Abstract
Introduction:
Appropriate prehospital (PH) triage of patients with chest pain can significantly improve outcomes in acute myocardial infarction (MI). We sought to explore how PH providers triage chest pain as high versus low risk and to evaluate the accuracy and predictors of their triage decision.
Methods:
This was a prospective, observational cohort study that enrolled consecutive patients with chest pain transported by emergency medical services (EMS) to 3 tertiary care hospitals in the US. EMS triage decision (high risk versus low-risk) was defined based on the transmission of PH electrocardiogram (ECG) to a command center for medical consultation with or without catheter laboratory activation. Two independent reviewers examined in-hospital medical records to adjudicate the presence of acute MI and to audit the findings on the presenting ECG.
Results:
We enrolled 2,065 patients (aged 56 ± 17, 53% male) of whom 768 (37%) were triaged as high risk. Those triaged as high risk were older, were more likely to be men or have significant cardiac history, and had a higher rate of acute MI events(14.2% versus 3.5%). The sensitivity and specificity for triaging MI events as high risk were 70% and 97%, respectively. A total of 46/155 (30%) MI events were misclassified as low risk. No previous coronary revascularization and ECG misinterpretation were strong independent predictors of such undertriage.
Conclusions:
PH providers have moderate sensitivity in triaging high-risk patients; 1 in 3 MI events are undertriaged. Emergency nurses need to pay special attention to patients with benign past histories during transition of care and should always reinterpret ECGs for subtle ischemic changes.
Keywords: Chest pain, Prehospital, Triage, Electrocardiogram
Early diagnosis and treatment are associated with reduced morbidity and mortality in patients with acute myocardial infarction (MI).1–3 The priority of emergency medical service (EMS) providers during the initial encounter is to identify patients with high-risk chest pain who are at increased risk for acute MI. EMS providers are trained to risk stratify chest pain based on focused history and physical exam and a quick interpretation of a prehospital (PH) 12-lead electrocardiogram (ECG) (acute ischemsia, arrhythmia, etc). If the patient is deemed to be at high risk for acute MI, EMS providers typically transmit the PH-ECG to the receiving hospital and consult with a command physician. Early activation of the catheterization laboratory based on the PH-ECG has been shown to significantly reduce door-to-balloon time (DBT) by more than 50 minutes and in-hospital mortality by nearly 40%.4–8
EMS providers rely on their personal skills and the automated machine annotations in their interpretation of the PH-ECG. However, previous studies have shown that EMS providers tend to have lower sensitivity (0.63 to 0.95) and specificity (0.72 to 0.94),9 and automated ECG interpretation algorithms tend to have lower sensitivity.10 Although systematic over-reading of PH-ECGs by a medical command physician could overcome these shortcomings,11 it has not been widely implemented by EMS systems because of excessive cost and the lack of around-the-clock access to specialized physicians.8 Therefore, EMS providers remain the gatekeeper for risk stratifying chest pain and identifying high-risk patients. As such, regional variations in successful transmission of PH-ECGs exist because there is a high degree of provider subjectivity of what constitutes a “highly suspicious” presentation. The aims of this study are to explore the demographic and clinical characteristics of patients with chest pain deemed by EMS as high-risk cases, evaluate the accuracy of initial EMS triage in relation to the eventual diagnosis of acute MI, and explore the factors associated with misclassifying (or undertriaging) a patient with MI as low risk.
Methods
SAMPLE AND SETTINGS
Subjects for this study were recruited from ECG Methods for the Prompt Identification of Coronary Events (EMPIRE). The methods of EMPIRE have been reported in detail elsewhere.12 Briefly, EMPIRE prospectively enrolled consecutive patients with nontraumatic chest pain transported by EMS to 1 of 3 University of Pittsburgh Medical Center (UPMC)-affiliated tertiary care hospitals with percutaneous coronary intervention (PCI) capabilities between May 2013 and August 2014 (n = 2,065). Consecutively enrolled patients met the following criteria: (1) 18 years of age or older and (2) chief complaint of nontraumatic chest pain or the equivalent. We enrolled all consecutive eligible patients, and there were no modifications to routine medical care. The Institutional Review Board of the University of Pittsburgh approved this study with a waiver of the requirement of informed consent.
