Abstract
In many cases, an intra-arterial microcatheter loop is necessary to bypass the neck of wide-necked giant aneurysms for the placement of a stent across it. The removal of this loop is usually challenging, and many techniques have been described to achieve it. We describe a simple novel technique for straightening the microcatheter across the aneurysm’s neck, without the need for additional products/devices or complex exchanging techniques. The method has been successfully applied in two cases. We named this novel maneuver the “Lagman vacuum” technique.
Keywords: Intracranial aneurysm, therapeutic embolization, endovascular procedures, stents
Introduction
Placement of a stent for the treatment of intracranial aneurysms, for flow diversion or coiling assistance, is nowadays very common. Bypass of wide-necked giant aneurysms for stent placement is often extremely difficult. In many cases direct catheterization of the distal segment of the parent vessel is impossible and navigation through the aneurysm dome may be required. In these cases, the loop of the microcatheter should be straightened before the delivery of the stent. In most of the cases, simple retraction of the catheter results in retrieval of the whole system without release of the loop. Many techniques have been described for this achievement.1–8 We describe a simple novel technique for the microcatheter straightening, naming it the “Lagman vacuum” technique.
Technique
Case 1
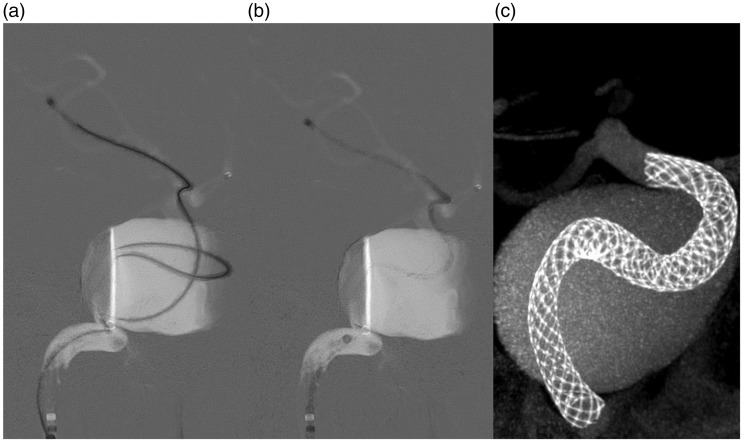
A 63-year-old female with a giant cavernous segment internal carotid artery aneurysm was planned to be treated with a flow diverter (Pipeline Flex, Medtronic, Irvine, CA, USA). After standard access with a long sheath and a distal access catheter and several failed attempts to bypass the aneurysm’s neck, navigation of the microcatheter (Phenom, Medtronic, Irvine, CA, USA) through the aneurysm dome seemed to be the only way to reach the distal normal vasculature. After the successful microcatheter advance in good distance of the aneurysm’s neck, several unsuccessful attempts to straighten the microcatheter by simple retraction were tried, but the distal tip was sliding down instead of the loop straightening. At this point, we applied our novel technique. The microcatheter advanced again until the wall of a distal artery was engaged (Figure 1(a)). The microwire then was totally removed and a 20-ml syringe was applied to the hub of the microcatheter. A slight aspiration was applied using the syringe and the microcatheter pulled back again, this time resulting in catheter straightening (Figure 1(b)). We then pulled back the microcatheter slightly to allow a blood backflow and assure that the tip was away from the wall. The following steps of the procedure were performed according to the standard technique. After stent placement, we performed a high resolution Cone beam CT (Vaso CT, Philips, ND) where the stent follows the microcatheter's route (Figure 1(c)).
Figure 1.
(a) To reach the distal vasculature an intrasaccular loop was necessary. (b) After withdrawal of the microwire and the application of our technique, the withdrawal of the small catheter results in the resolve of the loop. The tip of the microcatheter remains stable during the maneuver without the need of any additional material. (c) High resolution cone beam computed tomography (VasoCT, Philips Healthcare, Best, the Netherlands) shows the pathway of the stent within the aneurysm that follows the course of the microcatheter.
