Abstract
Background
The ginsenoside Rg3, one of active components of red ginseng, has chemopreventive and anticancer potential. Cancer stem cells retain self-renewal properties which account for cancer recurrence and resistance to anticancer therapy. In our present study, we investigated whether the standardized Korean Red Ginseng extract (RGE) and Rg3 could modulate the manifestation of breast cancer stem cell–like features through regulation of self-renewal activity.
Methods
The effects of RGE and Rg3 on the proportion of CD44high/CD24low cells, as representative characteristics of stem-like breast cancer cells, were determined by flow cytometry. The mammosphere formation assay was performed to assess self-renewal capacities of breast cancer cells. Aldehyde dehydrogenase activity of MCF-7 mammospheres was measured by the ALDEFLUOR assay. The expression levels of Sox-2, Bmi-1, and P-Akt and the nuclear localization of hypoxia inducible factor-1α in MCF-7 mammospheres were verified by immunoblot analysis.
Results
Both RGE and Rg3 decreased the viability of breast cancer cells and significantly reduced the populations of CD44high/CD24low in MDA-MB-231 cells. RGE and Rg3 treatment attenuated the expression of Sox-2 and Bmi-1 by inhibiting the nuclear localization of hypoxia inducible factor-1α in MCF-7 mammospheres. Suppression of the manifestation of breast cancer stem cell–like properties by Rg3 was mediated through the blockade of Akt-mediated self-renewal signaling.
Conclusion
This study suggests that Rg3 has a therapeutic potential targeting breast cancer stem cells.
Keywords: Breast cancer stem cells, Ginseng, Ginsenoside Rg3, Red ginseng extract, Self-renewal
1. Introduction
According to 2012 global statistics, breast cancer is the second death malignancies in the women worldwide [1]. Although several therapeutic options have been suggested for patients with breast cancer, the incidence and relapse of this malignancy are still forecasted to continuously increase [2]. Interestingly, patients retaining CD44high/CD24low breast stem-like cancer cells have a higher recurrence rate than those having CD44low/CD24high non–stem breast cancer cells [3]. The conventional treatment of various tumors has been largely unsuccessful which may be due to the survival of cancer stem cells (CSCs) present in a small proportion of cancer cell population within a tumor microenvironment. CSCs are considered to confer resistance to anticancer therapy as well as enhanced tumor growth, metastasis, and recurrence [4]. In this context, CSC-targeted therapies, which accentuate their efficacy in eliminating the fundamental cause of cancer rather than tumor bulk, have attracted special attention [5].
Self-renewal capacity is critical for maintaining features of stem-like cancer cells and sustaining mother stem cell property [6]. Upregulation of Bmi-1 and Sox-2 expression has been recognized as molecular signature in stem-like breast cancer cells [7], [8]. Bmi-1 is a polycomb group family protein involved in the maintenance of CSCs as an epigenetic modifier [9]. Bmi-1 is highly expressed in stem-like breast cancer cells and is indispensable for regulation of self-renewal signaling [8], [10]. Sox-2, a regulator of cell fate during development, also plays a role in the maintenance of CSCs. It has been reported that the overexpression of Sox-2 in CSCs presents the coherent induction of self-renewal signaling, eventually leading to tumor progression [11]. Based on these findings, Bmi-1 and Sox-2 are considered to lie in the central node of self-renewal machinery of CSCs.
Recently, red ginseng extract (RGE) has been used in Asian countries because of its remedial potential in the management of various symptoms as well as maintenance or improvement of health [12], [13], [14], [15]. Among the different components of RGE, ginsenosides are identified to be responsible for the majority of its biological activities. Notably, some ginsenosides in raw ginseng are converted into different forms by the heat treatment during the RGE production [16], [17]. Rg3 is one such archetype of RGE which is barely detected in raw ginseng, but its content markedly increases through the steaming process. Considering these perspectives, it could be suggested that the increased content of Rg3 constitutes a principle axis of the enhanced pharmacological activities of RGE.
It has been reported that the ginsenoside Rg3 has the cytotoxic activity toward cancer cells [18]. Rg3 exerts direct anticancer effects by inhibiting tumor growth and inducing apoptotic cell death [19], [20]. Nonetheless, the mechanism by which Rg3 regulates the signal transduction pathway involved in the maintenance of CSCs and manifestation of their properties still remains to be largely explored. Therefore, we have examined the effects of the ginsenoside Rg3 on manifestation and maintenance of breast cancer stem cell–like properties in the context of its novel anticancer activity.
2. Materials and methods
2.1. Reagents and antibodies
The standardized Korean Red Ginseng extract powder and 20-(S)-Rg3 (purity: 96.1%) were supplied by the Korean Ginseng Corporation (KGC; Daejeon, Korea). The main components of the RGE powder are 1.91 mg/g ginsenoside-Rg1, 2.17 mg/g Re, 1.56 mg/g Rf, 1.71 mg/g Rh1, 1.67 mg/g Rg2s, 9.14 mg/g Rb1, 4.16 mg/g Rc, 3.38 mg/g Rb2, 1.36 mg/g Rd, 2.37 mg/g Rg3s, and 1.11 mg/g Rg3r. The water content is 5.29% of the total weight. Cell culture medium was purchased from Gibco BRL (Grand Island, NY, USA), and fetal bovine serum (FBS) was obtained from GenDEPOT (Barker, TX, USA). Primary antibodies for Bmi-1, Sox-2, P-Akt (S473), Akt, and extracellular signal-regulated kinases (ERK) were supplied by Cell Signaling Technology (Danvers, MA, USA). Antibodies against Lamin B1, P-ERK, and β-actin were purchased from Santa Cruz Biotechnology (Dalls, TX, USA). Antibodies against CD24 and hypoxia inducible factor-1α (HIF-1α) were purchased from BD Biosciences (Bedford, MA, USA). Antibody against CD44 was purchased from eBioscience (San Diego, CA, USA). The Akt inhibitor (LY294002) was a product of TOCRIS (Bristol, United Kingdom).
2.2. Cell culture
Human breast cancer (MCF-7 and MDA-MB-231) cell lines obtained from the Korean Cell Line Bank (Seoul, Korea) were maintained at 37°C in a humid atmosphere of 5% CO2/95% air in Roswell Park Memorial Institute (RPMI) and complete Dulbecco's Modified Eagle's Medium (DMEM) complete media, respectively [21]. Each medium contains 10% FBS and 1% antibiotics.
2.3. Mammosphere formation assay
MCF-7 and MDA-MB-231 cells were cultured in a serum free DMEM/F12 medium supplemented with B27 (Gibco), 20 ng/mL epidermal growth factor (Sigma-Aldrich, St. Louis, MO, USA), 20 ng/mL basic fibroblast growth factor (PeproTech, Rocky Hill, NJ, USA), and 4 ng/mL heparin (Sigma-Aldrich) [22]. Primary mammospheres were seeded at a density dependent on cell types in 100 mm ultralow attachment plates (Corning, NY, USA) for 7 consecutive days, and the cells were maintained by addition of the medium every 2–3 days. To culture secondary mammospheres, primary mammospheres were gently collected and spheres were dissociated into a single-cell suspension using 40 μm strainer. Single cells were counted and then seeded again for another 5 days by addition of medium every 2–3 days. Using the same experimental method, tertiary mammospheres were generated with or without treatment of RGE or Rg3. The number of mammospheres formed (>100 μm) was counted at indicated times under a microscope.
