Abstract
The health care domain is experiencing a shift from traditional hospital-based care to care delivered in a patient’s home setting. Although home health care provides many benefits, it creates new challenges and difficulties for professional caregivers (e.g., registered nurses) who are performing complex medical tasks without the support often present in a health care environment. In addition to performing these tasks themselves, registered nurses are also responsible for training patients to perform many of these tasks, which may include using medical devices and managing complex medication regimens. The purpose of this research was to identify and systematically categorize the issues facing registered nurses (RNs) when training older adult patients. Eight RNs participated in individual structured interviews wherein they were asked to describe the difficulties and frustrations associated with training older adult patients to use medical devices and manage medication independently. The data were categorized as patient-related, RN-related, or situation-related issues. The results highlight the complexity of training device use and medication management, as well as the needs of RNs for forms of additional support in training older adult patients.
INTRODUCTION
Many older adults prefer to age in place, or remain in their own homes as they age (Gitlin, 2003). Home health care has thus become an attractive alternative to traditional hospital care, particularly for managing chronic health conditions. In 2000, approximately 955,200 of older adults (65 and older) received some form of home health care in the United States (CDC, 2004). Home health care services vary across patients and may include skilled nursing, personal care, various therapies, and psychosocial support.
Skilled nursing services are provided to approximately 75% of older adult home health care recipients (CDC, 2004) and are typically provided by registered nurses (RNs). Two of the most commonly performed skilled nursing tasks include training patients to use various medical technologies and teaching patients how to manage their medication. Approximately 211,700 older adults (aged 65 and over) receive help with using medical devices, and 183,500 receive assistance with taking medications (CDC, 2004).
Given that home health care is typically a temporary form of assistance, training patients how to perform tasks correctly themselves is essential to support their independence and safety. For example, research has demonstrated that training can successfully address the physical limitations faced by many older adults, particularly for bathing and toileting (Gitlin et al., 2006). However, training in a home health setting may be particularly challenging for certain tasks, such as using medical devices and managing medication (McBride, Beer, Mitzner, & Rogers, 2011).
A report from the U.S. Food and Drug Administration (FDA) has also suggested that training patients to perform healthcare tasks can be challenging. Regarding training patients to use medical devices, the report stated that, “a major problem with the current system is that the education and training of homecare users is woefully deficient” (FDA, 2002, p. 5). The report also states that, “…the consequences of error with medical devices are much higher than with consumer devices, since errors with some devices might even result in a patient’s death” (FDA, 2002, p. 9).
Previous human factors research has identified the importance of training, even for “walk-up-and-use” medical devices, such as automated external defibrillators (Mitchell, Gugerty, & Muth, 2008). Indeed, training individuals to use assistive devices can result in improved overall functioning (Chiu & Man, 2004). However, all training is not created equal. Training older adults to use medical devices may be especially challenging for a number of reasons. Previous research on training computer skills found that older adults make more errors, require more time to attain basic skills, and need more assistance during training than their younger counterparts (Kelley & Charness, 1995). Additionally, older adults may require certain training formats to reap the benefit of training, whereas younger adults are less influenced by this factor (Mykityshyn, Fisk, & Rogers, 2002).
Regarding the complexity of medication management, a recent report estimated that approximately 36.7% of adults (aged 60 and over) are taking five or more medications (Department of Health and Human Services, 2010). Factoring in the varying dosages and schedules of these numerous medications, it becomes clear why proper adherence is difficult. Yet, the cost of improper adherence can be quite serious; one study discovered that as many as 28% of hospital admissions among older adults were drug related (Col, Fanale, & Kronholm, 1990).
Training older adults to manage their medications may require that the health care provider should be aware of and adjust the training to accommodate age-related changes in cognition. For example, declines in prospective memory, or remembering to do something in the future (such as take medication), are common and can even occur for habitual tasks (Boron, Rogers, & Fisk, 2006).
The consequences of improper device use and poor medication adherence can be life-threatening. The goal of this study was to investigate the challenges faced by RNs when training older patients to use medical devices and manage medication independently. The findings will be discussed within the framework of potential human factors interventions that may aid RNs in training patients to perform these tasks more proficiently.
METHOD
Participants
We interviewed eight RNs recruited from local home health care agencies. The RNs had at least two years experience in the home health care industry, and experience working with older adult patients. Participants were between the ages of 37 and 69 (M=47.25, SE=4.55), worked full-time, and had an Associate’s degree or higher. Participants were provided with monetary compensation for their participation.
