Abstract
Purpose:
Increased intracranial pressure (ICP) is one of the prevalent symptoms of trauma, especially traumatic headache, which requires quick action for the diagnosis and treatment. The optic nerve sheath diameter (ONSD) is a newly proposed technique for the detection of an increase in ICP. The aim of this study was to assess the efficacy of this new diagnostic method in patients with increased ICP induced by trauma.
Methods:
This prospective study was conducted between December 2016 and February 2017. The patients with traumatic headache and who had been diagnosed with increased ICP using clinical signs and computed tomography scan were compared to the voluntary healthy group. In each patient, measurements were performed employing ultrasound three times on each eye in an axial region, and the mean of these sizes was obtained as the ONSD.
Results:
A total of 112 participants were examined. The mean ONSD measurement of the patients and the voluntary healthy group was 6.01 ± 0.76 and 3.41 ± 0.56 mm in the right eye, 6.11 ± 0.75 and 3.39 ± 0.54 mm in the left eye, and 6.06 ± 0.75 and 4.02 ± 1.07 mm in both sides, respectively. The ONSD in the right and left sides had high and significant correlation in the patients (r = 0.929, P < 0.000) and voluntary healthy (r = 0.630, P < 0.000) group. The mean ONSD of one of the patients was 6.24 ± 0.56 mm, and in another patient with no clinical sign of increased ICP, the mean ONSD was 4.61 ± 0.09 mm.
Conclusions:
Ultrasound performed on the diaphragm of the optic nerve with acceptable sensitivity can detect patients with an increase in ICP and can be efficacious in expediting the action needed to reduce ICP. Due to the sensitivity and specificity of the ultrasound and high accuracy of the diameter of optic nerve sheath in detecting increase in ICP, as well as considering the fact that ultrasound is a noninvasive and available technique; it can be performed at the patient's bedside.
Keywords: Intracranial pressure, optic nerve sheath, traumatic brain injury, ultrasound
INTRODUCTION
The intracranial pressure (ICP) is determined by the total volume of the brain, the cerebrospinal fluid (CSF) fluid, and the blood in the skull and its contents.[1] Increased ICP is one of the prevalent symptoms of trauma, especially traumatic headache, which requires quick action to diagnose and posttreatment measures.[2,3] This challenge associated with increased ICP increases the mortality rate.[4] Today, several techniques are employed to diagnose ICP; each technique has its challenges. The use of intracranial catheters may cause coagulopathy or thrombocytopenia.[5] The use of skull computed tomography (CT) scan is an invasive technique; because it contains ionizing radiation,[6] and CT scan may not be available in every healthcare delivery center.[7] The use of transcranial Doppler is a safe technique for the diagnosis of increased ICP, but its use requires mastery. About 5% of the pictures taken by CT scan are undesirable.[7,8] In these situations, to detect a timely increase in ICP, a noninvasive technique can be useful in detecting an increase in ICP or modifying ICP. The eyes often reflect the presence of the disease in various parts of the body. It occurs in the form of changes in the retina due to hypertension episodes or in the form of papilledema secondary to increased ICP.[9] The optic nerve sheath diameter (ONSD) is a newly proposed technique for detecting an increase in ICP.[10] The proximal portion of the optic nerve sheath complex in the hypoechoic ultrasound contrasts with the hyperechoic ultrasound, which is Retro Blub fat, and provides a noninvasive technique for detecting the increase in ICP.[11] Some studies in different parts of the world have observed that the changes in ONSD are strongly in consonance with CT scan image findings, which has vivid evidence of an increase in ICP.[12,13,14,15] The aim of this study was to assess the efficacy of ultrasound of the optic nerve sheath in the diagnosis of increase in ICP in trauma patients.
METHODS
This prospective study was conducted according to the Sequenced Treatment Alternatives to Relieve Depression (STARD)[16] between December 2016 and February 2017. After obtaining approval from the Ethics Committee of Ahvaz Jundishapur University and written consent, the patients referred to the Emergency Department of Ahvaz Golestan Hospital, who had clinical traumatic symptoms of increased ICP as shown by CT scan, were compared with voluntary healthy group. The CT scan image was then taken from the patients, and these findings were examined by two radiologists who were blinded to ONSD measurements. CT scan was carried out to investigate the presence of brain lesion and symptoms of increased ICP such as midline shifts, 3 mm or more due to the effect of space-occupying lesions, third ventricle collapse, hydrocephalus, sulcal effacement with significant edema symptoms, and abnormal mesencephalic cistern.