2.4. Flow cytometry analysis
Cells were collected and dissociated with Accutase solution (Sigma-Aldrich). After washing with phosphate buffered saline (PBS) and suspension in Hank’s Buffered Salt Solution (HBSS) solution containing 2% FBS and 0.1% Tween-20, cells were stained with CD24-PE and CD44-APC incubated in rotator at 4°C. Following dissociation into single cells by using 40 μm strainer, the proportion of CD44high/CD24low cells were measured using BD FACSCalibur (Becton Dickinson Biosciences, San Jose, CA, USA).
2.5. ALDEFLUOR assay
The ALDEFLUOR kit (StemCell Technologies, Durham, NC, USA) was used to measure the cells that express aldehyde dehydrogenase (ALDH) enzyme activity. The vehicle-treated MCF-7 mammospheres were incubated with an ALDH specific inhibitor, diethylaminobenzaldehyde, to assess background fluorescence. The sorting gates were established by eliminating the cells stained positive with ALDH in a negative control group following the method described by Ginestier et al [23]. Samples were analyzed by the FACSCalibur (Becton Dickinson Biosciences).
2.6. Western blot analysis
To obtain the protein sample from cell lysates, cells were washed with cold PBS and suspended in cell lysis buffer according to the procedure described earlier [21]. For nuclear and cytosolic extractions, cell pellets were suspended in hypotonic buffer [10 mM HEPES (pH 7.8), 1.5 mM MgCl2, 10 mM KCl, 0.5 mM dithiothreitol, 0.2 mM phenylmethylsulfonyl fluoride (PMSF)]. After incubation for 10 min on ice and centrifugation at 5,200 g for 6 min, supernatant was collected as a cytosolic fraction. The residual pellets were suspended in hypertonic buffer [20 mM HEPES (pH 7.8), 1.5 mM MgCl2, glycerol, 420 mM NaCl, 0.5 mM dithiothreitol, 0.2 mM PMSF, and 0.2 mM EDTA] and incubated on ice for 30 min. Protein samples were subjected to immunoblot analysis, as described previously [21].
2.7. Transient transfection of HIF-1α siRNA
Tertiary MCF-7 mammospheres were seeded in 6-well ultralow attachment plate (5 × 103 cells/mL) in mammosphere culture media. HIF-1α siRNA was transfected into mammospheres with lipofectamin RNAiMAX reagents (Invitrogen, Carlsbad, CA, USA) following the method described by Kim et al [21]. Human HIF-1α siRNA sequence was 5′–GUGGUUGGAUCUAACACUA–3′ (forward) and 5′–UAGUGUUAGAUCCAACCAC–3′ (reverse). siRNA oligonucleotide targeting HIF-1α was purchased from Bioneer (Daejeon, Korea).
2.8. Cell viability assay
Cells were seeded in 8,000 cells per well in a 48-well plate. One day after seeding, the cells were incubated with RGE and Rg3, following the method described by Kim et al [24]. The absorbance was measured at 570 nm using a microplate reader (Bio-Rad Laboratories, Hercules, California, USA).
2.9. Statistical analysis
Data were represented as the mean ± standard deviation of three independent experiments. Statistical analysis between groups was determined by the Student's t test. A value p < 0.05 was considered to be statistically significant.
3. Results
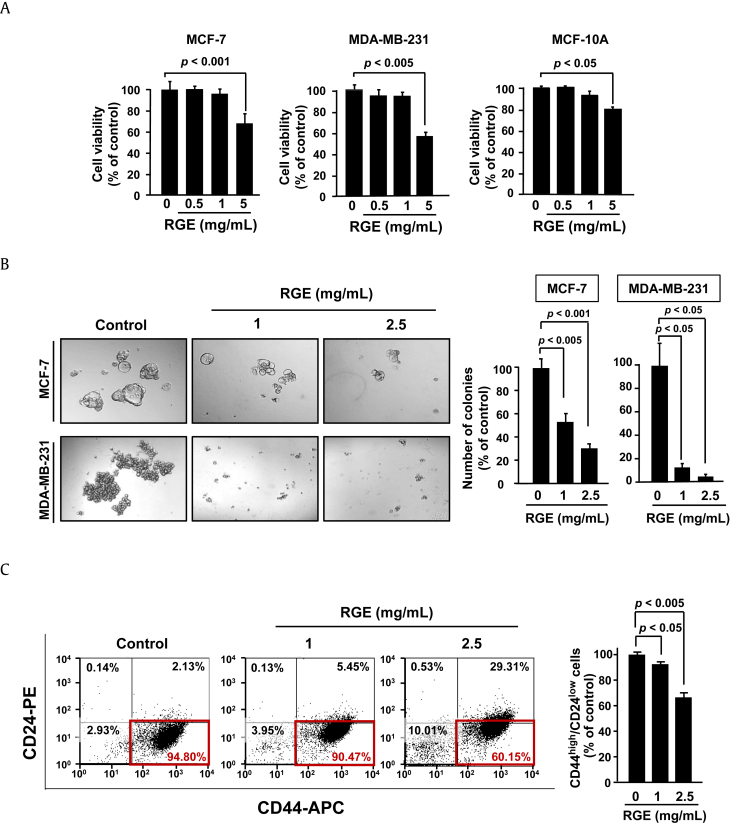
3.1. RGE reduces the viability and attenuates stemness of breast cancer cells
First, we investigated the effects of RGE on the viability of human breast cancer (MCF-7 and MDA-MB-231) cells and normal mammary epithelial (MCF-10A) cells. Treatment of these cells with RGE at relatively low concentrations (0.5 and 1 mg/mL) did not affect the cell viability. However, incubation with 5 mg/mL of RGE for 48 h resulted in cytotoxic effect in both breast cancer cell lines and to a lesser extent, in normal mammary epithelial MCF-10A cells (Fig. 1A). Therefore, in determining the effects of RGE on self-renewal activity of stem-like breast cancer cells, noncytotoxic concentrations (1 and 2.5 mg/mL) were used. The mammosphere formation assay is widely used to identify stem cells based on the self-renewal activity [25]. To generate mammospheres, breast cancer cells were cultured in ultralow attachment surface plates enriched with serum-free stem cell media through serial passages. MCF-7 and MDA-MB-231 mammospheres were then incubated with RGE (1 and 2.5 mg/mL) for 5 days. As a result, RGE treatment significantly inhibited the number and the size of mammospheres in MCF-7 and MDA-MB-231 cells (Fig. 1B). These results suggest that RGE could inhibit self-renewal ability of stem-like breast cancer cells. The different cell populations within a tumor can be identified using the signature of specific proteins expressing on the surface of particular cells [26]. For example, CD44high/CD24low breast stem-like cancer cells promote the tumorigenesis in breast cancer tissue [3]. When MDA-MB-231 cells were treated with RGE (1 and 2.5 mg/mL) for 48 h, the proportion of the CD44high/CD24low cell population was decreased in a concentration-dependent manner, indicating that RGE abrogated the manifestation of breast cancer stem cell–like properties (Fig. 1C).
Fig. 1.
