90.1.121 [DOI] [PubMed] [Google Scholar]
- Karimi M., Amirfattahi R., Sadri S., Marvasti S. A. (2005). “Noninvasive detection and classification of coronary artery occlusions using wavelet analysis of heart sounds with neural networks,” in Proceedings of the The 3rd IEE International Seminar on Medical Applications of Signal Processing 2005, London: IET. [Google Scholar]
- Karmakar C., Udhayakumar R. K., Li P., Venkatesh S., Palaniswami M. (2017). Stability, consistency and performance of distribution entropy in analysing short length heart rate variability (HRV) signal. Front. Physiol. 8:720. 10.3389/fphys.2017.00720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar M., Pachori R. B., Acharya U. R. (2016). An efficient automated technique for cad diagnosis using flexible analytic wavelet transform and entropy features extracted from hrv signals. Int. J. 63 165–172. 10.1016/j.eswa.2016.06.038 [DOI] [Google Scholar]
- Kumar M., Pachori R. B., Acharya U. R. (2017). Characterization of coronary artery disease using flexible analytic wavelet transform applied on ECG signals. Biomed. Signal Process. Control 31 301–308. 10.1016/j.bspc.2016.08.018 [DOI] [Google Scholar]
- Lavoie K. L., Fleet R. P., Laurin C., Arsenault A., Miller S. B., Bacon S. L. (2004). Heart rate variability in coronary artery disease patients with and without panic disorder. Psychiatr. Res. 128 289–299. 10.1016/j.psychres.2004.06.005 [DOI] [PubMed] [Google Scholar]
- Lee H. G., Noh K., Ryu K. H. (2008). “A data mining approach for coronary heart disease prediction using hrv features and carotid arterial wall thickness,” in Proceeding of the 2008 International Conference on BioMedical Engineering and Informatics, Sanya: IEEE. [Google Scholar]
- Lee H. G., Noh K. Y., Ryu K. H. (2007). Mining Biosignal Data: Coronary Artery Disease Diagnosis Using Linear and Nonlinear Features of HRV. Berlin: Springer-Verlag. [Google Scholar]
- Lewenstein K. (2001). Radial basis function neural network approach for the diagnosis of coronary artery disease based on the standard electrocardiogram exercise test. Med. Biol. Eng. Comput. 39 362–367. 10.1007/BF02345292 [DOI] [PubMed] [Google Scholar]
- Li P., Liu C., Li K., Zheng D., Liu C., Hou Y. (2015). Assessing the complexity of short-term heartbeat interval series by distribution entropy. Med. Biol. Eng. Comput. 53 77–87. 10.1007/s11517-014-12160 [DOI] [PubMed] [Google Scholar]
- Li T., Zhou M. (2016). ECG classification using wavelet packet entropy and random forests. Entropy 18:285 10.3390/e18080285 [DOI] [Google Scholar]
- Liang Z., Wang Y., Sun X., Li D., Voss L. J., Sleigh J. W., et al. (2015). EEG entropy measures in anesthesia. Front. Comput. Neurosci. 9:16. 10.3389/fncom.2015.00016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., Liu C., Shao P., Li L., Sun X., Wang X., et al. (2011). Comparison of different threshold values r for approximate entropy: application to investigate the heart rate variability between heart failure and healthy control groups. Physiol. Meas. 32 167–180. 10.1088/0967-3334/32/2/002 [DOI] [PubMed] [Google Scholar]
- Lu S., Chen X., Kanters J. K., Solomon I. C., Chon K. H. (2008). Automatic selection of the threshold value R for approximate entropy. IEEE Trans. Biomed. Eng. 55 1966–1972. 10.1109/tbme.2008.919870 [DOI] [PubMed] [Google Scholar]
- Martis R. J., Acharya U. R., Min L. C. (2013). ECG beat classification using PCA, LDA, ICA and discrete wavelet transform. Biomed. Signal Process. Control 8 437–448. 10.1016/j.bspc.2013.01.005 [DOI] [Google Scholar]