Procedure
The one-on-one structured interviews took place either in person or over the telephone and lasted a maximum of three hours. Prior to the structured interview, participants completed questionnaires that documented demographic and background information, including education, training, and employment history.
During the interview, participants were asked to discuss how they train older adult patients on a variety of tasks, including using devices (e.g., medical technologies and durable medical equipment), and medication management. For each task, they gave detailed descriptions of their process for training as well as discussed what frustrations and difficulties were commonly encountered during training.
RESULTS
The interviews were transcribed verbatim. For each task, the researchers identified trends in participant utterances and organized those trends into categories representing issues related to training. These categories included patient-, RN-, and situation-related issues.
Device Use
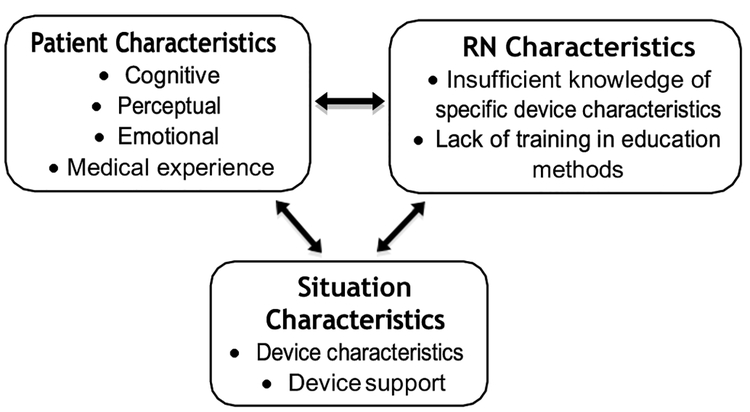
Medical technologies and durable medical equipment are necessary for managing many health conditions. For example, testing one’s blood sugar level is a critical aspect of managing diabetes. However, the RNs we interviewed reported several challenges that impeded their ability to successfully train older adult patients to use medical devices (see Figure 1).
Figure 1.
Issues related to training device use.
Patient characteristics.
Several RNs indicated that the characteristics of the person being trained were a critical factor in the training approach used. They stated that they used a different approach depending upon the patient’s capabilities and limitations, including the patient’s cognitive status. RNs reported that memory impairments often made training to usea device problematic. As one solution to this problem, the RNs left materials such as step-by-step instructions to which patients could refer later. RNs reported that they often had to develop such training materials because they were not available.
RNs stated that changes in older adults’ perceptual capabilities, such as vision, also had a negative impact on their ability to perform the task without assistance. For example, one RN discussed that a patient could not read the message displayed on his/her infusion pump. RNs discussed emotional barriers to training, as well. They stated that a patient’s fear or anxiety surrounding use of the device in question hindered learning at times. Using a walker was reported as being frightening for many older patients who have mobility impairments. RNs reported that providing encouragement and making the patient feel confident were important aspects of overcoming fear and anxiety; “It’s just making them feel like they’re comfortable and confident enough to perform it without any assistance,” commented one participant.
RNs reported that a patient’s previous medical experience or knowledge also influenced their training approach. As one RN stated, “…my biggest frustration would be dealing with people who are non-medical natured who have no medical background and you’re trying to instruct them and they just don’t get it.” However, because this is likely to be the case with a majority of patients, identifying ways to bridge the gap and make a medical background less of a requirement will be a critical step to improve training.
RN characteristics.
RNs were asked how they developed their process of teaching or instruction. The majority indicated that learning how to train patients was not part of their formal education, and more commonly was something they had to figure out on their own. As one RN responded, “That’s just something I came up with, that’s just me.”
In some cases, RNs stated that when teaching a patient to use a device for the first time, their strategy was to provide the same form of instruction they received when they were taught how to use a device, either in school or elsewhere. As stated by one RN, “It’s just the education that I received.” Considering how divergent the experience and domain knowledge an RN and an older adult patient are likely to have, using the same strategy to train both is unlikely to be the most effective approach.
Situation characteristics.
Many medical devices used in home health care are supplied by the health care recipient, rather than the health care provider or home health agency. These devices might range from smaller electronics such as blood glucose meters or electronic blood pressure cuffs, to larger devices such as Power Chairs, Hoyer lifts, and adjustable hospital-like beds.
In many cases, the manufacturer or company delivering the device is responsible for training patients on proper use of the device. However, the RN assigned to the patient may or may not be present for this training. This limits an RN’s ability to provide additional support to the patient when it is needed. On the other hand, RNs may believe they have the requisite understanding to provide training for the device. As one RN stated, “…it falls on the nursing staff to educate them further on what it is that they do not fully understand.” However, if RNs misjudge their own level of understanding, they may inadvertently teach patients incorrectly.
