Abstract
Depression is not only a major global public health concern, but also a common comorbidity among patients who experience chronic diseases, such as cancer, stroke, heart disease, diabetes, and chronic obstructive pulmonary disease. Yet the recognition and treatment varies widely around the world. This study (1) provides an integrated review of the literature on the prevalence of depression among patients with chronic diseases in China and the United States and its relationship to poorer health outcomes and (2) compares the differences in the percentages of patients receiving treatments for depression between the United States and China. Given the current situation, we recommended that primary care and specialty providers should be knowledgeable and alert regarding the signs of depression. Efforts should be directed to further implement integrated care based interventions to manage depression and improve quality of life among patients suffering chronic diseases in both China and the United States.
Keywords: Chronic disease, China, Depression, United States
1. Introduction
Depression is a major global public health concern. In 2015, the World Health Organization (WHO) reported that 4.4% of the global population were living with depression [1]. Moreover, depression is ranked as the largest contributor to non-fatal health loss [1]. The prevalence of depression varies nationally and geographically. For example, the WHO reported that approximately 5.9% and 4.2% of the population exhibit depression in the United States and China, respectively [1]. Additionally, a recent systematic review by Gu et al. [2] demonstrates that rural residents in China display a higher prevalence of major depressive disorder (2.0%) compared to urban residents (1.7%).
China and the United States share some similarities regarding these public health challenges related to chronic disease as a result of their respective aging populations. For example, in 2012, the Institute of Medicine declared chronic disease to be a threat to public health and social economics in the United States [3]. Nearly 48 million Americans are living with various chronic diseases, which account for 70% of total mortality [3]. In 2016, heart disease, malignant neoplasms (i.e., cancer), accidents, chronic obstructive pulmonary disease (COPD), cerebrovascular diseases, Alzheimer's disease, diabetes mellitus, influenza, nephrotic disease and suicide accounted for 74% of all deaths in the United States [4], and seven of these are chronic diseases. Meanwhile, in China, chronic diseases, especially cancer, heart disease, and chronic respiratory diseases, also are a major public health problem, accounting for 86.6% of total mortality [5]. As a result, in 2017, the Chinese government issued the “Medium-to-Long Term Plan for the Prevention and Treatment of Chronic Diseases in China (2017–2025)” to address the burden of these chronic diseases [6].
Individuals presenting chronic conditions are more likely to experience depressive symptoms. Indeed, depression worldwide has been found to be more prevalent among patients with cancer, heart disease, diabetes, stroke, and respiratory issues than in the general population [7]. However, making a definitive diagnosis can be difficult because of the overlapping clinical symptoms between depression and chronic diseases [8]. Unrecognized depression in primary care is becoming a serious concern, with the growing aging population and associated burden of chronic disease [9]. Therefore, not only clinicians must be equipped to recognize depression among patients with chronic disease, but also patients with chronic diseases must be educated to understand depression.
Concerning the burden of chronic disease and depression, China and the United States face similar public health challenges—especially because their growing aging populations will precipitate and increase the prevalence of chronic disease in both countries. No study has compared depression in chronic diseases in China and the United States Against this backdrop, this paper (1) outlines the prevalence and poor health outcomes for depression among patients of the five most common chronic diseases (i.e., cancer, stroke, heart disease, diabetes, and COPD) and (2) compares the level of treatment for depression in the United States and China.
2. Prevalence and poor health outcomes for depression among chronic diseases
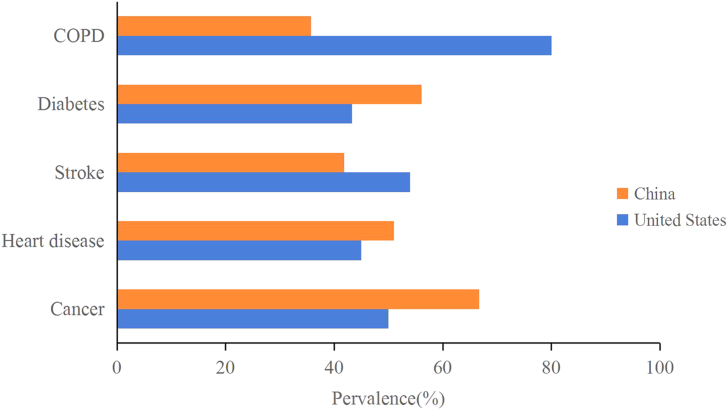
Depression is highly prevalent among individuals suffering cancer, diabetes, heart disease, stroke, and COPD in both countries (see Fig. 1). In general, China has a higher prevalence of depression among patients with diabetes, heart disease and cancer, compared with the United States. Furthermore, a variety of poor health outcomes (e.g., impaired self-management, compromised quality of life (QOL), and reduced life expectancy) are related to depression among patients with chronic illnesses [[10], [11], [12]]. See Table 1.
