Abstract
Background:
Conceptual literature has consistently noted that health literacy exists within a social context. This review examined how the intersection of social context and health literacy has been operationalized in quantitative, empirical research.
Methods:
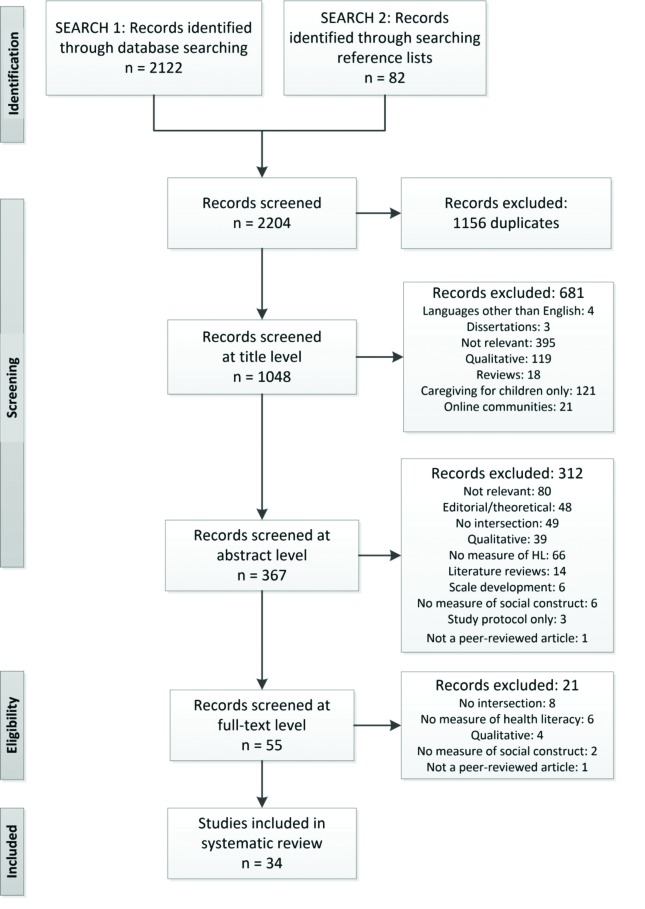
Following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, we searched seven databases, including PubMed and CINAHL (The Cumulative Index to Nursing and Allied Health Literature), using a range of potentially relevant keywords, and we hand-searched bibliographies. Inclusion criteria were quantitative studies of any design in which measurement of health literacy and measurement of social context intersected. We identified 1,052 unduplicated articles; 34 met inclusion criteria.
Key Results:
We found three distinct perspectives on the intersection between health literacy and social context. Most common (n = 23) were studies measuring an association between individual health literacy and individual social capital, social support, or social engagement, particularly whether social support varied by health literacy and/or if this relationship mediated health outcomes. Another group of studies (n = 6) took the perspective that being health literate by definition included social context, including access to and/or use of social support as a domain in individual health literacy assessment. Five studies considered the social context of health literacy as an independent property measured beyond the individual level; two measured community-level health literacy and three measured health literacy capacity/concordance in caregiving dyads. The studies showed significant definitional and measurement complexity and overlap. In the most dramatic example, a similar question was used across various studies to measure (1) health literacy, (2) a social support domain in health literacy, (3) social support, and (4) a study outcome distinct from, but associated with, health literacy. Potential useful methods, such as social network analyses, were missing from the literature.
Discussion:
Existing quantitative research on health literacy in a social context supports more attention to this topic. This review quantified evidence, revealed gaps, noted limitations, and identified important questions for future research. [Health Literacy Research and Practice. 2017;1(2):e41–e70.]
Plain Language Summary:
This study systemically compiles existing quantitative empirical research (34 articles) focusing on the intersection of health literacy in the social context. We find considerable measurement complexity in the current body of work on this topic and identify three distinct perspectives that researchers have taken while considering this topic. This information will be useful for future development of this important research area.
Health literacy is often defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and health services in order to make appropriate health decisions” (Ratzan & Parker, 2000). Low health literacy has been associated with many health outcomes, including poor health status among older adults, less diabetes-related knowledge, and increased hospitalization risk (Bailey et al., 2014; Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011). Health literacy is an active area of research, policy, and practice with the goal of improving health care outcomes and quality (Batterham, Hawkins, Collins, Buchbinder, & Osborne, 2016; Koh, Brach, Harris, & Parchman, 2013; Parker, Ratzan, & Lurie, 2003).
The conceptual literature has often noted that health literacy takes place within a social context, calling for empirical research to look beyond individual-level health literacy skill assessments and patient-provider interactions to consider the roles of dyads, families, and communities in health information acquisition, comprehension, and decision-making (Baker, 2006; Bevan & Pecchioni, 2008; Ishikawa & Yano, 2008; Lee, Arozullah, & Cho, 2004; McCormack, Haun, Sørensen, & Valerio, 2013; Nutbeam, 2000; Ratzan & Parker, 2000; Roter, Erby, Larson, & Ellington, 2007; Squiers, Peinado, Berkman, Boudewyns, & McCormack, 2012; Zaracadoolas, Pleasant, & Greer, 2005). A socially contextualized consideration of health literacy would better align empirical research on this topic with broader definitions of health literacy used in many international settings, where the ability to communicate effectively and/or to engage one's social network to achieve health goals is often considered a part of health literacy (Altin, Finke, Kautz-Freimuth, & Stock, 2014; Nutbeam, 2000; Roter et al., 2007). For instance, the World Health Organization's definition of health literacy explicitly includes “the social resources needed for individuals and communities to access, understand, appraise and use information and services to make decisions about health” (Greenhalgh, 2015). Greater inclusion of social context in health literacy research is also strongly supported by findings from other research traditions illuminating diverse ways in which social context can affect health information acquisition, comprehension, and decision-making, and the role social context plays in health outcomes generally (Heany & Israel, 2008; House, Landis, & Umberson, 1988; Sayers, White, Zubritsky, & Oslin, 2006; Smith & Christakis, 2008; Valente, 2010; Vassilev, Rogers, Kennedy, & Koetsenruijter, 2014). An important research gap exists in pursuit of this goal. No systematic assessment has been performed to identify if and how the active area of quantitative health literacy research is conceptualizing and operationalizing social context as recommended by both conceptual literature and international practice.
This review assessed the extent to which the intersection between social context and health literacy has been examined in quantitative research. As Lee et al. (2004) noted, much research considers low health literacy “simply as an individual trait independent of support and resources in an individual's social environment.” We sought to gain a broad understanding of how quantitative research is conceptualized and operationalized when health literacy is not considered an individual trait, and/or when support and resources in an individual's social environment are explicitly included in health literacy-focused analyses. To clarify terms, by “intersection” we mean any research that brings explicit measurement of social context and health literacy together, whether as an interaction, association, or measurement of health literacy beyond the individual level (such as in dyads, families, or communities). For “social context,” we include a variety of social research constructs, including social networks, social support, and social capital (Berkman, Glass, Brissette, & Seeman, 2000; Heany & Israel, 2008; Sampson, 1991; Smith & Christakis, 2008;). Generally, social networks are linkages among people that can be measured and assessed (Heany & Israel, 2008; Lin, 2001). Social support is the provision of emotional or instrumental support that can flow through social networks (Heany & Israel, 2008; Lin, 2001). Social capital is resources embedded within social networks that can be used or mobilized (Heany & Israel, 2008; Lin, 2001). All these constructs were possible examples of social context under our study criteria.
To our knowledge, existing reviews examining quantitative evidence relevant to health literacy and social context have had a narrower focus than this review, while also demonstrating the importance of this topic. Lee et al. (2004), in particular, set a clear research agenda for improved understanding of the relationships between health literacy, social support, and health outcomes, calling for more work to assess how social networks might “buffer and alleviate” the consequences of low health literacy after finding little literature on this important topic. The degree to which this agenda has been followed is not known. A 2015 review (Guzys, Kenny, Dickson-Swift, & Threlkeld, 2015) looked at health literacy measurement at the population level, concluding that the relevant instrumentation for measuring population health literacy were limited and primarily consisted of aggregates of individual assessments. Other reviews have considered the specific topic of caregiver/family literacy in cancer-focused communication, finding that the health literacy of an individual's caregiver or family is relevant to health outcomes but understudied (Bevan & Pecchioni, 2008; Sparks & Nussbaum, 2008). Existing reviews have focused on smaller pieces of our broad research concern—synthesizing the ways in which social context has been considered in current quantitative health literacy research— and this narrower focus may have led authors to miss key areas of conceptual or empirical overlap.
The study goal was to systematically review quantitative health literacy studies to determine (1) if they included an intersection between a measurement of both health literacy and social context (defined broadly) and, (2) if so, how they operationalized both health literacy and the social construct.
Method
We followed PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Moher, Liberati, Tetzlaff, Altman, & PRISMA Group, 2009), as presented in Table A. We searched seven databases, including PubMed and CINAHL (The Cumulative Index to Nursing and Allied Health Literature) (EBSCO), up to March 1, 2017 with no restriction on earlier dates. Keywords were health literacy plus the following terms: dyad OR triad OR caregiver OR social network OR social capital OR social support OR social network analysis/es. We also searched for the following exact phrases: social health literacy, group health literacy, community health literacy, family health literacy, neighborhood health literacy, caregiver health literacy, and distributed health literacy. We hand-searched the bibliographies of relevant articles. Specific details regarding databases and search terms are in Table B.
Table A.
