Abstract
Background:
Patient awareness of their chronic kidney disease (CKD) and health literacy (HL) are both important for adherence to therapies that slow CKD progression and to reduce risk of complications. Little is known about the association between HL and CKD awareness.
Objective:
We sought to determine if patient HL is associated with CKD awareness.
Methods:
We conducted a cross-sectional study of general medicine inpatients at an urban academic medical center discharged between June 2011 and July 2013 with CKD, defined as having at least one CKD International Classification of Diseases, ninth revision code (585.0–585.9), among their first 20 admission diagnoses. Logistic regression was used to analyze the influence of HL, demographic, clinical, and health care use covariates on the likelihood of patients' CKD awareness. Our primary outcome was patient awareness of their CKD, defined as correct patient self-report of “kidney problems.” We used the Brief Health Literacy Screen, a three-item verbal questionnaire, to assess HL.
Key Results:
Among 1,308 patients with CKD, awareness of CKD was 33%, and 48% had adequate HL. However, CKD awareness was not associated with HL even among patients with stage 4 or 5 CKD. In multivariable logistic regression, greater awareness was associated with being a woman, younger than age 50 years, married, White, having hypertension, and having a higher CKD stage (all p < .05). In stratified analyses, patients with hypertension had greater CKD awareness, regardless of HL or diabetes status (p < .05).
Conclusions:
Among hospitalized patients with CKD, both CKD awareness and HL are low and inadequate. Surprisingly, patients' knowledge of their CKD diagnosis was not related to patients' HL. Patients with hypertension who young, white, or married may be receiving or retaining more education related to CKD. More work is needed on how to effectively communicate CKD diagnosis to prevent widening health disparities. [Health Literacy Research and Practice. 2017;1(3):e117–e127.]
Plain Language Summary:
We studied whether patients with low health literacy also had low awareness of their chronic kidney disease (CKD). Hospitalized patients with CKD were asked three questions about their health literacy and whether they had “kidney problems.” Overall CKD awareness and health literacy were low, but a low score on one did not predict a low score on the other.
Chronic kidney disease (CKD) affects more than 14.8% of the population in the United States and is associated with increased morbidity, mortality, and health care costs (United States Renal Data System, 2016); however, only 10% of people in the US with CKD are aware of their diagnoses (Tuot et al., 2011). Even among those with CKD stage 5, only 60% of these patients are aware of their CKD (Kurella Tamura et al., 2011; Saunders, Kim, Patel, Meltzer, & Chin, 2015). This gap in patient knowledge may be due to failures of communication, such as lack of physician disclosure or lack of patient understanding (Ferris et al., 2009; Greer, Cooper, Crews, Powe, & Boulware, 2011; Greer, Crews, & Boulware, 2012).
Patient awareness of their CKD diagnosis is important because progression of kidney disease can be slowed by effective patient self-management of comorbid diseases such as diabetes mellitus (DM) and hypertension (HTN), and lifestyle changes such as smoking cessation, maintaining a healthy body mass index, and avoiding nephrotoxic drugs (James, Hemmelgarn, & Tonelli, 2010; Bakris et al., 2000). Patient awareness of CKD may also increase acceptance of pre–end-stage renal disease (ESRD) patient education and nephrology referral, which have also been shown to delay CKD progression and to improve clinical status at initiation of dialysis (Bakris et al., 2000).
One potential mediator of patient awareness of CKD is health literacy (HL), which is “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” (U.S. Department of Health and Human Services, 2010). Low HL is common among CKD patients; anywhere from 9% to 32% of CKD populations have inadequate HL (Cavanaugh et al., 2010; Grubbs, Gregorich, Perez-Stable, & Hsu, 2009; Ricardo et al. 2014). Further, among patients with CKD, low HL is associated with worse blood pressure control, increased use of emergency department services, lower likelihood of transplant referral, and increased mortality (Cavanaugh et al., 2010; Grubbs et al, 2009; Adeseun, Bonney, and Rosas, 2010; Green et al., 2013).
In our prior work, we found that CKD awareness among hospitalized patients was low, and only approximately half of these patients have adequate HL (Saunders et al., 2015; Press, Shapiro, Mayo, Meltzer, & Arora, 2013). To tailor educational interventions to improve CKD awareness, it is important to determine if and how HL is correlated with CKD awareness. If CKD awareness is lower among those with low HL, then efforts can focus on literacy-sensitive CKD education. However, if CKD awareness varies by comorbidity or demographic characteristics, then additional outreach should ensure that effective CKD education occurs in those underserved groups. Therefore, using patient survey and administrative data, we examined whether patient awareness of CKD was associated with HL and other sociodemographic and medical factors.
Methods
Participants and Data
We used data from the University of Chicago Hospitalist Project, an ongoing study of hospitalized patient outcomes (Meltzer et al., 2002). Within 48 hours of hospitalization, all general medicine patients are approached about participating in the study, and more than 80% enroll. During one-on-one inpatient interviews, a trained research assistant obtains demographic, health status, and health care utilization information. The study was approved by the University of Chicago Internal Review Board (IRB#9967).