The criteria for excluding patients from this study were age <18 years, having a history of glaucoma or taking medicines that affect CSF, having eye diseases such as tumors or eye trauma, exposure to substances or poison that reduce consciousness, as well as electrolyte disturbances (hypo or hyperthyroid and hypo or hyperglycemia). The characteristics of each patient, including Glasgow Coma Scale (GCS), age, sex, height, weight, mechanism, and severity of brain damage were collected.
Ultrasound measurements
First, the ultrasound of the eye of the patients was performed by a researcher with a SONOSCAPE-SSI 6000 (Shenzhen, Guangdong, P.R China) machine that had a linear probe of 5–10 MHz. The patients were placed in the supine position with their eyes closed, and then, the ultrasound gel was placed on the eyelid. For measurement of optic nerve sheath, a diameter of 3 mm was measured in the posterior to the globe [Figure 1]. In each patient, the measurement was done three times on each eye in an axial region, and the mean of these sizes was obtained as ONSD.
Figure 1.
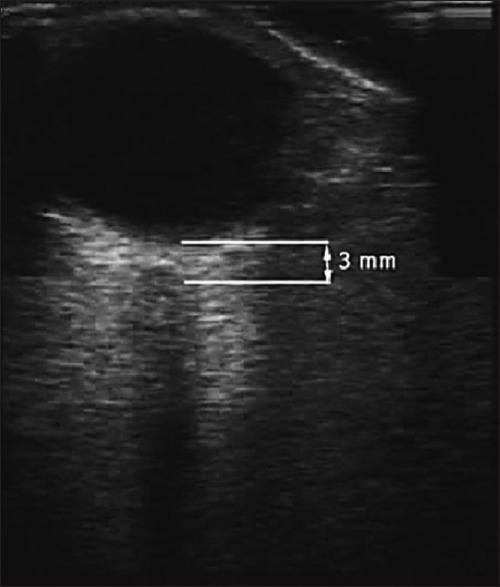
Measurement of the diameter of the optic nerve sheath, 3 mm posterior to the globe
Statistical analysis
All data were analyzed using SPSS software. To describe the data, the mean and standard deviation were employed for quantitative variables whereas frequency and percentage were used for qualitative variables. Pearson correlation coefficient or Spearman correlation coefficient, t-test, Mann–Whitney test, and Chi-square test were employed for data analysis.
RESULTS
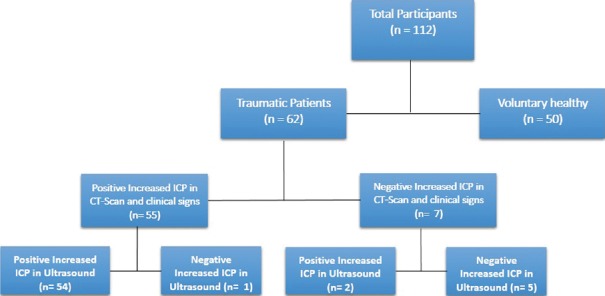
Of the 112 participants studied [Figure 2], 86 (76.8%) were male, and 26 (23.2%) were female. The mean age of the patients and the voluntary healthy group was 34.8 ± 14.3 years (between 19 and 75 years) and 29.8 ± 9.8 years (between 20 and 66 years), respectively.
Figure 2.
