Abstract
Background:
Hemodialysis patients need to make decisions about vascular access and diet that they may not fully understand. In this study, we hypothesized that patients with low health literacy are likely to choose a central venous catheter (CVC) and have higher serum potassium (K), serum phosphate (P), and inter-dialysis weight gains (IDWG).
Objective:
Primarily, the study sought to describe the health literacy of patients treated with hemodialysis in a Canadian tertiary care center. The secondary objective was to describe the association between health literacy and permanent vascular access choice, hyperkalemia, hyperphosphatemia, and IDWG.
Methods:
Adult patients receiving hemodialysis for more than 6 months were included. Health literacy was assessed with the Newest Vital Sign (NVS) test. Vascular access type and reasons for CVC use were determined. Serum K, P, and IDWG were collected retrospectively for 6 months. Student's t test and logistic regression were used to determine the association between health literacy (NVS score < 4 versus ≥ 4) and CVC choice, hyperkalemia, hyperphosphatemia, and high IDWG.
Key Results:
Fifty-six patients were involved. The average NVS score was 2.9. Overall, 66% of the patients had a CVC; one-third had chosen this access themselves. Poor control of K, P, and IDWG was experienced by 27%, 55%, and 36% of patients, respectively. The average NVS score was lower for patients choosing a CVC (p = .001), but not different for those with higher K, P, or IDWG. None of the patients who chose a CVC had adequate health literacy (NVS ≥ 4).
Conclusions:
Patients with low health literacy, who are eligible for both surgically created vascular access (fistula or graft) and CVC, are more likely to refuse fistula/graft creation compared to patients with adequate health literacy. Different educational strategies for such patients may help in appropriate decision-making. [Health Literacy Research and Practice. 2017;1(3):e136–e144.]
Plain Language Summary:
This study suggests that more than one-half of patients who receive hemodialysis may not understand all the information provided by their health care team. Despite a higher risk of complications with a central venous catheter, patients with lower health literacy prefer the catheter over fistula as their blood access for hemodialysis. We need to explore patient education to ensure that information is easy to understand.
The Canadian Public Health Association defines health literacy as the ability to access, understand, evaluate, and communicate information as a way to promote, maintain, and improve health in a variety of settings across the life course (Rootman & Gordon-El-Bihnety, 2008). It is estimated that 60% of adult Canadians lack the skills to manage their health literacy needs (Hoffman-Goetz, Donelle, & Ahmed, 2014). The most vulnerable groups among these are seniors, immigrants, and the unemployed, who all score far below the national average (Hoffman-Goetz, Donelle, & Ahmed, 2014).
Low health literacy skills are associated with poor disease knowledge and self-care abilities, difficulties making health-related decisions, increased morbidity and mortality, and higher health care costs (Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011; Cavanaugh et al., 2015; Cavanaugh et al., 2010; Gazmararian, Williams, Peel, & Baker, 2003; Geboers, de Winter, Spoorenberg, Wynia, & Reijneveld, 2016; Green et al., 2013; Heijmans, Waverijn, Rademakers, van der Vaart, & Rijken, 2015; Howard, Gazmararian, & Parker, 2005; Matsuoka et al., 2016; Weiss & Palmer, 2004; Williams, Baker, Parker, & Nurss, 1998). However, there is a lack of data linking low health literacy to decisions associated with poor clinical outcomes. Patients treated with hemodialysis are required to make complex choices regarding their vascular access and dietary regimen. Patients who use a central venous catheter (CVC) as a permanent hemodialysis vascular access are at higher risk for all-cause mortality, fatal infection, and cardiovascular events compared to patients with usable arteriovenous fistula (AVF) or arteriovenous graft (AVG) (Grubbs, Wasse, Vittinghoff, Grimes, & Johansen, 2014; Ravani et al., 2013; Zhang, Al-Jaishi, Na, de Sa, & Moist, 2014). For these reasons, there have been tremendous efforts to increase AVF/AVG use. As a result, in the United States, 68% of patients treated with hemodialysis are now using an AVF, and only 15% are using a CVC for dialysis. However, in Canada, CVC use is still about 45% (Pisoni, Zepel, Port, & Robinson, 2015). Similarly, poor dietary decisions can lead to poor control of potassium (K), phosphate (P), and large inter-dialysis weight gains (IDWG) that may also contribute to morbidity and mortality. High dietary K and P intake in patients treated with hemodialysis increases the risk of cardiac arrhythmia and sudden cardiac death (hyperkalemia) and metastatic calcification and progression of atherosclerosis (hyperphosphatemia) (Block, Hulbert-Shearon, Levin, & Port, 1998; Noori et al., 2010; Wu, Lee, & Wang, 2015). High sodium and fluid intake in dialysis patients leads to large IDWG necessitating high fluid removal rates to prevent volume overload. Rapid fluid removal during hemodialysis has been implicated in the development of myocardial stunning (Breidthardt, et al., 2012; Brown, Burrows, Pruett, & Burrows, 2015).