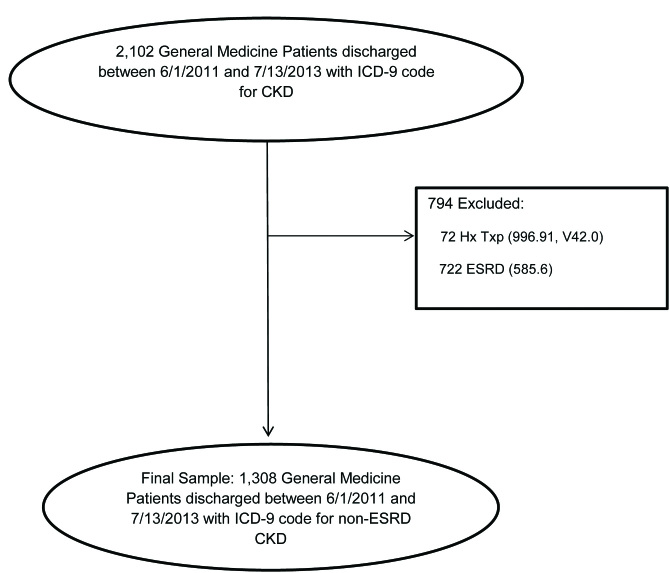
We obtained data on 2,102 general medicine patients discharged between June 1, 2011 and July 13, 2013 with an International Classification of Diseases, ninth revision (World Health Organization, 1979) (ICD-9) code for CKD (ICD-9 codes 585.0 to 585.5, 585.9) in their first 20 admission diagnoses. We excluded all patients with a history of transplant (ICD-9 code 996.81, V42.0; n = 72) or ESRD (ICD-9 code 585.6, n = 722). Our final sample included 1,308 unique patients with an ICD-9 diagnosis of CKD (Figure 1).
Figure 1.
Flow chart of study participants. CKD = chronic kidney disease, ESRD = end-stage renal disease, HX = history, ICD-9 = International Classification of Diseases, ninth revision, TXP = treatment.
Demographic, Health Literacy, Decision-Making, Clinical, and Health Service Utilization Characteristics
Our primary outcome was CKD awareness, (ie, the patient's correct self-report of kidney disease identified when participants selected “kidney problems” from a list of chronic medical conditions). In people with CKD, self-reported kidney problems had greater sensitivity than self-reports for CKD (Wright, Wallston, Elasy, Ikizler, & Cavanaugh, 2011). Demographic characteristics, including age, gender, race/ethnicity, marital status, and education, were also obtained. HL was assessed using the Brief Health Literacy Screen (BHLS), which consists of three questions: (1) “How confident are you filling out medical forms by yourself?” (2) “How often do you have someone help you read hospital materials?” and (3) “How often do you have problems learning about your medical condition because of difficulty understanding written information?” The BHLS is scored on a Likert scale from 0 to 4 (Chew, Bradley, & Boyko, 2004; Chew et al., 2008). Participants had low HL if they had a score of 2 or lower on at least one question.
Health care decision-making variables included patient understanding of the hospital visit, patient preference for provider opinions regarding their health care, and patient preference for leaving health care decisions to the provider. Health care utilization variables included number of visits to a health provider in the past year and prior hospitalization in the past year. Health care utilization has been associated with both HL and patient knowledge of disease (Cho, Lee, Arozullah, & Crittenden, 2008; Finkelstein et al., 2008). DM and HTN were assessed from patient self-report and ICD-9 codes: DM ICD-9 code 250.XX, and HTN ICD-9 codes 401.0, 401.9, 403, 405.09, 405.19, 405.91, 405.99. CKD stage was identified using ICD-9 codes: stage 1, 585.1; stage 2, 585.2; stage 3, 585.3; stage 4, 585.4; stage 5, 585.5; CKD unspecified, 585.9. Our variables were selected from available survey and administrative data using guidance from the literature regarding factors associated with CKD awareness and health literacy (Tuot et al., 2011; Saunders et al., 2015; Cavanaugh et al., 2010; Grubbs et al., 2009; Ricardo et al., 2014; Adesun et al., 2012; Green et al., 2013; Press et al., 2013).
Analysis
Chi-squared tests were used to compare proportions, and t tests were used to compare means. We used bivariable and multivariable logistic regression to analyze the influence of the following variables—demographic: gender, age, race, ethnicity, marital status, and education; HL and decision making: BHLS score, patient understanding of visit, and questions on patient preferences for decision-making; CKD stage and comorbidities: DM and HTN; and health care utilization in the last 12 months: any hospitalizations and the number of visits to a health provider—on the likelihood of patients reporting kidney problems. We conducted sensitivity analyses to see the effect of unspecified CKD stage disaggregated from CKD stage 1 and 2. We also examined only those with advanced CKD (stages 4 and 5) as per guideline recommendations that this group should have been informed of CKD diagnosis and referred to nephrology care (National Kidney Foundation, 2002). Additionally, we created categorical variables and used logistic regression to examine effect modification. All analyses were performed using Stata 14.0 (StatCorp LLC, College Station, TX).