Enrolled patients were attended, treated, and transported by the City of Pittsburgh Bureau of EMS. All Pittsburgh EMS providers are certified paramedics. As part of routine medical care, paramedics obtained 10-second, 12-lead ECGs on the scene in all patients with chest pain and administered standard medical care based on advanced cardiac life support (ACLS) algorithms or as prescribed by statewide EMS protocols. If the initial patient evaluation was judged to be highly suspicious for cardiac ischemia, EMS providers were instructed to transmit the PH-ECG to UPMC medical command center (MCC) for over-reading and possible activation of the catheterization laboratory; otherwise, transmission was not required. Paramedics were expected to interpret the ECG for significant ST elevation and were required to transmit ECGs with suspected ST-elevation myocardial infarction (STEMI) to UPMC-MCC. Transmitted ECGs are permanently stored in raw digital format in a secured UPMC network. If the patients are judged to be low risk, and hence their PH-ECGs are not transmitted, they get erased from the memory of the EMS monitor over time, and the only remaining interpretation of the PH-ECG is the documentation signed by EMS providers in electronic medical record.
DATA COLLECTION
Subjects meeting the study criteria were identified using custom reporting software in the PH electronic patient care record program (emsCharts, Warrendale, PA). We used a linkage list containing name, date of birth, sex, date/time of dispatch, and responding EMS agency to link PH records with in-hospital records from the receiving hospitals (PowerChart, Cerner Corporation, North Kansas City, MO). We obtained the initial ECG from the emergency department (ED-ECG) for all eligible patients as well as the PH-ECGs that were transmitted to the UPMC MCC.
STUDY VARIABLES
There were 2 primary outcomes. The first study outcome was EMS triage level of chest pain coded as (1) high-risk for acute MI (PH-ECG transmitted to UPMC-MCC and/or declared by EMS as STEMI-candidate) and (2) low-risk for acute MI (EMS followed routine care). The second outcome was acute MI at the primary admission, documented by elevation of cardiac troponin (> 99th percentile) and (1) subsequent development of labile, ischemic ECG changes (eg, ST deviation); (2) coronary angiography demonstrating greater than 70% stenosis, with or without treatment; and/or (3) functional cardiac evaluation (ie, stress testing) that demonstrates ECG, echo-cardiographic, or radionuclide evidence of focal cardiac ischemia.13 The presenting ECG (PH or emergency department) was coded as follows: (1) normal ST-T waveform or(2) acute ischemic ECG changes warranting further attention, defined as 2 contiguous leads with ST elevation or horizontal/down-sloping ST depression, left ventricular hypertrophy (LVH) with strain pattern, left bundle branch block (LBBB), or abnormal ventricular rhythm.13 Two independent reviewers evaluated patient records to adjudicate the study outcomes. All disagreements were resolved by a third reviewer.
There were multiple study predictors. The primary predictor was EMS providers’ interpretation of the PH-ECG as documented in emsCharts, coded as acute ischemia (ie, significant ST changes), abnormal ECG (pacing, bundle branch block, arrhythmia, etc), benign ECG (sinus tachycardia, PVC, etc), or no documentation (failure to document, ECG was not performed, etc). Of note, the EMS providers’ interpretation of the PH-ECG was based on their personal skills, assisted by the annotations printed on ECG papers by the device software (eg, “****Acute Ischemia****”). Other predictors included age, sex, past medical history, and vital signs.
STATISTICAL ANALYSIS
Values were reported as mean ± standard deviation (SD) for continuous variables or n (%) for categorical variables. Patients were grouped according to their status of PH triage (high risk/low risk) or the presence of acute MI (yes/no). Groups were compared using independent sample Students’ t-test for continuous variables (or Mann–Whitney if non-normally distributed), and chi-square for categorical variables. The sensitivity, specificity, and positive (PPV) and negative predictive values (NPV) of the accuracy of EMS triage were computed. Finally, in patients with acute MI, predictors of undertriage significant at the univariate level (P < 0.05) were entered in a multivariate logistic regression model with backward selection method. All analyses were done using SPSS 22 (IBM, Armonk, NY) with alpha of 0.05 for 2-tailed hypothesis testing.
