Abstract
Introduction:
The treatment of distal femur fractures in geriatric patients is challenging and has a high perioperative morbidity and mortality. Treatments have evolved significantly in the past decades. The aim of our study was to analyze local and systemic morbidity and mortality, as well as functional results in this frail cohort treated with distal femur locking plates.
Materials and methods:
In this single-institution case series, we retrospectively analyzed the data of patients aged 65 years and older with fractures of the distal femur between March 2013 and March 2018. All patients were operated with distal femur locking plates. Points of interest included perioperative morbidity, mortality, weight-bearing status, and care-dependency after hospital discharge.
Results:
We assessed 49 patients (median age: 86.5 years) with 52 distal femur fractures (AO type A 77%, type C 15%, type B 8%). A total of 30 (58%) periprosthetic fractures with 4 (8%) interimplant femur fractures were documented. The perioperative morbidity was 64%, and the 3-month and 1-year mortality rates were 29% and 35%, respectively. The local complication rate was 6% with no documented implant failure. Of the patients who were living at home before the surgery, 62% required long-term accommodation in residential or nursing homes after dicharge from the hospital or short-term rehabilitation.
Conclusions:
Geriatric patients with distal femur fractures face a high perioperative mortality. Osteosynthesis with distal femur locking plates is a reliable technique that can be used in various fracture patterns including periprosthetic and interimplant fractures.
Keywords: distal femur fractures, frailty, geriatric trauma, locking-plate, VA-LCP, LISS, weight-bearing
Introduction
Fractures of the distal femur account for approximately 0.4% of all human fractures and 3% to 6% of all femoral fractures.1 While these fractures mainly occur due to high-velocity accidents in young patients, low-energy trauma from ground-level falls can cause similar fracture patterns in the elderly population.2,3 The treatment of geriatic patients can be especially challenging due to poor bone quality, preexisting implants (eg, knee or hip arthroplasty), and impaired compliance during rehabilitation in mentally and physically restricted patients. Perioperative complication and mortality rates of distal femur fractures are similar to fractures of the proximal femur but have not been assessed as thoroughly. Patients with distal femur fractures aged 80 years or older face high mortality rates of up to 33% after 12 months and 50% after 5 years.4,5 The treatment options have evolved over the past decades due to a better understanding of fracture patterns and biology, as well as the development of biomechanically improved implants.6 In the 1960s, closed treatment with traction was found to have more satisfactory results compared with patients treated with osteosyntheses.7 In 1974, Schatzker et al8 shared their “Toronto experience” demonstrating good results for internal fixation in 75% of the cases, compared to 32% for nonoperative treatment with an ischial cast, concluding that operative treatment posed a valid therapeutic option. Nonetheless, in 1995, Karpman et al9 described an above-knee amputation being necessary in 9% of patients with distal femur fractures and osteoporotic bone due to displacement of fractures or infections, proposing primary amputation as a treatment option in selected patients.
With the introduction of angular stable implants, the options for operative treatment have greatly increased.7 Various implants and techniques for internal fixation of distal femur fractures are available including intramedullary nailing with different distal locking features, lateral locking plates, and primary distal femoral arthroplasty. Since 2013, all patients admitted to our clinic with distal femur fractures have been treated with distal femur locking plates. The aim of this analysis was to assess the mortality, local, and systemic morbidity as well as functional results in geriatric patients having a distal femur fracture.
Materials and methods
In this single-institution cohort study, we retrospectively included all patients 65 years and older which had been operated due to a fracture of the distal femur (AO/OTA 3310) between March 2013 and March 2018. Data were collected by chart review through one author (A.L.), who was not involved in the operative treatment of the cohort. Patients’ demographics, residency before and after hospitalization, prior prosthetic implants, implant details, cement augmentation, Barthel Index,11 ASA Score (American Society of Anesthesiologists Physical Status Classification System12), perioperative local and systemic morbidity, mortality, postoperative, and definitive weight-bearing status were assessed for all patients. Additional information regarding pain and mobilization at time of analysis was gathered from the patients or their nursing facilities. The dates of death were drawn from the local population registry. For patients who had died prior to the point of analysis the last documented residental status was used; level of pain or mobilization were not evaluated. Written consent was obtained when feasible in accordance with the local ethics committee.