Results
Patient Characteristics and Association with Patient CKD Self-Report
Of the 1,308 patients with ICD-9–coded CKD in our sample (Table 1), the average age was 64 years, 48% were men, 77% were African American, and only 18% were college graduates. Only 33% of patients had correct self-report of their CKD. Patients with CKD awareness were younger and more likely to be married than those without CKD awareness (66 vs. 62 years, and 40% vs. 30%, respectively). In addition, patients with DM, HTN, or CKD stage 4 or 5 were more likely to self-report CKD than those without DM, HTN, or with other CKD stage (DM: 37% vs. 28%, HTN: 44% vs. 12%, and CKD: 57% stage 4, 59% stage 5 vs. 29% stage 1, stage 2, and unspecified; all p < .05). Patients who preferred that their health care provider offer opinions and choices regarding their health care were more aware of their CKD than patients without this preference (40% vs. 24%, p < .05). Although more than half of patients with CKD (52%) had inadequate HL on the BHLS, the proportion was not significantly higher in the group without awareness of CKD.
Table 1.
Patient Characteristics, Overall, and Chronic Kidney Disease Self-Report
| Frequency | Total | Patient Aware of CKD | Patient Not Aware of CKD | p Value |
|---|---|---|---|---|
| Number of patients | 1,308 | 879 | 429 | |
| Female gender | 52% | 65% | 35% | .05 |
| Race | .13 | |||
| African American | 77% | 66% | 34% | |
| White | 16% | 59% | 41% | |
| Othera | 7% | 60% | 40% | |
| Hispanic | 4% | 62% | 38% | .38 |
| Mean age, year (SD) | 64.4 (17.3) | 65.8 (17.2) | 61.5 (17.2) | < .001 |
| Education | .99 | |||
| Less than high school | 23% | 61% | 39% | |
| High school graduate/some college | 56% | 61% | 39% | |
| College graduate or higher | 18% | 62% | 38% | |
| Don't know | 3% | 60% | 40% | |
| Married | 27% | 60% | 40% | .001 |
| Frequency of visits to primary health care provider | .06 | |||
| Once per year or less | 7% | 74% | 26% | |
| 2–3 times per year | 25% | 58% | 42% | |
| 4+ times per year | 69% | 58% | 42% | |
| Diabetes, either self-reported or ICD-9 codedb | 52% | 63% | 37% | < .001 |
| Hypertension, either self-reported or ICD-9 codedc | 66% | 56% | 44% | < .001 |
| CKD stage (ICD-9 coded)d | <. 001 | |||
| 1, 2, and unspecified | 70% | 71% | 29% | |
| 3 | 16% | 70% | 30% | |
| 4 | 11% | 43% | 57% | |
| 5 | 3% | 41% | 59% | |
| Age categories | .002 | |||
| Younger than age 50 years | 19% | 61% | 39% | |
| 50–64 years | 30% | 65% | 35% | |
| 65–79 years | 30% | 67% | 33% | |
| 80+ years | 21% | 76% | 24% | |
| Overall Brief Health Literacy Screen, insufficient | 52% | 62% | 38% | .66 |
| Confidence filling out medical forms (no) | 38% | 65% | 35% | .12 |
| Problems learning about medical condition (yes) | 23% | 63% | 37% | .53 |
| Needs help reading hospital materials (yes) | 35% | 62% | 38% | .98 |
| Patient decision-making | ||||
| Patient understands why he or she is in the hospital (yes) | 95% | 61% | 39% | .63 |
| Patient prefers that the doctor offers choices and asks opinions (yes) | 95% | 60% | 40% | .02 |
| Patient prefers to leave decisions about medical care to doctor (no) | 29% | 57% | 43% | .12 |
Note. CKD = chronic kidney disease. ICD-9 = International Classification of Diseases, 9th ed. SD = standard deviation.
Includes Asian, Pacific Islander/Alaskan Native, mixed race, and unknown/refused.
Diabetes ICD-9 codes 250.0–250.XX.
Hypertension ICD-9 codes 401.0, 401.0, 401.9, 403, 405.09, 405.19, 405.91, 405.99.
CKD ICD-9 codes: CKD Stage 1 585.1, Stage 2 585.2, Stage 3 585.3, Stage 4 585.4, Stage 5 585.5, CKD Unspecified 585.9.