PRISMA-P 2015 Checklist
| Section/Topic | Item # | Checklist Item |
|---|---|---|
| Administrative Information | ||
| Title | ||
| Identification | 1a | Identify the report as a protocol of a systematic review |
| We did this | ||
| Update | 1b | If the protocol is for an update of a previous systematic review, identify as such |
| N/A (It is not an update) | ||
| Registration | 2 | If registered, provide the name of the registry (e.g., PROSPERO) and registration number |
| We did not register this review | ||
| Authors | ||
| Contact | 3a | Provide name, institutional affiliation, and email address of all protocol authors; provide physical mailing address of corresponding author |
| Tetine Sentell, PhD: Office of Public Health Studies, University of Hawai'i, 1960 East-West Road, Honolulu, HI 96822; email: tsentell@hawaii.edu Ruth Pitt, MPH: Office of Public Health Studies, University of Hawai'i; email: ruthpitt@hawaii.edu Opal Vanessa Buchthal, DrPH: Office of Public Health Studies, University of Hawai'i; email: opalb@hawaii.edu |
||
| Contributions | 3b | Describe contributions of protocol authors and identify the guarantor of the review |
| T.S. - Conceived the protocol and drafted and finalized the protocol, will perform the abstract review, full text review, and quality assurance, and will be the guarantor R.P. - Commented on the study protocol, revised the protocol critically for important intellectual content, will be involved in the analysis and interpretation of the systematic review data, will also perform abstract review and full text review O.B. - Served as the adjudicator for the abstract review process, and was involved in analysis and interpretation of the systematic review data |
||
| Amendments | 4 | If the protocol represents an amendment of a previously completed or published protocol, identify as such and list changes; otherwise, state plan for documenting important protocol amendments. Expected protocol amendments are only to update search as needed before publication |
| Support | ||
| Sources | 5a | Indicate sources of financial or other support for the review |
| This study was funded by grant 1U54GM104944 from the Mountain West Clinical Translational Research - Infrastructure Network, under a grant from the National Institute of General Medical Sciences of the National Institutes of Health | ||
| Sponsor | 5b | Provide name for the review funder and/or sponsor |
| See above | ||
| Role of sponsor/funder | 5c | Describe roles of funder(s), sponsor(s), and/or institution(s), if any, in developing the protocol |
| The sponsor had no role in developing protocol | ||
| Introduction | ||
| Rationale | 6 | Describe the rationale for the review in the context of what is already known |
| Health literacy is a growing topic in research, policy, and practice. Conceptual literature has consistently noted that health literacy exists within a social context, but how often, and how the intersection of social context and health literacy has been conceptualized and operationalized in quantitative, empirical research is unknown | ||
| Objectives | 7 | Provide an explicit statement of the question(s) the review will address with reference to PICO |
Along with many others, we believe that health literacy is used and experienced within social networks. This systematic review will provide a timely evidence base on the empirical research about the following
We do not have specific study restrictions based on PICO. Our interest is describing which PCIO have been used in this research This will form a basis for future research, policy, and practice to allow health literacy research and efforts to more fully represent and more fully capitalize on the lived experience of how individuals use health information and make health decisions. This study will highlight gaps in the literature and areas for further research |
||
| Methods | ||
| Eligibility criteria | 8 | Specify the study characteristics (e.g., PICO, study design, setting, time frame) and report characteristics (e.g., years considered, language, publication status) to be used as criteria for eligibility for the review |
|
Overview: This review will include peer reviewed literature. To be included, studies must (a) include explicit measurement of both “health literacy” and of a “social construct,” and (b) quantitatively analyze an intersection between the measurement of health literacy and the measurement of a social construct. Study design: Only quantitative studies (or mixed methods with a quantitative study portion including the required portions) will be included Social context: We use the term “social context” to refer to a variety of social research constructs, including social networks, social support, and social capital. Social construct can also be measurement of health literacy at a level beyond that of the individual (e.g., dyad, family, community) Studies simply measuring the outcome for a child's health based on parental health literacy would not be included as there is no social context measure. However, a study that measured the health literacy concordance for two parents or the independent health literacy of a parent and a child would be included as the dyad then is the social context. Doctor-patient relationships are not included. Internet use is not included unless it explicitly includes a social engagement portion Study inclusion: Studies that explicitly measure a social construct and health literacy, but only include them as separate factors in a multivariable model are not included
Exclusion criteria: we will exclude studies not in English, dissertations, books or “gray” literature, or conference abstracts. Studies that do not include empirically measured, quantitative analyses of health literacy and the social construct, defined broadly, will be excluded. |
||
| Information sources | 9 | Describe all intended information sources (e.g., electronic databases, contact with study authors, trial registers, or other gray literature sources) with planned dates of coverage |
| We will search the databases for relevant articles as listed above. Reference lists of included articles will also be hand-searched | ||
| Search strategy | 10 | Present draft of search strategy to be used for at least one electronic database, including planned limits, such that it could be repeated |
| Keywords were “health literacy” plus the following terms: dyad OR triad OR social network OR social capital OR social support OR social network analysis/es. We also searched for the following terms: community health literacy, family health literacy, network health literacy, neighborhood health literacy, caregiver health literacy, and distributive health literacy. We also hand-searched the bibliographies of relevant articles | ||
| Study records | ||
| Data management | 11a | Describe the mechanism(s) that will be used to manage records and data throughout the review |
| We will upload search results into Zotero and Microsoft Excel and any duplicates will be removed | ||
| Selection process | 11b | State the process that will be used for selecting studies (e.g., two independent reviewers) through each phase of the review (i.e., screening, eligibility, and inclusion in meta-analysis) |
| Prior to any screening, reviewers will undergo training to ensure a comprehensive understanding of the review question, the inclusion and exclusion criteria, and a basic understanding of health literacy and social context principles. Titles and abstracts will first be screened for inclusion. For those that remain, eligibility will be assessed through full-text screening. Two reviewers will complete all screening separately and then discuss together to reach concordance At the title and abstract screening level, consensus must be reached with both reviewers to exclude an article; conflicts will be included. During full-text screening, disagreements will require resolution through consensus. If consensus cannot be achieved, a third reviewer will be called to make a decision Quality monitoring of the screening process will be done by the first author [T.S.], who will randomly select 10% of the total articles for revision. Assistance from an independent reviewer will be used if problems are found |
||
| Data collection process | 11c | Describe planned method of extracting data from reports (e.g., piloting forms, done independently, in duplicate), any processes for obtaining and confirming data from investigators |
| A data extraction form will be developed and pilot-tested on a selected subsection of studies. We will then amend the extraction form based on the pilot testing phase. Data will be extracted from each study that meets the inclusion criteria, likely including PICOS along with reference, language of interview, health outcome focus, study location, and study instruments and variables used in analysis. (Note, in the final data extraction, comparisons were not relevant given the broad scope of our study, so we did not extract this specifically.) The extraction process will be completed independently. Quality monitoring of the extraction process will be done by the first author [T.S.], who will randomly select 10% of the included articles for revision. If there is a disagreement, this will be resolved through consensus. If a consensus cannot be reached, a third reviewer [O.B.] will adjudicate | ||
| Data items | 12 | List and define all variables for which data will be sought (e.g., PICO items, funding sources), any preplanned data assumptions, and simplifications |
| Reference: per the academic abstract database Location of study: state and country Population of study: target population Size of population: size of population used in the analyses How health literacy defined: measurement(s) used and how variable was constructed How social network defined: measurement(s) used and how variable was constructed Type of study: qualitative, quantitative, or theory/landscape Study health focus: general description of study topic Outcomes: overall findings, and specifically if health literacy was associated with social context |
||
| Outcomes and prioritization | 13 | List and define all outcomes for which data will be sought, including prioritization of main and additional outcomes, with rationale |
| We have no restrictions on study outcomes. Instead, the study goal is to systematically review quantitative health literacy studies to determine (1) if they include an intersection between a measurement of health literacy and a measurement of a social construct (defined broadly, including social networks, social support, social capital); (2) if so, how they conceptualize the intersection between health literacy and the social construct; and (3) how such studies operationalize health literacy and the social construct. We then synthesized these findings to identify research gaps and to determine the state of the quantitative evidence on health literacy in a social-ecological context. We want to know: are people doing this research? Who is doing this research and where? How are they measuring these constructs? Does existing evidence support this way of thinking about health literacy (that it occurs in a social network context)? | ||
| Risk of bias in individual studies | 14 | Describe anticipated methods for assessing risk of bias of individual studies, including whether this will be done at the outcome or study level, or both; state how this information will be used in data synthesis |
| For such a small existing research literature with such a broad, diverse topic, we do not expect to be able to grade the quality of evidence. We will evaluate for bias using standard considerations, including poor reporting, industry funding, or disclosed conflict of interest and their association with study findings | ||
| Data | 15a | Describe criteria under which study data will be quantitatively synthesized |
| Synthesis | From all the studies identified from our search terms, we will consider if they include an intersection between a measurement of health literacy and a measurement of a social construct (defined broadly, including social networks, social support, social capital) by counting the included studies compared to those that we found from our search terms who did not meet study inclusion From those that are included, we will describe studies in terms of their participants, health focus, and location of research by counting them From those that are included, we will consider how they conceptualize the intersection between health literacy and the social construct and count by types of perspectives identified To determine how such studies operationalize health literacy and the social construct, we will count the numbers of instruments/variables used for health literacy and the social construct(s) |
|
| 15b | If data are appropriate for quantitative synthesis, describe planned summary measures, methods of handling data, and methods of combining data from studies, including any planned exploration of consistency (e.g., I2, Kendall's tau). N/A | |
| 15c | Describe any proposed additional analyses (e.g., sensitivity or subgroup analyses, meta-regression) | |
| We do not anticipate this literature to provide data suitable for subgroup analyses | ||
| 15d | If quantitative synthesis is not appropriate, describe the type of summary planned | |
| Question two in Item #13 (how they conceptualize the intersection between health literacy and the social construct) will involve a consideration of themes identified in the study. Also, the final question (to synthesize these findings to identify research gaps and to determine the state of the quantitative evidence on health literacy in a social-ecological context) will include a qualitative consideration and synthesis of what is missing | ||
| Meta-bias(es) | 16 | Specify any planned assessment of meta-bias(es) (e.g., publication bias across studies, selective reporting within studies). N/A |
| Confidence in cumulative evidence | 17 | Describe how the strength of the body of evidence will be assessed (e.g., GRADE). N/A |
Note: CINAHL = Cumulative Index to Nursing and Allied Health Literature; ERIC = Education Resources Information Center; GRADE = Grades of Recommendation, Assessment, Development and Evaluation; N/A = not applicable; PICO = participants, interventions, comparators, and outcomes; PICOS = participants, interventions, comparators, outcomes, and study design; PRISMA-P = Preferred Reporting Items for Systematic Reviews and Meta-Analyses–Protocols.
Table B.
Databases and Search Terms
Databases searched
Combined search terms
Exact phrases
|
Note. CINAHL = Cumulative Index to Nursing and Allied Health Literature; ERIC = Education Resources Information Center.
Inclusion Criteria
To be included, studies had to (1) include explicit measurement of both health literacy and of a social context variable, and (2) quantitatively analyze an “intersection” between these variables as described above.
Exclusion Criteria
Studies were excluded if not written in English or not in a peer-reviewed journal. There were no limitations on study design, or whether the analysis of the relationship between social context and health literacy was the primary research question or a secondary analysis. Doctor-patient communication was excluded as a distinct topic area given that the interaction occurs in a medical, rather than a social, context.