Sequenced treatment alternatives to relieve depression flow diagram
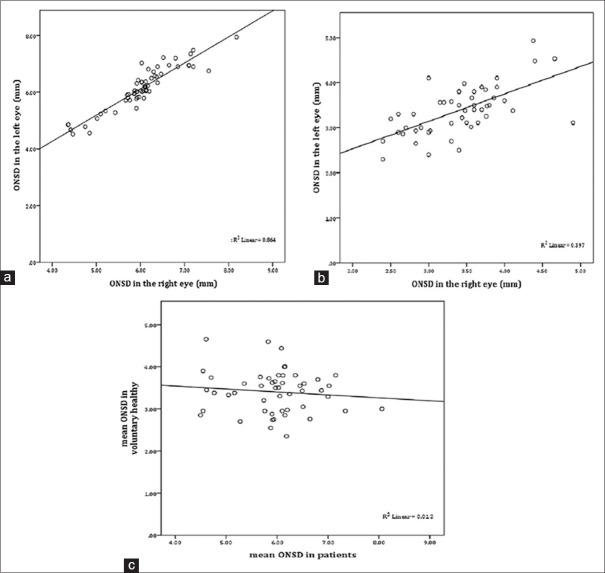
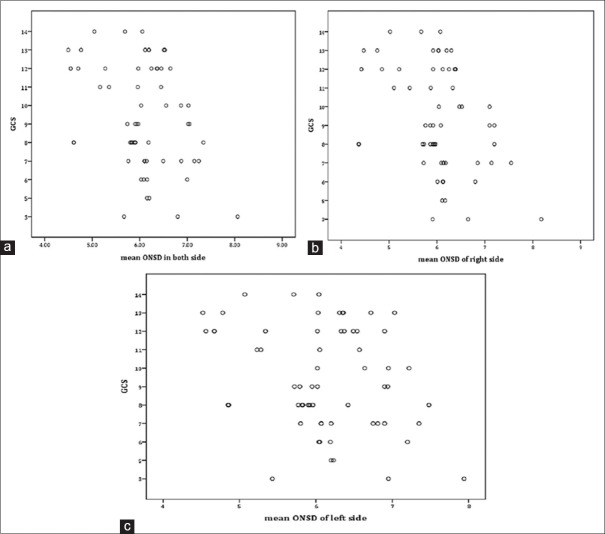
The mean ONSD measurement of the patients and voluntary healthy group was 6.01 ± 0.76 and 3.41 ± 0.56 mm in the right eye, 6.11 ± 0.75 and 3.39 ± 0.54 mm in the left eye, and 6.06 ± 0.75 and 4.02 ± 1.07 mm in both sides, respectively. Other related information is summarized in Table 1. The ONSD in the right and left sides had high and significant correlation in the patients (r = 0.929, P < 0.000) and voluntary healthy (r = 0.630, P < 0.000) group [Figure 3a and b]; however, the correlation of mean ONSD in the patients and voluntary healthy group was insignifican (r = −0.108, P = 456) [Figure 3c]. Univariate analysis showed that GCS was significantly associated with the mean ONSD (r = −347, P = 006) [Figure 4a], the right side (r = −0.382, P = 0.002), and the left side (r = −0.299, P = 0.018) among the patients [Figure 4b and c].
Table 1.
Investigating the characteristics of patients present in two groups
| Variable | Patients (n=62), n (%) | Voluntary healthy (n=50), n (%) | Total (n=112), n (%) |
|---|---|---|---|
| Sex | |||
| Male | 58 (93.5) | 28 (56) | 86 (76.8) |
| Female | 4 (6.5) | 22 (44) | 26 (23.2) |
| Age | 34.86±14.24 (19-75) | 29.82±9.8 (20-66) | 32.59±12.74 (19-75) |
| Right optic nerve diameter (mm) | 6.01±0.76 | 3.41±0.56 | 4.85±1.46 |
| Left optic nerve diameter (mm) | 6.11±0.75 | 3.39±0.54 | 4.89±1.51 |
| Mean of both side (mm) | 6.06±0.75 | 3.04±0.5 | 4.87±1.47 |
| Trauma mechanism | |||
| Driving crash | 44 (70.96) | - | 44 (70.96) |
| Fall from height | 12 (19.35) | - | 12 (19.35) |
| Stumble | 2 (3.24) | - | 2 (3.24) |
| Quarrel | 4 (6.45) | - | 4 (6.45) |
| Bleeding | |||
| Has it | 56 (90.3) | - | 56 (90.3) |
| Does not have it | 6 (9.7) | - | 6 (9.7) |
| Early symptoms | |||
| Decreased Glasgow coma | 49 (79.03) | - | 49 (79.03) |
| Focal nerve symptoms | 1 (1.61) | - | 1 (1.61) |
| Nausea and vomiting | 3 (4.84) | - | 3 (4.84) |
| Decreased Glasgow coma and focal nerve symptoms | 5 (8.05) | - | 5 (8.05) |
| Decreased Glasgow coma and nausea and vomiting | 3 (4.84) | - | 3 (4.84) |
| Decreased Glasgow coma and focal nerve symptoms and nausea and vomiting | 1 (1.61) | - | 1 (1.61) |
Figure 3.