Bivariable and Multivariable Associations with Patient CKD Self-Report
In bivariable analysis (Table 2), women were more likely than men (odds ratio [OR] 1.26, 95% confidence interval [CI] [1.00, 1.59]), married patients were more likely than unmarried patients (OR 1.56, 95% CI [1.21, 2.01]), and patients older than age 80 years were less likely than patients younger than age 50 years (OR 0.51, 95% CI [0.33, 0.71]) to self-report CKD. Patients who preferred that their doctor offer them choices and opinions regarding their health care were more likely to report CKD awareness than those without this preference (OR 2.13, 95% CI [1.13, 4.02]). Advanced CKD was associated with a higher likelihood of CKD awareness (stage 4 OR 3.31, 95% CI [2.31, 4.75]; Stage 5 OR 3.68, 95% CI [1.88, 7.19]). Patients with HTN (OR 5.71, 95% CI [4.16, 7.84]) and patients with DM (OR 1.54, 95% CI [1.22, 1.94]) were more likely to report CKD awareness than those without these conditions. Patients hospitalized in the past 12 months were more likely to report CKD awareness versus those not hospitalized (OR 1.68, 95% CI [1.31, 2.15]). Patients who visited a health care provider more than once a year were more likely to report CKD awareness (2–3 times per year OR: 2.05, 95% CI [1.08, 3.92]; 4+ times per year OR: 2.06, 95% CI [1.12, 3.80]), compared to fewer than once per year (all p < .05). There was no association between patient CKD awareness and HL.
Table 2.
Patient Factors Associated with Patient Chronic Kidney Disease Self-Report
| Factor (N = 1,308) | Bivariable Odds Ratio (95% CI) | Multivariablea Odds Ratio (95% CI) |
|---|---|---|
| Female gender | 1.26* (1, 1.59) | 1.51* (1.07, 2.11) |
| Age | ||
| <50 years | Reference group | Reference group |
| 50–64 years | 0.82 (0.59, 1.14) | 0.58* (0.36, 0.94) |
| 65–79 years | 0.77 (0.55, 1.07) | 0.42** (0.26, 0.69) |
| 80+ years | 0.49*** (0.33, 0.71) | 0.26*** (0.15, 0.45) |
| Race | ||
| African American | Reference group | Reference group |
| White | 1.35 (0.98, 1.85) | 1.71* (1.10, 2.67) |
| Otherb | 1.28 (0.81, 2.03) | 2.01 (0.98, 4.15) |
| Ethnicity (Hispanic is reference group) | 0.77 (0.44, 1.37) | 1.42 (0.58, 3.53) |
| Married | 1.56** (1.21, 2.01) | 1.56* (1.08, 2.24) |
| Education | ||
| Less than high school | Reference group | Reference group |
| High school graduate/some college | 0.99 (0.73, 1.34) | 1.02 (0.68, 1.54) |
| College graduate/higher | 0.95 (0.64, 1.39) | 0.94 (0.56, 1.60) |
| Don't know | 1.05 (0.51, 2.16) | 2.04 (0.80, 5.21) |
| Overall Brief Health Literacy Screen, insufficient | 0.95 (0.74, 1.21) | 1.12 (0.80, 1.56) |
| Patient understands why he or she is in the hospital | 1.16 (0.64, 2.08) | 0.82 (0.35, 1.88) |
| Patient prefers doctor offers choices and asks opinions | 2.13* (1.13, 4.02) | 1.32 (0.60, 2.94) |
| Patient prefers to leave decisions about medical care to doctor | 0.81 (0.62, 1.06) | 0.75 (0.53, 1.08) |
| CKD stage (ICD-9 coded) | ||
| 1, 2, and unspecified | Reference group | Reference group |
| 3 | 1.08 (0.78, 1.50) | 1.14 (0.75, 1.74) |
| 4 | 3.31*** (2.31, 4.75) | 4.65*** (2.74, 7.91) |
| 5 | 3.68*** (1.88, 7.19) | 17.96*** (3.97, 81.31) |
| Diabetes (ICD-9 coded or self-report)c | 1.54*** (1.22, 1.94) | 1.21 (0.87, 1.68) |
| Hypertension (ICD-9 coded or self-report)d | 5.71*** (4.16, 7.84) | 2.73*** (1.74, 4.29) |
| Hospitalized in past 12 months | 1.68*** (1.31, 2.15) | 1.28 (0.93, 1.76) |
| Yearly visits to a health care provider | ||
| Once per year or less | Reference group | Reference group |
| 2–3 times per year | 2.05* (1.08, 3.92) | 1.63 (0.79, 3.38) |
| 4+ times per year | 2.06* (1.12, 3.80) | 1.50 (0.75, 3.01) |
Note: CI = confidence interval; CKD = chronic kidney disease; ICD-9 = International Classification of Diseases, 9th ed.
Multivariable model includes demographic factors (gender, age, race, ethnicity, marital status and education), health literacy questions, CKD stage, diabetes, hypertension, health careuse in past 23 months (hospitalization and number of visits to a health provider).
Includes Asian, Pacific Islander/Alaskan Native, mixed race, and unknown/refused.
Diabetes ICD-9 codes 250.0–250.99.
Hypertension ICD-9 codes 401.0, 401.0, 401.9, 403, 405.09, 405.19, 405.91, 405.99.
p < .05
p < .01.
p < .001.