Screening
Two reviewers (T.S., R.P.) developed protocols to ensure a concordant understanding of the review questions and inclusion/exclusion criteria. Reviewers then independently screened titles and abstracts for duplicates and inclusion/exclusion criteria. If both reviewers agreed that a study did not meet inclusion criteria, the reason was noted and the study excluded. If there was disagreement, the study was included in full-text review.
Articles identified for full-text review were uploaded to a reference management database (Roy Rosenzweig Center for History and New Media, 2015). Full-text review was conducted independently by two reviewers, with disagreements resolved through consensus. If consensus could not be achieved, a third reviewer (O.B.) independently assessed the article and adjudicated.
Data Extraction
A data extraction form was developed, pilot-tested, and refined. Study design, sample size, participant demographics, health outcome focus, study location, health literacy measurement instrument(s), social context measurement instrument(s), and study variable(s) were extracted from each included study. Extraction was completed independently by the two reviewers (T.S., R.P.). A third reviewer (O.B.) again resolved disagreements.
Results
We identified 2,122 articles from the search terms and an additional 82 from hand-searching. After excluding duplicates, 1,048 articles were screened at the title level. A detailed PRISMA flow chart is shown in Figure 1.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram.
Thirty-four studies met inclusion criteria. Notable exclusions were studies that were relevant but qualitative, conceptual pieces/editorials, and/or quantitative articles that included health literacy and a social context variable as separate factors, often in multivariable models, but did not assess any intersection between them.
Study Descriptions
Included studies were diverse in design, location, and health topic focus, while focusing on many topics that have strong evidence in health literacy research generally, including the elderly, health care use, and chronic disease outcomes (Bailey et al., 2014; Berkman et al., 2011). For instance, whereas six studies focused explicitly on elder care/older adults (age ≥65 years), even in most studies of “adults” the mean age was older than 65 years. Few studies focused on adolescents. Detailed descriptions of these studies and their focal areas are in Table 1. Most studies (n = 21 of 34) were conducted in the United States; others were conducted in South Korea, Australia, the United Kingdom, Taiwan, Japan, China, and the Netherlands; 71% (n = 24) of articles were published in 2013 or later.
Table 1.
Description of Studies Meeting Inclusion Criteria
| Year | Authors | Sample Size | Sample Location | Sample Location Type | Focal Population | Health Issue | Age (mean years) |
|---|---|---|---|---|---|---|---|
| 1999 | Kalichman et al. | 138 people | USA (Georgia) | Community-recruited | African Americans with HIV | HIV treatment adherence | Adults (M = 39.7) |
| 2006 | Arozullah et al. | 400 people | USA (Chicago, IL) | Veteran's Affairs general inpatients | General inpatients | Preventable hospitalizations | Adults (M = 60.5) |
| 2006 | Lee et al. | 3,260 people | USA (Ohio, Texas, Florida) | Medicare enrollees in a national managed care organization | New Medicare enrollees | Health care use for older adults | 65+ |
| 2009 | Lee et al. | 489 people | USA (Illinois) | One hospital and one health center | Medicare recipients | Heath status of older adults | 65+ (M = 77.8) |
| 2010 | Johnson et al. | 275 people | USA (Georgia) | Pharmacy-based | Pharmacy patients | Medication adherence | Adults (M = 53.9) |
| 2010 | Osborn et al. | 130 people | USA (South Carolina) | One university medical clinic | Adults with diabetes | Type 2 diabetes | Adults (M = 62.7) |
| 2010 | Rosland et al. | 439 people | USA (Michigan) | A large university-based healthcare system | Patients with diabetes or heart failure | Diabetes or heart failure | Adults (range, 25–95) |
| 2010 | Ussher et al. | 321 people | UK (London) | One hospital | Adults with coronary heart disease | Coronary heart disease | 21–91 (M = 64.4) |
| 2011 | Rosland et al. | 439 patients, 88 primary care providers | USA (Michigan) | A large university-based healthcare system | Patients with diabetes or heart failure | Diabetes or heart failure | Adults (range, 25–95) |
| 2011 | Rubin et al. | 334 people | USA (Georgia) | Older adults receiving nutritional services from public agencies | Older adults receiving public nutritional services, African American or white | Health information and communication for older adults | 65+ (M = 74.70) |
| 2013 | Cimasi et al. | 114 counties | USA (Missouri) | Population-level analysis of state data | County-level population | Preventable hospitalization | Age groups from <15 to >65 |
| 2013 | Garcia et al. | 174 patient-caregiver dyads | USA (Texas) | Community clinics and senior centers in one city | Hispanic elders and caregivers | General health for older adults | 65+ (M elders = 75.5; M carers = 57.2) |
| 2013 | Inoue et al. | 269 people | Japan | 17 clinics | Adult diabetes patients | Type 2 diabetes | Adults (M = 64.4) |
| 2013 | Yang et al. | 1,098 people | Taiwan | Community-based, island-wide sampling frame | General population | Health information and communication | 15–85 years (M = 35.3) |
| 2014 | Fry-Bowers et al. | 124 people | USA (California) | Five women, infants and children clinics in one city | Low-income, Latina mothers | Child health | Adults (M = 30.25) |
| 2014 | Levin et al. | 17 patient/caregiver dyads | USA (Ohio) | Academic heart failure management program | Patients with heart failure and their caregivers | Heart failure | 65+ (M patients = 80.2; M caregivers = 66.9) |
| 2014 | Mayberry et al. | 192 people | USA (Tennessee) | One federally qualified health center | Adults with type 2 diabetes receiving care at a Federally Qualified Health Center | Type 2 diabetes | Adults (M = 51.6) |
| 2014 | Santos et al. | 144 teachers, 116 learners | USA (California) | Five English as a Second Language classes | English as a Second Language learners | Type 2 diabetes prevention | Adults |
| 2014 | Sentell et al. | 11,779 people | USA (Hawaii) | Population-based in a state | Hawaii residents | Individual and community-level health literacy | Age groups from 18–85+ |
| 2014 | Stewart et al. | 200 people | USA (Texas) | Subsample of larger smoking cessation treatment study | Adult smokers | Smoking and depression | Adults (M = 46.1) |
| 2014 | Waldrop-Valverde et al. | 210 people | USA (Florida) | One hospital and one clinic in one state | HIV positive | HIV and health care use | Adults |
| 2015 | Aikens et al. | 98 people | USA (Michigan, Ohio, Illinois, Indiana) | 16 outpatient Veterans' Affairs clinics in four states | Veterans' Affairs patients with diabetes | Diabetes medication adherence | Adults (M = 66.6) |
| 2015 | Beauchamp et al. | 813 people | Australia (urban and regional Victoria) | Health and community organizations | Health service users | Health information/communication | Adults (M = 72.1) |
| 2015 | Chisolm et al. | 278 parent/teen dyads | USA (Ohio) | Pediatric Medicaid accountable care organization | Teens with special health care need, Medicaid population | Adolescent health/chronic or disabling conditions/health communication | Teens (12–18) and their adult caregivers |
| 2015 | Hahn et al. | 295 people | USA (Illinois) | One outpatient clinic | Type 2 diabetes | Type 2 diabetes | Adults (M English = 54.8; M Spanish = 54.5) |
| 2015 | Kim et al. | 950 people | South Korea (Seoul) | Community-based; quota sampling on census data | Korean adults | Health information and communication | Adults 20–79 |
| 2015 | Kobayashi et al. | 4,368 people | England | Community-based, representative of population | Aging adults | Health literacy decline | Adults >52 |
| 2015 | Lambert et al. | 153 people | Australia (Wollongong) | Hospital renal unit | Patients with chronic kidney disease | Chronic kidney disease | Adults (M = 64.1) |
| 2015 | Maneze et al. | 552 people | Australia | Community-based (snowball sampling) | Filipino-Australians | Health-seeking behavior | Adults (M = 44) |
| 2016 | Dodson et al. | 100 dialysis patients and 813 controls | Australia (Melbourne) | Renal service (for dialysis patients) | People receiving dialysis vs. controls (consumers of other health or social services) | Quality of life and psychological distress of people receiving dialysis | Adults (M = 68.2) |
| 2016 | Geboers et al. | 3,241 people | The Netherlands | Subset of a population-based cohort study | Older adults | Health literacy, health behaviors, and social factors | Older adults (M = 68.9) |
| 2016 | Waverijn et al. | 1,811 people | The Netherlands | Population-based panel study | Chronic disease | Neighborhood social capital and chronic illness | Adults (M = 62.9) |
| 2016 | Zou et al. | 321 people | China (Shandong) | General hospital | Heart failure patients | Depressive symptoms and heart failure | Adults (M = 63.6) |
| 2017 | Jessup et al. | 384 people | Australia (Melbourne) | Acute public hospital | Hospital inpatients | Hospital services use | Adults (M = 64) |
Note. The study also included an additional 26 patients and 7 pharmacists in a qualitative component. The 275 individuals were in the quantitative component.
Constructs of Health Literacy and the Social Context Operationalized
A major issue identified was measurement inconsistency. Neither health literacy nor any aspect of social context was measured and/or operationalized in a consistent way across the 34 studies. Although various versions of the Test of Functional Health Literacy in Adults (TOFHLA) were the most common (n = 8), measures of health literacy in the 34 studies included 19 different instruments (Table 2).
Table 2.