- Mayer C. C., Bachler M., Hortenhuber M., Stocker C., Holzinger A., Wassertheurer S. (2014). Selection of entropy-measure parameters for knowledge discovery in heart rate variability data. BMC Bioinformatics 15(Suppl. 6):S2. 10.1186/1471-2105-15-s6-s2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan J., Tompkins W. J. (2007). A real-time QRS detection algorithm. IEEE Trans. Biomed. Eng. 32 230–236. 10.1109/tbme.1985.325532 [DOI] [PubMed] [Google Scholar]
- Patidar S., Pachori R. B., Rajendra Acharya U. (2015). Automated diagnosis of coronary artery disease using tunable-Q wavelet transform applied on heart rate signals. Knowl. Based Syst. 82 1–10. 10.1016/j.knosys.2015.02.011 [DOI] [Google Scholar]
- Peng C. K., Havlin S., Hausdorff J. M., Mietus J. E., Stanley H. E., Goldberger A. L. (1995). Fractal mechanisms and heart rate dynamics. Long-range correlations and their breakdown with disease. J. Electrocardiol. 28(Suppl.), 59–65. 10.1016/s0022-0736(95)80017-4 [DOI] [PubMed] [Google Scholar]
- Pincus S. M. (1991). Approximate entropy as a measure of system complexity. Proc. Natl. Acad. Sci. U.S.A. 88 2297–2301. 10.1073/pnas.88.6.2297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajendra A. U., Bhat P. S., Kannathal N., Rao A., Lim C. M. (2005). Analysis of cardiac health using fractal dimension and wavelet transformation. IRBM 26 133–139. 10.1016/j.rbmret.2005.02.001 [DOI] [Google Scholar]
- Rajendra Acharya U., Vidya K. S., Ghista D. N., Lim W. J. E., Molinari F., Sankaranarayanan M. (2015). Computer-aided diagnosis of diabetic subjects by heart rate variability signals using discrete wavelet transform method. Knowl. Based. Syst. 81 56–64. 10.1016/j.knosys.2015.02.005 [DOI] [Google Scholar]
- Román J. A., San Vilacosta I., Castillo J. A., Rollán M. J., Hernández M., et al. (1998). Selection of the optimal stress test for the diagnosis of coronary artery disease. Heart 80 370. 10.1136/hrt.80.4.370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sridhar C., Acharya U. R., Fujita H., Bairy G. M. (2017). “Automated diagnosis of coronary artery disease using nonlinear features extracted from ECG signals,” in Proceedings of the 2016 IEEE International Conference on Systems, Man, and Cybernetics (SMC), Budapest: IEEE. [Google Scholar]
- Steinberg D., Gotto A. M. (1999). Preventing coronary artery disease by lowering cholesterol levels: fifty years from bench to bedside. JAMA 282:2043. 10.1001/jama.282.21.2043 [DOI] [PubMed] [Google Scholar]
- Udhayakumar R. K., Karmakar C., Peng L., Palaniswami M. (2016). “Influence of embedding dimension on distribution entropy in analyzing heart rate variability,” in Proceeding of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL: IEEE. [DOI] [PubMed] [Google Scholar]
- World Health, and Organization. (2015). Global status report on noncommunicable diseases 2014. Women 47 2562–2563. [Google Scholar]
- Xie H., He W., Liu H. (2008). Measuring time series regularity using nonlinear similarity-based sample entropy. Phys. Lett. A 372 7140–7146. 10.1016/j.physleta.2008.10.049 [DOI] [Google Scholar]
- Yang L., Peng L., Karmakar C., Liu C. (2015). ““Distribution entropy for short-term QT interval variability analysis: a comparison between the heart failure and normal control groups,” in Proceedings of the 2015 Computing in Cardiology Conference (CinC), Nice: IEEE. [Google Scholar]
- Zhang T., Chen W., Li M. (2018). Fuzzy distribution entropy and its application in automated seizure detection technique. Biomed. Signal Process. Control 39 360–377. 10.1016/j.bspc.2017.08.013 [DOI] [Google Scholar]
- Zhao Z., Ma C. (2008). “An intelligent system for noninvasive diagnosis of coronary artery disease with EMD-TEO and BP neural network,” in Education Technology and Training & Geoscience and Remote Sensing, Vol. 2 (Shanghai: IEEE; ), 631–635. 10.1109/ETTandGRS.2008.361 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.physionet.org/physiobank/database/incartdb/.