The primary aim of this hypothesis-generating study was to describe the health literacy of patients treated with hemodialysis in a tertiary care Canadian center and secondarily to describe the association between health literacy and (1) permanent vascular access choice and (2) dietary measures (hyperkalemia, hyperphosphatemia, and high IDWG). We hypothesized that patients with low health literacy skills would be more likely to choose a CVC and have worse potassium, phosphate, and fluid control compared to patients with adequate health literacy.
Methods
Patient Population
Adult patients, with end stage renal disease (ESRD) being treated with hemodialysis 3 times per week at The Ottawa Hospital (Ontario, Canada), were screened for study participation if they had been on dialysis for more than 6 months. We chose the 6-month period to allow enough time for the initial education that is, in our center, provided to all new patients treated with hemodialysis and/or their families. The education focuses on the pros and cons of each type of vascular access, as well as renal dietary restrictions. Initial vascular access education is provided by a coordinator and/or physician and reassessed at regular intervals. Initial education about diet is provided by a registered dietician and reassessed monthly.
Patients were excluded if they (1) were not fluent in English or Spanish (Newest Vital Sign [NVS], the health literacy tool we used in this study, was validated only in English and Spanish); (2) had moderate or severe dementia (Mini-Mental State Examination < 18) to minimize confounding due to cognitive dysfunction; (3) had severe vision/hearing impairment; (4) were too unwell to participate in the study; or (5) were unwilling or unable to provide written informed consent. The study was reviewed and approved by the Ottawa Hospital Science Network Research Ethics Board (protocol # 20140426-01H).
Measurement and Data Collection
After providing written consent, basic demographic data including age, sex, race, dialysis vintage, and comorbidities [calculated as Charlson comorbidity index adapted for patients with ESRD (Charlson, Pompei, Ales, & MacKenzie, 1987; Hemmelgarn, Manns, Quan, & Ghali, 2003)] were recorded. Type of vascular access and the reasons for CVC use, such as patient choice, imminent transfer to another treatment modality, or lack of surgical options, were collected from the electronic health record and from the vascular access coordinator at The Ottawa Hospital.
Data on IDWG, pre-dialysis serum potassium and phosphate levels over the 6 months prior to the patient's date of informed consent were extracted from the electronic medical record. IDWG was calculated as a percentage of the patient's target weight (TW). At least one IDWG greater than 5% of TW, serum K concentration > 6 mmol/L, and serum P concentration > 2 mmol/L were considered poor fluid and diet management.
Assessment of a Patient's Eligibility for a Surgically Created Access
Generally, a surgically created access (AVF or AVG) was not indicated if there was an expected imminent (within 3 months) transfer to another treatment modality (peritoneal dialysis or renal transplant) or AVF/AVG creation was contraindicated for medical reasons such as frailty, severe cardiac failure with ejection fraction < 30%, poor overall prognosis (< 6 months), and/or inadequate arm vasculature. The patient's fitness for AVF/AVG was first assessed by the responsible dialysis physician. Risks and benefits of the different vascular access options were reviewed and potential candidates were then referred to the vascular access clinic where a vascular surgeon made the final decision on patient's eligibility for AVF or AVG creation. Although patients were encouraged to consider a surgically created access, ultimately patients chose their type of vascular access.
Assessment of Health Literacy
Health literacy was assessed with the NVS test. NVS is a validated health literacy tool that tests the ability to read and apply information from a nutrition label. It consists of six items, each scoring one point. A score of ≥ 4 on the NVS is considered adequate health literacy. A score of 2 and 3 indicates the possibility of limited health literacy, and a score < 2 suggests a high likelihood of having inadequate health literacy skills (Weiss et al., 2005). In our study, we considered a score of < 4 as low health literacy. NVS was administered during dialysis sessions by trained study personnel in a private area of the clinic. All patients were in stable condition at the time of health literacy screening.
Outcomes
The primary outcome of our study was to describe the health literacy of patients treated with hemodialysis at The Ottawa Hospital, a Canadian tertiary care hospital. Our secondary outcomes were to determine the association between low health literacy (NVS < 4) and (1) the use of a CVC as the vascular access by patient choice, (2) hyperkalemia (K > 6 mmol/L), (3) hyperphosphatemia (P > 2 mmol/L), and (4) high IDWG (> 5% of target weight).