The scatter plot of the optic nerve sheath diameter in the right and left sides in the patients and voluntary healthy groups (a and b). Correlation of mean optic nerve sheath diameter in the patients and voluntary healthy (c)
Figure 4.
Correlation of Glasgow Coma Scale and mean optic nerve sheath diameter in patients (a). Correlation of Glasgow Coma Scale and mean optic nerve sheath diameter in the right and left sides (b and c)
Fifty-six (90.3%) patients exhibited clinical signs of increased ICP based on CT scan findings. The mean ONSD of one of the patients was 6.24 ± 0.56 mm, and the ONSD in another patient (11.3%) which showed no clinical sign of increased ICP was 4.61 ± 0.09 mm [Figure 5]. The critical values of the risk mean ONSD were 5.3 mm, the sensitivity was 96.4%, and the specificity was 71.4% [Figure 6].
Figure 5.
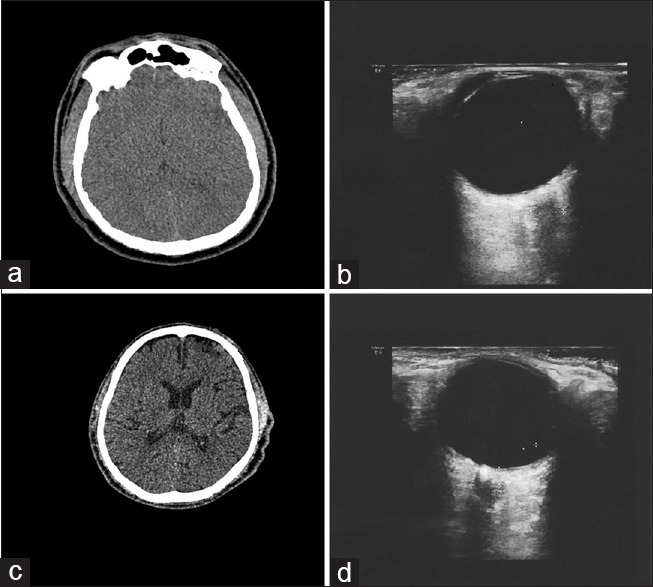
(a) Computed tomography scan showing the increased intracranial pressure (b) ultrasound showing increased diameter of optic nerve sheath in traumatic patient (optic nerve sheath diameter = 5.4 cm) (c) computed tomography scan in healthy control (d) ultrasound in healthy control (optic nerve sheath diameter = 3.4 cm)
Figure 6.
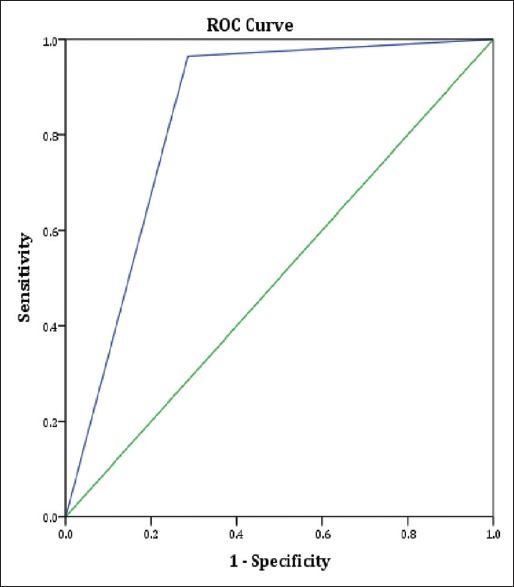
Receiver operating characteristic curve for the mean optic nerve sheath diameter. The area under the curve of 0.839 means that 83.9% of the time, a randomly selected individual who with increased intracranial pressure has a wider mean optic nerve sheath diameter than that of patients who with normal increased intracranial pressure
DISCUSSION
Although the ultrasonic method is widely employed daily for the measurement of the ONSD to detect ICP, there is no definite threshold for the diameter of the optic nerve sheath to detect an increase in ICP.[17,18] The diameter of the optic nerve sheath is measured between 4.7 and 5 mm[19,20] by ultrasound in the previous studies. The studies on cutoff point have considered the diameter of the optic nerve sheath to be 5 mm for increasing ICP.[19,21,22] However, other studies stated that a diameter >5.5 mm can predict an ICP.[23]
Most emergency doctors work in an environment, where brain CT scans are available; however, in some certain circumstances, alternative diagnostic tools, noninvasive, and reliable tools for diagnosing ICP can be helpful. One of these situations is in times of crisis. Another application of noninvasive methods of measuring the increase in ICP is the monitoring of increase in ICP during patient transmission by airway. The relationship between ONSD and ICP has been well documented. In this study, it can be seen that patients with increased cranial pressure have suffered from the increased diameter of the optic nerve sheath. The diameter of the patient's optic nerve sheath was higher than usual in comparison with the control group.[24]