Results
Included were 49 patients (median age 86.5 years [65-99], 44 female [90%]) with 52 distal femur fractures. Two patients had bilateral synchronous fractures and one patient had a contralateral fracture 14 weeks after the first fracture. In total 50 in-hospital treatments for distal femur fractures were analyzed. The vast majority of fractures were type A (77% [40/52]) followed by type C (15% [8/52]) and type B (8% [4/52]) injuries according to the OTA-classification.10 There were no open fractures in our study group. In one patient, simultaneous bilateral femur fractures were primarily stabilized with 2 external fixators on the day of the trauma with definitive osteosynthesis 6 and 9 days after the trauma. Otherwise all patients were treated within 48 hours post-traumatically with primary lateral femur plate osteosynthesis. In 58% (30/52) of the affected femurs at least 1 prior osteoprosthetic implant of the proximal (n = 20/52) or distal femur (n = 10/52) was in place. In 13% (7/52) of cases more than 1 implant was present and 8% (4/52) had a so-called interimplant fracture (Table 1; Figure 1). A total of 52 plates were implanted. The implants used were the LISS-plate (Less Invasive Stabilization System, DePuy Synthes, Zuchwil, Switzerland; 83%, 43/52) until April 2017 and thereafter the VA-LCP (Variable Angle—Locking Compression Plate, DePuy Synthes; 17%, 9/52). Cerclage wiring as an adjunct was used in 55% (29/52) to optimize the reduction. In 21% (11/52), bone augmentation with cement was performed due to osteopenia (Figure 2).
Table 1.
Fracture and Treatment Characteristics.
| N Femurs (Total = 52) | In % | ||
|---|---|---|---|
| Preexisting implants/osteosyntheses | THA/HA | 16 | 31 |
| TKA | 10 | 19 | |
| PFN/LFN | 7 | 13 | |
| Other | 4 | 8 | |
| >1 implant | 7 | 13 | |
| Interprosthetic | 4 | 8 | |
| Total | 30 | 58 | |
| Fracture classification OTA 33 | A | 40 | 77 |
| B | 4 | 8 | |
| C | 8 | 15 | |
| Plates used | LISS | 43 | 83 |
| VA-LCP | 9 | 17 | |
| N cases (total = 50) |
In % | ||
| Postoperative weight-bearing | No (wheelchair) | 28 | 56 |
| Partial | 19 (23a) | 38 (46a) | |
| Full | 3 | 6 | |
| N patients (total = 20) |
In % | ||
| Mobilizationb | No (Wheelchair) | 7 | 35 |
| Wheeled walker | 5 | 25 | |
| Cane | 3 | 15 | |
| No aid | 5 | 25 | |
| Persistent painb | Yes | 4 | 20 |
| No | 16 | 80 | |
Abbreviations: HA, hemiarthroplasty; LFN, lateral femoral nail; PFN, proximal femoral nail; THA, total hip arthroplasty, TKA, total knee arthroplasty.
aFour patients were not able to perform partial weight-bearing and were therefore restricted to no weight-bearing and analyzed as no weight-bearing.
bMedian 25 months postoperatively (5-55 months).
Figure 1.
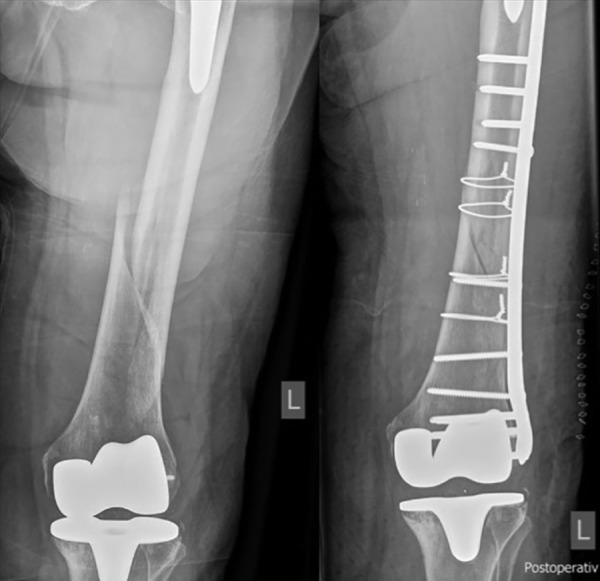
Interimplant fracture pre- and postoperative, LISS plate.
Figure 2.

Pre- and postoperative, cement augmentation, VALCP.