Case 2
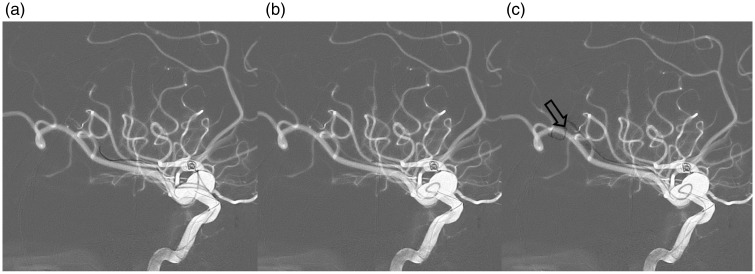
The second patient was a 53-year-old male with a large right middle cerebral artery aneurysm with wide neck that needed stent-assisted coiling. We decided to place a braided stent (leo+baby, Balt, Montmorency, France) using a 0.017-in microcatheter (prowler-14, Codman, Raynham, MA, USA). Again, the navigation for direct distal artery catheterization was impossible and the intrasaccular route was attempted (Figure 2(a)). To release the loop, we first tried to carefully pull back the microcatheter, but every time the distal tip slid down. After some failed attempts, we applied the “Lagman vacuum” technique. The first attempt was unsuccessful, probably due to the discrepancy between the caliber of the microcatheter and the hosting angular artery. The microcatheter was navigated to a smaller posterior parietal artery to a position where the tip was against the artery wall (Figure 2(b)). The technique worked successfully this time and the microcatheter remained across the neck of the aneurysm allowing the deployment of the stent. To ensure that the hosting vessel was not affected by the technique, we injected a small amount of contrast before the loading of the stent (Figure 2(c)).
Figure 2.
(a) After creating a loop, the microcatheter navigated in a small M3-M4 branch of the right middle cerebral artery. The technique did not work when the microcatheter was in the larger angular artery. (b) The loop has been successfully resolved with the “Lagman vacuum” technique, with the microcatheter within the smaller branch. (c) A small contrast amount shows normal flow in the hosting branch.
Discussion
Endovascular treatment of wide-necked large or giant aneurysms, where the parent artery should be preserved, is often challenging. Reconstruction of the parent artery with a stent or flow diversion has enormously increased the number of cases that can be treated endovascularly. In these cases, the so-called bypass of the neck of the aneurysm is needed. However, the navigation of microcatheters to distal normal arteries may be impossible with standard techniques and navigation of the microcatheter through the aneurysm’s dome is necessary. Afterwards, straightening of the microcatheter is needed and several techniques and maneuvers have been developed by various neuro-interventionalists to accomplish this difficult task.1–8
Cekirge et al. were the first to describe a technique to release an intrasaccular catheter loop, by using a balloon.1 In this paper, they described the “balloon-assisted endovascular neck bypass technique,” where a hyperform balloon (ev3, Irvine, CA, USA) was advanced all along the inner wall of the aneurysm until it made a loop to reach its outflow. Then, the balloon was inflated for the stabilization of the whole system and it was pulled back gently to remove the slackened part within the aneurysm sac. After the successful reduction of the loop, an exchange microwire was introduced to replace the balloon catheter with the catheter needed for the stent.
Three years later Snyder et al. described almost the same technique under the name “balloon anchor technique.”2 The steps were identical with the only difference being that the balloon used for anchoring to the distal vessels was the Gateway (Boston Scientific, Fremont, CA, USA).
The “sea anchor technique”3 was based on the same idea, with some type of device utilized to keep the distal part of a catheter stable in order to release the intrasaccular loop. This time the device was an aneurysm coil with a sufficient length (as long as 30 cm) to play the role of an anchor. By keeping the detachment zone of the coil within the microcatheter and locking the pushing wire with the rotating hemostatic valve, the authors managed to extinguish the loop within the sac.