Compounding this problem is the variety of devices that the health care provider must use. Given that devices are supplied by the patient, for each different home that RNs service, they may have to use a different model or version of a device. Having to train on different devices is challenging because standardization in the design between devices is lacking. Moreover, devices are often outdated and training materials may not be available. RNs reported having to take the time to learn various makes and models of different devices, such blood glucose meters (maybe via instruction manual), before being able to train the patient. Not only does self-training for many different devices take time, it can increase the chance of errors as well.
Infusion pump.
As a testament to why training is such a critical component of what RNs do as part of their care giving duties, let us consider one task in particular. One of the most difficult devices for patients to use is an intravenous (IV) infusion pump. RNs were asked to estimate, on a scale from 1 to 5 (where one is not challenging at all and five is extremely challenging), how challenging using an infusion pump is for an older adult patient or informal caregiver. Of the four RNs that had trained patients to use that particular device, all of them responded with a four or higher. As one RN reported, “IV tubing at home…you always have some problems with that…most of the time these people are medical limited so they have no idea, so it takes a while and then it’s trial and error for them just like it is for us, so it’s always going to be some difficulties with that.” This quote reflects the complexity of using an infusion pump, as it is a device that both the RN and the patient encounter problems with.
Some of the challenges RNs reported older patients have with using the infusion pump included ensuring that all of the air was removed from the tubing before connecting it to the IV site. A mistake at this step could result in a venous air embolism, which can be life-threatening. An additional challenge that patients reportedly encountered is interpreting the infusion pump’s text and auditory messages. These messages typically alert the user to a dangerous state, but are often difficult for the patient to interpret and do not provide enough information to determine the appropriate course of action.
Medication Management
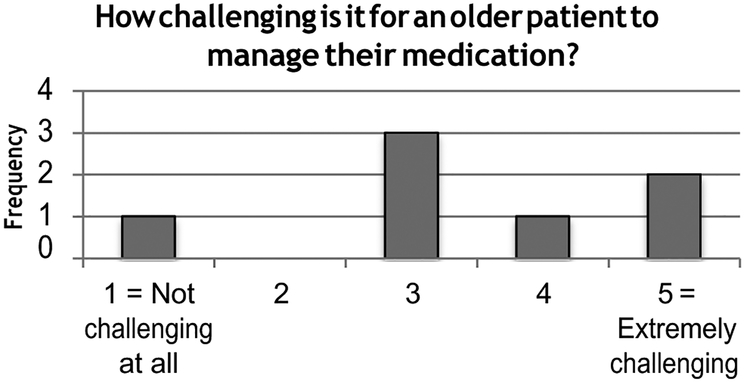
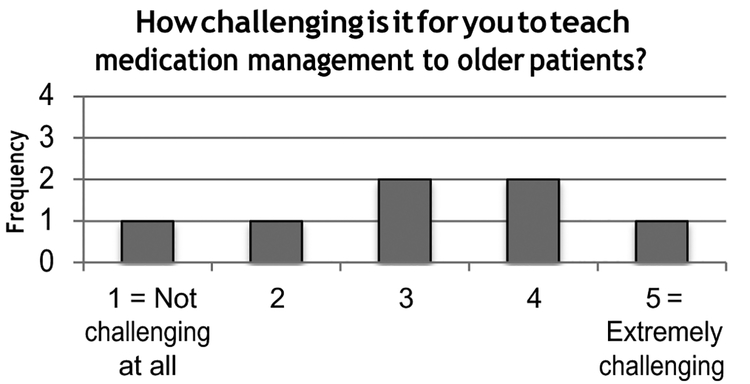
Training patients how to manage their medications is another critical aspect of the tasks performed by RNs in the home health setting. Unfortunately, it is also one of the most difficult tasks. As one RN stated, “Management in medication is probably one of our major issues in home health.” RNs were asked to estimate, using a 1 to 5 scale, how challenging medication management is for an older adult patient, as well as how challenging it is to teach medication management to an older patient (see Figures 2 and 3).
Figure 2.
Frequency of ratings describing the difficulty older adults have managing medication as perceived by RNs. Note that one RN did not provide a rating.
Figure 3.
Frequency of ratings describing the difficulty older adults have managing medication as perceived by RNs. Note that one RN did not provide a rating.