Statistical Analyses
Summary descriptive statistics for the study population including mean and standard deviation or median and interquartile range as appropriate were calculated. Student's t-test was used to compare selected variables between patients with adequate (NVS ≥ 4) versus low/limited health literacy (NVS < 4). The average NVS score was calculated for (1) patients who chose a CVC as their primary access, (2) had poor K control (> 6 mmol/L at least once in the preceding 6 months), (3) had poor P control (> 2 mmol/L at least once in the preceding 6 months), (4) had poor fluid management (IDWG > 5% of TW at least once in the preceding 6 months), and compared with a Student's t test. Lastly, odds ratios were calculated for these same variables for patients with adequate (NVS ≥ 4) versus low/limited health literacy (NVS < 4). All analyses were conducted with SAS (Version 9.4, SAS Inc. Cary, NC).
Results
Study Population and Baseline Characteristics
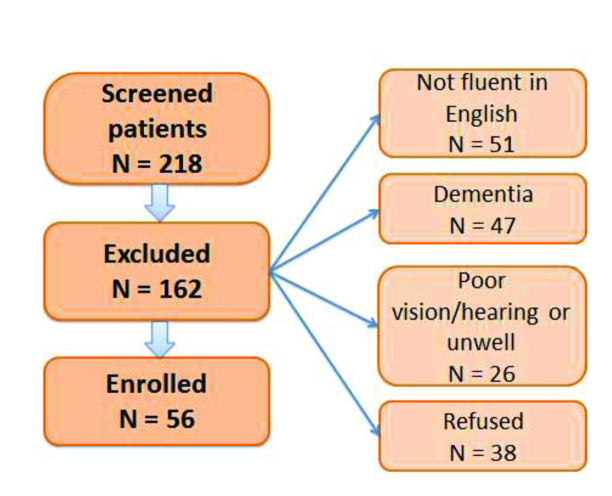
From 218 screened patients that had been treated with hemodialysis for more than 6 months, 162 patients did not meet enrollment criteria and were excluded (Figure 1). The baseline characteristics of the study cohort are presented in Table 1. Of 56 enrolled patients, most participants (63%) were men and had been treated with hemodialysis for more than 3 years. The average Charlson comorbidity index was 4. Thirty-seven of the 56 patients (66%) were using a CVC as a primary vascular access of which 12 patients had chosen this access type despite being candidates for AVF or AVG creation. Their characteristics are summarized in Table 2. Among the 12 patients who preferred a CVC over surgically created access, 4 reported fears of needles, 2 reported fear of witnessed AVF complications, and 6 patients did not attend or follow-up with the vascular access clinic without giving us any specific reason. From our electronic medical record, most of these 6 patients stated that they are content with the CVC and were not willing to pursue AVF/AVG.
Figure 1.
Creation of study cohort.
Table 1.
Characteristics of the Study Population
| Characteristic | All (N = 56) | Adequate HL (NVS ≥ 4); (N = 25) | Low HL (NVS < 4); (N = 31) | p value (Adequate vs. Low HL) |
|---|---|---|---|---|
| Age, years; mean (SD) | 62.6 (15.8) | 58.3 (15.8) | 66 (15.3) | .07 |
| Men; n (%) | 35 (62.5) | 15 (60) | 20 (64.5) | .79 |
| Ethnic minority; n (%) | 9 (16.1) | 2 (8) | 7 (22.6) | .14 |
| HD vintage, months; median (IQR) | 36.5 (13–66) | 34 (6–55) | 45 (21–92) | .23 |
| Charlson comorbidity index; mean (SD) | 4.0 (2.8) | 2.9 (2.7) | 4.9 (2.6) | .007 |
| Overall CVC;a n (%) | 37 (66.1) | 16 (64) | 21 (67.7) | .79 |
| CVC as patient choice;b n (%) | 12 (21.4) | 0 (0) | 12 (38.7) | <.001 |
| K, mmol/L; mean (SD) | 4.8 (0.5) | 4.8 (0.4) | 4.9 (0.5) | .77 |
| P, mmol/L; mean (SD) | 1.7 (0.4) | 1.7 (0.3) | 1.7 (0.4) | .87 |
| IDWG, % of TW, mean (SD) | 2.6 (0.9) | 2.8 (1) | 2.5 (0.9) | .26 |
Note. CVC = central venous catheter; HD = hemodialysis; HL= health literacy; IDWG = inter-dialysis weight gain; IQR = interquartile range; K = serum potassium; NVS = Newest Vital Sign; P = serum phosphate; SD = standard deviation; TW = target weight.