In multivariable analyses, sex, age, race, marital status, CKD stage, and HTN remained consistently associated with CKD awareness. In the adjusted model, women were more likely to report CKD awareness than men (OR 1.51, 95% CI [1.07, 2.11]). Patients older than age 50 years were less likely to report CKD awareness than patients younger than age 50 years, with the association increasing in magnitude with each increasing age group (age 50–64 years, OR: 0.58, 95% CI [0.36, 0.94]; age 65–79 years, OR: 0.42, 95% CI [0.26, 0.69]; age 80 years or older, OR: 0.26, 95% CI [0.15, 0.45]). Compared to Black patients, White patients were more likely to report CKD awareness (OR 1.71, 95% CI [1.10, 2.67]). Married patients were more likely to report CKD awareness than unmarried patients (OR 1.56, 95% CI [1.08, 2.24]). Patients with HTN had 2.73 greater odds of CKD awareness than those without HTN (95% CI [1.74, 4.29]). Compared to patients with an unspecified or CKD stage 1 or 2, patients with CKD stage 4 and 5 had greater odds of CKD awareness (OR 4.65 and 17.96, respectively; all p < .05). A large proportion of patients (68%) were CKD unspecified by ICD-9 codes. In sensitivity analyses, using unspecified CKD stage as the reference group changed the magnitude of the effect of CKD stage on CKD awareness by less than 2%; removing unspecified CKD stage increased the magnitude of CKD stage. Additionally, there was still no relationship between CKD awareness and HL in sensitivity analyses with unspecified CKD as the reference, with unspecified CKD removed, and with CKD stage 4 or 5 only (Table A).
Table A.
Sensitivity Analyses for Factors Associated with Patient Chronic Kidney Disease Self-Report
| Using CKD Unspecified as Reference (n= 1,308) | Without CKD Unspecified (n = 420) | With Advanced Stage CKD Only (n= 181) | ||||
|---|---|---|---|---|---|---|
| Bivariable odds ratio (95% CI) | Bivariable odds ratio (95% CI) | Bivariable odds ratio (95% CI) | Multivariableaodds ratio (95% CI) | Bivariable odds ratio (95% CI) | Multivariablea odds ratio (95% CI) | |
| Overall brief health literacy screen insufficient | 0.95 (0.74, 1.21) | 1.12 (0.80, 1.56) | 0.99 (0.64, 1.51) | 0.97 (0.52, 1.83) | 1.03 (0.51, 2.10) | 0.51 (0.15, 1.76) |
| CKD stage (ICD-9 coded) | ||||||
| Unspecified | Reference group | Reference group | — | — | — | — |
| 1 and 2 | 1.05 (0.46, 2.45) | 0.89 (0.36, 2.35) | Reference group | Reference group | — | — |
| 3 | 1.08 (0.78, 1.51) | 1.14 (0.75, 1.74) | 1.02 (0.43, 2.47) | 1.38 (0.46, 4.14) | — | — |
| 4 | 3.31* (2.31, 4.76) | 4.63* (2.72, 7.88) | 3.14** (1.29, 7.65) | 5.6*** (1.7, 18) | Reference group | Reference group |
| 5 | 3.68* (1.88,7.21) | 17.9* (3.95, 81.01) | 3.48**(1.21, 10) | 47.3*** (4.55, 92.2) | 1.11 (0.53, 2.31) | 15.8** (1.1, 225.7) |
| Hypertension (ICD-9 coded or self-report)b | 5.71* (4.16, 7.84) | 2.73* (1.73, 4.29) | 7.81* (4.4, 13.9) | 2.13 (0.92, 4.96) | 9.76* (4.3, 22) | 0.98 (0.14, 6.24) |
Note. CI = confidence interval; CKD = chronic kidney disease; ICD-9 = International Classification of Diseases, 9th ed.
Multivariable model includes demographic factors (gender, age, race, ethnicity, marital status, education), health literacy questions, CKD stage, diabetes, hypertension, and health care use (hospitalization and number of visits to a health provider) in past 24 months.
Hypertension ICD-9 codes 401.0, 401.0, 401.9, 403, 405.09, 405.19, 405.91, 405.99 (not all results shown).
p < .001.
p < .05.
p < .01.
Effects of Hypertension Status on Patient CKD Self-Report
In the stratified analysis, patient awareness of CKD was highest in patients with both DM and HTN (Table B). Compared to patients with both DM and HTN, CKD patients without HTN were 85% less likely to report awareness of CKD, regardless of DM diagnosis (with DM, OR: 0.15, 95% CI [0.09, 0.25]; no DM, OR: 0.15, 95% CI [0.10, 0.23]). Similarly, patients with HTN had greater awareness of their CKD, regardless of HL status (Table C). Compared to patients with HTN and inadequate HL (referent), patients without HTN were 53% to 70% less likely to report awareness of CKD regardless of HL status (adequate HL, OR: 0.47, 95% CI [0.29, 0.74]; inadequate HL, OR: 0.30, 95% CI [0.18, 0.49]).
Table B.
Association of Diabetes and Hypertension on Adjusted Odds of Patient Chronic Kidney Disease Self-Report
| Diabetes | Hypertension | ||
| Yes | No | ||
| Yes | Reference group n = 495 (38%) |
0.15* (0.9, 0.25) n = 186 (14%) |
|
| No | 0.73** (0.55, 0.96) n = 368 (28%) |
0.15* (0.1, 0.23) n = 259 (20%) |
|
Note. N = 1,308. Health literacy defined by Brief Health Literacy Screen (Chew et al., 2004).
p < .001
p < .05
Table C.