Fargen et al.6 suggested a ‘stent anchor technique’, which utilized the original treatment stent to stabilize the distal part of the looped catheter. Once the loop was removed, the stent was recaptured to place it in the ideal position across the aneurysm’s neck. The major advantage of this technique was that no additional device was necessary. A similar technique, using a different stent on purpose for the loop retraction, was described by Parry et al.,9 where a solitaire stent was used. However, a major disadvantage of both techniques, in our opinion, is that the stent should go all the way around the dome of the aneurysm, increasing the wall stress and consequently the risk of rupture.
Trying to avoid the usage of extra devices and exchange maneuvers, Oran et al.4 described the “rapid pull-back technique” where, after withdrawal of the microguidewire, the microcatheter was pulled back rapidly up to a predetermined length. They claimed that this rapid movement preferentially released the intrasaccular loop instead of retracting the distal part of the catheter, thus helping them to navigate across wide-necked aneurysms. However, they noticed that the technique is successful probably with small-caliber microcatheters and potential risks due to the rapid microcatheter movement may still exist. Moreover, if a larger microcatheter is needed for a stent-assisted coiling or flow diversion, an exchange maneuver will be necessary.
Chapot et al.,5 using their experience that a second microcatheter tends to preferentially follow the same artery as a previously placed one, described the “sheeping technique or how to avoid exchange maneuvers.” As its name implies, they first place a 1.7-F microcatheter by overcurving the distal tip of it, and then the remodeling balloon or the stent microcatheter is advanced in the same division branch. This technique helps the bypass without the need of a loop at the dome; however, it requires a direct bypass, which often is impossible even with a smaller microcatheter.
The latest technique that has been described for the traction of an intra-aneurysmal loop was the “wire anchor loop traction (WALT) maneuver.”7 The authors here tried to avoid any additional material to maximize cost effectiveness and simplicity. In this technique the microwire was withdrawn to a proximal point within the microcatheter, in a parallel direction with the distal exiting branch from the aneurysm. The rest of the technique is a repetition of gentle traction of the microcatheter and wire and repositioning of the wire every time the loop is getting smaller.
Our technique is applied when an intra-aneurysmal microcatheter loop has been created by the operator to bypass the neck of a giant or/and wide-necked aneurysm. In these cases, attempting to straighten the loop by simply withdrawing the catheter frequently results in prolapse of the microcatheter tip out of the distal vessel and into the aneurysm’s dome.6 To achieve this without losing the access, several techniques have been described.1–4,6,7 Most of these techniques described above use a device for anchoring the distal position of the system, so that the pull-back movement results in loop reduction.1–3,6,7 When the device that has been used for the anchoring is not the device intended for the procedure, then an extra exchange maneuver is needed.
Our technique combines simplicity and cost effectiveness since it does not require additional material. It seems effective since it has worked in both cases where we have applied it. The only additional material that is needed is a syringe for a gentle suction to create a negative pressure within the microcatheter. We suppose that a combination of phenomena results in anchoring of the microcatheter. Initially, disconnection of the microcatheter from arterial infusion system results in a drop of pressure that releases the stress at the microcatheter’s body. This might be sufficient to enable the loop retraction. If not, additional suction works like a straw trying to suck blood within. If the microcatheter is in a wedge position, the blood backflow creates a vacuum space and negative pressure beyond the tip that may hold it in position. This is probably the reason the technique did not work in the large angular artery in our second case. Another possible mechanism is that the tip of the microcatheter gently suckles the wall of the vessel, keeping the tip attached to it during retraction of the catheter. This could be more possible when the microcatheter tip is located at a vessel bifurcation or against a wall.