Results obtained from a study in 2017 revealed that the relationship between increasing the diameter of the optic nerve sheath and increasing ICP is significant and can be used as a safe method.[25] Evidence of a case study of a patient with a severe headache, where the final diagnosis of the disease was ICP showed that the diameter of the optic nerve sheath by ultrasound was more than normal.[26] Moreover, studies on healthy volunteers showed no increase in the diameter of the optic nerve sheath.[27] Overview and ultrastructure studies have also emphasized on the accuracy and validity of this diagnosis method.[28,29,30]
GCS has long been used to assess the presence of brain lesions and GCS, and based on that, the patients are classified into three categories including mild 13–15, moderate 9–12, and severe 3.[31] In this study, there is a significant relationship between the increase in the ONSD and the GCS (P = 0.02), by decrease of GCS, the diameter of the optic nerve sheath is more dilated. In a study conducted by Soldatos et al. (2009),[15] the diameter of the optic nerve sheath and increased ICP in the patients with moderate brain injury have increased (GCS: 9–12).[32]
The critical values of the risk mean ONSD were 5.3 mm, the sensitivity was 96.4%, and the specificity was 71.4%. It indicates that the use of ultrasound in detecting increased ICP arising from trauma is a noninvasive and safe solution and has a high diagnostic power. This test, due to its ease of use, reduces the patient's chance of death by timely diagnosis. Moreover, using ultrasound, in comparison with other methods, reduces the cost of treatment for patients and the hospital.
CONCLUSIONS
Ultrasound of the optic nerve diaphragm with acceptable sensitivity can detect the increased ICP, and it is important to expedite the actions required to reduce ICP. Due to the sensitivity and specificity of the ultrasound of the optic nerve sheath diaphragm in detecting increased ICP, and since ultrasound is a noninvasive and available technique that can be performed at the patient's bedside, it is suggested that this tool should be employed in the early diagnosis of patients with increased ICP. Moreover, in patients with unstable conditions that do not allow the patients to be transferred from the emergency department, this method is employed as an alternative to CT scan and other diagnostic methods of increased ICP.
Limitations
There are some limitations in this study. We could not estimate the increased ICP by lumbar puncture (LP) because patients with suspected traumatic increased ICP may have brain hernia by performing an LP.
Financial support and sponsorship
This study was financially supported by the office of research and technology development of Ahvaz Jundishapur University of Medical Sciences under the research code U-95104.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The present research is derived from Sima Norouzi Parei's dissertation and is supported by the Office of research and technology development of Ahvaz Jundishapur University of Medical Sciences under the research code U-95104.