Fig. 1.
Prevalence of depression with chronic diseases in China and the United States.
Table 1.
Poor health outcomes related to depression among different chronic illnesses.
| Poor health outcomes | Cancer | Stroke | Heart disease | Diabetes | COPD |
|---|---|---|---|---|---|
| Decreased QOL | x | x | x | x | |
| Increased mortality | x | x | x | x | |
| Reduced life expectancy | x | ||||
| Functional disability | x | x | |||
| Impaired self-managements | x | ||||
| Reduced adherence to treatment | x | x | |||
| Rehospitalization | x | ||||
| Exacerbation of disease | x |
2.1. Cancer
Cancer poses a major physical and psychological challenge for any individual. As such, depression is common among cancer patients. Depression not only compromises the QOL of cancer patients, but also increases their mortality [12]. Depression occurred among 7%–50% of cancer patients with different stages of cancer and different health environments in the United States [7]. A 2014 meta-analysis of research on depression among cancer patients evaluated 211 studies and revealed that the incidence of depression varied by the location of the cancer and the time course of the cancer [13]. Cancer patients are more likely to experience depression at the time of cancer diagnosis [14]. Indeed, depression is highly prevalent among patients with brain tumor (41%–93%) and pancreatic cancer (50%), with the lowest prevalence among colon and lymphoma cancer patients in the United States [15]. In terms of the type of cancer, in China, a 2014 study among 1217 cancer patients indicated that the prevalence of depression is nearly 67%, with the highest prevalence among patients with lung cancer and esophagus cancer [16].
2.2. Stroke
The decreased QOL, increased mortality, and more severe functional disability that occur after stroke increasingly have been recognized to be associated with depression [10,17]. Indeed, approximately 5%–54% of patients have reported depressive symptoms in the acute period following stroke; moreover, these depressive symptoms not only appear in the acute period following a stroke, but also persist for a prolonged period [18]. Similarly, a 2013 systematic review and meta-analysis of depression after stroke demonstrates that 29% patients exhibited depressive symptoms after stroke, and these symptoms remained present after 5 years among 39%–52% of patients in the United States [17]. In terms of gender, women and inpatients have been observed to exhibit a higher incidence of depression post-stroke compared to men and patients in community settings in both countries [19]. In China, the prevalence of depression post-stroke ranges from 27.47% to 41.8% [20,21].
2.3. Heart disease
Depression has been shown to increase the mortality rate among not only outpatients with chronic heart failure [22], but also increase the likelihood of hospital readmission and heart transplantation [23]. For example, in the United States, about 30%–45% of coronary artery disease patients report depressive symptoms in clinic settings [24]. In China, a 2014 meta-analysis demonstrates that the prevalence of depression in patients with coronary heart disease ranges from 34.6% to 51% in community and hospital settings [25]. Depressive symptoms persist for a long time among patients with heart disease. For example, the occurrence of depression increases up to 1 year after myocardial infarction (MI) and is most prevalent 6 months after MI [26]. Moreover, depression can last 2 years after implantable cardioverter-defibrillator (ICD) placement, irrespective of country [27].
2.4. Diabetes
Depression contributes to impaired self-management, compromised QOL, and reduced life expectancy among patients with diabetes [28]. Moreover, depression can lead to poor self-care (e.g., medication nonadherence, less exercise, poor diet, insufficient blood glucose testing, and higher risk to develop microvascular and macrovascular complications) among patient with Type 2 diabetes [29,30]. Indeed, studies of depression among diabetics reveal that 5.8%–43.3% of diabetes patients exhibit depression [31]. Compared to healthy members of the general population, individuals with type 1 and type 2 diabetes are 2 and 3 times more likely to exhibit depression, respectively [31]. In China, the prevalence of depression among patients with type 2 diabetes ranges from 6.1% to 56.1% [25,32].