Results
We enrolled 2,065 patients (age 56 ± 17; 53% male). Table 1 summarizes the demographic and clinical characteristics of the study sample. Overall, 768 patients (37%) were triaged by EMS providers as high risk for acute MI. Compared with those triaged as low risk, patients triaged as high risk were older, of male sex, and had histories of coronary risk factors (hypertension, diabetes mellitus, known coronary artery disease [CAD], previous MI, or previous PCI/coronary artery bypass graft [CABG]). More importantly, of the 155 patients (7.5%) diagnosed with acute MI during the primary admission, 109 were triaged as high risk, and 46 were triaged as low risk (14.2% versus 3.5%, odds ratio [OR] = 3.4 [95% confidence interval (CI) 2.4–4.8], P < 0.001). The sensitivity, specificity, PPV, and NPV of EMS triage level for identifying acute MI cases were 70%, 97%, 14%, and 86%, respectively.
TABLE 1.
Demographic and clinical characteristics in study sample
| Clinical Characteristics | All patients (N = 2,065) | EMS Triage Level | |
|---|---|---|---|
| High risk for acute MI (n = 768) | Low risk for acute MI (n = 1,297) | ||
| Age (years) | 56 ± 17 | 59 ± 17‡ | 55 ± 17 |
| Male Sex | 975 (47%) | 443 (58%)‡ | 647 (50%) |
| Past Medical History | |||
| Hypertension | 1039 (50%) | 553 (720/0)‡ | 486 (38%) |
| Diabetes mellitus | 368 (18%) | 156 (20%)* | 212 (16%) |
| Known CAD | 465 (23%) | 305 (40%)‡ | 160 (12%) |
| Previous MI | 297 (14%) | 154 (20%)‡ | 143 (11%) |
| Prior PCI/CABG | 360 (17%) | 364 (34%)‡ | 96 (7%) |
| Clinical Presentation | |||
| Heart rate | 91 ± 26 | 90 ± 30 | 91 ± 22 |
| Respiratory rate | 18 ± 3 | 18 ± 4 | 18 ± 3 |
| Systolic blood pressure | 144 ± 31 | 146 ± 33† | 142 ± 30 |
| Diastolic blood pressure | 86 ± 18 | 87 ± 20 | 85 ± 17 |
| Oxygen saturation | 98 ± 5 | 97 ± 7 | 98 ± 4 |
| Atypical symptoms | 575 (28%) | 215 (28%) | 360 (28%) |
| EMS Interpretation of PH-ECG | |||
| No documentation | 515 (25%) | 154 (20%) | 361 (28%) |
| Benign ECG findings | 1027 (50%) | 385 (50%) | 642 (50%) |
| Abnormal ECG | 479 (23%) | 192 (25%) | 287 (22%) |
| Acute ischemia | 44 (2%) | 37 (4.8%)‡ | 7 (0.5%) |
| PH treatment given en route | |||
| Nitroglycerin | 721 (35%) | 408 (53%)‡ | 313 (24%) |
| Aspirin | 1024 (50%) | 601 (78%)‡ | 423 (33%) |
| Morphine | 113 (5.5%) | 112 (15%)‡ | 1 (0.1%) |
| Final diagnosis of acute MI | 155 (7.5%) | 109 (14.2%)† | 46 (3.5%) |
Values are mean ± standard deviation (SD) or n (%). Percentages are based on total numbers in each column. Bold indicates significant difference between groups. CABG, coronary artery bypass graft; CAD, coronary artery disease; MI, myocardial infarction; PCI, percutaneous coronary intervention; PH, prehospital.
P < 0.05.
P < 0.01.
P < 0.001.
