Abstract
Introduction
Antipsychotics improve symptoms associated with schizophrenia and bipolar disorder. To improve medication adherence and decrease the need for hospitalization, many antipsychotics have been developed into long-acting injectable (LAI) formulations. Though mirror-image studies have demonstrated significantly decreased hospitalization rates with LAI use, there is limited data when suboptimal use parameters are present.
Methods
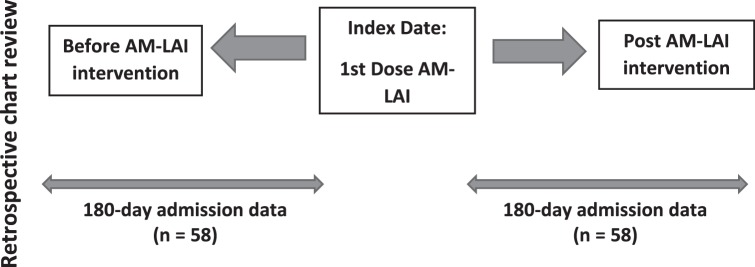
A retrospective chart review was conducted on patients who were administered aripiprazole monohydrate long-acting injectable (AM-LAI) in an adult mental health unit. Demographics and AM-LAI use parameters were analyzed descriptively. Endpoints compared the days between encounters pre and post AM-LAI administration and number of inpatient encounters between the 180 days pre and post AM-LAI administration. Effects of AM-LAI on inpatient encounters were analyzed using a Wilcoxon signed rank test with an alpha set to <0.05 for significance.
Results
Fifty-eight patients met inclusion criteria. Mean (± SD) age was 39.4 (11.4) years with 55.2% of the sample male. Most patients were diagnosed with schizophrenia or unspecified psychotic disorder and admitted involuntarily. The mean number of days from last admission to the date of initial AM-LAI administration was 109.3 (75.2), compared with 131.3 (69.8) days to next encounter (P = .044) post AM-LAI. Total inpatient encounters were also reduced (P = .004), although no differences in encounters for psychiatric reasons were detected.
Discussion
Use of AM-LAI was associated with a prolonged time to next inpatient encounter and reduced total inpatient encounters, however its use failed to demonstrate reductions in psychiatric encounters.
Keywords: long-acting, injectable, depot, antipsychotic, adherence, aripiprazole
Introduction
Patients with severe mental illness such as schizophrenia or bipolar I disorder are at increased risk for medication non-adherence for multiple reasons including cognitive deficits, poor insight, comorbid substance use, medication side effects, and lack of motivation to comply with prescribed therapies.1 Therefore, in a multifaceted sense, medication nonadherence is a major reason for illness decompensation, resulting in lower quality of life, increased hospitalization rates, and increased costs of care to the healthcare system.2 To improve medication adherence, many oral second-generation antipsychotics have long-acting injectable (LAI) antipsychotic counterparts, which are recommended primarily for patients with severe mental illness and frequent psychiatric hospital admissions secondary to nonadherence.3
Meta-analyses of available randomized trials comparing LAI antipsychotics to oral antipsychotics have failed to demonstrate superiority for symptom control or readmission rates.4,5 The lack of observed superiority may be because of detection bias, stringent selection processes that enroll high functioning patients, or the effects of increased monitoring and encouragement to remain in a trial, thus negating purported benefits on adherence associated with LAI use.4-7 Mirror-image studies have become popular for studying LAI antipsychotics because they may have higher generalizability to clinical practice.7 In a meta-analysis8 of these study types, LAIs were found to be superior to oral antipsychotics in preventing hospitalization. Mirror-image study designs have high external validity, although they are subject to increased bias and confounding relative to randomized trials. A systematic review and meta-analysis9 that included both interventional and noninterventional designs found higher reductions in hospitalization rates when LAIs were used compared with oral antipsychotics. In totality, the evidence supports LAIs reducing psychiatric hospitalizations. However, the literature is limited regarding effects of LAIs when suboptimal use parameters are present, such as short oral trial periods or use in patients with bipolar or psychotic disorders that are comorbid with substance use disorders.