2.5. COPD
Depression can lead to increased mortality, reduced adherence to treatment, impaired QOL, and exacerbated COPD among patients with COPD [11,33]. Moreover, if depression remains un-identified and untreated among COPD patients, it has a negative impact on physical performance, energy, social behavior, and healthcare utilization [33,34]. In fact, among COPD patients, the prevalence rate of depression is 8%–80% [22]. Specifically, in China, patients with COPD are 1.9 times more likely to experience depression compared to non-COPD patients [35], and the prevalence rate of depression is 35.7% [36].
3. Comparison of the level of treatment for depression in the United States and China
In the United States, a 2009 meta-analysis of the clinical diagnosis of depression in primary care demonstrates that only 47% of patients with depression were recognized by primary care clinicians [37]. Moreover, the National Health and Nutrition Examination Survey, conducted from 2009 to 2012, reveals that only 35% of individuals with depression received treatment from a mental health specialist [38]. One reason for these low rates of depression diagnosis is that chronic comorbidities can negatively influence the recognition of depressive symptoms by primary care providers [39].
In China, the percentage of patients with mental disorders who received treatment was even lower. A World Health Survey conducted in 2003 indicates that only 1% of people with depressive symptoms had been treated in China [40], and this trend continues. For example, in 2014, only 6.9% of Chinese oncology patients with major depressive disorders were found to have been treated by oncologists [41]. Additionally, a 2012 study conducted in urban primary care settings in China reports that only 3% of elderly residents with major depressive disorders received treatment by a mental health provider; moreover, less than 1% of them were treated with an antidepressant [42].
4. Discussion
Depression is highly prevalent in patients with cancer, heart disease, stroke, diabetes and COPD in both countries. However, differences exist in the percentage receiving treatment for depression in China and the United States. Those differences can be attributed to the differences in culture (e.g., stigma of mental illness) and health care systems (e.g., integrated care model) endemic to the two places.
4.1. Role of depression in chronic diseases
The high prevalence of depression among individuals presenting chronic diseases in both China and the United States begs the questions of underlying mechanisms. Depression exhibits a bidirectional relationship with chronic diseases such as cancer, diabetes, heart disease, stroke, and COPD [8]. Emerging evidence suggests that some common biological mechanism exist between depression with chronic disease. For example, depression exacerbates some chronic diseases through promoting an increase in pro-inflammatory cytokines, a hyperactive HPA axis, and dysfunction of the autonomic nervous system and metabolic factors [43]. Moreover, in the presence of both depression and diabetes, the HPA axis works together with the sympathetic nervous system to increase catecholamine and cytokines, which ultimately leads to insulin resistance [43]. In a clinical review of depression and cardiovascular disease, the autonomic nervous system, pro-inflammatory cytokines, neurohormonal, coagulopathic genetic factors, and platelet receptors have been posited to be the plausible biological mechanisms connecting depression with cardiovascular disease [44]. Depression can worsen the prognoses among cancer patients, and stress can increase inflammation through stimulating the sympathetic nervous system [45].
In general, across various chronic diseases, inflammation is a common biological mechanism associating depression with chronic disease. Depression can worsen the prognoses among cancer patients, and stress can increase inflammation through stimulating the sympathetic nervous system [45]. Pro-inflammatory cytokines are biomarkers of increased inflammation among cancer patients experiencing depression. Research has shown that chronic inflammation is the underlying pathway between depressive symptoms and worsening pulmonary function [46]. Although depression and chronic disease share some common underlying biological mechanisms, some treatments and pharmacological interventions also may contribute to depressive symptoms so the relevant mechanisms could differ. Nevertheless, none of the papers examined the underlying mechanism between depression and a heterogeneous population reflecting different chronic diseases. As such, additional longitudinal research is needed to identify any causal relationship between depression and chronic disease.
4.2. Similarities and differences in the prevalence of depression among chronic diseases between China and the United States
Both countries exhibit a high prevalence of depression in cancer, heart disease, stroke, diabetes and COPD with slight differences. In general, China has a higher prevalence of depression in patients with cancer, heart disease and diabetes. This variability can be attributed to heterogeneous samples across studies, differences in study designs, measurement variability, and some risk factors.