Effects of RGE on viability and stemness properties of breast cancer cells. (A) MCF-7, MDA-MB-231, and MCF-10A cells were treated with RGE (0.5, 1 or 5 mg/mL) or vehicle for 48 h. The data are presented as means ± SD. (B) At the tertiary mammosphere state, cells cultured in a 96-well ultralow attachment surface plate were treated with RGE (1 or 2.5 mg/mL) for 5 days. The number, the size, and the shape of mammospheres were examined by phase-contrast microscopy. Illustrations are the representative phase-contrast photomicrographs of mammospheres, and the graph bars are presented based on the number of mammospheres bigger than 100 μm. The values are presented as means ± SD (n = 3). (C) MDA-MB-231 cells treated with 1 or 2.5 mg/mL of RGE for 48 h were stained with anti-CD44-APC and anti-CD24-PE. Flow cytometric dot plots represent changes in the proportion of CD44high/CD24low cells. Quadrant analysis of fluorescence intensity of gated cells in FL2 and FL4 channels was from 10,000 events. Numerical values in the cytogram indicate the percentage of gated cells in each quadrant. The values are expressed as means ± SD (n = 3). APC, allophycocyanin; RGE, red ginseng extract; SD, standard deviation.
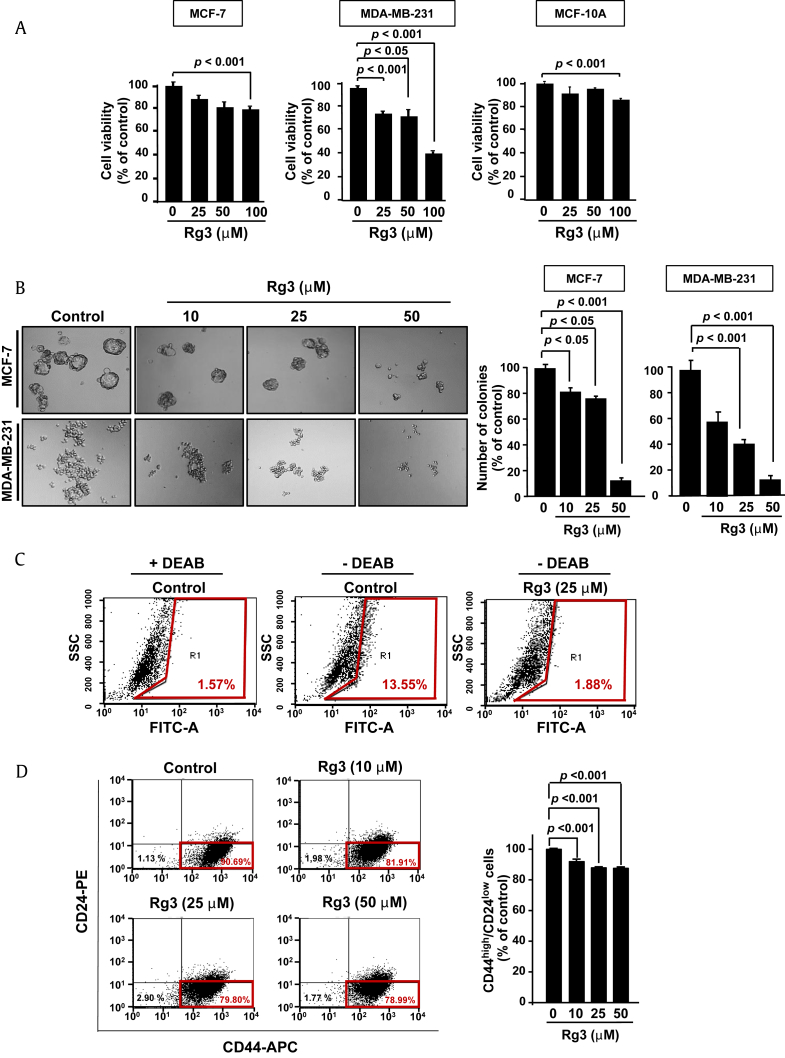
3.2. Rg3 reduces the viability of breast cancer cells and alleviates their stemness properties
Rg3 is one of the major components of RGE and has chemopreventive/chemotherapeutic potential [20], [27], [28]. The distinct biological activities of red ginseng have been considered to arise from a change in the chemical constituents that occurs during the steaming process [16]. In an initial experiment, the effect of Rg3 on the cell viability of breast cancer cells was examined. MCF-7 and MDA-MB-231 cells were incubated with different concentrations of Rg3 (25, 50, or 100 μM) for 72 h. This concentration range was based on other reports [19], [24]. As shown in Fig. 2A, Rg3 reduced the viability of both MCF-7 and MDA-MB-231 cells in a concentration-dependent manner whereas it barely caused cytotoxicity to normal mammary epithelial (MCF-10A) cells. After confirming that RGE treatment inhibited the self-renewal capacity of MCF-7 and MDA-MB-231 mammospheres, a similar effect was assessed for Rg3 treatment. Treatment of MCF-7 and MBA-MB-231 tumorspheres with different concentrations of Rg3 (10, 25, and 50 μM) reduced the number and the size of spheres (Fig. 2B). The aldefluor assay measuring the oxidation of intracellular aldehydes is widely used to identify the stem-like breast cancer cells with elevated ALDH activity [23]. The stem-like breast cancer cells containing ALDH-positive subpopulation have the capacity to self-renew and regenerate [23]. Rg3 (25 μM) was treated twice at 2-day intervals for 5 days during the tertiary mammosphere formation. Diethylaminobenzaldehyde, a specific inhibitor of ALDH, was utilized for measuring the background enzyme activity of the negative control group. The ALDH activity, which was elevated in the absence of its inhibitor, was markedly suppressed upon Rg3 treatment (Fig. 2C). Subsequently, we examined the effect of Rg3 on the proportion of CD24 and CD44 proteins expressed on the cell surface of MDA-MB-231 cells. Rg3 treatment significantly reduced the proportion of CD44high/CD24low cells (Fig. 2D).
Fig. 2.
Effects of Rg3 on viability and stemness properties of breast cancer cells. (A) MCF-7, MDA-MB-231, and MCF-10A cells were treated with Rg3 (25, 50 or 100 μM) for 72 h. The data are presented as means ± SD. (B) On tertiary mammosphere formation, Rg3 was treated twice at an interval of 2 days during the 5 days of maintenance. The number, the size, and the shape of mammospheres were examined by phase-contrast microscopy. Pictures are the representative phase-contrast photomicrographs of mammospheres, and the graph bars are presented based on the number of mammospheres bigger than 100 μm. The values are presented as means ± SD (n = 3). (C) MCF-7 mammospheres were subjected to the ALDFLUOR assay, followed by flow cytometry to detect cells with the ALDH activity. Tertiary MCF-7 mammospheres were treated with Rg3 (25 μM) twice at an interval of 2 days during the 5 days of maintenance. An ALDH inhibitor, DEAB was used to assess the background fluorescence. Quadrant analysis of fluorescence intensity of gated cells in FL1 channels was from 10,000 events. Numerical values in the plots indicate the percentage of gated cells in R1 quadrant. (D) MDA-MB-231 cells treated with Rg3 (10, 25 or 50 μM) for 48 h were stained with anti-CD44-APC and anti-CD24-PE. Flow cytometric dot plots represent changes in the proportion of CD44high/CD24low cells. Quadrant analysis of fluorescence intensity of gated cells in FL2 and FL4 channels was from 10,000 events. Numerical values in the cytogram indicate the percentage of gated cells in each quadrant. The values are expressed as means ± SD (n = 3).ALDH, aldehyde dehydrogenase; APC, allophycocyanin; DEAB, diethylaminobenzaldehyde; SD, standard deviation.