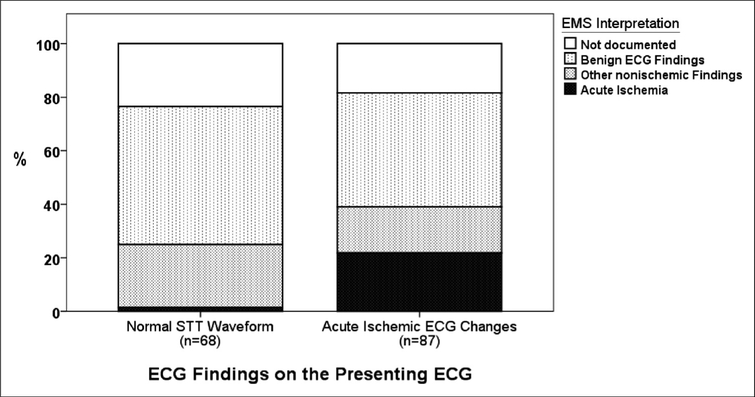
Figure 1 shows the EMS accuracy of ECG interpretation in patients with acute MI (n = 155). Overall, 87 patients with MI (56%) had acute ischemic ECG changes, and 68 (44%) had normal ST-T waveform on the presenting ECG. Among those with evidenced acute ischemic ECG changes, EMS accurately identified only 20% of these changes and documented nearly half as benign findings. The latter group was classified as ECG misinterpretation in subsequent regression models.
FIGURE 1.
EMS providers’ accuracy of ECG interpretation.
PREDICTORS OF UNDERTRIAGE IN PATIENTS WITH MI
Overall, 46 of the 155 MI events (30%) were undertriaged by EMS providers as low risk. Table 2 shows the univariate and multivariate predictors of such misclassification. At the univariate level, lack of past medical history of hypertension, diabetes, CAD, or previous revascularization, as well as ECG misinterpretation, were significant predictors of undertriage. EMS providers were more likely to misclassify an MI event as low risk if the patient had no past history of coronary revascularization (OR = 7.5 [95% CI 2.1–26.1], P = 0.002) or if their interpretation of the PH-ECG was inaccurate (OR = 2.9 [1.2–6.8], P = 0.018). Patient age, gender, and initial vital signs had no role in leading to undertriage in the context of MI.
TABLE 2.
Predictors of undertriage in patients with acute MI (n = 155)
| Predictor | Univariate P value | Multivariate P value | ||
|---|---|---|---|---|
| B | P value | B | P value | |
| Age in years | - | NS | - | - |
| Female Sex | - | NS | - | - |
| No history of HTN | 1.04 | <0.01 | 0.59 | NS |
| No history of DM | 0.99 | 0.058 | - | - |
| No history of CAD | 1.40 | <0.01 | 0.19 | NS |
| No history of previous MI | - | NS | - | - |
| No history of PCI/CABG | 1.77 | <0.01 | 2.01 | 0.002 |
| ECG misinterpretation | 0.97 | 0.02 | 1.05 | 0.018 |
| Initial heart rate (per bpm) | - | NS | - | - |
| Initial respiratory rate | - | NS | - | - |
| Initial systolic blood pressure | - | NS | - | - |
Bold indicates statistical significance.
CABG, coronary artery bypass graft; CAD, coronary artery disease; DM, diabetes mellitus; HTN, hypertension; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Discussion
This study explored the factors associated with proper PH triage of patients with chest pain. We found that EMS providers triaged one third of patients as high risk. EMS providers were more likely to triage those with older age, male sex, and significant cardiac history as high risk. Those triaged as high risk were 3 times more likely to have acute MI, yielding an acceptable sensitivity, specificity, and NPV (>70%) but poor PPV (14%). We also found that approximately 30% of MI events were misclassified as low risk. Lack of significant coronary history and ECG misinterpretation were the strongest predictors of undertriage by EMS providers. Of note, nearly 40% of the acute ischemic ECG changes seen in patients with acute MI were misinterpreted as benign by the EMS providers.