Instrumentation of Health Literacy
| Instrument Used to Measure Health Literacy | Studies (n) | Study Citations |
|---|---|---|
| TOFHLA | 8 | |
| TOFHLA-Short Version | 7 | Garcia et al., 2013; Lee et al., 2006; Lee et al., 2009; Mayberry et al., 2014; Rubin et al., 2011; Stewart et al., 2014; Waldrop-Valverde et al., 2014 |
| TOFHLA (adapted to include HIV/AIDS related information) | 1 | Kalichman et al., 1999 |
| REALM | 5 | |
| REALM | 3 | Arozullah et al., 2006; Johnson et al., 2010; Ussher et al., 2010 |
| REALM-Teen | 1 | Chisolm et al., 2015 |
| REALM-Revised | 1 | Osborn et al., 2010 |
| Chew items | 6 | |
| Three Chew items | 3 | Levin et al., 2014; Maneze et al., 2015; Geboers et al., 2016 |
| One self-reported item (difficulty understanding written items) | 2 | Rosland et al., 2010; Rosland et al., 2011a |
| Unnamed self-reported measure of functional health literacyb | 1 | Aikens et al., 2015 |
| Other | 11 | |
| One self-reported item (“confidence filling out medical forms by yourself”) | 1 | Sentell et al., 2014 |
| Health LiTT | 1 | Hahn et al., 2015 |
| A validated instrument of health literacyc | 1 | Yang et al., 2013 |
| Korean Adult Health Literacy Scale | 1 | Kim et al., 2015 |
| Scales developed in Japan to assess functional, communicative, and critical health literacy | 1 | Inoue et al., 2013 |
| Four reading comprehension questions from fictitious medicine label-reading taskd | 1 | Kobayashi et al., 2015 |
| National Assessment of Adult Literacy data | 1 | Cimasi et al., 2013 |
| Chinese version of Health Literacy Scale for Patients with Chronic Disease | 1 | Zou et al., 2016 |
| Measure of Interactive Health Literacy | 1 | Rubin et al., 2011 |
| Assumed from study context: students taking ESL courses | 1 | Santos et al., 2014 |
| Health Literacy Management Scale | 1 | Lambert et al., 2015 |
Note:.ESL = English as a Second Language, LiTT = Health Literacy Assessment Using Talking Touchscreen Technology; REALM = Rapid Estimate of Adult Literacy in Medicine; TOFHLA = Test of Functional Health Literacy in Adults.
Authors deliberately exclude the other two Chew questions to avoid confounding.
Authors cite Chew et al. (2004, 2008) but do not indicate which questions were used or how scores were calculated.
From the information available in the article, the items in this instrument appear to be knowledge-based not skill/capacity-based, such as information about ideal body weight, fitness, and vaccines. This is a distinct way in which to define health literacy.
Developed by the Organisation for Economic Co-operation and Development and Statistics Canada for the Adult Literacy & Life Skills Survey.
The social context factor was also operationalized differently in each study. Even in the 19 studies using social support as a key outcome measure, none used the same version of the same scale. Four studies included iterations of the Medical Outcomes Study Social Support Scale (Lee, Gazmararian, & Arozullah, 2006; Lee, Arozullah, Cho, Crittenden, & Vicencio, 2009; Osborn, Bains, & Egede, 2010; Arozullah, et al., 2006). Some other validated social support scales included the Perceived Social Support Scale (Kalichman, Catz, & Ramachandran, 1999), the Family Support Scale (Fry-Bowers, Maliski, Lewis, Macabasco-O'Connell, & DiMatteo, 2014), the Duke Social Support Index (Maneze et al., 2015), the Social Support Questionnaire (Waldrop-Valverde, Guo, Ownby, Rodriguez, & Jones, 2014), the Enriched Social Support Instrument (Johnson, Jacobson, Gazmararian, & Blake, 2010), and the Interpersonal Support Evaluation List (Stewart et al., 2014). Social support was also measured by self-report using single items (Rosland, Piette, Choi, & Heisler, 2011), items created specifically for the study (Rosland, Heisler, Choi, Silveira, & Piette 2010), and unidentified measures (Hanh et al., 2015).
The three studies considering social capital also measured it in different ways. Two considered social capital as an individual-level construct: one asked who people knew by professional status (Yang, Kuo, Yang, & Yu, 2013), and the other used questions about participation in social groups (Kim, Lim, & Park, 2015). The third (Waverijn, Heijmans, Spreeuwenberg, & Groenewegen, 2016) considered social capital as a neighborhood-level construct. Kobayashi, Wardle, and von Wagner (2015) measured social engagement using participation in a variety of social activities, which was similar to the measure of social capital used by Kim et al. (2015).
Twelve studies analyzed distinct roles for different domains and/or types of at least one of the key study constructs (e.g., belonging vs. tangible social support; communicative vs. critical health literacy). Table C provides detailed information on how such domains/types were included in study measurement and analyses. Domains were not consistently chosen for analyses across studies, nor were they defined or measured in a standardized way, making domain-specific finding comparisons extremely challenging. Some studies noted that they used a measurement of health literacy or social context built from instruments that specifically captured distinct domains, but then used only one cumulative measure in analyses. That said, most studies that considered distinct roles for different domains found evidence of variation.
Table C.
Detail About Instrumentation for Health Literacy and the Social Construct of Interest for Associational Studies
| Authors | How HL is Measured | How the HL Variable is Operationalized | How Relevant Social Context Construct Is Measured | How Social Context Construct Is Operationalized | Domains in Analyses |
|---|---|---|---|---|---|
| Kalichman et al., 1999 | TOFHLA (adapted to include HIV/AIDS related information) | TOFHLA and self-reported education combined and dichotomized (low vs. higher-education literacy) | “A 15-item scale of perceived social support” (no details or citation given) | One continuous variable | No |
| Arozullah et al., 2006 | REALM | Dichotomized low vs. not low literacy, tried various cutpoints | Asked about social support structure and social support using the Medical Outcomes Social Support survey and also asking about “medical care support” | Three variables (medical support, organizational membership, people talked to in a typical week) | Yes in social support (and domains varied) |
| Lee et al., 2006 | S-TOFHLA | Dichotomized (low HL vs. high HL) | Five indicators from the Medical Outcomes Social Support instrument; plus two more questions: “How often do you have someone help you read things you get from the doctor or hospitals?” and “Does someone remind you to do things that will help you stay healthy, such as getting enough sleep or exercise or taking medications?” | Medical Outcomes Social Support items summed to one tangible support variable; other questions measured two other domains (medical information support and healthy reminder support) | Yes in social support (and domains varied) |
| Johnson et al., 2010 | REALM | Dichotomized (inadequate/marginal HL vs. adequate) | Enriched Social Support Instrument, which measures different types of social support (e.g., someone who listens, gives good advice, shows love and affection, helps with daily chores, someone whom they trust and can confide in) | One summed score; also considered subscales independently | Yes in social support (and domains varied) |
| Lee et al., 2009 | S-TOFHLA | Dichotomized (low HL vs. not) | 21-item Medical Outcome Study Social Support instrument | One summed score | No |
| Osborn et al., 2010 | REALM-R | Dichotomized (poor HL vs. not) Appear to use continuous score for analyses | 19-item Medical Outcomes Study Social Support Survey | One summed score | No |
| Rosland et al., 2010 | One self-reported item (difficulty understanding written items) | Dichotomized (low HL vs. not) | Created a family support for self-management' scale with five domains | One continuous variable in multivariable models | No |
| Ussher et al., 2010 | REALM | Dichotomized (low HL vs. adequate) | Three items of perceived social support: how much support from family and friends to discuss health problems, enough support from family and friends to discuss health problems, how important to see the same doctor or nurse | Each item analyzed separately (dichotomized) | Yes in social support (and domains varied) |
| Rosland et al., 2011 | One self-reported item (difficulty understanding written items) | Dichotomized (low HL vs. not) | One item self-report: whether one of your friends or family members comes into the exam room with you for your doctor's visit? | Dichotomous in main analysis (Yes or No) | No |
| Yang et al., 2013 | A validated instrument of health literacya | One summed scale | Asked about jobs of relatives, friends, and acquaintances sampled from two structural dimensions: occupational prestige and class. Indexes constructed about extensity, upper reachability, and range. | One composite social capital variable from indexes. | No |
| Inoue et al., 2013 | “Scales developed in Japan to assess functional, communicative and critical health literacy” Functional HL: need help to read instructions or leaflets from hospitals/pharmacies; Communicative HL: collect information from various sources; Critical HL: considered credibility of information |
All three subscales analyzed separately (as continuous) | Short-form version of the Multidimensional Scale of Perceived Social Support (Japanese version) | One summed score | Yes in health literacy (and domains varied) |
| Fry-Bowers et al., 2014 | Newest Vital Sign (English and Spanish) | Continuous | Family Support Scale | Total family support and two subscales: total informal support, and total formal support (all continuous) | Yes in social support (and domains varied) |
| Mayberry et al., 2014 | S-TOFHLA | Dichotomized (limited vs. adequate) | Diabetes Family Behavior Checklist II | Two subscales of positive and obstructive activities | Yes in social support (and domains varied) |
| Stewart et al., 2014 | S-TOFHLA | Descriptive data for inadequate, marginal and adequate HL. Appears to be used continuously in models | 12-item, Interpersonal Support Evaluation List | Looked at both total and three subscales (all continuous): appraisal (i.e., availability of emotional support), belonging (i.e., availability of companionship), and tangible (i.e., availability of material aids) | Yes in social support (and domains varied) |
| Waldrop-Valverde et al., 2014 | S-TOFHLA | Descriptive data for inadequate, marginal and adequate HLb | The Social Support Questionnaire (an HIV-specific instrument) | Used one scale from one domain as a continuous variable (“How often have you experienced social support since learning of HIV diagnosis?”) | No |
| Aikens et al., 2015 | Self-reported measure of functional health literacyc | Dichotomized (inadequate health care literacy vs. not)d | One item: Did patients opt to designate a care partner (a support person) to co-participate in a telemonitoring program? | Dichotomous (Yes or No) | No |
| Hahn et al., 2015 | Health LiTT (14-item short form using touch screen) | One T-score summary measure and one raw score (continuous) | Three items: Social support for diet item (a subscale of a diabetes-specific measure of health beliefs) | One continuous variable | No |
| Kim et al., 2015 | Korean Adult Health Literacy Scale | One summed score | Asked about participation in seven different types of social groups and counted the number of social groups. Asked about homogeneity (bonding social capital) and heterogeneity (bridging social capital) of each of the seven social groups | Total scale and two subscales (bridging and bonding social capital) | Yes, in social capital (and domains varied) |
| Kobayashi et al., 2015 | Four reading comprehension questions from fictitious medicine label reading task. Measure developed by the Organisation for Economic Co-operation and Development and Statistics Canada for the Adult Literacy & Life Skills Survey | Health literacy was defined using a continuous measure to indicate health literacy decline, defined as decreasing in score by ≥1 point between certain study waves | Social Detachment Index, which includes a range of civic, leisure, and cultural activities that would use diverse cognitive abilities | Engaged or not engaged at each time period; three levels from these over time periods: consistent, intermittent, or none | Yes for social engagement, with a cumulative effect for more engagement domains |
| Maneze et al., 2015 | Three self-reported items: difficulty understanding medical information, confidence in completing forms, and help needed reading hospital materials (Chew et al., 2004) | Summed and used as one continuous variable | Duke Social Support Index (modified to include social media) | One continuous variable | No |
| Geboers et al. 2016 | Chew et al. (2004; 2008) self-report screening questions: help reading hospital materials, confidence filling out medical forms, and problems learning about your medical condition because of difficulty understanding written information | Summed scores then dichotomized to high and low; also did sensitivity analyses for different cutpoints | Various social factors were considered, including social support, social activities and engagement with others, and the number of social contacts | Most social factors dichotomized in main analyses | Yes for various social context variables (and relationships varied) |
| Waverijn et al., 2016 | Four subscales from the Health Literacy Questionnaire | Looked specifically at subscales in analyses. No overall health literacy score | Neighborhood social capital was measured by five questions on contacts among neighbors: direct neighbors, other neighbors, how well people in the neighborhood know each other, if they are friendly, if there is a friendly neighborhood atmosphere in the neighborhood | Neighborhood-level variable indicating the degree to which the neighborhood social capital differed from the grand mean | Yes, in health literacy |
| Zou et al, 2016 | Chinese version of Health Literacy Scale for Patients with Chronic Disease | Continuous | Social support was measured by the Chinese version of the Multidimensional Scale of Perceived Social Support | Continuous | No |
Note. HL = health literacy; LiTT = health literacy assessment using talking touchscreen technology; REALM = Rapid Estimate of Adult Literacy in Medicine; REALM-R = Rapid Estimate of Adult Literacy in Medicine, Revised; S-TOFHLA = Short Test of Functional Health Literacy in Adults; TOFHLA = Test of Functional Health Literacy in Adults.