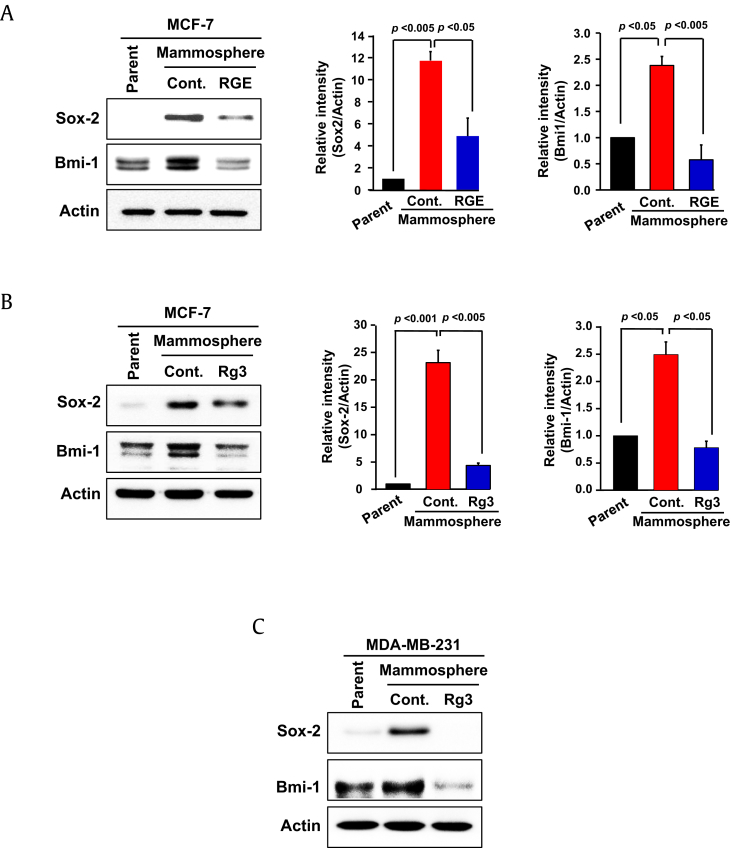
3.3. RGE and Rg3 reduce the expression of self-renewal signaling molecules in stem-like breast cancer cells
Self-renewal is the predominant property of CSCs that accounts for the regeneration of the tumor in all aspects [10]. Bmi-1 is one of the critical proteins in regulation of self-renewal signaling [29], [30]. Overexpression or deregulation of Bmi-1 is frequently found in human breast cancer tissues [5]. Moreover, upregulation of the transcription factor Sox-2 is essential for self-renewal capability in tumor initiating cells [31]. Because tertiary MCF-7 mammospheres bear most of the fundamental features of CSCs, such as self-renewal capacity, expression of Sox-2 and Bmi-1 in tertiary mammospheres was compared to that of the parent breast cancer cells. Mammospheres exhibited the increased protein expression of Sox-2 and Bmi-1, which was decreased by RGE treatment (Fig. 3A). The concurrent results were observed in mammospheres derived from MCF-7 (Fig. 3B) and MDA-MB-231 (Fig. 3C) cells treated with Rg3. These findings suggest that RGE and Rg3 are likely to modulate self-renewal ability through inhibition of Sox-2 and Bmi-1 signaling in stem-like breast cancer cells.
Fig. 3.
Effects of RGE and Rg3 on self-renewal signaling of stem-like breast cancer cells. (A) On tertiary mammosphere formation, MCF-7 mammospheres were treated with RGE (1 mg/mL) twice at an interval of 2 days during the 5 days of maintenance. (B, C) MCF-7 and MDA-MB-231 mammospheres were treated with Rg3 (25 μM) in the same manner. The protein levels of Sox-2 and Bmi-1 were measured by Western blot analysis. The values are presented means ± SD (n = 3). RGE, red ginseng extract; SD, standard deviation.
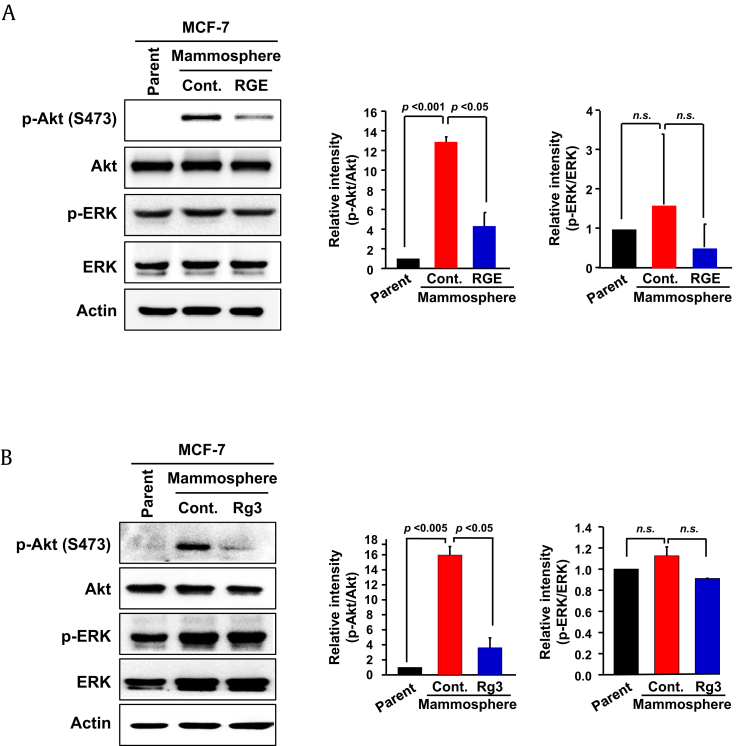
3.4. RGE and Rg3 inhibit phosphoinositide 3-kinase signaling in MCF-7 mammospheres
In addition to Bmi-1 and Sox-2, Akt-related signaling molecules have also been suggested as a master regulator of self-renewal capability of CSCs [32]. Moreover, a recent study has proposed the critical role of the ERK/mitogen-activated protein kinase (MAPK) signaling pathway in drug resistance of cancer cells [33]. To further verify the molecular basis for the inhibition of self-renewal capacity by RGE and Rg3, their effects on the activity of Akt and ERK in MCF-7 mammospheres were explored. As illustrated in Figs. 4A, 4B, treatment of RGE and Rg3 strongly inhibited the phosphorylation of Akt which was constitutively overexpressed in MCF-7 mammospheres. However, neither phosphorylation nor expression of ERK was altered by RGE or Rg3 treatment under the same experimental conditions.
Fig. 4.
Effects of RGE and Rg3 on phosphorylation of Akt in MCF-7 mammospheres. Tertiary MCF-7 mammospheres were generated. The expression and phosphorylation of Akt were determined after treatment with RGE or Rg3. (A) With RGE (1 mg/mL) for 5 days. (B) With Rg3 (25 μM) for 5 days. The whole lysates were subjected to Western blot analysis. The values are presented means ± SD (n = 3). n.s., nonsignificant; RGE, red ginseng extract; SD, standard deviation.