Total number of patients with CVC.
CVC as patient's choice even if considered a good candidate for arteriovenous fistula/graft.
Table 2.
Characteristics of the Patients Who Have Chosen Central Venous Catheter Despite Being Good Candidates for Arteriovenous Fistula or Graft
| Characteristic | Patients Who “Choose” CVC (N = 12) |
|---|---|
| Age, years; mean (SD) | 62 (12.8) |
| Men; n (%) | 7 (58.3) |
| Ethnic minority; n (%) | 3 (25) |
| HD vintage, months; median (IQR) | 40 (22–55) |
| Charlson comorbidity index; mean (SD) | 5.1 (2.2) |
| K, mmol/L; mean (SD) | 4.6 (0.4) |
| P, mmol/L; mean (SD) | 1.8 (0.4) |
| IDWG, % of TW, mean (SD) | 2.3 (0.9) |
Note. CVC = central venous catheter; HD = hemodialysis; HL= health literacy; IDWG = inter-dialysis weight gain; IQR = interquartile range; K = serum potassium; P = serum phosphate; SD = standard deviation; TW = target weight.
Health Literacy and Patients' Characteristics Associated with Low NVS Score
The overall average NVS score was 2.9 ± 2.1 (out of 6). Twenty-five patients (45%) had adequate health literacy skills (NVS ≥ 4) and 31 patients (55%) had a low score (< 4) on the NVS test, indicating limited or inadequate health literacy skills. Patients with low health literacy were older (p = .07) and had a significantly higher degree of comorbid illnesses, with an average Charlson comorbidity index of 4.9 compared to 2.9 in the group of patients with adequate health literacy (p = .007).
Clinical Outcome of Patients with Adequate and Low Health Literacy
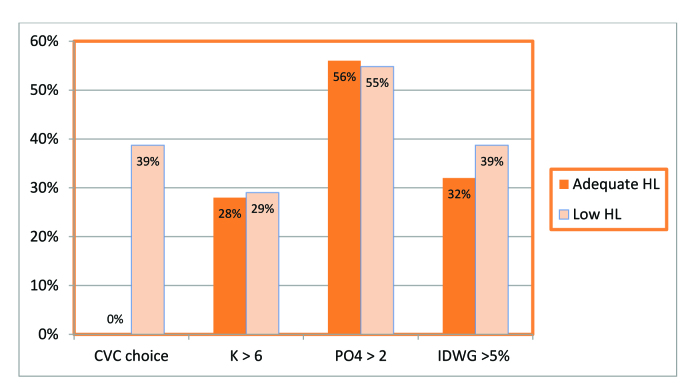
There was no difference in overall CVC use between adequate and low health literacy groups. However, none of the patients who had chosen a CVC despite being a good candidate for an AVF or AVG had adequate health literacy skills (Table 1 and Figure 2) The two groups did not differ in average pre-dialysis K, P, and IDWG (Table 1 and Figure 2). Poor control of K (at least one value above 6 mmol/L), P (at least one value above 2 mmol/L), and IDWG (at least one IDWG above 5% of TW) in the preceding 6 months was experienced by 27%, 55%, and 36% of patients, respectively. The average NVS score was not different for those with higher K, P, and IDWG, but was different for patients choosing a CVC (p = .001) (Table 3). Neither was using logistic regression NVS score was associated with poor control of K (OR 0.95 [0.30–3.06]), P [OR 1.05 (0.36–3.03)], or IDWG (OR 1.34 [0.44–4.07]).
Figure 2.
Clinical outcomes of patients with adequate and low health literacy. CVC = central venous catheter; HL = health literacy; IDWG = inter-dialysis weight gains; K = serum potassium.
Table 3.
NVS Test Average for CVC Choice, High Potassium, High Phosphate, and High Inter-dialysis Weight Gain
| Variable | Yes (No. of Patients) | No (No. of Patients) | p Value |
|---|---|---|---|
| CVC choice | 1.17a (12) | 3.64b (25) | .001 |
| K (at least one value >6 mmol/L) | 3.13 (16) | 2.88 (40) | .697 |
| P (at least one value >2 mmol/L) | 3.16 (31) | 2.68 (25) | .409 |
| IDWG (at least one value >5% TW) | 2.75 (20) | 3.06 (36) | .614 |
Note. CVC = central venous catheter; IDWG = inter-dialysis weight gain; K = serum potassium; NVS = Newest Vital Sign; P = serum phosphate; TW = target weight.
Patients who were good candidates for both CVC and fistula/graft, but chose CVC.