TRIAGE BASED ON PATIENT HISTORY
EMS providers rely heavily on patient history and vital signs to quickly triage patients with chest pain in the field. Using the classical patient profile (male patients with risk factors known to be associated with acute MI), EMS providers properly triaged 70% of MI events in this cohort. This is not surprising, given that patient demographics, significant cardiac history, and chronic comorbidities are well-known predictors of in-hospital advanced cardiac care in patients with undifferentiated PH chest pain.14 Most importantly, the history of previous coronary revascularization seems to be a major determinant in EMS providers’ overall assessment and risk-stratification approach. This reinforces the findings of a previous meta-analysis that the absence of a history of coronary revascularization has a modest negative likelihood ratio for identifying patients who are unlikely to have acute MIs.15
On the other hand, our data show that EMS providers were more inclined to triage male patients as high risk with disregard to their age. This is worrisome, given that men were not at increased risk of MI compared with women (8.3% versus 6.7%, P = 0.17). The presence of sex disparities in emergency care for acute MI has been reported previously. It has been shown that women are less likely to be treated with guideline-based medical therapy or cardiac catheterization,16 less likely to receive aspirin or nitroglycerin in the field,17 as well as less likely to have PH-ECGs performed.11 This finding highlights a potential opportunity to address treatment disparities across the care continuum.
TRIAGE BASED ON THE PH-ECG
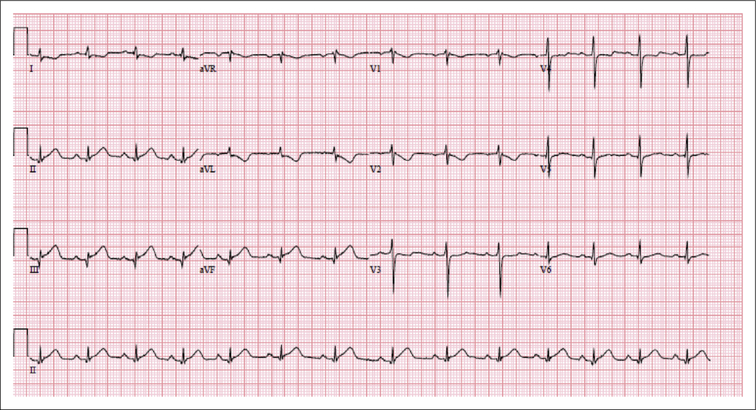
EMS providers are trained to obtain 12-lead ECGs in the field and to look for possible ST changes indicative of STEMI. Our data show that EMS providers misinterpreted nearly half of acute ischemic ECG changes in acute MI as benign (Figure 1). To better understand the factors associated with such low sensitivity, we qualitatively audited all misinterpreted ECGs and identified 2 potential sources of error. The first source of error is the underestimation of ST elevation if the ECG does not mimic the classical tomb-stone morphology. Figure 2 shows the ECG of a patient with inferior STEMI that was interpreted by EMS providers as normal sinus rhythm. Borderline ST-segment elevation has been shown in a recent paper to be the leading cause of false negative results in PH STEMI events.18 The second source of error is that EMS providers are less sensitive to ECG changes other than ST elevation that are indicative of acute myocardial injury (eg, ST depression, new-onset LBBB, LVH with strain, high-degree atrioventricular block). Our data show that EMS providers classified 17% of acute ischemic ECG changes in acute MI as other nonischemic abnormalities (Figure 1).
FIGURE 2.
Prehospital ECG of a selected patient with MI triaged at low risk. Initial 12-lead ECG of a 46-year-old male patient who presented with chest pain radiating bilaterally, associated with shortness of breath and a free past medical history. The patient was triaged by EMS personnel as low risk, and his PH-ECG was interpreted as benign. The patient was eventually diagnosed with inferior STEMI and was successfully stented. This PH-ECG shows 1-mm STEMI in leads II, III, and aVF, with reciprocal changes in leads I and aVL.
CLINICAL IMPLICATIONS TO EMERGENCY NURSING
The findings of our study have several implications for emergency nurses, as they remain at the forefront of evaluating and managing patients with acute chest pain at the emergency department. First, given that nurses are primarily responsible for patient care during care transitions to the emergency department, they should be aware that nearly 30% of patients with MI might be undertriaged. Performing a full assessment and an ECG analysis by the emergency nurse, while being mindful of the most significant predictors for an ongoing acute MI, remains the cornerstone for evaluating patients with PH chest pain, regardless of the level of triage reported en route to the emergency department. In fact, previous studies have shown poor agreement between EMS and nursing triage.19 Second, as this study revealed, patients without histories of coronary revascularization posed a challenge during initial patient assessment, which might lead to undertriage. Nurses should have a lower threshold for suspicion during the initial evaluation of patients with benign medical histories, with an added emphasis on ECG evaluation. Finally, nurses are expected to have basic proficiency in interpreting an array of ischemic ECG abnormalities, independent of the ECG findings reported by EMS providers. Identifying the complex ECG patterns that are proving to be problematic in that setting should help streamline these cases for immediate evaluation by a medical specialist.