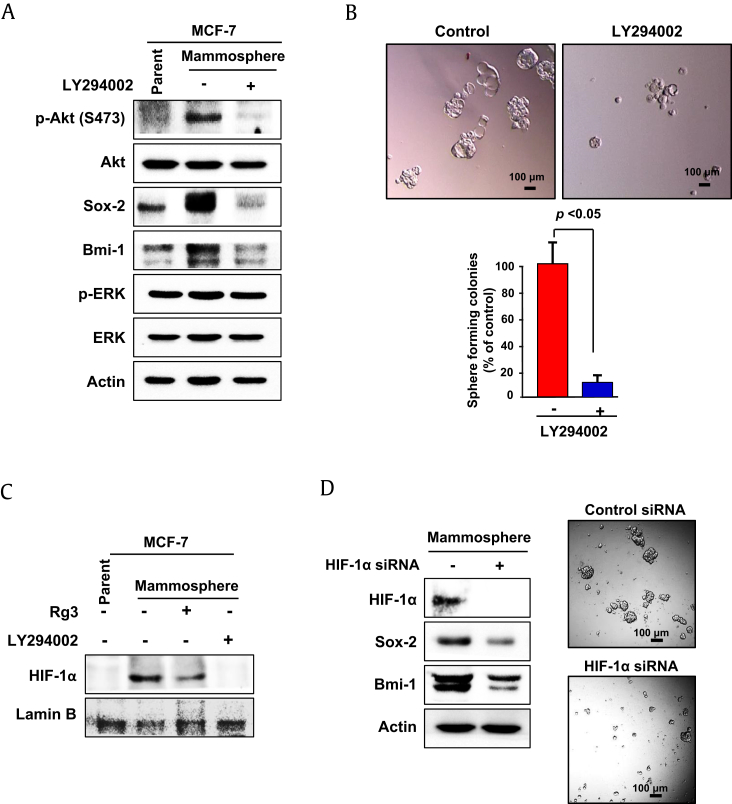
3.5. The phosphoinositide 3-kinase pathway regulates self-renewal signaling, and HIF-1α may be a potential modulator of Akt-mediated self-renewal signaling in MCF-7 mammospheres
In order to investigate whether Akt can regulate self-renewal activity of stem-like breast cancer cells, we used LY294002, a specific inhibitor of phosphoinositide 3-kinase (PI3K), an upstream of Akt. The pharmacological inhibition of Akt abolished the expression of Sox-2 and Bmi-1 (Fig. 5A) and further reduced the number and the size of MCF-7 mammospheres (Fig. 5B). These results support the notion that the PI3K signaling pathway modulates breast CSC-like properties via regulation of self-renewal signaling. However, a question that still needs to be addressed is how Akt regulates self-renewal signaling. As seen in the present study, Akt acts as an upstream signaling molecule that modulates the expression of Sox-2 and Bmi-1. To validate the correlation between Akt and self-renewal signaling, we examined a possible candidate signaling molecule that could regulate downstream molecules, Sox-2 and Bmi-1. Notably, HIFs have been reported to upregulate the expression of stem-cell associated molecules [34], [35]. Among these, HIF-1α is a well-known transcription factor which acts by binding to the HIF-responsive elements present in the promotor of target genes [36]. The nuclear accumulation of HIF-1α was higher in mammospheres than in parent MCF-7 cells (Fig. 5C). In addition, treatment of MCF-7 mammospheres with Rg3 or the Akt inhibitor blocked the nuclear localization of HIF-1α. The ablation of HIF-1α expression by use of siRNA attenuated the expression of Sox-2 and Bmi-1 and reduced the number and the size of MCF-7 mammospheres compared to those of control (Fig. 5D).
Fig. 5.
Involvement of the PI3K-Akt axis and a possible role of HIF-1α in self-renewal signaling of MCF-7 mammospheres. (A) LY294002, an Akt inhibitor was treated for 3 days to tertiary MCF-7 mammospheres. The expression of Sox-2 and Bmi-1 was measured by Western blot analysis. (B) The effect of LY294002 on mammosphere formation was confirmed by the mammosphere assay. The number, the size, and the shape of mammospheres were examined by phase-contrast microscopy. The graph represents the number of spheres that were bigger than 100 μm. The values are indicated as means ± SD (n = 3). (C) Tertiary MCF-7 mammospheres were treated with Rg3 (25 μM) or LY294002 (20 μM) for 5 and 3 days, respectively. Nuclear and cytosolic fractions were isolated from the cells and the localization of HIF-1α in MCF-7 mammospheres was measured by Western blot analysis. (D) Tertiary MCF-7 mammospheres were transfected with HIF-1α siRNA on the tertiary mammosphere formation for 72 h before the sample collection. The expression of Sox-2 and Bmi-1 was measured by Western blot analysis. The effect of HIF-1α knockdown on the formation of mammospheres was examined by phase-contrast microscopy. Pictures are the representative phase-contrast photomicrographs of mammospheres. HIF-1α, hypoxia inducible factor-1α; PI3K, phosphoinositide 3-kinase; SD, standard deviation.
4. Discussion
It has been known that the presence of CSCs in tumor tissues confers resistance to chemotherapeutic agents, which often leads to recurrence in various human cancers [37]. Therapeutic drugs used to treat breast cancer include cisplatin, doxorubicin, paclitaxel, etc. Among them, paclitaxel acts by binding to microtubules with high affinity to block disassembly of microtubules [38]. It has been reported that the upregulation of class III β-tubulin augments the resistance to paclitaxel treatment and cancer progression in advanced breast cancer patients [39]. In addition, treatment of human triple negative breast cancer with paclitaxel resulted in an increase of HIF expression and its transcriptional activity, which enriched the breast CSC population to acquire chemoresistance through interleukin-6 and interleukin-8 signaling [40]. According to the above study, the combinatorial therapy of HIF inhibitors and paclitaxel was effective to overcome the resistance of CSCs [40]. Therefore, it has been suggested that the therapeutic effects of traditional chemotherapy or radiotherapy could be improved by employing combinational treatment targeting CSCs. In this context, natural products are good candidates for combination with synthetic chemotherapeutic drugs.
Rg3, a pharmacologically active ingredient of red ginseng, has been extensively investigated in regard to chemotherapeutic as well as chemopreventive effects exerted by itself or combination treatment. There are several different types of ginsenosides present in RGE. Approximately, 50 kinds of ginsenosides have been identified, and it has been reported that some ginsenosides are converted into different forms by the heat treatment during the RGE production [16], [17]. As a representative RGE-derived ginsenoside, Rg3 exerts cancer chemopreventive and antitumor effects through multiple mechanisms. Rg3 exists in two stereoisomers, 20-(S)-Rg3 and 20-(R)-Rg3, depending on the orientation of the C-20 hydroxyl group. According to Nag et al, this difference in the stereochemistry produces different pharmacological effects [41]. It has been reported that the 20-(S)-Rg3 possesses better antiproliferative effects in cancer than 20-(R)-Rg3 counterparts because of its orientation of the C-20 hydroxyl, making the molecule act as a more efficient regulator of ion channels [41], [42]. Rg3 inhibits the growth of colon cancer cell lines through attenuation of Wnt signaling [19]. Rg3 also induces apoptosis in human leukemia by suppressing the PI3K/Akt pathway [20]. Several studies have presented the synergistic and sensitizing effects of Rg3 in bladder and prostate cancer when used in combination with chemotherapeutic agents [43], [44], [45].
Notwithstanding the great efficacy of Rg3 in suppressing proliferation or growth of cancer cells, its effect on the oncogenic potential of CSCs remains largely unexplored. Some dietary cancer preventive phytochemicals have the capacity to interfere with the various signal molecules which are essential for the maintenance of CSCs [26]. For instance, curcumin, epigallocatechin gallate, and genistein decrease the population of CSCs through downregulation of STAT3, Hedgehog, and nuclear factor-kappa B (NF-kB) signaling pathways [46], [47]. Regarding the effects of different types of ginsenosides present in RGE on CSCs, the ginsenoside Rb1 exerted potent cytotoxicity in ovarian CSCs by targeting Wnt/β-catenin signaling [6]. In addition, the ginsenoside Rh2 was reported to inhibit the effect on the growth of the squamous skin cell carcinoma by reducing the expression Lgr5, an intestinal epithelium stem cell–associated marker [48]. In line with these previous reports, our current study demonstrates the capability of Rg3, another ginsenoside present in RGE, to inhibit stem-like breast cancer cells. Notably, Rg3 can modulate the manifestation of cancer stem cell–like features by suppressing the Akt-mediated self-renewal activity.