While it is ideal and encouraged to follow package insert recommendations when using LAIs and selecting patients judiciously, suboptimal use patterns occur in some psychiatric settings. At the investigator's institution, suboptimal use of aripiprazole monohydrate long-acting injectable (AM-LAI) was suspected. Because of limited evidence from pre-post study designs and randomized trials investigating the use of AM-LAI when suboptimal use parameters are present, a naturalistic retrospective mirror-image study and medication use evaluation of AM-LAI was conducted. The objectives were to determine if a single injection of AM-LAI improved frequency of inpatient encounters and to collect data that could lead to quality improvement in the future if suboptimal use parameters were discovered. The objective of this study was to investigate the effect of AM-LAI on inpatient encounters.
Methods
Aripiprazole monohydrate long-acting injectable was administered in an inpatient mental health unit (MHU) within a small community hospital. The MHU has a maximum of 30 patients and an average census of 12 to 20 patients. In December 2015, AM-LAI was added to hospital formulary. A medication use report from the time of formulary addition through August 31, 2017 was used to identify AM-LAI recipients. Retrospective inpatient encounter data on psychiatric inpatients was collected up to 180 days prior to initiation of AM-LAI (index date) and compared to data 180 days after AM-LAI administration (Figure). During the time frame of interest there was no formal procedure to help ensure patients follow up with additional injections. Data regarding follow up injections was not available for this study.
FIGURE.
Mirror-image study design (AM-LAI = aripiprazole monohydrate long-acting injectable)
Persons admitted to the MHU that received the initial injection of AM-LAI were eligible for study inclusion. Patients were excluded if they were receiving a follow-up injection of AM-LAI rather than an initial injection. This retrospective chart review of existing data was determined to be exempt from review by the institutional review board.
Time of initial AM-LAI administration defined the index date, during the index hospitalization. Data collected from their index hospitalization included demographic variables, urine toxicology results, length of stay, days the patient received oral aripiprazole prior to AM-LAI, days from AM-LAI administration to discharge or verifiable oral overlap period, dose of AM-LAI administered, and whether the patient was receiving at least 10 mg of oral aripiprazole per day. Demographic variables, AM-LAI use parameters, and data from the samples' index admission were analyzed descriptively.
The primary endpoint compared the mean number of days between the MHU admission prior to the index date and the mean number of days to the next inpatient psychiatric encounter. Inpatient psychiatric encounters included either an emergency department (ED) visit for a psychiatric reason or readmission to the MHU. Secondary outcomes included the number of psychiatric or medical ED encounters and hospital or MHU admissions as well as total patient encounters within the 180 days pre- and postindex hospitalization. Total inpatient encounters combined ED visits and hospital admission for any reason. The Wilcoxon signed rank test was used to analyze primary and secondary endpoints with an alpha value set to 0.05 for significance.
Results
Fifty-eight subjects were identified who met study inclusion criteria with a mean (± SD) age of 39.4 (11.4) and range of 21 to 64 years. Most subjects were admitted involuntarily with schizophrenia or unspecified psychosis. Almost half the subjects were white (44.8%), and a large proportion identified as Latino or Hispanic (39.7%). Approximately half of the subjects had a urine toxicology or blood test that was positive for drugs or alcohol (Table 1). The most commonly detected drug in subjects' urine samples was amphetamine 32.8% (n = 19), and 25.9% (n = 15) had urine toxicology positive for at least 2 substances. The majority of prescriptions (75.9%, n = 44) for AM-LAI were written by a single psychiatrist, although 3 were servicing the MHU during the study period. Additional demographic information can be found in Table 1.
TABLE 1.