REFERENCES
- 1.Schwab S, Aschoff A, Spranger M, Albert F, Hacke W. The value of intracranial pressure monitoring in acute hemispheric stroke. Neurology. 1996;47:393–8. doi: 10.1212/wnl.47.2.393. [DOI] [PubMed] [Google Scholar]
- 2.Czosnyka M, Matta BF, Smielewski P, Kirkpatrick PJ, Pickard JD. Cerebral perfusion pressure in head-injured patients: A noninvasive assessment using transcranial doppler ultrasonography. J Neurosurg. 1998;88:802–8. doi: 10.3171/jns.1998.88.5.0802. [DOI] [PubMed] [Google Scholar]
- 3.Tayal VS, Neulander M, Norton HJ, Foster T, Saunders T, Blaivas M. Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med. 2007;49:508–14. doi: 10.1016/j.annemergmed.2006.06.040. [DOI] [PubMed] [Google Scholar]
- 4.Frumin E, Schlang J, Wiechmann W, Hata S, Rosen S, Anderson C, et al. Prospective analysis of single operator sonographic optic nerve sheath diameter measurement for diagnosis of elevated intracranial pressure. West J Emerg Med. 2014;15:217–20. doi: 10.5811/westjem.2013.9.16191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee LA, Sharar SR, Lam AM. Perioperative head injury management in the multiply injured trauma patient. Int Anesthesiol Clin. 2002;40:31–52. doi: 10.1097/00004311-200207000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Bajoghli M, Bajoghli F, Tayari N, Rouzbahani R. Children, CT scan and radiation. Int J Prev Med. 2010;1:220–2. [PMC free article] [PubMed] [Google Scholar]
- 7.Sarkisian AE, Khondkarian RA, Amirbekian NM, Bagdasarian NB, Khojayan RL, Oganesian YT, et al. Sonographic screening of mass casualties for abdominal and renal injuries following the 1988 armenian earthquake. J Trauma. 1991;31:247–50. [PubMed] [Google Scholar]
- 8.Hassler W, Steinmetz H, Gawlowski J. Transcranial Doppler ultrasonography in raised intracranial pressure and in intracranial circulatory arrest. J Neurosurg. 1988;68:745–51. [PubMed] [Google Scholar]
- 9.Rassam SM, Patel V, Kohner EM. The effect of experimental hypertension on retinal vascular autoregulation in humans: A mechanism for the progression of diabetic retinopathy. Exp Physiol. 1995;80:53–68. doi: 10.1113/expphysiol.1995.sp003834. [DOI] [PubMed] [Google Scholar]
- 10.Hansen HC, Helmke K. Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: Ultrasound findings during intrathecal infusion tests. J Neurosurg. 1997;87:34–40. doi: 10.3171/jns.1997.87.1.0034. [DOI] [PubMed] [Google Scholar]
- 11.Aduayi OS, Asaleye CM, Adetiloye VA, Komolafe EO, Aduayi VA. Optic nerve sonography: A noninvasive means of detecting raised intracranial pressure in a resource-limited setting. J Neurosci Rural Pract. 2015;6:563–7. doi: 10.4103/0976-3147.165347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karakitsos D, Soldatos T, Gouliamos A, Armaganidis A, Poularas J, Kalogeromitros A, et al. Transorbital sonographic monitoring of optic nerve diameter in patients with severe brain injury. Transplant Proc. 2006;38:3700–6. doi: 10.1016/j.transproceed.2006.10.185. [DOI] [PubMed] [Google Scholar]
- 13.Girisgin AS, Kalkan E, Kocak S, Cander B, Gul M, Semiz M, et al. The role of optic nerve ultrasonography in the diagnosis of elevated intracranial pressure. Emerg Med J. 2007;24:251–4. doi: 10.1136/emj.2006.040931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goel RS, Goyal NK, Dharap SB, Kumar M, Gore MA. Utility of optic nerve ultrasonography in head injury. Injury. 2008;39:519–24. doi: 10.1016/j.injury.2007.09.029. [DOI] [PubMed] [Google Scholar]
- 15.Soldatos T, Chatzimichail K, Papathanasiou M, Gouliamos A. Optic nerve sonography: A new window for the non-invasive evaluation of intracranial pressure in brain injury. Emerg Med J. 2009;26:630–4. doi: 10.1136/emj.2008.058453. [DOI] [PubMed] [Google Scholar]