From the information available in the article, the items in this instrument appear to be knowledge-based, not skill capacity-based such as information about ideal body weight, fitness, and vaccines. This is a distinct way in which to define health literacy. They do not include a citation for this instrument.
These appear to be used continuously in model, although the authors don't state this.
Authors cite Chew et al. (2004, 2008), but do not indicate which questions were used or how scores were calculated.
Authors use both inadequate and low functional health literacy terminology.
A number of studies used the same question (“How often do you have someone help you read health care materials?” or a similarly-worded question), but characterized this as measuring different constructs. Several used this question as a functional health literacy measure (Inoue, Takahashi, & Kai, 2013; Levin, Peterson, Dolansky, & Boxer, 2014; Maneze et al., 2015). Another study characterized it as a measure of social support (Lee et al., 2006). Yet another used the question as an outcome variable called “competence with written material” and considered its relationship with a different measure of health literacy (as measured by the Newest Vital Sign) (Chisolm, Sarkar, Kelleher, & Sanders, 2015). One set of studies explicitly excluded this item because of the overlap with social support (Rosland, et al., 2010; Rosland et al., 2011). Finally, a similar question was used in the social support domain of at least one multidimensional health literacy instrument (Jordan, et al., 2013).
The Intersection Between Health Literacy and the Social Context
Another important finding was the distinct ways in which health literacy in a social context is being studied. From the 34 included studies, three perspectives for considering health literacy in a social context were identified, which we have termed association, definition, and property. One study (Inoue, et al., 2013) was included in both definition and association due to the various focal topics in this work. Details on this article can be found in Table 3 with the association articles.
Table 3.
Findings from Association Studies by Study Focus
| Social Factor | General Finding | Authors | Specific Health Literacy/Social Factor Intersection Finding |
|---|---|---|---|
| Social support | |||
| Lower health literacy is associated with increased social support | |||
| Arozzullah et al., 2006 | Patients with less than seventh-grade literacy were significantly more likely than patients with greater or equal than seventh-grade literacy to report always having social support for medical care. In contrast to similar studies, this study found that low literacy was not directly associated with preventability of hospitalization, possibly because prior studies did not account for social support resources | ||
| Rosland et al., 2010 | Low health literacy was associated with higher family involvement in care (compared to those without low health literacy) | ||
| Rosland et al., 2011 | Patients with low health literacy were more likely to have friends or family come to a doctor visit (compared to those without low health literacy) | ||
| Aikens et al., 2015 | Patients choosing to have a support person in care were more likely to have low health literacy than those who did not | ||
| Lower health literacy is associated with lower social support | |||
| Kalichman et al., 1999 | Those with lower education-health literacy lacked social support | ||
| Ussher et al., 2010 | Those with less social support from family and friends for discussing health problems had significantly lower health literacy than those with higher social support | ||
| Maneze et al., 2015 | Lower social support was related to lower health literacy in structural equation models | ||
| Social support does mediate/moderate the effects of health literacy to health outcomes | Stewart et al., 2014 | Lower health literacy was associated with more symptoms of depression; lower social support significantly mediated this relationship (lower health literacy was associated with lower perceived support, which predicted elevated symptoms of depression). The belonging support subscale accounted for most of the observed effect | |
| Osborn et al., 2010 | Health literacy had a direct effect on social support and, through social support, had an indirect effect on diabetes self-care and glycemic control. Lower health literacy was associated with more social support, which was in turn associated with better diabetes self-management | ||
| Social support does not mediate/moderate the effects of health literacy to health outcomes | Waldrop-Valverde et al., 2014 | Health literacy did not have a significant effect on study outcome (phlebotomy visit adherence). Social support was not a moderator of the effects of health literacy on the study outcome | |
| Health literacy does mediate/moderate the effects of social support to health outcomes | |||
| Johnson et al., 2010 | Social support was only associated with better medication adherence for patients with adequate health literacy, not for those with limited health literacy. In subscale analyses, having a trusted confidant was the only type of social support associated with better medication adherence for patients with limited literacy | ||
| Lee et al., 2009 | Social support had a stronger and more positive association with physical health in the high health literacy group. | ||
| Mayberry et al., 2014 | Participants with limited health literacy reported more supportive family behaviors for diabetes self-care than those with adequate health literacy, but did not report fewer obstructive family behaviors. At low levels of supportive family behaviors, obstructive family behaviors were associated with worse glycemic control and this effect was stronger for participants with limited health literacy | ||
| Zou et al., 2016 | In patients with heart failure, health literacy mediated the relationship between subjective social status and depressive symptoms | ||
| Mixed/no findings in social support | |||
| Geboers et al., 2016 | Low health literacy was associated with greater loneliness, engaging in fewer social activities, and having fewer social contacts, but not with social support. Low health literacy was negatively associated with both health behaviors and social factors in older adults. Social factors only moderated the associations between health literacy and cigarette smoking, not the other six tested health outcomes | ||
| Lee et al., 2006 | Those with low health literacy were more likely to have medical information support and heathy reminder support, but not tangible support. Only tangible support was associated with health outcomes | ||
| Inoue et al., 2013 | The relationship of health literacy to social support depends on the health literacy domain. Social support was associated with communicative and critical heath literacy, but not functional health literacy | ||
| Fry-Bowers et al., 2014 | No relationship between health literacy and social support. Maternal health literacy tended toward a negative relationship with formal support, but was not significant. | ||
| Hahn et al., 2015 | Higher health literacy was associated with less social support for diet. Health literacy did not mediate the effects of other factors, including social support, on health status or other health-related outcomes | ||
| Social capital (measured at the individual level) | |||
| Social capital is associated with health literacy | Yang et al., 2013 | Social capital was positively associated with individual health literacy | |
| Social capital does mediate/moderate the effects of health literacy to health outcomes | Kim et al., 2015 | There was a significant moderation effect of bridging social capital on the relation between health literacy and health information self-efficacy, and a moderation effect of bonding social capital on the relation between health literacy and health information-seeking intention | |
| Social capital (measured at the neighborhood level) | Waverijn et al., 2016 | Neighborhood social capital has a positive effect on health for people with a chronic illness, and this effect is stronger for people with better health literacy skills for accessing and understanding health information | |
| Social engagement | Social engagement helps to maintain health literacy over time | Kobayashi et al., 2015 | Social engagement (especially cultural engagement) was associated with aging-related health literacy decline in a protective manner, independent of cognitive function and decline |
Association
Most common (n = 23 or 68% of included studies) were those measuring an association between health literacy and a social context variable, where both are measured at the individual level. Nineteen focused on social support, three on social capital, and one on social engagement. The association articles primarily considered (1) whether people with low health literacy had more or less social support/social capital than those with higher health literacy, (2) if this social support/social capital was available/used in the health care context, or (c) whether the relationship between health literacy and social support/social capital influenced health-related outcomes. Table 3 presents these articles in terms of their general study findings and focus, revealing that findings on these questions are mixed. For instance, four studies found that those with lower health literacy had more social support for health than those with higher health literacy (e.g., Arozullah et al., 2006), whereas three others (e.g., Kalichman, et al., 1999) found that that those who reported less social support for health had lower health literacy.
Definition
The second perspective was that, by definition, part of being “health literate” includes the social context, typically the ability to leverage a social network to achieve health-related goals (n = 6). These met our study criteria of the intersection between health literacy and social context because these studies were asserting that the social context is, by definition, inextricably embedded in what it means to be health literate. In these studies, social support and/or use of this social support was included in the actual measurement instrument of “health literacy.” Details can be found in Table 4. The Health Literacy Management Scale uses four items to determine individuals' ability to seek social support to manage their health (Lambert, Mullan, Mansfield, Lonergan, 2015). The Health Literacy Questionnaire (HLQ) also includes a social support domain (Beauchamp et al., 2015). Of note, one recent study using the HLQ analyzed it only by domains and never created a cumulative health literacy score, effectively performing an associational study under our definition (Waverijn et al., 2016).
Table 4.