After surgery, weight-bearing restrictions were defined by each surgeon individually depending on bone quality, expected stability of the osteosynthesis as well as the patients’ cognitive and physical abilities and their comorbidities: 48% (24/50) of the patients were restricted to no weight-bearing (wheelchair) for 6 to 8 weeks, while 46% (23/50) were allowed partial and 6% (3/50) immediate full weight-bearing. Four patients were physically unable to perform partial weight-bearing and were therefore restricted to no weight-bearing and included in the wheelchair group for analysis (Table 1).
The ASA Score was documented for all patients; 80% (40/50) of the patients were graded ASA III or IV (Table 2). The preoperative Barthel Index was available in 26 cases (52%) with a mean score of 73 (25-100).
Table 2.
Perioperative Morbidity and Mortality
| N Cases (Total = 50) | In % | |
|---|---|---|
| ASA | ||
| I | 0 | 0 |
| II | 10 | 20 |
| III | 33 | 66 |
| IV | 7 | 14 |
| Morbidity | ||
| Systemic | ||
| Anemia (Hb < 80 g/L) | 25 | 50 |
| Delirium | 8 | 16 |
| Urinary tract infection | 7 | 14 |
| Cardial decompensation | 6 | 12 |
| Pneumonia | 4 | 8 |
| Decubital ulcer | 2 | 4 |
| Acute kidney failure | 1 | 2 |
| Local | ||
| Impaired wound healing | 2 | 4 |
| Reoperation | 1 | 2 |
| Total of patients with ≥1 morbidity | 32 | 64 |
| Mortality | ||
| All | N patients (total = 49) | In % |
| In hospital | 4 | 8 |
| 1 month | 6 | 12 |
| 3 months | 14 | 29 |
| 1 year | 17 | 35 |
| ≤85 years | N patients (total = 18) | In % |
| In hospital | 0 | 0 |
| 1 month | 0 | 0 |
| 3 months | 1 | 6 |
| 1 year | 2 | 11 |
| >85 years | N patients (total = 31) | In % |
| In hospital | 4 | 13 |
| 1 month | 6 | 19 |
| 3 months | 13 | 42 |
| 1 year | 15 | 48 |
Overall postoperative morbidity was high with 64% (32/50) of patients who had at least 1 adverse event. Postoperative anemia, defined as hemoglobin levels lower than 80 g/L, occurred in 50% of all patients, accounting for the most common complication (Table 2). The local complication rate was low: 2 (4%) cases of impaired wound-healing were noted and there were no documented implant failures or surgical site infections. One interimplant fracture occurred in a patient 5 weeks after osteosynthesis with a 9-hole-LISS-plate between the plate and a total hip arthroplasty (resulting in a periprosthetic Vancouver C fracture) and was treated with a 13-hole LISS-plate after removal of the previous plate (Figure 3).
Figure 3.
Osteosynthesis with 9-hole LISS plate and cement augmentation. Interimplantary fracture 5 weeks postoperatively. Revision osteosynthesis with 13-hole LISS plate.
Perioperative mortality was high with 4 (8%) cases of in-hospital fatalities and a 1-month mortality of 12% (6/50). At the time of analysis, 27 (55%, 27/49) patients had died. The 3-month and 1-year mortality rate was 29% (14/49) and 35% (17/49), respectively. When looking at the patients aged 65 to 85 years, the 1-year mortality was 11% (2/18) compared to 48% (15/31) in the group of patients older than 85 years (Table 2).
We were able to assess the residental status for 47 patients. All patients received either short-term rehabilitation or immediate placements in nursing homes after the hospitalization. Prior to the injury, 62% (29/47) of the patients lived independently in their own home. Only 34% (10/29) of these patients were able to return to their domestic environment while 62% (18/29) required long-term accomondation in residental or nursing homes after dicharge from the hospital or short-term rehabilitation (Table 3). Data regarding postoperative pain and mobility at the time of analysis were gathered from the patients directly or via the respective nursing facilities through telephone interviews and was available for 20 patients (mean follow-up of 25 months [5-55]). Of these patients, 20% (4/20) had persistent pain in the affected leg, 35% (7/20) required a wheelchair for mobilization, 25% (5/20) used a wheeled walker, and 15% (3/20) were using one cane. Only 5 (25%) of these patients were ambulating without any walking aid.
Table 3.