- 16.Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, et al. STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies. BMJ. 2015;351:h5527. doi: 10.1136/bmj.h5527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dubourg J, Javouhey E, Geeraerts T, Messerer M, Kassai B. Ultrasonography of optic nerve sheath diameter for detection of raised intracranial pressure: A systematic review and meta-analysis. Intensive Care Med. 2011;37:1059–68. doi: 10.1007/s00134-011-2224-2. [DOI] [PubMed] [Google Scholar]
- 18.Messerer M, Berhouma M, Messerer R, Dubourg J. Interest of optic nerve sheath diameter ultrasonography in dectecting non-invasively raised intracranial pressure. Neurochirurgie. 2013;59:55–9. doi: 10.1016/j.neuchi.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 19.Guthoff R, Thijssen JM. Ultrasound in Ophthalmologic Diagnosis: A Practical Guide. Georg Thieme Verlag. 1991 [Google Scholar]
- 20.Ossoinig KC. Ophthalmic Echography. 13th ed. Dordrecht: Springer; 1993. Standardized echography of the optic nerve; pp. 3–99. [Google Scholar]
- 21.Blaivas M, Theodoro D, Sierzenski PR. Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Acad Emerg Med. 2003;10:376–81. doi: 10.1111/j.1553-2712.2003.tb01352.x. [DOI] [PubMed] [Google Scholar]
- 22.Kimberly HH, Shah S, Marill K, Noble V. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Acad Emerg Med. 2008;15:201–4. doi: 10.1111/j.1553-2712.2007.00031.x. [DOI] [PubMed] [Google Scholar]
- 23.Amini A, Kariman H, Arhami Dolatabadi A, Hatamabadi HR, Derakhshanfar H, Mansouri B, et al. Use of the sonographic diameter of optic nerve sheath to estimate intracranial pressure. Am J Emerg Med. 2013;31:236–9. doi: 10.1016/j.ajem.2012.06.025. [DOI] [PubMed] [Google Scholar]
- 24.Geeraerts T, Launey Y, Martin L, Pottecher J, Vigué B, Duranteau J, et al. Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury. Intensive Care Med. 2007;33:1704–11. doi: 10.1007/s00134-007-0797-6. [DOI] [PubMed] [Google Scholar]
- 25.Liu D, Li Z, Zhang X, Zhao L, Jia J, Sun F, et al. Assessment of intracranial pressure with ultrasonographic retrobulbar optic nerve sheath diameter measurement. BMC Neurol. 2017;17:188. doi: 10.1186/s12883-017-0964-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Williams P. Optic nerve sheath diameter as a bedside assessment for elevated intracranial pressure. Case Rep Crit Care. 2017;2017:3978934. doi: 10.1155/2017/3978934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goeres P, Zeiler FA, Unger B, Karakitsos D, Gillman LM. Ultrasound assessment of optic nerve sheath diameter in healthy volunteers. J Crit Care. 2016;31:168–71. doi: 10.1016/j.jcrc.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 28.Ohle R, McIsaac SM, Woo MY, Perry JJ. Sonography of the optic nerve sheath diameter for detection of raised intracranial pressure compared to computed tomography: A systematic review and meta-analysis. J Ultrasound Med. 2015;34:1285–94. doi: 10.7863/ultra.34.7.1285. [DOI] [PubMed] [Google Scholar]
- 29.Hylkema C. Optic nerve sheath diameter ultrasound and the diagnosis of increased intracranial pressure. Crit Care Nurs Clin North Am. 2016;28:95–9. doi: 10.1016/j.cnc.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 30.Jeon JP, Lee SU, Kim SE, Kang SH, Yang JS, Choi HJ, et al. Correlation of optic nerve sheath diameter with directly measured intracranial pressure in Korean adults using bedside ultrasonography. PLoS One. 2017;12:e0183170. doi: 10.1371/journal.pone.0183170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Komut E, Kozacı N, Sönmez BM, Yılmaz F, Komut S, Yıldırım ZN, et al. Bedside sonographic measurement of optic nerve sheath diameter as a predictor of intracranial pressure in ED. Am J Emerg Med. 2016;34:963–7. doi: 10.1016/j.ajem.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 32.Robba C, Bragazzi NL, Bertuccio A, Cardim D, Donnelly J, Sekhon M, et al. Effects of prone position and positive end-expiratory pressure on noninvasive estimators of ICP: A pilot study. J Neurosurg Anesthesiol. 2017;29:243–50. doi: 10.1097/ANA.0000000000000295. [DOI] [PubMed] [Google Scholar]