Findings from Definitional Studies
| Study | Measurement of Health Literacy | Specific Health Literacy/Social Factor Intersection Finding |
|---|---|---|
| Rubin et al., 2011 | Measure of Interactive Health Literacy | Interactive health literacy had an independent effect from document-based health literacy as measured by the Test of Functional Health Literacy in Adults. Both satisfaction with health care services and efficacy for chronic disease self-management were associated with turn-taking, the measure of interactivity |
| Santos et al., 2014 | Students taking English as a Second Language courses | About two-thirds reported having shared health information from the class with others (other classmates, spouses, elderly parents, friends, co-workers) |
| Beauchamp et al., 2015 | Health Literacy Questionnaire | Women had lower scores for social support for health (although effect sizes were small). Participants older than age 65 years were more likely to report having social support for health compared with younger participants. Living alone was associated with lower scores in social support for health |
| Lambert et al., 2015 | Health Literacy Management Scale | Having inadequate health literacy was common in chronic kidney disease patients, particularly in certain domains. These included social support as well as attending to one's health needs, understanding health information, and socioeconomic factors |
| Dodson et al., 2016 | Health Literacy Questionnaire | Compared to the control group, dialysis patients scored higher on the health literacy domains social support for health and engagement with health care providers but lower on active management of health |
| Jessup et al., 2017 | Health Literacy Questionnaire | In no analyses was there an association between a lower score on a Health Literacy Questionnaire scale and greater use of hospital services. This included the “social support for health” score. Instead, higher health literacy scores were associated with more use of services, with variation seen across relevant scales by outcome |
Property
The third perspective was that health literacy is an aggregated property (i.e., it can be understood at a group or network level). Of the five studies in this category, two measured health literacy at a community level and three measured health literacy capacity/concordance in a caregiving dyad. Table 5 provides more detail on these studies. Community-level measurement included health literacy within zip codes (Sentell, Zhang, Davis, Baker, & Braun, 2014) and counties (Cimasi, Sharamitaro, & Seiler, 2013). Dyads included parent-teen dyads (Chisolm et al., 2015) and older patient-caregiver dyads (Garcia, Espinoza, Lichtenstein, & Hazuda, 2013; Levin, et al., 2014). Dyads were not always concordant, and discordance had distinct health associations, highlighting the importance of considering the health literacy of caregivers and family members separately when studying health decision-making as well as considering the shared capacity for health literacy.
Table 5.
Property Studies
| Focus | Study | Measurement of Relevant Social Construct | Specific Health Literacy/Social Factor Intersection Finding |
|---|---|---|---|
| Community | |||
| Cimasi et al., 2013 | Population-level health literacy (by county) | Low community-level health literacy rates were associated with increased rates of preventable hospitalizations by county | |
| Sentell et al., 2014 | Individual and community-level health literacy (from zip codes) | Both individual and community health literacy were separately, independently associated with self-reported health | |
| Dyads | |||
| Chisolm et al., 2015 | Parent-teen dyads | Considered four categories by Rapid Estimate of Adult Literacy in Medicine-measured health literacy concordance: concordant high, parent high/teen low, parent low/teen high, and concordant low. Parent and teens were nonconcordant in more than 40% of dyads. Teens in parent high/teen low dyads reported lower competence with written material than concordant high dyads | |
| Garcia et al., 2013 | Caregiver dyads | No strong association between health literacy levels within caregiving dyads for older Hispanic patients | |
| Levin et al., 2014 | Caregiver dyads | 29% of caregivers had inadequate health literacy as evaluated by the label-reading task, although all caregivers had adequate health literacy as assessed by the self-report measure | |
Discussion
This systematic literature review identified 34 empirical studies that quantified some aspect of the intersection between social context and health literacy. In comparison, our search found over 50 theoretical, conceptual, or editorial pieces discussing the importance of social context and health literacy. Despite widespread theoretical discussions acknowledging the social context of health literacy, a number of explicit calls to research such topics (notably Lee et al., 2004), and a growing focus on this type of definition in international settings, the empirical evidence base that might advance our understanding of the connections between social context, health literacy, and health outcomes remains limited. However, given the recent dates of most of the identified articles (71% since 2013), it appears that this research area is growing. Yet, development of an evidence base on this topic is hampered by definitional and measurement complexity and overlap. In the most dramatic example, the question “How often do you have someone help you read health care materials?” or a very similar iteration was used across various studies to measure (1) health literacy, (2) a social support aspect of health literacy, (3) social support, and (4) a study outcome distinct from, but associated with, health literacy. This question has been correlated with health literacy or health outcomes in many empirical studies (Chew, Bradley, & Boyoko, 2004; Morris, MacLean, Chew, & Littenberg, 2006). But is this question measuring health literacy, social support, or some interactive combination of the two?
The previous example shows overlap in how the concepts of health literacy and social context were measured. There was also significant measurement complexity within each concept. For example, social capital was measured in three distinct ways (Kim et al., 2015; Yang et al., 2013), one of which was similar to the measurement instrument for social engagement in a third study (Kobayashi et al., 2015). In health literacy assessment, a wide range of measures were used. Even in the 19 studies using social support as the main outcome measure, none used the same version of the same scale. This makes comparisons across study findings complicated, possibly even misleading (i.e., if what is termed “social capital” in one study is the same as what is termed “social engagement” in another).
Lack of empirical or measurement clarity is not a new criticism of health literacy research (Altin et al., 2014; Baker, 2006; Guzys et al., 2015; Jordan, Buchbinder, & Osborne, 2010; Ussher, Ibrahim, Reid, Shaw, & Rowlands, 2010). Similarly, whereas social capital and social support are distinct constructs in the theoretical literature, in practice they are often operationalized using overlapping definitions and measurement (Berkman et al., 2000; Smith & Christakis, 2008). Given the growing interest in research on the intersection between social context and health literacy, there is an urgent need for empirical clarity across these constructs so research findings can be better understood and compared.
This need for clarity is underscored by the mixed findings in the best-studied topic in the review: social support and health literacy. Are mixed findings explained by the lack of consistency in the choice of measurement tools for both social support and health literacy? Are they a result of measurement and construct overlap across studies? Or perhaps the mixed findings reflect the diversity of research settings, as many were conducted in specific locations and cultures with a single health focus, making direct comparisons challenging, but also opening up numerous lines of investigation for future research. How does the relationship between social support and health literacy vary by health conditions, health status, age, populations, measurement instruments, and health literacy/social support domains? When are people most likely to draw on their social networks for health literacy support? Who do they include in these networks? When do social networks have a negative influence on health literacy and when is their influence positive (Berkman et al., 2000; Rosland et al., 2010)? It is also possible that the findings of existing studies are actually consistent. Perhaps those with low health literacy have less social support in general, but, to the extent that they are able, bring a companion to medical visits (as per Rosland et al., 2010) as a way to alleviate cognitive burden. Because of measurement complexity, it is challenging to use existing literature to resolve this question.
As a partial answer, the current literature suggests that the social context of health literacy may be particularly important for vulnerable groups, including those with English as a Second Language (Fry-Bowers, et al., 2014; Santos, Handley, Omark, & Schillinger, 2014), and may be highly relevant to communities with a family or communal (rather than individualistic) orientation, including racial/ethnic minorities and immigrant communities (Aranda & Knight, 1997; Choi, 2008; Garcia et al., 2013; Weiss, Gonzalez, Kabeto, & Langa, 2005). Thus, interventions that consider the social context of health literacy could help reduce health disparities. Most of our identified studies were conducted among those older than age 65 years, which is appropriate given that health literacy decreases with age, and older adults are particularly likely to have caregivers. However, other groups whose health literacy would be greatly affected by their social context, including teens and young adults, are understudied. In terms of geographical location, this review uncovered limited data from developing countries, where literacy may be lower and oral communication among social networks particularly salient. Most studies examined the relationship between health literacy and individual-level social support variables, with a few expanding into studying the patient-caregiver dyad. Relatively few studies examined health literacy within the broader context of the individual's community or social system.
No study used multidimensional measures for both health literacy and social context, which does not reflect the current multidimensional conceptualizations of these constructs (Berkman, et al., 2000; Heany & Israel, 2008; Sampson, 1991; Smith & Christakis, 2008). For example, whereas four studies used an iteration of the Medical Outcomes Study Social Support Survey, which has multiple domains, only two analyzed subdomains. Studies that did consider domain-specific findings found distinct variation in the relationship of the outcomes by domain (e.g., Lee et al., 2006).
The current evidence base on the broad topic of social context and health literacy is also missing relevant methods from other research traditions, especially social network analyses. Social network analysis is a distinct method of mapping and measuring relationships and information flows between people, groups, and/or organizations (Borgatti, Mehra, Brass, Labianca, 2009; Valente, 2010). Concerns include who is central to information flow, how often network members communicate, and how connected the network of one person might be to another's network. Such issues may be very important in health literacy, affecting how health information might be transmitted, comprehended, decided, or acted upon.
Another challenge in consolidating the evidence is the diverse conceptualizations of the intersection of health literacy and social context, as demonstrated by the three perspectives identified in this review. Nevertheless, each perspective is supported by a broader research tradition. The research considering an association draws from work describing social influences as both moderators and mediators of health literacy in conceptual models, such as the health literacy skills framework, in which social influences can affect both the development of individual health literacy and the relationship of health literacy to health outcomes (Squiers et al., 2012). The incorporation of social support into the actual definition of health literacy aligns with a long line of theoretical literature (e.g., Greenhalgh, 2015; Nutbeam, 2000; Roter et al., 2007). The idea of measuring health literacy beyond the individual level as a property of a group or network is supported by research in areas such as social network analyses.
These three different perspectives lead to distinct, but mutually supportive, policy and practice recommendations. The property perspective suggests that more work is required to assess the strength of community networks and their quality in terms of ability to provide support for health. The association perspective suggests fostering support from family and friends will be a useful intervention, if this can be done in a way that avoids unintended negative consequences. Supporting such efforts, Kobayashi et al. (2015) found that social engagement itself helps to sustain health literacy. If effective use of social networks is part of what makes one health literate, ensuring that people have both informed networks and the skills to draw on them should be part of effective interventions (Osborn et al., 2010).
Despite the many challenges identified, the overall body of research on health literacy in a social context strongly supports more attention to this topic. Evidence demonstrates what many know from experience: people do not deal with health issues alone, but use others to increase their “capacity to obtain, process, and understand basic health information and health services in order to make appropriate health decisions” (Ratzan & Parker, 2000). The relationship between social support and health literacy was statistically significant in all but one study (Waldrop-Valverde, et al., 2014). Although this is likely driven, to some extent, by the bias for publishing research presenting positive findings, we presume that the evidence is, generally, supporting the hypotheses of the many conceptual studies asserting that social context matters to health literacy in important, albeit complex, ways.
Limitations
We believe our search strategy identified most quantitative articles for which the primary research goal was to consider both health literacy (specifically named as such) and a measurement of social context. We may have missed some studies including an analysis of these variables as a secondary focus. Many other lines of research relevant to the ability to obtain, process, and understand health information exist, but do not include the specific term “health literacy.” This may be particularly true for relevant research around obtaining, processing, and understanding health information in a social context conducted in developing countries (Fonseca-Becker & Valente, 2006). Importantly, these are limitations that most researchers would similarly encounter in trying to access information on this topic, highlighting the utility of this project to systematically identify and consolidate the evidence base and to improve conceptual clarity in future research.