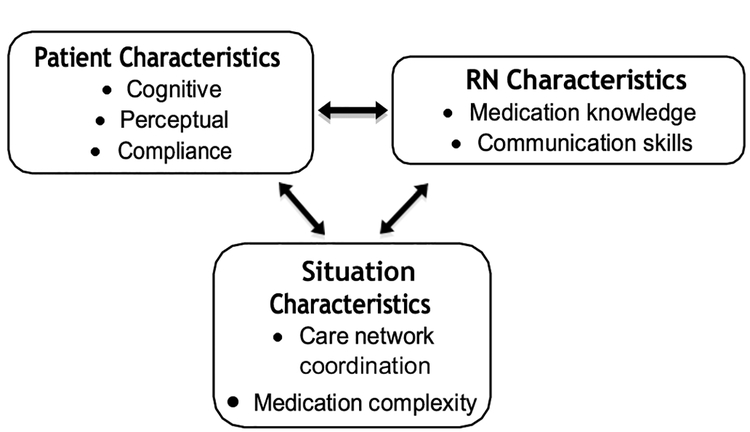
For both questions, the majority responded with a three or higher, with several RNs rating the tasks as “extremely challenging”. The challenges associated with training patients to manage medications are depicted in Figure 4, and are subdivided into patient, provider, and situational-related issues.
Figure 4.
Issues related to training medication management.
Patient characteristics.
RNs reported a variety of factors associated with older patients that influence the success of teaching them to manage their medication. From a cognitive perspective, many training challenges stemmed from a lack of comprehension surrounding the medication. This includes understanding all the critical information associated with a particular medication, such as the purpose of the medication, possible side effects, dosing schedule (e.g., twice a day), and dosing instructions (e.g., with food). RNs commented that being able to convey this information along with the importance of the medication regimen was a critical aspect of increasing compliance and adherence.
However, RNs also reported that many older adult patients failed to understand the importance of adhering to the dosing schedule and instructions, and assumed that they could take the medicine “as needed”. As one RN noted, “If they are having a good day or good week they won’t take the medicine, they will only take it when they are feeling bad.” Another issue pertained to patients’ consuming expired medications, rather than disposing of them at the appropriate time. RNs also reported that patients have issues with the memory component of medication management. However, the majority of RNs discussed how some patients’ use of pill boxes or pill planners often helps to alleviate this issue.
From a sensory perspective, RNs reported that even if patients are compliant and do not have memory issues, medication management can still be troublesome due to age-related changes in vision and motor control. For example, older patients may have difficulty reading the text on pill bottles or medication information sheets. Additionally, opening medication bottles and handling small pills can also pose a challenge.
RN characteristics.
One of the primary challenges faced by the RNs is understanding the tens of thousands of prescription medications that are on the market. The precursor to explaining a medication to a patient involves the RNs researching the medication themselves. As one RN discussed, “Yes, medications are really, really a problem and can be really challenging if you don’t know your medications. So your best thing to do is to either walk with your med book, so that you can know what your patients are on…But in a way you’re not sure for the first time, you always need to go to a source, you need to have a resource.”
Once the RNs have familiarized themselves with the medication, the next step is communicating this information to the patient. Because the medication information is often written with medical terminology that can be incomprehensible to a patient, the provider is tasked with “translating” this information to make it accessible and understandable to the patient. One RN described the process of adjusting her explanation to suit the patient as, “…it needs to be in terminology that is basic. A lot of times these print outs, they are addressing patients with a higher education level, so again it’s kind of like when you were back in school and your instructor said, ok…write a paper on a topic and address the appropriate audience.”
Situation characteristics.
The primary challenge faced during training patients to manage their medication was the lack of communication within the patients’ care network. Many patients receive care from multiple doctors and specialists, however the RNs reported that there is little or no communication between these various healthcare providers. Consequently, patients were receiving prescriptions for the same conditions from multiple doctors, with neither the doctors nor the patient aware of this overlap. Further complicating the matter is the fact that a pharmacy specialist who would likely identify and correct overlaps in prescriptions was often circumvented because patients were using multiple pharmacies. This problem was repeatedly discussed by the RNs, such as, “…you get to a patient’s home and you find out that they’ve been seeing four different doctors and none of the doctors know what each of the other doctors and prescribing and you have 50 different prescriptions and four of them are for the same thing and that’s probably one of the biggest problems that we face with medication management… consolidating and reconciling their medications.”
DISCUSSION
Receiving health care in one’s own home is a valued option for many older adult patients. Unfortunately, it often results in new, and possibly unanticipated, challenges to the successful delivery of care. Some of these difficulties appear during the process of training older adult patients to complete certain tasks independently, such as using medical devices and managing medication. Such barriers may impede patients’ ability to safely and correctly perform tasks once the professional caregivers are no longer present, creating an opportunity for life-threatening errors.