Housing Situation Before and After Surgery
| Before | |||
|---|---|---|---|
| After | Home (n = 29) | RH (n = 11) | NH (n = 7) |
| Home (n = 10) | 34% (10/29) | ||
| RH (n = 10) | 7% (2/29) | 73% (8/11) | |
| NH (n = 23) | 48% (14/29) | 18% (2/11) | 100% (7/7) |
| In-hospital mortality | 10% (3/29) | 9% (1/11) | |
Abbreviations: NH, nursing home; RH, residential home.
Discussion
The results of our study show that geriatric patients with fractures of the distal femur face a high morbidity and mortality. In our cohort, the mortality after 1 month, 3 months, and 1 year was 12%, 29%, and 35%, respectively. The mean age of the assessed cohort was 86.5 years which might explain the comparably high-mortality rate when looking at data of other studies where the 1-year mortality was found to be 18% to 25%.5,13,14,15 In a subgroup analysis, patients older than 85 years appeared to be especially at risk, with a 1-year mortality of 50% compared to 8% in the younger patients (aged 65-85 years; Table 2). The findings of Ruder et al15 show similar numbers: The 1-year mortality of patients with periprosthetic distal femur fractures aged older than 85 years was 27.7% and therefore significantly higher when compared to patients below the age of 85 where it was 17.7%.15 There were few local complications with only 2 cases of impaired wound healing (4%) and no documented implant failures in our study group. However, there was one interimplant fracture 5 weeks after primary osteosynthesis with a 9-hole LISS plate. The plate chosen for the osteosynthesis of the initial fracture—with a prior total hip arthroplasty in situ—had most likely been to short16 causing a lot of stress to the bone in between the 2 implants and resulting in a second fracture. The plate was removed and replaced by a longer plate (13 holes; Figure 3). Other authors described rates of implant failures of up to 16% (11/67) with distal femur plating.17 The current literature offers diverging advice ranging from weight-bearing restrictions after surgery for 8 to 12 weeks17-19 to immediate full weight-bearing.13,14 Poole et al13 examined 127 patients treated with locking plate osteosynthesis of distal femur fractures who were all allowed immediate full weight-bearing after surgery and found no increase in implant failure or other adverse events. All of our patients were initially discharged to rehabilitation or nursing facilities. However, only 22% (10/46) of the patients were able to return home after temporary in care, leaving 78% (36/46) of the patients in need for permanent caretaking (Table 3). These numbers match the results of Ruder et al15 who reported 80% of patients being discharged to a skilled nursing facility after treatment of periprosthetic distal femur fractures.
Limitations
This study has several limitations, due to the retrospective data collection and inconsistent follow-up as well as the heterogeneity of the population analyzed (age span of 34 years [65-99 years], heterogenous fracture patterns and the 2 different plates used). Not all patients were seen for regular clinical and radiographic follow-up after discharge due to the underlying comorbidities and the related logistic reasons thus the number of implant failures might be underestimated. However, in the follow-up of 20 patients via phone with a mean of 25 months postoperatively (5-55 months), no implant failures or refractures were documented. Due to the inconsistent follow-up, data evaluating nonunion rates is missing. Information on the patients’ mobility prior to the trauma is missing, and the data of 20 patients are too small to draw any definitive conclusions regarding the impact of postoperative weight-bearing on the long-term mobilization. The postoperative mobilization restrictions were very heterogenously since there was no protocol for the postoperative mobilization of patients and it was up to the surgeon to define the postoperative procedure. Most likely only physically and mentally capable patients were admitted to partial weight-bearing postoperatively causing a selection bias. Furthermore, consistent data on the patients’ mobility preoperatively are missing. To our knowledge, our cohort is the oldest found in recent literature and follow-up was difficult. A prospective design could help eliminate these limitations by implementing standardized questionnaires and follow-ups.
Conclusions
Geriatric patients with fractures of the distal femur are at risk due to high perioperative morbidity and mortality. Osteosynthesis with distal femur locking plates (LISS and VA-LCP) is a safe technique that can be used in various fracture patterns including periprosthetic and interimplant fractures. In our assessed cohort, there was a low local complication rate and no implant failure. Further research is necessary to assess the effect of postoperative weight-bearing restrictions on long-term mobilization.