We focused only on quantitative studies. Qualitative evidence supports the supposition that health literacy takes place in a social context for both those with low individual health literacy (Adkins & Corus, 2009) and those with higher health literacy (Moloney, 2016).
This topic may be a fruitful one for secondary data analyses and for subanalyses in future projects. Many articles were excluded because they considered health literacy and a social construct (typically social support) as separate factors in a multivariable model, but did not consider any interaction between the two. Also, many included studies touted multidimensional instrumentation for health literacy and/or social context, but ultimately analyzed only one cumulative score. Thus, data already exist to consider and untangle some of the research gaps identified from this overview. Given the small and diverse literature, we did not grade the quality of evidence or perform a meta-analysis. Given the diversity of the findings (in both unexpected and expected directions), we did not expect major publication biases. As this is an active field, it is likely relevant new articles will soon exist.
Conclusions
Despite widespread discussion of the importance of the social context to health literacy in conceptual work, quantitative empirical evidence on this topic is limited. Findings are mixed; notably so in the most widely studied topic of social support and health literacy. At the same time, existing quantitative research on health literacy in a social context strongly supports more attention to this topic. Our review supports this work by quantifying the evidence, revealing research gaps, noting measurement limitations, and identifying important questions for future research.
References
- Adkins N. R. Corus C. (2009). Health literacy for improved health outcomes: Effective capital in the marketplace. Journal of Consumer Affairs, 43, 199–222. . 10.1111/j.1745-6606.2009.01137.x [DOI] [Google Scholar]
- Altin S. V. Finke I. Kautz-Freimuth S. Stock S. (2014). The evolution of health literacy assessment tools: A systematic review. BMC Public Health, 14, 1207. 10.1186/1471-2458-14-1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aikens J. E. Trivedi R. Aron D. C. Piette J. D. (2015). Integrating support persons into diabetes telemonitoring to improve self-management and medication adherence. Journal of General Internal Medicine, 30, 319–326. 10.1007/s11606-014-3101-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aranda M. P. Knight B. G. (1997). The influence of ethnicity and culture on the caregiver stress and coping process: A sociocultural review and analysis. The Gerontologist, 37, 342–354. 10.1093/geront/37.3.342 [DOI] [PubMed] [Google Scholar]
- Arozullah A. M. Lee S.-Y. D. Khan T. Kurup S. Ryan J. Bonner M. Yarnold P. R. (2006). The roles of low literacy and social support in predicting the preventability of hospital admission. Journal of General Internal Medicine, 21(2), 140–145. 10.1007/s11606-006-0248-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey S. C. Brega A. G. Crutchfield T. M. Elasy T. Herr H. Kaphingst K. Rothman R. A the NIDDKM-funded Centers for Diabetes Translational Research Centers' Health Literacy Interest Group. (2014). Update on health literacy and diabetes. Diabetes Educator, 40, 581–604. 10.1177/0145721714540220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker D. W. (2006). The meaning and the measure of health literacy. Journal of General Internal Medicine, 21, 878–883. 10.1111/j.1525-1497.2006.00540.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batterham R. W. Hawkins M. Collins P. A. Buchbinder R. Osborne R. H. (2016). Health literacy: Applying current concepts to improve health services and reduce health inequalities. Public Health, 132, 3–12. 10.1016/j.puhe.2016.01.001 [DOI] [PubMed] [Google Scholar]
- Beauchamp A. Buchbinder R. Dodson S. Batterham R. W. Elsworth G. R. McPhee C. Osborne R. H. (2015). Distribution of health literacy strengths and weaknesses across socio-demographic groups: A cross-sectional survey using the Health Literacy Questionnaire (HLQ). BMC Public Health, 15, 678. 10.1186/s12889-015-2056-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevan J. L. Pecchioni L. L. (2008). Understanding the impact of family caregiver cancer literacy on patient health outcomes. Patient Education and Counseling, 71, 356–364. 10.1016/j.pec.2008.02.022 [DOI] [PubMed] [Google Scholar]
- Berkman N. D. Sheridan S. L. Donahue K. E. Halpern D. J. Crotty K. (2011). Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine, 155, 97–107. 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- Berkman L. F. Glass T. Brissette I. Seeman T. E. (2000). From social integration to health: Durkheim in the new millennium. Social Science & Medicine, 51, 843–857. 10.1016/S0277-9536(00)00065-4 [DOI] [PubMed] [Google Scholar]
- Borgatti S. P. Mehra A. Brass D. J. Labianca G. (2009). Network analysis in the social sciences. Science, 323, 892–895. 10.1126/science.1165821. [DOI] [PubMed] [Google Scholar]
- Chew L. D. Bradley K. A. Boyko E. J. (2004). Brief questions to identify patients with inadequate health literacy. Family Medicine, 36, 588–594. [PubMed] [Google Scholar]
- Chew L. D. Grill J. P. Snyder A. Bradley K. A. Nugent S. M. Baines A. D. (2008). Validation of screening questions for limited health literacy in a large VA outpatient population. Journal of General Internal Medicine, 23, 561–566. 10.1007/s11606-008-0520-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisolm D. J. Sarkar M. Kelleher K. J. Sanders L. M. (2015). Predictors of health literacy and numeracy concordance among adolescents with special health care needs and their parents. Journal of Health Communication, 20, 43–49. 10.1080/10810730.2015.1058443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J. Y. (2008). Seeking health care: Marshallese migrants in Hawai'i. Ethnicity & Health, 13, 73–92. 10.1080/13557850701803171 [DOI] [PubMed] [Google Scholar]
- Cimasi R. J. Sharamitaro A. R. Seiler R. L. (2013). The association between health literacy and preventable hospitalizations in Missouri: Implications in an era of reform. Journal of Health Care Finance, 40, 1–16. [PubMed] [Google Scholar]
- Dodson S. Osicka T. Huang L. McMahon L. P. Roberts M. A. (2016). Multifaceted assessment of health literacy in people receiving dialysis: Associations with psychological stress and quality of life. Journal of Health Communication, 21(suppl. 2), 91–98. 10.1080/10810730.2016.1179370 [DOI] [PubMed] [Google Scholar]
- Fonseca-Becker F. Valente T. W. (2006). Promoting breastfeeding in Bolivia: Do social networks add to the predictive value of traditional socioeconomic characteristics? Journal of Health, Population and Nutrition, 24, 71–80. [PubMed] [Google Scholar]
- Fry-Bowers E. K. Maliski S. Lewis M. A. Macabasco-O'Connell A. DiMatteo R. (2014). The association of health literacy, social support, self-efficacy and interpersonal interactions with health care providers in low-income Latina mothers. Journal of Pediatric Nursing, 29, 309–320. 10.1016/j.pedn.2014.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia C. H. Espinoza S. E. Lichtenstein M. Hazuda H. P. (2013). Health literacy associations between Hispanic elderly patients and their caregivers. Journal of Health Communication, 18, 256–272. 10.1080/10810730.2013.829135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geboers B. Reijneveld S. A. Jansen C. J. M. de Winter A. F. (2016). Health literacy is associated with health behaviors and social factors among older adults: Results from the LifeLines Cohort Study. Journal of Health Communication, 21(suppl 2), 45–53. 10.1080/10810730.2016.1201174 [DOI] [PubMed] [Google Scholar]
- Greenhalgh T. (2015). Health literacy: Towards system level solutions. BMJ, 350, h1026. 10.1136/bmj.h1026 [DOI] [PubMed] [Google Scholar]
- Guzys D. Kenny A. Dickson-Swift V. Threlkeld G. (2015). A critical review of population health literacy assessment. BMC Public Health, 15, 215. 10.1186/s12889-015-1551-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn E. A. Burns J. L. Jacobs E. A. Ganschow P. S. Garcia S. F. Rutsohn J. P. Baker D. W. (2015). Health literacy and patient-reported outcomes: A cross-sectional study of underserved English- and Spanish-speaking patients with type 2 diabetes. Journal of Health Communication, 20, 4–15. 10.1080/10810730.2015.1061071 [DOI] [PubMed] [Google Scholar]
- Heaney C.A. Israel B.A. (2008). Social networks and social support. In Glanz K., Rimer B.K., Viswanath K. (Eds.),Health behavior and health education: Theory, research, and practice (pp. 189–210). San Francisco, CA: Jossey-Bass. [Google Scholar]
- House J. S. Landis K. R. Umberson D. (1988). Social relationships and health. Science, 241, 540–545. 10.1126/science.3399889 [DOI] [PubMed] [Google Scholar]
- Inoue M. Takahashi M. Kai I. (2013). Impact of communicative and critical health literacy on understanding of diabetes care and self-efficacy in diabetes management: A cross-sectional study of primary care in Japan. BMC Family Practice, 14, 40. 10.1186/1471-2296-14-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikawa H. Yano E. (2008). Patient health literacy and participation in the health-care process. Health Expectations, 11(2), 113–122. 10.1111/j.1369-7625.2008.00497.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jessup R. L. Osborne R. H. Beauchamp A. Bourne A. Buchbinder R. (2017). Health literacy of recently hospitalised patients: A cross-sectional survey using the Health Literacy Questionnaire (HLQ). BMC Health Services Research, 17 10.1186/s12913-016-1973-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson V. R. Jacobson K. L. Gazmararian J. A. Blake S. C. (2010). Does social support help limited-literacy patients with medication adherence? Patient Education and Counseling, 79, 14–24. 10.1016/j.pec.2009.07.002 [DOI] [PubMed] [Google Scholar]
- Jordan J. E. Buchbinder R. Osborne R. H. (2010). Conceptualising health literacy from the patient perspective. Patient Education and Counseling, 79, 36–42. 10.1016/j.pec.2009.10.001 [DOI] [PubMed] [Google Scholar]
- Jordan J. E. Buchbinder R. Briggs A. M. Elsworth G. R. Busija L. Batterham R. Osborne R. H. (2013). The health literacy management scale (HeLMS): A measure of an individual's capacity to seek, understand and use health information within the health-care setting. Patient Education and Counseling, 91, 228–235. 10.1016/j.pec.2013.01.013 [DOI] [PubMed] [Google Scholar]