Recent studies have revealed the central role of self-renewal signaling involved in the maintenance of the cancer stem cell–like phenotype [6], [49]. Among the stem cell–associated factors, Sox-2 and Bmi-1 are of prime interest. Sox-2 plays a crucial role in self-renewal activity mediated by epidermal growth factor–receptor in pancreatic CSCs, and its ectopic overexpression enhances the proportion of breast CSCs by activating the Wnt signaling pathway [7], [50]. Moreover, Sox-2 overexpression induces the expression of other self-renewal markers, NANOG and OCT4, in melanoma-initiating cells [31]. Furthermore, several reports have proposed targeting self-renewal regulator, Bmi-1as Achilles's heel of CSCs [8], [51]. Kreso et al [52] demonstrated that the immunodeficient mice transplanted with Bmi-1 knockdown human colorectal cancer cells showed the reduced tumor growth as compared to those harboring the functional Bmi gene. Bmi-1 also regulated the cellular senescence in hematopoietic stem cells and involved in life span extension through inhibition of the p16Ink4a-dependent senescence signaling pathway [53]. In this context, Sox-2 and Bmi-1 are considered the threatening dynamic duo in maintenance of the cancer stem cell–like phenotype.
CSCs reside within specialized tumor microenvironment where they remain in a quiescent state and go through different metabolic pathways [54]. It is noteworthy that there is an intimate relationship between HIFs and the metabolism of CSCs [34], [35]. It has been known that HIF-1α is involved in self-renewal activity and chemoresistance of CSCs. Thus, the activation of HIF-1α that coincides with glycolysis endows CSCs with the optimal metabolic pathway to survive a hypoxic microenvironment [55]. In addition, HIF-1α stimulates increased glycolytic flux through upregulation of transcriptional activity of genes encoding enzymes, such as lactate dehydrogenase A and pyruvate dehydrogenase kinase 1 [56]. Having demonstrated the vital role of hypoxic conditions in CSC metobolism, a few studies have speculated an interesting cross-link between the metabolic and self-renewal pathways of CSCs. Stabilization of HIFs causes a metabolic reprogramming to encode glycolytic enzymes and promote self-renewal [57]. Moreover, Soeda et al [58] reported that CD133-positive cells show the self-renewal activity through upregulation of HIF-1α. The results from our present study demonstrate that HIF-1α modulates Sox-2 and Bmi-1, but its implication in CSC metabolism remains elusive.
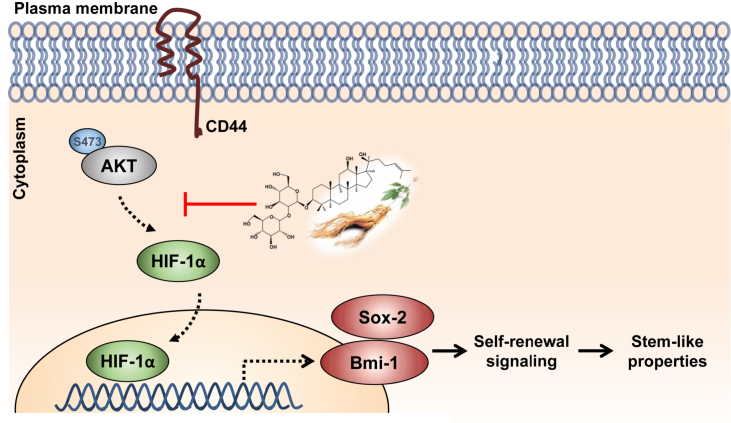
In summary, Rg3 inhibits self-renewal activity of breast stem–like cancer cells by blocking Akt-induced HIF-1α activation and subsequent expression of Bmi-1 and Sox-2 (Fig. 6). Thus, Rg3 acts as a potential agent for purging stemness capacity of breast CSCs. Whether Rg3 has the same effects on the manifestation of stemness properties of other types of CSCs and whether it could be applied for clinical trial at an optial and/or safe concentration need further investigation.
Fig. 6.
Schematic representation of a proposed mechanism underlying the inhibitory effects of Rg3 on self-renewal signaling. Rg3, a major anticancer component of RGE, inhibits the Akt-mediated self-renewal signaling which, in turn, modulates stem-like properties. HIF-1α, hypoxia inducible factor-1α; RGE, red ginseng extract.
Conflicts of interest
All authors have no conflicts of interest to declare.
Acknowledgments
This work was supported by the grant from the Korean Society of Ginseng funded by the Korean Ginseng Corporation (2015–2016).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jgr.2018.05.004.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Torre L.A., Bray F., Siegel R.L., Ferlay J., Lortet-Tieulent J., Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Youlden D.R., Cramb S.M., Yip C.H., Baade P.D. Incidence and mortality of female breast cancer in the Asia-Pacific region. Cancer Biol Med. 2014;11:101–115. doi: 10.7497/j.issn.2095-3941.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ailles L.E., Weissman I.L. Cancer stem cells in solid tumors. Curr Opin Biotechnol. 2007;18:460–466. doi: 10.1016/j.copbio.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Bjerkvig R., Tysnes B.B., Aboody K.S., Najbauer J., Terzis A.J. Opinion: the origin of the cancer stem cell: current controversies and new insights. Nat Rev Cancer. 2005;5:899–904. doi: 10.1038/nrc1740. [DOI] [PubMed] [Google Scholar]
- 5.Klonisch T., Wiechec E., Hombach-Klonisch S., Ande S.R., Wesselborg S., Schulze-Osthoff K., Los M. Cancer stem cell markers in common cancers-therapeutic implications. Trends in Mol Med. 2008;14:450–460. doi: 10.1016/j.molmed.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Deng L., Xu J., Wang D., Liu S. Springer; 2015. Self-renewal pathways in mammary stem cells and carcinogenesis. Cancer stem cells: emerging concepts and future perspectives in translational oncology; pp. 155–174. [Google Scholar]
- 7.Piva M., Domenici G., Iriondo O., Rabano M., Simoes B.M., Comaills V., Barredo I., Lopez-Ruiz J.A., Zabalza I., Kypta R. Sox2 promotes tamoxifen resistance in breast cancer cells. EMBO Mol Med. 2014;6:66–79. doi: 10.1002/emmm.201303411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang M.C., Li C.L., Cui J., Jiao M., Wu T., Jing L., Nan K.J. BMI-1, a promising therapeutic target for human cancer. Oncol Lett. 2015;10:583–588. doi: 10.3892/ol.2015.3361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siddique H.R., Saleem M. Role of BMI1, a stem cell factor, in cancer recurrence and chemoresistance: preclinical and clinical evidences. Stem Cells. 2012;30:372–378. doi: 10.1002/stem.1035. [DOI] [PubMed] [Google Scholar]
- 10.O'Brien C.A., Kreso A., Jamieson C.H. Cancer stem cells and self-renewal. Clin Cancer Res. 2010;16:3113–3120. doi: 10.1158/1078-0432.CCR-09-2824. [DOI] [PubMed] [Google Scholar]