Patients with CVC who were not good candidates for fistula or graft, or who were awaiting an imminent treatment modality change (to peritoneal dialysis or transplant).
Discussion
In this study of 56 patients treated with hemodialysis, we found that more than one-half lacked adequate health literacy skills. Patients with low health literacy appear to be older and have a higher degree of comorbid illnesses compared to patients with adequate health literacy. Patient with lower health literacy were more likely to choose a CVC even if they were good candidates for an AVF/AVG creation. There was no association between health literacy and pre-dialysis serum levels of K, P, or IDWG. To our knowledge, this is the first report on the association of health literacy and the choice of vascular access in a population of Canadian patients who are treated with hemodialysis.
Limited health literacy is common among patients treated with hemodialysis with an overall prevalence of 27% (Fraser et al., 2013; Taylor et al., 2017). In our study, a much higher proportion (55%) of patients treated with hemodialysis lack adequate health literacy skills. This may be secondary to real differences or the use of different health literacy screening tools in each of the studies. In keeping with this hypothesis, a previously published US study that tested a non-dialysis chronic kidney disease population by NVS reported the prevalence of limited health literacy as 63% (Devraj et al., 2015).
We chose NVS for two reasons. First, the NVS tests the ability to read and understand a nutrition label, which is a critical self-management skill for a dialysis patient. Second, health literacy consists of several components including reading, writing, listening, speaking, cultural knowledge, and numeracy. The evaluation of numeracy in the NVS offers an additional advantage as many of the functional tasks patients are required to perform involve manipulation of numbers. Even patients who are highly educated and literate may have difficulty with understanding numbers (Shealy & Threatt, 2016). Approximately 55% of Canadian adults lack the numeracy skills to meet to demands of everyday life (Statistics Canada, 2005). Thus, NVS eliminates the ceiling effects of other non-numeracy health literacy screening tools (Morrison, Schapira, Hoffmann, & Brousseau, 2014; Rothman et al., 2006; Wright Nunes, Osborn, Ikizler, & Cavanaugh, 2015).
Several baseline characteristics of patients treated with hemodialysis have been shown to be associated with low health literacy: ethnic minorities, lower education attainment, lower income, older age, and greater level of comorbidity (Cavanaugh, et al., 2010; Green, et al., 2011; Grubbs, Gregorich, Perez-Stable, & Hsu, 2009). In our study, we specifically looked at age, sex, race, dialysis vintage, and the Charlson comorbidity index. Consistent with previous studies, we found that patients with lower health literacy are more likely to be older and have significantly higher comorbidity burden. We did not assess education level; therefore, it is difficult to determine if older age is a marker of a lower level of education attained and/or subtle cognitive changes that may contribute to lower health literacy scores. The association between higher comorbidity burden and lower health literacy may also be secondary to subtle cognitive dysfunction. Lastly, as a form of reverse causation, it is interesting to speculate that perhaps lower health literacy may lead to a greater risk of poor health choices that increase the risk for disease states.
There is limited information on choice of vascular access by patients treated with hemodialysis and health literacy. In a cross-sectional US study, patients dialyzing with AVF or AVG (as compared to CVC) were more likely to demonstrate limited health literacy in unadjusted analysis, however, further analyses suggested that this association was driven by study site (Green, et al., 2011). In another US cross-sectional study, low health literacy was associated with a 5-fold greater likelihood of CVC use compared to a surgically created vascular access, even after adjustment for age, gender, race, and years of dialysis (Cavanaugh et al., 2010). There are a few important differences between that study and ours, including a younger patient population surveyed (average age 51years), a higher percentage of African Americans (74%), and no adjustment for previous access history that may limit surgical options. Another study (by the same author) included 490 chronic incidents of patients treated with hemodialysis and concluded that lower dialysis knowledge is associated with CVC use. Patients who scored the equivalent of one standard deviation higher on the CHeKS (Chronic Hemodialysis Knowledge Survey) were 25% more likely to use an AVF or AVG at initiation of dialysis (Cavanaugh, Wingard, Hakim, Elasy, & Ikizler, 2009).
In our study of patients treated with hemodialysis, the overall CVC use was not different between adequate and low health literate groups. However, after excluding patients who were not candidates for a surgically created vascular access, or were awaiting an imminent transfer to another treatment modality (peritoneal dialysis or transplant), we found that none of the patients with adequate health literacy skills were using a CVC. This is an interesting finding as it suggests that the dialysis education we provide for our patients who are treated with hemodialysis may not be appropriate for less advanced learners. In other studies designed to identify the predictors of patient vascular access preference, sociocultural factors appear to be playing an important role and they may be modifiable (Fissell et al., 2013; Xi et al., 2011).