- Kalichman S. C. Catz S. Ramachandran B. (1999). Barriers to HIV/AIDS treatment and treatment adherence among African American adults with disadvantaged education. Journal of the National Medical Association, 91, 439–446. [PMC free article] [PubMed] [Google Scholar]
- Kim Y.-C. Lim J. Y. Park K. (2015). Effects of health literacy and social capital on health information behavior. Journal of Health Communication, 20, 1084–1094. 10.1080/10810730.2015.1018636 [DOI] [PubMed] [Google Scholar]
- Kobayashi L. C. Wardle J. von Wagner C. (2015). Internet use, social engagement and health literacy decline during ageing in a longitudinal cohort of older English adults. Journal of Epidemiology and Community Health, 69, 278–283. 10.1136/jech-2014-204733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh H. K. Brach C. Harris L. M. Parchman M. L. (2013). A proposed “health literate care model” would constitute a systems approach to improving patients' engagement in care. Health Affairs, 32, 357–367. 10.1377/hlthaff.2012.1205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert K. Mullan J. Mansfield K. Lonergan M. (2015). A cross-sectional comparison of health literacy deficits among patients with chronic kidney disease. Journal of Health Communication, 20, 16–23. 10.1080/10810730.2015.1080329 [DOI] [PubMed] [Google Scholar]
- Lee S.-Y. D. Arozullah A. M. Cho Y. I. (2004). Health literacy, social support, and health: A research agenda. Social Science & Medicine, 58(7), 1309–1321. 10.1016/S0277-9536(03)00329-0 [DOI] [PubMed] [Google Scholar]
- Lee S.-Y. D. Gazmararian J. A. Arozullah A. M. (2006). Health literacy and social support among elderly Medicare enrollees in a managed care plan. Journal of Applied Gerontology, 25, 324–337. 10.1177/0733464806291314 [DOI] [Google Scholar]
- Lee S.-Y. D. Arozullah A. M. Cho Y. I. Crittenden K. Vicencio D. (2009). Health literacy, social support, and health status among older adults. Educational Gerontology, 35(3), 191–201. 10.1080/03601270802466629 [DOI] [Google Scholar]
- Levin J. B. Peterson P. N. Dolansky M. A. Boxer R. S. (2014). Health literacy and heart failure management in patient-caregiver dyads. Journal of Cardiac Failure, 20(10), 755–761. 10.1016/j.cardfail.2014.07.009 [DOI] [PubMed] [Google Scholar]
- Lin N. (2001). Social capital: A theory of social structure and action. Cambridge, UK: Cambridge University Press; 10.1017/CBO9780511815447 [DOI] [Google Scholar]
- Lubetkin E. I. Zabor E. C. Isaac K. Brennessel D. Kemeny M. M. Hay J. L. (2015). Health literacy, information seeking, and trust in information in Haitians. American Journal of Health Behavior, 39(3), 441–450. 10.5993/AJHB.39.3.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macario E. Emmons K.M. Sørensen G. Hunt M.K. Rudd R.E. (1998). Factors influencing nutrition education for patients with low literacy skills. Journal of the American Dietetic Association, 98, 559–564. 10.1016/S0002-8223(98)00125-4 [DOI] [PubMed] [Google Scholar]
- Maneze D. Salamonson Y. Poudel C. DiGiacomo M. Everett B. Davidson P. M. (2015). Health-seeking behaviors of Filipino migrants in Australia: The influence of persisting acculturative stress and depression. Journal of Immigrant and Minority Health, 18, 779–786. 10.1007/s10903-015-0233-x [DOI] [PubMed] [Google Scholar]
- Mayberry L. S. Rothman R. L. Osborn C. Y. (2014). Family members' obstructive behaviors appear to be more harmful among adults with type 2 diabetes and limited health literacy. Journal of Health Communication, 19, 132–143. 10.1080/10810730.2014.938840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack L. Haun J. Sørensen K. Valerio M. (2013). Recommendations for advancing health literacy measurement. Journal of Health Communication, 18, 9–14. 10.1080/10810730.2013.829892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D. Liberati A. Tetzlaff J. Altman D. G. PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6, e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moloney M. E. (2016). Bitten: A patient with tickborne disease struggles to find the right provider. Health Affairs, 35, 169–173. 10.1377/hlthaff.2015.0404 [DOI] [PubMed] [Google Scholar]
- Morris N. S. MacLean C. D. Chew L. D. Littenberg B. (2006). The Single Item Literacy Screener: Evaluation of a brief instrument to identify limited reading ability. BMC Family Practice, 7, 21. 10.1186/1471-2296-7-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutbeam D. (2000). Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 15, 259–267. 10.1093/heapro/15.3.259 [DOI] [Google Scholar]
- Osborn C. Y. Bains S. S. Egede L. E. (2010). Health literacy, diabetes self-care, and glycemic control in adults with type 2 diabetes. Diabetes Technology & Therapeutics, 12, 913–919. 10.1089/dia.2010.0058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker R. M. Ratzan S. C. Lurie N. (2003). Health literacy: A policy challenge for advancing high-quality health care. Health Affairs, 22, 147–153. 10.1377/hlthaff.22.4.147 [DOI] [PubMed] [Google Scholar]
- Ratzan S. C. Parker R. M. (2000). Introduction. In: Selden C.R., Zorn M., Ratzan S.C., Parker R.M. (Eds.), National Library of Medicine current bibliographies in medicine: Health literacy. NLM Pub. No. CBM 2000–1. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services. [Google Scholar]
- Rosland A-M. Heisler M. Choi H. Silveira M. J. Piette J. D. (2010). Family influences on self-management among functionally independent adults with diabetes or heart failure: Do family members hinder as much as they help? Chronic Illness, 6, 22–33. 10.1177/1742395309354608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosland A-M. Piette J. D. Choi H. Heisler M. (2011). Family and friend participation in primary care visits of patients with diabetes or heart failure: Patient and physician determinants and experiences. Medical Care, 49, 37–45. 10.1097/MLR.0b013e3181f37d28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roter D. L. Erby L. H. Larson S. Ellington L. (2007). Assessing oral literacy demand in genetic counseling dialogue: Preliminary test of a conceptual framework. Social Science & Medicine, 65, 1442–1457. 10.1016/j.socscimed.2007.05.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy Rosenzweig Center for History and New Media, 2015. Zotero. https://www.zotero.org/
- Rubin D. L. Parmer J. Freimuth V. Kaley T. Okundaye M. (2011). Associations between older adults' spoken interactive health literacy and selected health care and health communication outcomes. Journal of Health Communication, 16, 191–204. 10.1080/10810730.2011.604380 [DOI] [PubMed] [Google Scholar]
- Sampson J. (1991). Linking the micro-level and macro-level dimensions of community social organization. Social Forces, 70, 43–64. 10.2307/2580061 [DOI] [Google Scholar]
- Santos M. G. Handley M. A. Omark K. Schillinger D. (2014). ESL participation as a mechanism for advancing health literacy in immigrant communities. Journal of Health Communication, 19, 89–105. 10.1080/10810730.2014.934935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayers S. L. White T. Zubritsky C. Oslin D. W. (2006). Family involvement in the care of healthy medical outpatients. Family Practice, 23, 317–324. 10.1093/fampra/cmi114 [DOI] [PubMed] [Google Scholar]
- Sentell T. Zhang W. Davis J. Baker K. K. Braun K. L. (2014). The influence of community and individual health literacy on self-reported health status. Journal of General Internal Medicine, 29, 298–304. 10.1007/s11606-013-2638-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith K. P. Christakis N. A. (2008). Social networks and health. Annual Review of Sociology, 34, 405–429. 10.1146/annurev.soc.34.040507.134601 [DOI] [Google Scholar]
- Sparks L. Nussbaum J. F. (2008). Health literacy and cancer communication with older adults. Patient Education and Counseling, 71, 345–350. 10.1016/j.pec.2008.02.007 [DOI] [PubMed] [Google Scholar]
- Squiers L. Peinado S. Berkman N. Boudewyns V. McCormack L. (2012). The Health Literacy Skills Framework. Journal of Health Communication, 17, 30–54. 10.1080/10810730.2012.713442 [DOI] [PubMed] [Google Scholar]
- Stewart D. W. Reitzel L. R. Correa-Fernández V. Cano M. Á. Adams C. E. Cao Y. Vidrine J. I. (2014). Social support mediates the association of health literacy and depression among racially/ethnically diverse smokers with low socioeconomic status. Journal of Behavioral Medicine, 37, 1169–1179. 10.1007/s10865-014-9566-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ussher M. Ibrahim S. Reid F. Shaw A. Rowlands G. (2010). Psychosocial correlates of health literacy among older patients with coronary heart disease. Journal of Health Communication, 15, 788–804. 10.1080/10810730.2010.514030 [DOI] [PubMed] [Google Scholar]
- Valente T.W. (2010). Social networks and health: Models, methods, and applications. New York, NY: Oxford University Press; 10.1093/acprof:oso/9780195301014.001.0001 [DOI] [Google Scholar]
- Vassilev I. Rogers A. Kennedy A. Koetsenruijter J. (2014). The influence of social networks on self-management support: A metasynthesis. BMC Public Health, 14, 719. 10.1186/1471-2458-14-719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldrop-Valverde D. Guo Y. Ownby R. L. Rodriguez A. Jones D. L. (2014). Risk and protective factors for retention in HIV care. AIDS and Behavior, 18, 1483–1491. 10.1007/s10461-013-0633-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waverijn G. Heijmans M. Spreeuwenberg P. Groenewegen P. P. (2016). Associations between neighborhood social capital, health literacy, and self-rated health among people with chronic illness. Journal of Health Communication, 21(suppl. 2), 36–44. 10.1080/10810730.2016.1179369 [DOI] [PubMed] [Google Scholar]
- Weiss C. O. González H. M. Kabeto M. U. Langa K. M. (2005). Differences in amount of informal care received by non-Hispanic whites and Latinos in a nationally representative sample of older Americans. Journal of the American Geriatrics Society, 53, 146–151. 10.1111/j.1532-5415.2005.53027.x [DOI] [PubMed] [Google Scholar]
- Yang H-H. Kuo S-C. Yang H-J. Yu J-C. (2013). Social capital and health literacy in Taiwan. Health, 5, 898–902. 10.4236/health.2013.55118 [DOI] [Google Scholar]
- Zarcadoolas C. Pleasant A. Greer D. S. (2005). Understanding health literacy: An expanded model. Health Promotion International, 20, 195–203. 10.1093/heapro/dah609 [DOI] [PubMed] [Google Scholar]
- Zou H. Chen Y. Fang W. Zhang Y. Fan X. (2016). The mediation effect of health literacy between subjective social status and depressive symptoms in patients with heart failure. Journal of Psychosomatic Research, 91, 33–39. 10.1016/j.jpsychores.2016.10.006 [DOI] [PubMed] [Google Scholar]