Association of Health Literacy and Hypertension on Patient Chronic Kidney Disease Self-Report
| Health literacy | Hypertension | ||
| Yes | No | ||
| Low | Reference group n = 426 (40%) |
0.3* (0.18, 0.49) n = 124 (12%) |
|
| High | 0.97 (0.74, 1.28) n = 400 (38%) |
0.47** (0.29, 0.74) n = 111 (10%) |
|
Note. Health literacy defined by the Brief Health Literacy Screen (Chew et al, 2004).
p < .001.
p < .01.
Discussion
To our knowledge, this is the first study examining the association between CKD awareness and HL in an urban, underserved, hospitalized population. We were surprised to find that inadequate HL was not associated with low CKD awareness, even though both CKD awareness and HL are low and inadequate among hospitalized patients with CKD. Many of our hospitalized patients may not have received information about their CKD diagnosis, or CKD information may have been given more consistently or effectively to particular groups, such as patients with HTN, advanced-stage CKD, and those who are White, a woman, or married. Our null results demonstrate that although HL is an important factor for patients obtaining and receiving high-quality care, other factors related to both patients and providers may impact CKD awareness.
Although patients' CKD awareness was low overall (33%), it was higher than the national average, likely due to the larger proportion of hospitalized patients with advanced CKD compared to the general population (Tuot et al., 2011). Our work is consistent with studies that demonstrate increasing CKD awareness with advancing CKD stage (Tuot et al., 2011; Saunders et al., 2015; Plantinga et al., 2008). As CKD advances, patients may be more receptive to messages regarding prevention of CKD progression. In addition, physicians have a greater need to educate patients with advanced stage CKD as planning for renal replacement therapy begins. (National Kidney Foundation, 2002).
Concordant comorbidities (e.g., DM and HTN) have already been associated with improved patient awareness of CKD. (Plantinga et al., 2008). In our stratified analyses, HTN was strongly associated with patient awareness of CKD independent of DM and HL. Although both DM and HTN were associated with greater CKD awareness, the results were less robust for DM after controlling for other factors. Physicians may motivate patients to control their HTN, which is largely silent in its early stages, by relying on fear of known long-term sequelae such as stroke or CKD progression. This linked education may motivate adherence to antihypertensive regimens and lifestyle changes, as well as increase patient awareness of CKD.
Race and marital status were also associated with patient awareness of CKD. White patients were significantly more likely to correctly self-report CKD even after controlling for comorbidity, education, HL, and shared decision-making preferences. Providers may be more likely to discuss CKD with White patients due to an unconscious belief that Whites have a greater interest in their health and better adherence with recommendations (Street, Gordon, & Haidet, 2007). Married patients were also more likely to correctly report CKD. Marriage may provide social support, which enables patients to have greater knowledge of their medical conditions (August & Sorkin, 2010). For example, married patients may listen more carefully to a physician's explanation because they have to explain the results to their spouse. In addition, physicians may provide more detailed explanations to patients when a spouse is present (Schilling et al., 2002).
The generalizability of our findings may be limited due to our study population, which is largely African American patients, a group for whom the link between uncontrolled HTN and kidney disease is more salient (Hebert et al., 1997; Parsa et al., 2013). In addition, ICD-9 coding for CKD case-finding has been shown in prior work to be highly specific but not sensitive (Winkelmayer et al., 2005). (Most of our patients with physician-identified CKD were “CKD unspecified.”) It is unclear whether this large undifferentiated group is due to poor coding, physician under-documentation, or under-recognition of CKD stage. Patients with early-stage CKD may not have been told about their CKD diagnosis. In sensitivity analyses that excluded CKD unspecified and early-stage CKD, our findings were robust; however, there was still no association between HL and CKD awareness even with advanced-stage CKD. An additional limitation is the cross-sectional study design of hospitalized patients. Patients interviewed earlier in their hospital stay may have had worse recall due to distress or delirium. Patients interviewed later in their stay may have introduced selection bias as they were likely sicker with more comorbidities. To reduce bias, patients usually were interviewed within 48 hours of admission and screened for cognitive impairment with a mental status examination. Even with these study limitations, our study significantly contributes to the literature by illuminating areas for improvement of CKD awareness for a high-risk, urban, hospitalized ethnic minority population.
Conclusion
Patients with CKD lack awareness of their diagnosis that cannot be attributed to patients' HL. Providers face challenges in CKD education due to time constraints, competing management demands, and the complexity of CKD management (Greer et al., 2001; Greer et al., 2012; National Kidney Foundation, 2002). Interdisciplinary care models and group education can help ensure patients receive information about their CKD diagnosis and management at multiple points of care and in multiple ways (Nunes, 2013; Narva, Norton, & Boulware, 2016; Strand & Parker, 2012.) However, further work is needed to increase provider motivation and ability to communicate about CKD diagnosis and management to all patients in a way they can understand, retain, and implement. We need to glean why communication about CKD is more effective for patients with HTN, advanced stage CKD, and those who are white, women, or married. Without increased efforts to inform patients of their CKD, there is risk of widening health disparities through systematic provision of lower-quality care.