Our analysis identified numerous challenges faced when training older patients to use medical devices and manage medications. These issues were grouped into three categories; 1) patient-related, 2) provider-related, or 3) situation-related. Some of the commonly discussed challenges relating to training for devices included the cognitive, sensory, and emotional demands placed on older adult patients. The RNs also indicated that they received little to no education on how to train patients to use devices. The RNs reportedly struggled with training device use because they did not have knowledge or access to training materials for each particular make and model of the devices that are on the market.
With regard to training medication management, a primary obstacle was the complexity of the medication information, not only for patients to understand but also for RNs to try to communicate in a simple and effective manner. In addition, there appears to be a serious issue with coordination across multiple health care providers in a patient’s care network. This resulted in multiple prescriptions for the same medications from different health care providers. RNs were required to reconcile the various medications while training patients to understand why the situation was inappropriate and how to better organize and handle their various medications.
This analysis of training challenges faced by RNs in a home health care context highlights several opportunities for human factors interventions. First, health care providers who engage in training should receive formal education regarding effective teaching methods, particularly for training older adults. Due to the diversity of older adult capabilities, limitations, and disease states, a central component of this training should be how to select an appropriate and effective training approach based on patient characteristics. Giving RNs a greater number of training tools and resources to use with patients would also be beneficial.
Changes in device design should be made such that their use is fundamentally easier for novices and more consistent across brands and models. When this is not an option, support materials should be easily accessible and comprehensible. Improved communication and coordination between health care providers will help to eliminate errors in medication prescriptions that complicate medication management. Such improvements will increase the effectiveness and safety with which home health care can be delivered.
ACKNOWLEDGMENTS
This research was supported in part by a grant from the National Institutes of Health (National Institute on Aging) Grant P01 AG17211 under the auspices of the Center for Research and Education on Aging and Technology Enhancement (CREATE; http://www.createcenter.org).
REFERENCES
- Boron JB, Rogers WA, & Fisk AD (2006). Medication adherence strategies in older adults In Proceedings of the Human Factors and Ergonomics Society 50th Annual Meeting (pp. 170–175). Santa Monica, CA: Human Factors and Ergonomics Society. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) (2004). Current home health care patients Retrieved from http://www.cdc.gov/nchs/data/nhhcsd/curhomecare00.pdf
- Chiu C, & Man D (2004). The effect of training older adults with stroke to use home-based assistive devices. OTJR: Occupation, Participation and Health, 24(3), 113–120. [Google Scholar]
- Col N, Fanale JE, & Kronholm P (1990). The role of medication non-compliance and adverse drug reactions in hospitalizations in the elderly. Archives of Internal Medicine, 150, 841–845. [PubMed] [Google Scholar]
- Department of Health and Human Services (2010). Prescription drug use continues to increase: U.S. prescription drug data for 2007–2008. Retrieved from http://www.cdc.gov/nchs/data/databriefs/db42.pdf
- Gitlin L (2003). Conducting research on home environments: Lessons learned and new directions. The Gerontologist, 43(5), 628–637. [DOI] [PubMed] [Google Scholar]
- Gitlin L, Winter L, Dennis M, Corcoran M, Schinfeld S, & Hauck W (2006). A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. Journal of the American Geriatrics Society, 54(5), 809–816. doi: 10.1111/j.1532-5415.2006.00703.x [DOI] [PubMed] [Google Scholar]
- Kelley CL, & Charness N (1995). Issues in training older adults to use computers. Behaviour and Information Technology, 14(2), 107–120. [Google Scholar]
- McBride SE, Beer JM, Mitzner TL, & Rogers WA (2011). Challenges for home health care providers: A needs assessment. Physical & Occupational Therapy in Geriatrics, 29(1), 5–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell K, Gugerty L, & Muth E (2008). Effects of brief training on use of automated external defibrillators by people without medical expertise. Human Factors, 50(2), 301–310. [DOI] [PubMed] [Google Scholar]
- Mykityshyn AL, Fisk AD, & Rogers WA (2002). Learning to use a home medical device: Mediating age-related differences with training. Human Factors, 44(3), 354–364. [DOI] [PubMed] [Google Scholar]
- U.S. Food and Drug Administration (FDA) (2002). Report on home use medical device meetings. Retrieved from http://www.fda.gov/cdrh/meetings/FDLI-home.html#b
- U.S. Census Bureau (2009). International database of population estimates and projects. Retrieved from http://www.census.gov/ipc/www/idb/informationGateway.php