Demographics of study participants
|
Category |
N (%) |
| Sex | |
| Male | 32 (55.2) |
| Female | 26 (44.8) |
| Ethnicity | |
| White | 26 (44.8) |
| Latino/Hispanic | 23 (39.7) |
| African American/Black | 3 (5.2) |
| Asian/Pacific Islander | 3 (5.2) |
| Unspecified | 3 (5.2) |
| Voluntary status | |
| Involuntary/Placed on a hold | 39 (67.2) |
| Voluntary | 19 (32.8) |
| Primary diagnosis | |
| Schizophrenia/Unspecified psychosis | 47 (81) |
| Bipolar disorder | 9 (15.5) |
| Major depressive disorder | 2 (3.4) |
| Urine toxicology | |
| Urine toxicology positive | 27 (46.6) |
| Amphetamine | 19 (32.8) |
| Tetrahydrocannabinol (THC) | 14 (24.1) |
| Alcohol | 8 (13.8) |
| Cocaine | 1 (1.7) |
| Opiate | 1 (1.7) |
| Benzodiazepine | 1 (1.7) |
The average length of stay for the index admission was 5.6 (2.7) days. The mean trial period of oral aripiprazole prior to receiving AM-LAI was 1.8 (1.6) days, although 20.7% of the sample (n = 12) did not receive any oral aripiprazole prior to starting AM-LAI. Of those who received oral aripiprazole prior to AM-LAI (n = 46), all were taking ≥10 mg. The mean verifiable oral overlap period with aripiprazole after administration of AM-LAI was 2.4 (2.2) days. All patients received AM-LAI 400 mg.
The mean number of days between the MHU admission prior to AM-LAI administration was 109.3 (SD 75.2; 95% confidence interval [CI], 89.6 to 129.1), and the mean number of days to the next inpatient psychiatric encounter was 131.3 (SD 69.8; 95% CI, 112.9 to 149.6; P = .044). Of the subjects, 23 (39.7%) had at least 1 MHU admission in the 180 days prior to AM-LAI, compared to 17 (29.3%) in the 180 days after AM-LAI (P = .238). There was one subject who appeared to be an outlier, with 7 MHU admissions prior to AM-LAI and 8 MHU admissions after AM-LAI during the study period. Aripiprazole monohydrate long-acting injectable was associated with a reduced number of inpatient encounters including MHU admissions, ED visits for psychiatric and medical reasons, medical admissions, and total inpatient encounters. However, only ED visits for a medical reason and total inpatient encounters demonstrated statistically significant reductions (Table 2).
TABLE 2.
Inpatient encounters in 180 days before and after aripiprazole monohydrate long-acting injectable
|
Inpatient Encounter Type |
Pre: No. of Encounters |
Post: No. of Encounters |
P
Value (Wilcoxon Signed Rank) |
| Mental health unit admission | 47 | 35 | .256 |
| ED: Psychiatric Complaint | 29 | 13 | .095 |
| ED: Medical complaint | 35 | 11 | .011 |
| Medical admission | 5 | 4 | .739 |
| Total encounters | 116 | 63 | .004 |
ED = emergency department.
Discussion
Compared to previous studies8 of first and second generation LAI antipsychotics, our results are consistent with the broader literature base and demonstrated reduced total inpatient encounters for any reason. Most mirror image studies in the literature appear to have been conducted with risperidone LAI or first generation LAIs, with only a few examining effects of AM-LAI.10-12 Prior studies10,12,13 of AM-LAI have shown significant reductions in hospital bed days, improved outcomes compared to risperidone LAI or first generation LAIs in persons with bipolar disorder, and increased quality of life compared with paliperidone palmitate LAI. While the P value of our primary endpoint was <.05, the 95% CIs overlapped, suggesting there may not have been a significant difference between pre and post AM-LAI use after a single injection. Our study failed to detect significant differences in several of the secondary endpoints, including reductions in ED visits for psychiatric reasons or MHU admissions.
There are several explanations for why AM-LAI may have underperformed in this study that may collectively constitute suboptimal use parameters. Some factors that may decrease effectiveness of AM-LAI include high rates of presumed illicit drug use reflected by urine toxicology results and lack of attention to transitions of care plans for outpatient follow-up. Conversely, our study may have been underpowered to detect significant differences.