References
- Adeseun G. A. Bonney C. C. Rosas S. E. (2012). Health literacy associated with blood pressure but not other cardiovascular disease risk factors among dialysis patients. American Journal of Hypertension, 25(3), 348–353. 10.1038/ajh.2011.252 [DOI] [PubMed] [Google Scholar]
- August K. J. Sorkin D. H. (2010) Marital status and gender differences in managing a chronic illness: The function of health-related social control. Social Science and Medicine, 71(10), 1831–1838. 10.1016/j.socscimed.2010.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakris G. L. Williams M. Dworkin L. Elliott W. J. Epstein M. Toto R. Sowers J. (2000) Preserving renal function in adults with hypertension and diabetes: A consensus approach. American Journal of Kidney Disease, 36(3), 646–661. 10.1053/ajkd.2000.16225 [DOI] [PubMed] [Google Scholar]
- Cavanaugh K. L. Wingard R. L. Hakim R. M. Eden S. Shintani A. Wallston K. A. Ikizler T. A. (2010) Low health literacy associates with increased mortality in ESRD. Journal of the American Society of Nephrology, 21(11), 1979–1985. . 10.1681/ASN.2009111163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew L. D. Bradley K. A. Boyko E. J. (2004). Brief questions to identify patients with inadequate health literacy. Family Medicine, 36(8), 588–594. [PubMed] [Google Scholar]
- Chew L. D. Griffin J. M. Partin M. R. Noorbaloochi S. Grill J. P. Snyder A. Vanryn M. (2008). Validation of screening questions for limited health literacy in a large VA outpatient population. Journal of General Internal Medicine, 23(5), 561–566. 10.1007/s11606-008-0520-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho Y. I. Lee S. D. Arozullah A. M. Crittenden K. S. (2008). Effects of health literacy on health status and health service utilization amongst the elderly. Social Science and Medicine, 66(8), 1809–1816. 10.1016/j.socscimed.2008.01.003 [DOI] [PubMed] [Google Scholar]
- Ferris M. Shoham D. A. Pierre-Louis M. Mandhelker L. Detwiler R. K. Kshirsagar A. V. (2009) High prevalence of unlabeled chronic kidney disease among inpatients at a tertiary-care hospital. The American Journal of the Medical Sciences, 337(2), 93–97. 10.1097/MAJ.0b013e318181288e [DOI] [PubMed] [Google Scholar]
- Finkelstein F. O. Story K. Firanek C. Barre P. Takano T. Soroka S. Mendelssohn D. (2008). Perceived knowledge among patients cared for by nephrologists about chronic kidney disease and end-stage renal disease therapies. Kidney International. 74(9), 1178–1184. 10.1038/ki.2008.376 [DOI] [PubMed] [Google Scholar]
- Green J. A. Mor M. K. Shields A. M. Sevick M. A. Arnold R. M. Palevsky P.M. Weisbord S. D. (2013). Associations of health literacy with dialysis adherence and health resource utilization in patients receiving maintenance hemodialysis. American Journal of Kidney Disease, 62(1), 73–80. 10.1053/j.ajkd.2012.12.014 [DOI] [PubMed] [Google Scholar]
- Greer R. C. Cooper L. A. Crews D. C. Powe N. R. Boulware L. E. (2011). Quality of patient-physician discussions about CKD in primary care: A cross-sectional study. American Journal of Kidney Disease, 57(4), 583–591. 10.1053/j.ajkd.2010.08.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greer R. C. Crews D. C. Boulware L. E. (2012). Challenges perceived by primary care providers to educating patients about chronic kidney disease. Journal of Renal Care, 38(4), 174–181. 10.1111/j.1755-6686.2012.00323.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grubbs V. Gregorich S. E. Perez-Stable E. J. Hsu C. Y. (2009) Health literacy and access to kidney transplantation. Clinical Journal of the American Society of Nephrology, 4(1), 195–200. 10.2215/CJN.03290708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebert L. A. Kusek J. W. Greene T. Agodoa L. Y. Jones C. A. Levey A. S. Wang S. R. (1997). Effects of blood pressure control on progressive renal disease in blacks and whites. Modification of Diet in Renal Disease study group. Hypertension, 30(3), 428–435. 10.1161/01.HYP.30.3.428 [DOI] [PubMed] [Google Scholar]
- James M. T. Hemmelgarn B. R. Tonelli M. (2010). Early recognition and prevention of chronic kidney disease. The Lancet, 375(9722), 1296–1309. 10.1016/S0140-6736(09)62004-3 [DOI] [PubMed] [Google Scholar]
- Kurella Tamura M. Anand S. Li S. Chen S. C. Whaley-Connell A. T. Stevens L. A. Norris K. C. (2011). Comparison of CKD awareness in a screening population using the Modification of Diet in Renal Disease (MDRD) study and CKD Epidemiology Collaboration (CKD-EPI) equations. American Journal of Kidney Disease, 57(3), (Suppl. 2), S17–S23. 10.1053/j.ajkd.2010.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer D. Manning W. G. Morrison J. Shah M. N. Jin L. Guth T. Levinson W. (2002). Effects of physician experience on costs and outcomes on an academic general medicine service: Results of a trial of hospitalists. Annals of Internal Medicine, 137(11), 866–874. 10.7326/0003-4819-137-11-200212030-00007 [DOI] [PubMed] [Google Scholar]