We anticipated that low health literacy would be associated with poor compliance with the dialysis diet due to a lack of understanding as demonstrated by poor K, P, and volume control. However, our study did not support this hypothesis as we did not find any differences between the adequate and low health literacy groups. Our small sample size and lack of information about residual renal function may have prevented us from detecting a significant difference by health literacy status. Alternatively, it is possible that the information provided by our registered dietitians is comprehensible for all patients. Conversely, the lack of a discernable difference between dietary measures may also imply that both patient groups do not understand the implications of poor diet choices. To our knowledge, no other study has addressed the impact of health literacy in the population of patients treated with hemodialysis at risk of hyperkalemia, hyperphosphatemia, and high inter-dialysis weight gains. However, limited health literacy has been associated with an increased incidence of missed dialysis treatments, emergency department visits, and hospitalizations due to ESRD-related complications (Green, et al., 2013).
Our study has several limitations including an inability to adjust for potential confounding variables secondary to our small sample size. Our cross-sectional study design prohibited us from increasing the number of participants. We had to exclude a significant number of patients because of language barrier and dementia. Although cognitive impairment is common and undiagnosed in the population of patients treated with hemodialysis, (Murray et al., 2006) a high proportion of patients with moderate and severe dementia in our center could be due to the fact that patients with preserved cognitive function tend to do home dialysis (peritoneal or hemodialysis) or are treated in our satellite dialysis units. We examined dietary measures over a relatively short window (6 months) and this may not adequately capture events. Socioeconomic factors, which are associated with health literacy, were not measured in our study. The observational nature of our study limits our conclusions to association and not causation.
In conclusion, our study suggests that low health literacy is a common problem that extends to the Canadian population of patients who are treated with hemodialysis and is associated with inappropriate vascular access decisions that may lead to unfavorable clinical outcomes. Health literacy-friendly strategies may need to be incorporated into our patient education sessions with a goal to decrease CVC utilization. However, larger studies with the ability to adjust for potential confounding variables are necessary before making any definitive conclusions.
References
- Berkman N. D. Sheridan S. L. Donahue K. E. Halpern D. J. Crotty K. (2011). Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine, 155(2), 97–107. 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- Block G. A. Hulbert-Shearon T. E. Levin N. W. Port F. K. (1998). Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: A national study. American Journal of Kidney Diseases, 31(4), 607–617. 10.1053/ajkd.1998.v31.pm9531176 [DOI] [PubMed] [Google Scholar]
- Breidthardt T. Burton J. O. Odudu A. Eldehni M. T. Jefferies H. J. McIntyre C. W. (2012). Troponin T for the detection of dialysis-induced myocardial stunning in hemodialysis patients. Clinical Journal of the American Society of Nephrology, 7(8), 1285–1292. 10.2215/CJN.00460112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown M. Burrows L. Pruett T. Burrows T. (2015). Hemodialysis-induced myocardial stunning: A review. Nephrology Nursing Journal, 42(1), 59–66. [PubMed] [Google Scholar]
- Cavanaugh K. L. Osborn C. Y. Tentori F. Rothman R. L. Ikizler T. A. Wallston K. A. (2015). Performance of a brief survey to assess health literacy in patients receiving hemodialysis. Clinical Kidney Journal, 8(4), 462–468. 10.1093/ckj/sfv037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh K. L. Rothman R. L. Wright J. A. Ikizler T. A. (2010, April). Limited health literacy associated with catheter use for chronic hemodialysis. Paper presented at the meeting of National Kidney Foundation, Orlando, FL. [Google Scholar]