Additionally, the oral overlap period was short or even absent in some cases which could impact effectiveness or tolerability of AM-LAI and deter participants from continuing the medication. Because of its long half-life, the package insert recommends up to 2 weeks of oral aripiprazole prior to injection to establish tolerability.14 In our study participants received an average of 1.8 (1.6) days for an oral trial period, which is really only enough to rule out an allergic reaction. Furthermore, 20.7% (12) patients did not receive any oral aripiprazole prior to AM-LAI, which could put patients at risk for prolonged side effects if the medication is not tolerated. Similarly, the verifiable period of oral overlap after AM-LAI and prior to discharge was 2.4 (2.2) days, which is much shorter than the 14 days recommended by the package insert and supported by pharmacokinetic data.14,15 Another study16 with similar endpoints, design, and sample size to ours that was able to track the receipt of follow-up injections found significant reductions in psychiatric hospitalizations for subjects who remained adherent with LAIs, although it failed to find differences in nonadherent subjects. This may suggest that the suboptimal use parameters observed in our study translated into nonadherence and increased risks for further inpatient encounters.
There are many limitations to our study that deserve mention. This was a retrospective chart review at a single institution, which could introduce the possibility of bias or confounding. For example, it is possible that patients were hospitalized at other facilities without the data being recorded in our study, which could create an omission bias. There were also high rates of positive urine toxicology, which may confound effectiveness of AM-LAI or readmission rates. The time horizon of 180 days may have limited the data collected and a longer study period may have resulted in demonstrable differences, however the study time frame was constrained by the formulary addition of AM-LAI. We were unable to gather data on adherence behaviors before or after AM-LAI administration. An a priori power calculation was not conducted, thus failure to demonstrate significant improvements could be related to being underpowered to detect differences. Finally, it is assumed that failure to return to the inpatient setting represents a favorable outcome, although this may not be true.
Conclusion
Aripiprazole monohydrate long-acting injectable initiated in psychiatric inpatients demonstrated reduced total inpatient encounters, although it failed to demonstrate significant reductions in ED visits for psychiatric reasons or MHU admissions. Low sample size or suboptimal use parameters may explain these findings.
References
- 1.Zhornitsky S, Stip E. Oral versus long-acting injectable antipsychotics in the treatment of schizophrenia and special populations at risk for treatment nonadherence: a systematic review. Schizophr Res Treatment. 2012;2012(2):1–12. doi: 10.1155/2012/407171. DOI: 10.1155/2012/407171 PubMed PMID: 22966436 PubMed Central PMCID: PMC3420751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pesa JA, Muser E, Montejano LB, Smith DM, Meyers OI. Costs and resource utilization among medicaid patients with schizophrenia treated with paliperidone palmitate or oral atypical antipsychotics. Drugs Real World Outcomes. 2015;2(4):377–85. doi: 10.1007/s40801-015-0043-4. DOI: 10.1007/s40801-015-0043-4 PubMed PMID: 26689953 PubMed Central PMCID: PMC4674518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161(2 Suppl):1–56. PubMed PMID: 15000267. [PubMed] [Google Scholar]