- Narva A. S. Norton J. M. Boulware L. E. (2016). Educating patients about CKD: The path of self-management and patient-centered care. Clinical Journal of the American Society of Nephrology, 11(4), 694–703. 10.2215/CJN.07680715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Kidney Foundation. (2002). K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification and stratification. American Journal of Kidney Disease, 39(Suppl. 1), S1–S266. [PubMed] [Google Scholar]
- Nunes J. A. (2013). Education of patients with chronic kidney disease at the interface of primary care providers and nephrologists. Advances in Chronic Kidney Disease, 20(4), 370–378. 10.1053/j.ackd.2013.03.002 [DOI] [PubMed] [Google Scholar]
- Parsa A. Kao W. H. L. Xie D. Astor B. C. Li M. Hsu C-Y. Appel L. J. (2013). APOL1 risk variants, race, and progression of chronic kidney disease. The New England Journal of Medicine, 369(23), 2183–2196. 10.1056/NEJMoa1310345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plantinga L. C. Boulware L. E. Coresh J. Stevens L. A. Miller E. R. 3rd Saran R. Powe N.R. (2008). Patient awareness of chronic kidney disease: Trends and predictors. Archives of Internal Medicine, 168(20), 2268–2275. 10.1001/archinte.168.20.2268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Press V. G. Shapiro M.I. Mayo A. M. Meltzer D. O. Arora V. M. (2013). More than meets the eye: Relationship between low health literacy and poor vision in hospitalized patients. Journal of Health Communication, 18(Suppl. 1), 197–204. 10.1080/10810730.2013.830346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricardo A. C. Yang W. Lora C. M. Gordon E. J. Diamantidis C. J Ford V. Lash J. P. (2014). Limited health literacy is associated with low glomerular filtration in the Chronic Renal Insufficiency Cohort (CRIC) study. Clinical Nephrology, 81(1), 30–37. 10.5414/CN108062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders M. R. Kim S. D. Patel N. Meltzer D. O. Chin M. H. (2015) Hospitalized patients frequently unaware of their chronic kidney disease. Journal of Hospital Medicine, 10(9), 619–622. 10.1002/jhm.2395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilling L. M. Scatena L. Steiner J. F. Albertson G. A. Lin C. T. Cyran L. Anderson R. J. (2002). The third person in the room: Frequency, role, and influence of companions during primary care medical encounters. Journal of Family Practice, 51(8), 685–690. [PubMed] [Google Scholar]
- Strand H. Parker D. (2012). Effects of multidisciplinary models of care for adult pre-dialysis patients with chronic kidney disease: A systematic review. International Journal of Evidence-Based Healthcare, 10, 53–59. 10.1111/j.1744-1609.2012.00253.x [DOI] [PubMed] [Google Scholar]
- Street R. L. Gordon H. Haidet P. (2007). Physicians' communication and perceptions of patients: Is it how they look, how they talk, or is it just the doctor? Social Science and Medicine, 65(3), 586–598. 10.1016/j.socscimed.2007.03.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuot D. S. Plantinga L. C. Hsu C. Y. Jordan R. Burrows N. R. Hedgeman E. Powe N. R. (2011). Chronic kidney disease awareness among individuals with clinical markers of kidney dysfunction. Clinical Journal of the American Society of Nephrology, 6(8), 1838–1844. 10.2215/CJN.00730111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2010). Healthy people 2010: Understanding and improving health (2nd ed.). Retrieved from: http://www.healthypeople.gov/2010/document/pdf/uih/2010uih.pdf
- United States Renal Data System. (2016) USRDS annual data report: Epidemiology of kidney disease in the United States. Retrieved from: https://www.usrds.org/2016/view/Default.aspx
- Winkelmayer W. C. Schneeweiss S. Mogun H. Patrick A. R. Avorn J. Solomon D. H. (2005). Identification of individuals with CKD from Medicare claims data: A validation study. American Journal of Kidney Disease, 46(2), 225–232. 10.1053/j.ajkd.2005.04.029 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (1979). International classification of diseases and related health problems (9th ed.). Geneva, Switzerland. [Google Scholar]
- Wright J. A. Wallston K. A. Elasy T. A. Ikizler T. A. Cavanaugh K. L. (2011). Development and results of a kidney disease knowledge survey given to patients with CKD. American Journal of Kidney Disease, 57(3), 387–395. 10.1053/j.ajkd.2010.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]