- Cavanaugh K. L. Wingard R. L. Hakim R. M. Eden S. Shintani A. Wallston K. A. Ikizler T. A. (2010). Low health literacy associates with increased mortality in ESRD. Journal of the American Society of Nephrology. Advance online publication. 10.1681/ASN.2009111163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh K. L. Wingard R. L. Hakim R. M. Elasy T. A. Ikizler T. A. (2009). Patient dialysis knowledge is associated with permanent arteriovenous access use in chronic hemodialysis. Clinical Journal of the American Society of Nephrology, 4(5), 950–956. 10.2215/CJN.04580908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson M. E. Pompei P. Ales K. L. MacKenzie C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40(5), 373–383. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- Devraj R. Borrego M. Vilay A. M. Gordon E. J. Pailden J. Horowitz B. (2015). Relationship between health literacy and kidney function. Nephrology, 20(5), 360–367. 10.1111/nep.12425 [DOI] [PubMed] [Google Scholar]
- Fissell R. B. Fuller D. S. Morgenstern H. Gillespie B. W. Mendelssohn D. C. Rayner H. C. Pisoni R. L. (2013). Hemodialysis patient preference for type of vascular access: Variation and predictors across countries in the DOPPS. The Journal of Vascular Access, 14(3), 264–272. 10.5301/jva.5000140 [DOI] [PubMed] [Google Scholar]
- Fraser S. D. Roderick P. J. Casey M. Taal M. W. Yuen H. M. Nutbeam D. (2013). Prevalence and associations of limited health literacy in chronic kidney disease: A systematic review. Nephrology Dialysis Transplantation, 28(1), 129–137. 10.1093/ndt/gfs371 [DOI] [PubMed] [Google Scholar]
- Gazmararian J. A. Williams M. V. Peel J. Baker D. W. (2003). Health literacy and knowledge of chronic disease. Patient Education and Counseling, 51(3), 267–275. 10.1016/S0738-3991(02)00239-2 [DOI] [PubMed] [Google Scholar]
- Geboers B. de Winter A. F. Spoorenberg S. L. Wynia K. Reijneveld S. A. (2016). The association between health literacy and self-management abilities in adults aged 75 and older, and its moderators. Quality of Life Research, 25(11), 2869–2877. 10.1007/s11136-016-1298-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J. A. Mor M. K. Shields A. M. Sevick M. A. Arnold R. M. Palevsky P. M. Weisbord S. D. (2013). Associations of health literacy with dialysis adherence and health resource utilization in patients receiving maintenance hemodialysis. American Journal of Kidney Diseases, 62(1), 73–80. 10.1053/j.ajkd.2012.12.014 [DOI] [PubMed] [Google Scholar]
- Green J. A. Mor M. K. Shields A. M. Sevick M. A. Palevsky P. M. Fine M. J. Weisbord S. D. (2011). Prevalence and demographic and clinical associations of health literacy in patients on maintenance hemodialysis. Clinical Journal of the American Society of Nephrology, 6(6), 1354–1360. 10.2215/CJN.09761110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grubbs V. Gregorich S. E. Perez-Stable E. J. Hsu C. Y. (2009). Health literacy and access to kidney transplantation. Clinical Journal of the American Society of Nephrology, 4(1), 195–200. 10.2215/CJN.03290708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grubbs V. Wasse H. Vittinghoff E. Grimes B. A. Johansen K. L. (2014). Health status as a potential mediator of the association between hemodialysis vascular access and mortality. Nephrology Dialysis Transplantation, 29(4), 892–898. 10.1093/ndt/gft438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heijmans M. Waverijn G. Rademakers J. van der Vaart R. Rijken M. (2015). Functional, communicative and critical health literacy of chronic disease patients and their importance for self-management. Patient Education and Counseling, 98(1), 41–48. 10.1016/j.pec.2014.10.006 [DOI] [PubMed] [Google Scholar]
- Hemmelgarn B. R. Manns B. J. Quan H. Ghali W. A. (2003). Adapting the Charlson Comorbidity Index for use in patients with ESRD. American Journal of Kidney Diseases, 42(1), 125–132. 10.1016/S0272-6386(03)00415-3 [DOI] [PubMed] [Google Scholar]
- Hoffman-Goetz L. Donelle L. Ahmed R. (2014). Health literacy in Canada. A primer for students. Ontario, Canada: Canadian Scholars' Press, Inc. [DOI] [PubMed] [Google Scholar]
- Howard D. H. Gazmararian J. Parker R. M. (2005). The impact of low health literacy on the medical costs of Medicare managed care enrollees. The American Journal of Medicine, 118(4), 371–377. 10.1016/j.amjmed.2005.01.010 [DOI] [PubMed] [Google Scholar]
- Matsuoka S. Tsuchihashi-Makaya M. Kayane T. Yamada M. Wakabayashi R. Kato N. P. Yazawa M. (2016). Health literacy is independently associated with self-care behavior in patients with heart failure. Patient Education and Counseling, 99(6), 1026–1032. 10.1016/j.pec.2016.01.003 [DOI] [PubMed] [Google Scholar]