- 11.Liu A.F., Yu X.Y., Liu S.R. Pluripotency transcription factors and cancer stem cells: small genes make a big difference. Chin J Cancer. 2013;32:483–487. doi: 10.5732/cjc.012.10282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hong C.E., Lyu S.Y. Anti-inflammatory and Anti-oxidative effects of Korean red ginseng extract in human keratinocytes. Immune Netw. 2011;11:42–49. doi: 10.4110/in.2011.11.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee S.Y., Kim G.T., Roh S.H., Song J.-S., Kim H.-J., Hong S.-S., Kwon S.W., Park J.H. Proteomic analysis of the anti-cancer effect of 20(S)-ginsenoside Rg3 in human colon cancer cell lines. Biosci Biotechnol Biochem. 2009;73:811–816. doi: 10.1271/bbb.80637. [DOI] [PubMed] [Google Scholar]
- 14.Sumiyoshi M., Sakanaka M., Kimura Y. Effects of red ginseng extract on allergic reactions to food in Balb/c mice. J Ethnopharmacol. 2010;132:206–212. doi: 10.1016/j.jep.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 15.Vuksan V., Sung M.K., Sievenpiper J.L., Stavro P.M., Jenkins A.L., Di Buono M., Lee K.S., Leiter L.A., Nam K.Y., Arnason J.T. Korean red ginseng (Panax ginseng) improves glucose and insulin regulation in well-controlled, type 2 diabetes: results of a randomized, double-blind, placebo-controlled study of efficacy and safety. Nutr Metab Cardiovasc Dis. 2008;18:46–56. doi: 10.1016/j.numecd.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 16.Kim W.Y., Kim J.M., Han S.B., Lee S.K., Kim N.D., Park M.K., Kim C.K., Park J.H. Steaming of ginseng at high temperature enhances biological activity. J Nat Prod. 2000;63:1702–1704. doi: 10.1021/np990152b. [DOI] [PubMed] [Google Scholar]
- 17.Lee S.M., Bae B.S., Park H.W., Ahn N.G., Cho B.G., Cho Y.L., Kwak Y.S. Characterization of Korean red ginseng (Panax ginseng Meyer): history, preparation method, and chemical composition. J Ginseng Res. 2015;39:384–391. doi: 10.1016/j.jgr.2015.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dong H., Bai L.P., Wong V.K.W., Zhou H., Wang J.R., Liu Y., Jiang Z.H., Liu L. The in vitro structure-related anti-cancer activity of ginsenosides and their derivatives. Molecules. 2011;16:10619–10630. doi: 10.3390/molecules161210619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.He B.C., Gao J.L., Luo X., Luo J., Shen J., Wang L., Zhou Q., Wang Y.-T., Luu H.H., Haydon R.C. Ginsenoside Rg3 inhibits colorectal tumor growth through the down-regulation of Wnt/β-catenin signaling. Int J Oncol. 2011;38:437–445. doi: 10.3892/ijo.2010.858. [DOI] [PubMed] [Google Scholar]
- 20.Qiu X.M., Bai X., Jiang H.F., He P., Wang J.H. 20(S)-Ginsenoside Rg3 induces apoptotic cell death in human leukemic U937 and HL-60 cells through PI3K/Akt pathways. Anti-cancer Drugs. 2014;25:1072–1080. doi: 10.1097/CAD.0000000000000147. [DOI] [PubMed] [Google Scholar]
- 21.Kim D.H., Kim J.H., Kim E.H., Na H.K., Cha Y.N., Chung J.H., Surh Y.J. 15-Deoxy-Δ12,14-prostaglandin J2 upregulates the expression of heme oxygenase-1 and subsequently matrix metalloproteinase-1 in human breast cancer cells: possible roles of iron and ROS. Carcinogenesis. 2009;30:645–654. doi: 10.1093/carcin/bgp012. [DOI] [PubMed] [Google Scholar]
- 22.Cicalese A., Bonizzi G., Pasi C.E., Faretta M., Ronzoni S., Giulini B., Brisken C., Minucc S., Di Fiore P.P., Pelicci P.G. The tumor suppressor p53 regulates polarity of self-renewing divisions in mammary stem cells. Cell. 2009;138:1083–1095. doi: 10.1016/j.cell.2009.06.048. [DOI] [PubMed] [Google Scholar]
- 23.Ginestier C., Hur M.H., Charafe-Jauffret E., Monville F., Dutcher J., Brown M., Jacquemier J., Viens P., Kleer C.G., Liu S. ALDH1 is a marker of normal and malignant human mammary stem cells and a predictor of poor clinical outcome. Cell Stem Cell. 2007;1:555–567. doi: 10.1016/j.stem.2007.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim B.M., Kim D.H., Park J.H., Na H.K., Surh Y.J. Ginsenoside Rg3 induces apoptosis of human breast cancer (MDA-MB-231) cells. J Cancer Prev. 2013;18:177–185. doi: 10.15430/JCP.2013.18.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang R., Lv Q., Meng W., Tan Q., Zhang S., Mo X., Yang X. Comparison of mammosphere formation from breast cancer cell lines and primary breast tumors. J Thorac Dis. 2014;6:829–837. doi: 10.3978/j.issn.2072-1439.2014.03.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim D.H., Surh Y.J. Chemopreventive and therapeutic potential of phytochemicals targeting cancer ctem cells. Curr Pharm Rep. 2015;1:302–311. [Google Scholar]
- 27.Lee H.J., Kim J.S., Song M.S., Seo H.S., Moon C., Kim J.C., Jo S.K., Jang J.S., Kim S.H. Photoprotective effect of red ginseng against ultraviolet radiation-induced chronic skin damage in the hairless mouse. Phytother Res. 2009;23:399–403. doi: 10.1002/ptr.2640. [DOI] [PubMed] [Google Scholar]
- 28.Tian L., Shen D., Li X., Shan X., Wang X., Yan Q., Liu J. Ginsenoside Rg3 inhibits epithelial-mesenchymal transition (EMT) and invasion of lung cancer by down-regulating FUT4. Oncotarget. 2016;7:1619–1632. doi: 10.18632/oncotarget.6451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu S., Dontu G., Mantle I.D., Patel S., Ahn N.S., Jackson K.W., Suri P., Wicha M.S. Hedgehog signaling and Bmi-1 regulate self-renewal of normal and malignant human mammary stem cells. Cancer Res. 2006;66:6063–6071. doi: 10.1158/0008-5472.CAN-06-0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park I.K., Qian D.L., Kiel M., Becker M.W., Pihalja M., Weissman I.L., Morrison S.J., Clarke M.F. Bmi-1 is required for maintenance of adult self-renewing haematopoietic stem cells. Nature. 2003;423:302–305. doi: 10.1038/nature01587. [DOI] [PubMed] [Google Scholar]
- 31.Santini R., Pietrobono S., Pandolfi S., Montagnani V., D'Amico M., Penachioni J.Y., Vinci M.C., Borgognoni L., Stecca B. SOX2 regulates self-renewal and tumorigenicity of human melanoma-initiating cells. Oncogene. 2014;33:4697–4708. doi: 10.1038/onc.2014.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xia P., Xu X.Y. PI3K/Akt/mTOR signaling pathway in cancer stem cells: from basic research to clinical application. Am J Cancer Res. 2015;5:1602–1609. [PMC free article] [PubMed] [Google Scholar]
- 33.Mehdizadeh A., Somi M.H., Darabi M., Jabbarpour-Bonyadi M. Extracellular signal-regulated kinase 1 and 2 in cancer therapy: a focus on hepatocellular carcinoma. Mol Biol Rep. 2016;43:107–116. doi: 10.1007/s11033-016-3943-9. [DOI] [PubMed] [Google Scholar]