Since the maneuver may pose a source of complications, we suggest the usage of a rather large volume 20-ml syringe and not a smaller one, where the negative pressure might be overwhelming to the vessel’s wall and provoke endothelial damage and intra-arterial thrombosis. The syringe should be semi-filled with normal saline and a gradual vacuum is applied while slowly retrieving the microcatheter. When the tip of the microcatheter looks anchored, the vacuum is stabilized and the retrieval of the microcatheter results in loop reduction. This is usually achieved with a few milliliters pull back of the syringe’s plunger. We also suggest a slight withdrawal of the microcatheter to disengage from the vessel’s wall, after the straightening of the microcatheter. In case blood backflow does not happen automatically, which is more probable with the use of smaller microcatheters like the one we have used for our second case, we suggest the use of a small 1-ml syringe to achieve backflow manually and to be sure that the microcatheter is clear. Injection of a small amount of contrast media to inspect the integrity of the hosting vessel might be a useful precaution.
Another possible source of complication is the intra-aneurysmal loop per se. Compared to direct bypass, this maneuver creates stress to the aneurysm’s wall and this might be a possible reason for a catastrophic rupture. This complication does not occur so often, although it might be under-reported in the literature. Our technique might be superior over other similar maneuvers, since it uses only the microcatheter intended to be used for the stenting without the device within it. Thus, the wall stretching is far less compared with other devices, as for example is the case when a balloon1,2 or a stent6 makes the same loop. Ιn other techniques,3,7 the wall stretching might be comparable; but, as long as another material rather than the catheter intended for the planned treatment is used, an extra exchange maneuver will be needed, yielding a complication rate itself.
Conclusion
The technique we used to align the microcatheter is simple and effective since it was successful in two cases. It does not require the use of additional materials, resulting in cost reduction, and has a low risk of complications since it causes the smallest possible tension in the wall of the aneurysm and does not require material exchange techniques. Although simple, it has not been described so far, to the best of our knowledge, and it would be very convenient for many neuroradiologists facing these types of difficulties to bypass an aneurysm. We named this technique “Lagman vacuum” from the authors’ names in combination and the possible mechanism by which the technique works, which is the anchoring of the microcatheter on the vessel’s wall by creating a vacuum phenomenon at the microcatheter tip by aspiration.
Contributors
Both authors contributed equally to the presented work.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Cekirge SHH, Yavuz K, Geyik S, et al. HyperForm balloon-assisted endovascular neck bypass technique to perform balloon or stent-assisted treatment of cerebral aneurysms. AJNR Am J Neuroradiol 2007; 28: 1388–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Snyder KV, Natarajan SK, Hauck EF, et al. The balloon anchor technique: a novel technique for distal access through a giant aneurysm. J Neurointerv Surg 2010; 2: 363–367. [DOI] [PubMed] [Google Scholar]
- 3.Edwards L, Kota G, Morris PP. The sea anchor technique: a novel method to aid in stent-assisted embolization of giant cerebral aneurysms. J Neurointerv Surg 2013; 5: 1–5. [DOI] [PubMed] [Google Scholar]
- 4.Oran I, Çinar C, Bozkaya H, et al. The rapid pull-back technique for navigation across a wide-necked aneurysm: a report of four cases. Interv Neuroradiol 2013; 19: 16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chapot R, Nordmeyer H, Heddier M, et al. The sheeping technique or how to avoid exchange maneuvers. Neuroradiology 2013; 55: 989–992. [DOI] [PubMed] [Google Scholar]
- 6.Fargen KM, Velat GJ, Lawson MF, et al. The stent anchor technique for distal access through a large or giant aneurysm. J Neurointerv Surg 2013; 5: e24. [DOI] [PubMed] [Google Scholar]
- 7.Effendi K, Sacho RH, Belzile F, et al. The wire anchor loop traction (WALT) maneuver. BMJ Case Rep 2015; 2015: bcr2014011604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kan P, Wakhloo AK, Mokin M, et al. Techniques in distal access of wide-necked giant intracranial aneurysms during treatment with flow diversion. Surg Neurol Int 2015; 6: S284–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parry PV, Morales A, Jankowitz BT. Solitaire salvage: a stent retriever-assisted catheter reduction technical report. J Neurointerv Surg 2016; 8: e27. [DOI] [PubMed] [Google Scholar]