- Morrison A. K. Schapira M. M. Hoffmann R. G. Brousseau D. C. (2014). Measuring health literacy in caregivers of children. Clinical Pediatrics, 53(13), 1264–1270. 10.1177/0009922814541674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray A. M. Tupper D. E. Knopman D. S. Gilbertson D. T. Pederson S. L. Li S. Kane R. L. (2006). Cognitive impairment in hemodialysis patients is common. Neurology, 67(2), 216–223. 10.1212/01.wnl.0000225182.15532.40 [DOI] [PubMed] [Google Scholar]
- Noori N. Kalantar-Zadeh K. Kovesdy C. P. Murali S. B. Bross R. Nissenson A. R. Kopple J. D. (2010). Dietary potassium intake and mortality in long-term hemodialysis patients. American Journal of Kidney Diseases, 56(2), 338–347. 10.1053/j.ajkd.2010.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisoni R. L. Zepel L. Port F. K. Robinson B. M. (2015). Trends in US vascular access use, patient preferences, and related practices: An update from the US DOPPS practice monitor with international comparisons. American Journal of Kidney Diseases, 65(6), 905–915. 10.1053/j.ajkd.2014.12.014 [DOI] [PubMed] [Google Scholar]
- Ravani P. Palmer S. C. Oliver M. J. Quinn R. R. MacRae J. M. Tai D. J. James M. T. (2013). Associations between hemodialysis access type and clinical outcomes: A systematic review. Journal of the American Society of Nephrology, 24(3), 465–473. 10.1681/ASN.2012070643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rootman I. Gordon-El-Bihbety D. (2008). Canadian Public Health Association. A vision for a health literate Canada: Report of the expert panel on health literacy. Retrieved from https://www.cpha.ca/sites/default/files/uploads/resources/healthlit/report_e.pdf
- Rothman R. L. Housam R. Weiss H. Davis D. Gregory R. Gebretsadik T. Elasy T. A. (2006). Patient understanding of food labels: The role of literacy and numeracy. American Journal of Preventive Medicine, 31(5), 391–398. 10.1016/j.amepre.2006.07.025 [DOI] [PubMed] [Google Scholar]
- Shealy K. M. Threatt T. B. (2016). Utilization of the newest vital sign (NVS) in practice in the United States. Health Communication, 31(6), 679–687. 10.1080/10410236.2014.990079 [DOI] [PubMed] [Google Scholar]
- Statistics Canada. (2005). Human Resources and Skills Development Canada. Building on our Competencies: Canadian results of the international adult literacy and skills survey. Retrieved from http://www.statcan.gc.ca/pub/89-617-x/89-617-x2005001-eng.pdf
- Taylor D. M. Fraser S. D. S. Bradley J. A. Bradley C. Draper H. Metcalfe W. Roderick P. J. (2017). A systematic review of the prevalence and associations of limited health literacy in CKD. Clinical Journal of the American Society of Nephrology, 12(7), 1070–1084. 10.2215/CJN.12921216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss B. D. Mays M. Z. Martz W. Castro K. M. DeWalt D. A. Pignone M. P. Hale F. A. (2005). Quick assessment of literacy in primary care: The newest vital sign. The Annals of Family Medicine, 3(6), 514–522. 10.1370/afm.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss B. D. Palmer R. (2004). Relationship between health care costs and very low literacy skills in a medically needy and indigent Medicaid population. The Journal of the American Board of Family Medicine, 17(1), 44–47. 10.3122/jabfm.17.1.44 [DOI] [PubMed] [Google Scholar]
- Williams M. V. Baker D. W. Parker R. M. Nurss J. R. (1998). Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Archives of Internal Medicine, 158(2), 166–172. 10.1001/archinte.158.2.166 [DOI] [PubMed] [Google Scholar]
- Wright Nunes J. A. Osborn C. Y. Ikizler T. A. Cavanaugh K. L. (2015). Health numeracy: Perspectives about using numbers in health management from African American patients receiving dialysis. Hemodialysis International, 19(2), 287–295. 10.1111/hdi.12239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu H. C. Lee L. C. Wang W. J. (2015). Associations among time-average mineral values, mortality and cardiovascular events in hemodialysis patients. Renal Failure, 37(10), 343–353. 10.3109/0886022X.2015.1087862 [DOI] [PubMed] [Google Scholar]
- Xi W. Harwood L. Diamant M. J. Brown J. B. Gallo K. Sontrop J. M. Moist L. M. (2011). Patient attitudes towards the arteriovenous fistula: A qualitative study on vascular access decision making. Nephrology Dialysis Transplantation, 26(10), 3302–3308. 10.1093/ndt/gfr055 [DOI] [PubMed] [Google Scholar]
- Zhang J. C. Al-Jaishi A. A. Na Y. de Sa E. Moist L. M. (2014). Association between vascular access type and patient mortality among elderly patients on hemodialysis in Canada. Hemodialysis International, 18(3), 616–624. 10.1111/hdi.12151 [DOI] [PubMed] [Google Scholar]