STUDY LIMITATIONS
The main strength of this analysis is that we analyzed a large cohort of consecutive and unselected patients from an urban EMS system transporting patients to 3 tertiary care hospitals with PCI capabilities. Our study has several limitations. First, the rate of confirmed MI events was low (7.5%). Although these rates are typical in PH chest pain, the very low-prevalence rate of events might have led to the poor sensitivity and PPV observed in this study. Second, given that nontransmitted ECGs were not permanently stored at our MCC, we audited the PH-ECGs of the transmitted cases and the ED-ECGs of the nontransmitted cases. We have previously reported that 20% of PH ischemic changes resolve before arrival at the emergency department,20 which suggests that some differences in ECG interpretations between EMS providers and our independent reviewers might not be solely due to false positive or negative misinterpretations. Furthermore, EMS providers occasionally confront technical barriers that preclude PH-ECG transmission, an element that we could not quantify in our analysis, owing to the lack of data regarding attempted but failed transmissions. Finally, we do not know the extent of training that each EMS provider had as part of his or her basic training. We are also unable to establish whether EMS providers relied solely on their expertise or used computer-assisted interpretation for their final ECG judgment and documentation.
Conclusions
In this cohort of PH patients with chest pain, EMS providers triaged approximately one third of patients as high risk. Patients triaged as high risk were 3 times more likely to have acute MI. Older age, male sex, and significant cardiac history were the strongest determinants to triage a patient as high risk. EMS providers had moderate sensitivity but poor PPV to triage acute MI. The strongest predictors for misclassifying a patient with MI as low risk were the lack of a history of coronary revascularization and ECG misinterpretation. EMS providers had limited sensitivity and PPV to detect true ischemic ECG changes. To improve EMS sensitivity to STEMI detection, future EMS training should focus on (1) subtle and borderline ST elevation,(2) ST changes in anterior and lateral ECG leads, (3) nonspecific ECG changes that mimic ST elevation, and(4) appropriate global assessment for patients with benign past medical histories.
Contribution to Emergency Nursing Practice.
Appropriate prehospital (PH) triage of patients with chest pain can significantly improve outcomes in acute myocardial infarction.
The main finding of this research is that 1 in 3 patients with acute myocardial infarction are misclassified as low risk by PH providers. Absence of history of previous coronary revascularization and electrocardiographic (ECG) misinterpretation are the strongest independent predictors of undertriage.
Key implications for emergency nursing practice are that nurses need to perform rapid triage of patients with acute chest pain during the transition of care, regardless of field evaluation by emergency medical services (EMS). Special attention needs to be paid to patients with benign past history, including reinterpreting PHECG if possible and repeating an ECG on arrival.
Acknowledgments
This study was funded by National Institute of Health / National Heart, Lung, and Blood Institute (R01 HL 137761).