- 4.Kishimoto T, Robenzadeh A, Leucht C, Leucht S, Watanabe K, Mimura M, et al. Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: a meta-analysis of randomized trials. Schizophr Bull. 2014;40(1):192–213. doi: 10.1093/schbul/sbs150. DOI: 10.1093/schbul/sbs150 PubMed PMID: 23256986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fusar-Poli P, Kempton MJ, Rosenheck RA. Efficacy and safety of second-generation long-acting injections in schizophrenia: a meta-analysis of randomized-controlled trials. Int Clin Psychopharmacol. 2013;28(2):57–66. doi: 10.1097/YIC.0b013e32835b091f. DOI: 10.1097/YIC.0b013e32835b091f PubMed PMID: 23165366. [DOI] [PubMed] [Google Scholar]
- 6.Kane JM, Kishimoto T, Correll CU. Assessing the comparative effectiveness of long-acting injectable vs. oral antipsychotic medications in the prevention of relapse provides a case study in comparative effectiveness research in psychiatry. J Clin Epidemiol. 2013;66(8 Suppl):S37–41. doi: 10.1016/j.jclinepi.2013.01.012. DOI: 10.1016/j.jclinepi.2013.01.012 PubMed PMID: 23849151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miyamoto S, Wolfgang Fleischhacker W. The use of long-acting injectable antipsychotics in schizophrenia. Curr Treat Options Psychiatry. 2017;4(2):117–26. doi: 10.1007/s40501-017-0115-z. DOI: 10.1007/s40501-017-0115-z PubMed PMID: 28580230 PubMed Central PMCID: PMC5432557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kishimoto T, Nitta M, Borenstein M, Kane JM, Correll CU. Long-acting injectable versus oral antipsychotics in schizophrenia: a systematic review and meta-analysis of mirror-image studies. J Clin Psychiatry. 2013;74(10):957–65. doi: 10.4088/JCP.13r08440. DOI: 10.4088/JCP.13r08440 PubMed PMID: 24229745. [DOI] [PubMed] [Google Scholar]
- 9.Lafeuille M-H, Dean J, Carter V, Duh MS, Fastenau J, Dirani R, et al. Systematic review of long-acting injectables versus oral atypical antipsychotics on hospitalization in schizophrenia. Curr Med Res Opin. 2014;30(8):1643–55. doi: 10.1185/03007995.2014.915211. DOI: 10.1185/03007995.2014.915211 PubMed PMID: 24730586. [DOI] [PubMed] [Google Scholar]
- 10.Kane JM, Zhao C, Johnson BR, Baker RA, Eramo A, McQuade RD, et al. Hospitalization rates in patients switched from oral anti-psychotics to aripiprazole once-monthly: final efficacy analysis. J Med Econ. 2015;18(2):145–54. doi: 10.3111/13696998.2014.979936. DOI: 10.3111/13696998.2014.979936 PubMed PMID: 25347448 PubMed Central PMCID: PMC4743596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sapin C, Hartry A, Kamat SA, Beillat M, Baker RA, Eramo A. Pharmacoeconomic comparison of aripiprazole once-monthly and paliperidone palmitate from a head-to-head clinical trial in schizophrenia: a US analysis. Drugs Context. 2016;5:212301. doi: 10.7573/dic.212301. DOI: 10.7573/dic.212301 PubMed PMID: 27708677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor DM, Sparshatt A, Amin F, Osborne I, Dzahini O, Hughes G, et al. Aripiprazole long-acting injection - a mirror image study of its effects on hospitalisation at one year. J Psychopharmacol. 2017;31(12):1564–9. doi: 10.1177/0269881117735686. DOI: 10.1177/0269881117735686 PubMed PMID: 29039241. [DOI] [PubMed] [Google Scholar]
- 13.Yan T, Greene M, Chang E, Touya M, Broder MS. Impact of initiating long-acting injectable antipsychotics on hospitalization in patients with bipolar I disorder. J Comp Eff Res. 2018;7(11):1083–93. doi: 10.2217/cer-2018-0068. DOI: 10.2217/cer-2018-0068 PubMed PMID: 30129771. [DOI] [PubMed] [Google Scholar]
- 14.Rockville (MD): Otsuka America Pharmaceutical, Inc; c2018. ABILIFY MAINTENA [package insert] [Google Scholar]
- 15.Raoufinia A, Baker RA, Eramo A, Nylander A-G, Landsberg W, Kostic D, et al. Initiation of aripiprazole once-monthly in patients with schizophrenia. Curr Med Res Opin. 2015;31(3):583–92. doi: 10.1185/03007995.2015.1006356. DOI: 10.1185/03007995.2015.1006356 PubMed PMID: 25586294. [DOI] [PubMed] [Google Scholar]
- 16.Heesch CB, Moore TA, Gutierrez CA, Hospitalizations Lee S. and emergency room visits after initiation of long-acting injectable antipsychotics. Ment Health Clin [Internet] 2016;6(3):134–41. doi: 10.9740/mhc.2016.05.134. DOI: 10.9740/mhc.2016.05.134 PubMed PMID: 29955461 PubMed Central PMCID: PMC6007648. [DOI] [PMC free article] [PubMed] [Google Scholar]