- 34.Heddleston J.M., Li Z., Lathia J.D., Bao S., Hjelmeland A.B., Rich J.N. Hypoxia inducible factors in cancer stem cells. Br J Cancer. 2010;102:789–795. doi: 10.1038/sj.bjc.6605551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Keith B., Simon M.C. Hypoxia-inducible factors, stem cells, and cancer. Cell. 2007;129:465–472. doi: 10.1016/j.cell.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu W., Shen S.M., Zhao X.Y., Chen G.Q. Targeted genes and interacting proteins of hypoxia inducible factor-1. Int J Biochem Mol Biol. 2012;3:165–178. [PMC free article] [PubMed] [Google Scholar]
- 37.Vidal S.J., Rodriguez-Bravo V., Galsky M., Cordon-Cardo C., Domingo-Domenech J. Targeting cancer stem cells to suppress acquired chemotherapy resistance. Oncogene. 2014;33:4451–4463. doi: 10.1038/onc.2013.411. [DOI] [PubMed] [Google Scholar]
- 38.Horwitz S. Taxol (paclitaxel): mechanisms of action. Ann Oncol. 1993;5:S3–S6. [PubMed] [Google Scholar]
- 39.Tommasi S., Mangia A., Lacalamita R., Bellizzi A., Fedele V., Chiriatti A., Thomssen C., Kendzierski N., Latorre A., Lorusso V. Cytoskeleton and paclitaxel sensitivity in breast cancer: the role of beta-tubulins. Int J Cancer. 2007;120:2078–2085. doi: 10.1002/ijc.22557. [DOI] [PubMed] [Google Scholar]
- 40.Samanta D., Gilkes D.M., Chaturvedi P., Xiang L., Semenza G.L. Hypoxia-inducible factors are required for chemotherapy resistance of breast cancer stem cells. Proc Natl Acad Sci USA. 2014;111:E5429–E5438. doi: 10.1073/pnas.1421438111. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 41.Nag S.A., Qin J.J., Wang W., Wang M.H., Wang H., Zhang R. Ginsenosides as anticancer agents: in vitro and in vivo activities, structure-activity relationships, and molecular mechanisms of action. Front Pharmacol. 2012;3:25. doi: 10.3389/fphar.2012.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu T., Zhao L., Hou H., Ding L., Chen W., Li X. Ginsenoside 20(S)-Rg3 suppresses ovarian cancer migration via hypoxia-inducible factor 1 alpha and nuclear factor-kappa B signals. Tumour Biol. 2017:39. doi: 10.1177/1010428317692225. [DOI] [PubMed] [Google Scholar]
- 43.Kim S.M., Lee S.Y., Cho J.S., Son S.M., Choi S.S., Yun Y.P., Yoo H.S., Yoon D.Y., Oh K.W., Han S.B. Combination of ginsenoside Rg3 with docetaxel enhances the susceptibility of prostate cancer cells via inhibition of NF-κB. Eur J Pharmacol. 2010;631:1–9. doi: 10.1016/j.ejphar.2009.12.018. [DOI] [PubMed] [Google Scholar]
- 44.Kim S.M., Lee S.Y., Yuk D.Y., Moon D.C., Choi S.S., Kim Y., Han S.B., Oh K.W., Hong J.T. Inhibition of NF-kappaB by ginsenoside Rg3 enhances the susceptibility of colon cancer cells to docetaxel. Arch Pharm Res. 2009;32:755–765. doi: 10.1007/s12272-009-1515-4. [DOI] [PubMed] [Google Scholar]
- 45.Lee Y.J., Lee S., Ho J.N., Byun S.-S., Hong S.K., Lee S.E., Lee E. Synergistic antitumor effect of ginsenoside Rg3 and cisplatin in cisplatin-resistant bladder tumor cell line. Oncol Rep. 2014;32:1803–1808. doi: 10.3892/or.2014.3452. [DOI] [PubMed] [Google Scholar]
- 46.Chung S.S., Vadgama J.V. Curcumin and epigallocatechin gallate inhibit the cancer stem cell phenotype via down-regulation of STAT3-NF-κB signaling. Anticancer Res. 2015;35:39–46. [PMC free article] [PubMed] [Google Scholar]
- 47.Fan P.H., Fan S.J., Wang H., Mao J., Shi Y., Ibrahim M.M., Ma W., Yu X.T., Hou Z.H., Wang B. Genistein decreases the breast cancer stem-like cell population through Hedgehog pathway. Stem Cell Res Ther. 2013;4:1. doi: 10.1186/scrt357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu S., Chen M., Li P., Wu Y., Chang C., Qiu Y., Cao L., Liu Z., Jia C. Ginsenoside Rh2 inhibits cancer stem-like cells in skin squamous cell carcinoma. Cell Physiol Biochem. 2015;36:499–508. doi: 10.1159/000430115. [DOI] [PubMed] [Google Scholar]
- 49.Borah A., Raveendran S., Rochani A., Maekawa T., Kumar D.S. Targeting self-renewal pathways in cancer stem cells: clinical implications for cancer therapy. Oncogenesis. 2015;4:e177. doi: 10.1038/oncsis.2015.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rybak A.P., Tang D. SOX2 plays a critical role in EGFR-mediated self-renewal of human prostate cancer stem-like cells. Cell Signal. 2013;25:2734–2742. doi: 10.1016/j.cellsig.2013.08.041. [DOI] [PubMed] [Google Scholar]
- 51.Wicha M.S. Targeting self-renewal, an Achilles' heel of cancer stem cells. Nat Med. 2014;20:14–15. doi: 10.1038/nm.3434. [DOI] [PubMed] [Google Scholar]
- 52.Kreso A., van Galen P., Pedley N.M., Lima-Fernandes E., Frelin C., Davis T., Cao L.X., Baiazitov R., Du W., Sydorenko N. Self-renewal as a therapeutic target in human colorectal cancer. Nat Med. 2014;20:29–36. doi: 10.1038/nm.3418. [DOI] [PubMed] [Google Scholar]
- 53.Park I.K., Morrison S.J., Clarke M.F. Bmi1, stem cells, and senescence regulation. J Clin Investig. 2004;113:175–179. doi: 10.1172/JCI20800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Suda T., Takubo K., Semenza G.L. Metabolic regulation of hematopoietic stem cells in the hypoxic niche. Cell Stem Cell. 2011;9:298–310. doi: 10.1016/j.stem.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 55.Ito K., Suda T. Metabolic requirements for the maintenance of self-renewing stem cells. Nat Rev Mol Cell Biol. 2014;15:243–256. doi: 10.1038/nrm3772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim J.W., Tchernyshyov I., Semenza G.L., Dang C.V. HIF-1-mediated expression of pyruvate dehydrogenase kinase: a metabolic switch required for cellular adaptation to hypoxia. Cell Metab. 2006;3:177–185. doi: 10.1016/j.cmet.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 57.Philip B., Ito K., Moreno-Sanchez R., Ralph S.J. HIF expression and the role of hypoxic microenvironments within primary tumours as protective sites driving cancer stem cell renewal and metastatic progression. Carcinogenesis. 2013;34:1699–1707. doi: 10.1093/carcin/bgt209. [DOI] [PubMed] [Google Scholar]
- 58.Soeda A., Park M., Lee D., Mintz A., Androutsellis-Theotokis A., McKay R., Engh J., Iwama T., Kunisada T., Kassam A. Hypoxia promotes expansion of the CD133-positive glioma stem cells through activation of HIF-1α. Oncogene. 2009;28:3949–3959. doi: 10.1038/onc.2009.252. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.