REFERENCES
- 1.Scholz KH, Maier SKG, Maier LS, et al. Impact of treatment delay on mortality in ST-segment elevation myocardial infarction (STEMI) patients presenting with and without haemodynamic instability: results from the German prospective, multicentre FITT-STEMI trial. Eur Heart J. 2018;39(13):1065–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson JL, Adams CD, Antman EM, et al. 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non–ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(23):e179–e347. [DOI] [PubMed] [Google Scholar]
- 3.O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: Executive Summary. A Report of the ACC/AHA Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):485–510. [DOI] [PubMed] [Google Scholar]
- 4.Patel M, Dunford JV, Aguilar S, et al. Pre-hospital electrocardiography by emergency medical personnel: effects on scene and transport times for chest pain and ST-segment elevation myocardial infarction patients. J Am Coll Cardiol. 2012;60(9):806–811. [DOI] [PubMed] [Google Scholar]
- 5.Squire BT, Tamayo-Sarver JH, Rashi P, Koenig W, Niemann JT. Effect of prehospital cardiac catheterization lab activation on door-to-balloon time, mortality, and false-positive activation. Prehosp Emerg Care. 2014;18(1):1–8. [DOI] [PubMed] [Google Scholar]
- 6.Zegre Hemsey JK, Drew BJ. Prehospital electrocardiography: a review of the literature. J Emerg Nurs. 2012;38(1):9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zegre Hemsey JK, Dracup K, Fleischmann K, Sommargren CE, Drew BJ. Prehospital 12-lead ST-segment monitoring improves the early diagnosis of acute coronary syndrome. J Electrocardiol. 2012;45(3):266–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Zaiti S, Shusterman V, Carey MG. Novel technical solutions for wireless ECG transmission and analysis in the age of the internet cloud. J Electrocardiol. 2013;46(6):540–545. [DOI] [PubMed] [Google Scholar]
- 9.Wilson C, Harley C, Steels S. Systematic review and meta-analysis of pre-hospital diagnostic accuracy studies. Emerg Med J. 2018;35(12): 757–764. [DOI] [PubMed] [Google Scholar]
- 10.Schläpfer J, Wellens HJ. Computer-interpreted electrocardiograms: benefits and limitations. J Am Coll Cardiol. 2017;70(9):1183–1192. [DOI] [PubMed] [Google Scholar]
- 11.Bosson N, Kaji AH, Niemann JT, et al. The utility of prehospital ECG trans-mission in a large EMS system. Prehosp Emerg Care. 2015;19(4):496–503. [DOI] [PubMed] [Google Scholar]
- 12.Al-Zaiti SS, Martin-Gill C, Sejdic E, Alrawashdeh M, Callaway C. Rationale, development, and implementation of the Electrocardiographic Methods for the Prehospital Identification of Non-ST Elevation Myocar-dial Infarction Events (EMPIRE). J Electrocardiol. 2015;48(6):921–926. [DOI] [PubMed] [Google Scholar]
- 13.Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction. J Am Coll Cardiol. 2018;72(18):2231–2264. [DOI] [PubMed] [Google Scholar]
- 14.Frisch A, Heidle KJ, Frisch SO, et al. Factors associated with advanced cardiac care in prehospital chest pain patients. Am J Emerg Med. 2018;36(7):1182–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fanaroff AC, Rymer JA, Goldstein SA, Simel DL, Newby L. Does this patient with chest pain have acute coronary syndrome? The rational clinical examination systematic review. JAMA. 2015;314(18):1955–1965. [DOI] [PubMed] [Google Scholar]
- 16.Mehta LS, Beckie TM, DeVon HA, et al. Acute myocardial infarction in women: a scientific statement from the American Heart Association. Circulation. 2016;133(9):916–947. [DOI] [PubMed] [Google Scholar]
- 17.Meisel ZF, Armstrong K, Mechem CC, et al. Influence of sex on the out-of-hospital management of chest pain. Acad Emerg Med. 2010;17(1):80–87. [DOI] [PubMed] [Google Scholar]
- 18.Bosson N, Sanko S, Stickney RE, et al. Causes of prehospital misinterpretations of ST elevation myocardial infarction. Prehosp Emerg Care. 2017;21(3):283–290. [DOI] [PubMed] [Google Scholar]
- 19.Buschhorn HM, Strout TD, Sholl JM, Baumann MR. Emergency medical services triage using the emergency severity index: is it reliable and valid? J Emerg Nurs. 2013;39(5):e55–e63. [DOI] [PubMed] [Google Scholar]
- 20.Ownbey M, Suffoletto B, Frisch A, Guyette FX, Martin-Gill C. Prevalence and interventional outcomes of patients with resolution of ST-segment elevation between prehospital and in-hospital ECG. Prehosp Emerg Care. 2014;18(2):174–179. [DOI] [PubMed] [Google Scholar]