Footnotes
Authors’ Note: The institutional review board and the local ethical committee approved the study protocol, BASEC-Nr. Req-2018-02013. Informed consent, which included surgical treatment and follow-up examinations, was obtained from each patient. Level III, Therapeutic study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Michael Dietrich, MD  https://orcid.org/0000-0003-2512-3368
https://orcid.org/0000-0003-2512-3368
References
- 1. Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. [DOI] [PubMed] [Google Scholar]
- 2. Singer BR, McLauchlan GJ, Robinson CM, Christie J. Epidemiology of fractures in 15,000 adults: the influence of age and gender. J Bone Joint Surg Br. 1998;80(2):243–248. [DOI] [PubMed] [Google Scholar]
- 3. Arneson TJ, Melton LJ, Lewallen DG, O’Fallon WM. Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965-1984. Clin Orthop Relat Res. 1988;234:188–194. [PubMed] [Google Scholar]
- 4. Ehlinger M, Ducrot G, Adam P, Bonnomet F. Distal femur fractures. Surgical techniques and a review of the literature. Orthop Traumatol Surg Res. 2013;99(3):353–360. [DOI] [PubMed] [Google Scholar]
- 5. Moloney GB, Pan T, Van Eck CF, Patel D, Tarkin I. Geriatric distal femur fracture: are we underestimating the rate of local and systemic complications? Injury. 2016;47(8):1732–1736. [DOI] [PubMed] [Google Scholar]
- 6. Gangavalli AK, Nwachuku CO. Management of distal femur fractures in adults. An overview of options. Orthop Clin North Am. 2016;47(1):85–96. [DOI] [PubMed] [Google Scholar]
- 7. Henderson CE, Kuhl LL, Fitzpatrick DC, Marsh JL. Locking plates for distal femur fractures: is there a problem with fracture healing? J Orthop Trauma. 2011;25(suppl 1):S8–S14. [DOI] [PubMed] [Google Scholar]
- 8. Schatzker J, Horne G, Waddell J. The Toronto experience with the supracondylar fracture of the femur, 1966-1972. Injury. 1974;6(2):113–128. [DOI] [PubMed] [Google Scholar]
- 9. Karpman RR, Del Mar NB. Supracondylar femoral fractures in the frail elderly: fractures in need of treatment. Clin Orthop Relat Res. 1995;316:21–24. [PubMed] [Google Scholar]
- 10. Meinberg EG, Agel J, et al. Fracture and Dislocation Compendium – 2018. J Orthop Trauma. 2018;32:1–169. [DOI] [PubMed] [Google Scholar]
- 11. Mahoney FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 12. Meyer S. Grading of Patients for surgical procedures. Anesthesiology. 1941;2:281–284. [Google Scholar]
- 13. Poole WEC, Wilson DGG, Guthrie HC, et al. “Modern” distal femoral locking plates allow safe, early weight-bearing with a high rate of union and low rate of failure. Bone Jt J. 2017;99-B(7):951–957. [DOI] [PubMed] [Google Scholar]
- 14. Smith JRA, Halliday R, Aquilina AL, et al. Distal femoral fractures: the need to review the standard of care. Injury. 2015;46(6):1084–1088. [DOI] [PubMed] [Google Scholar]
- 15. Ruder JA, Hart GP, Kneisl JS, Springer BD, Karunakar MA. Predictors of functional recovery following periprosthetic distal femur fractures. J Arthroplasty. 2017;32(5):1571–1575. [DOI] [PubMed] [Google Scholar]
- 16. Mardian S, Rau D, Schwabe P, Tsitsilonis S, Simon P. Operative therapy of fractures of the distal femur: predictive factors for a complicated course. Orthopade. 2016;45(1):32–37. [DOI] [PubMed] [Google Scholar]
- 17. Tank JC, Schneider PS, Davis E, et al. Early mechanical failures of the synthes variable angle locking distal femur plate. J Orthop Trauma. 2016;30(1):e7–e11. [DOI] [PubMed] [Google Scholar]
- 18. Gwathmey FWJ, Jones-Quaidoo SM, Kahler D, Hurwitz S, Cui Q. Distal femoral fractures: current concepts. J Am Acad Orthop Surg. 2010;18(10):597–607. [DOI] [PubMed] [Google Scholar]
- 19. Chen AF, Choi LE, Colman MW, et al. Primary versus secondary distal femoral arthroplasty for treatment of total knee arthroplasty periprosthetic femur fractures. J Arthroplasty. 2013;28(9):1580–1584. [DOI] [PubMed] [Google Scholar]