Gender, age, education, income, and BMI level are associated with depression among individuals presenting chronic disease [47]. In general, women with low income and low educational levels are more likely to exhibit depression when they present with chronic disease [48]. In China, older women generally possess lower education and lower income. Moreover, because patients with higher education are more knowledgeable about the disease process, they exhibit less anxiety compared with patients possessing a lower level of education.
In the case of COPD, patients in the United States exhibit a higher prevalence of depression than Chinese patients. This can be explained by the different disease burdens between the two countries. According to the Global Burden of Disease 2016 study, the top three causes of death in China and the United States were stroke, heart disease, and road injury and heart disease, cancer, and COPD, respectively [48]. Compared with China, COPD is a more problematic disease in the United States.
The prevalence of depression among different types of cancer patients differs between China and the United States. For example, depression is highly prevalent among lung cancer patients in China—and less prevalent among U.S. lung cancer patients [15,16]. This difference can be attributed to differences in the cancer incidence between the United States and China. In China, lung cancer is the most dominant cancer, and gastrointestinal cancers, such as liver, esophagus, and stomach cancer are more commonly seen in China than the United States [49]. Due to changing dietary habits, typical Chinese usually exhibit high consumption of preserved or salted food, instead of fresh vegetables and fruits. Diet risk factors such as these, combined with heavy alcohol consumption and low social economic status appreciably contribute to gastrointestinal cancers in China [50].
In general, studies of depression among patients presenting chronic diseases in China are limited in number. For example, most studies in China that evaluated depression among one specific cancer, and only three studies evaluated depression among different cancer patients. Meta-analyses and literature reviews addressing depression among patients with cancer, stroke, COPD, and diabetes in China are needed.
4.3. Differences in receiving treatment for depression between the United States and China
The differences in the percentage of those receiving treatment for depression in China and the United States can be attributed to the differences in culture and health care systems endemic to the two places. For example, in China, social stigma discourages individuals from acknowledging depression, somatization, and help-seeking behaviors [51]. In Chinese culture, mental disorders are highly stigmatized because they can disrupt social harmony and violate Confucian principles [52]. However, in the wake of China's opening-up and reform policies that began in 1978, Western culture has exerted a growing influence in China [53]. Part and parcel of this influence is that increasingly more research has been conducted—and policies developed and implemented—germane to the recognition and treatment of depression in China [54].
In addition to the use of Western approaches to managing depression in China, alternative novel interventions also have been studied for their efficiency in the treatment of depression. For example, a 2015 meta-analysis demonstrates that traditional Chinese exercises (e.g., Qigong or Taichi) can reduce depressive symptoms and improve QOL among patients with both depression and chronic disease [55]. In addition, Chinese patients with depression have benefited from acupuncture combined with selective serotonin reuptake inhibitors (SSRI) compared with SSRI alone [56]. Moreover, a 2015 randomized controlled trial demonstrates the efficacy of sertraline plus deanxit to treat Chinese patients with depression and anxiety in chronic diseases [57]. In many countries, including the United States and China, sociodemographic factors, such as age, gender, education, employment, financial barriers, and the wealth of the country also can affect an individual's likelihood of receiving treatment for depression, and these factors indeed play a role in the differences in treatment available in China and the United States [58].
4.4. Integrated care
In the United States, an integrated care model (ICM) has been adapted for use in different healthcare contexts. Models of integrated care, sometimes called collaborative care, refer to the systematic coordination of physical and mental health for patients in primary care [59]. For example, the improving mood-promoting access to collaborative treatment (IMPACT) collaborative care management program has been demonstrated to not only be feasible, but also provide greater efficacy in reducing the severity of depression than usual care [60]. Moreover, other studies have shown that integrated care can improve treatment response and remission [61]. Examples of successful ICMs from across the United States include the Integrated Behavioral Health Project in California, the Community Mental Health Case Management in Missouri, and the Harris County Community Behavioral Health Program in Texas.
In 2006, the Chinese government enacted a new policy concerning the development of community health services. This policy stipulates that mental disorders should be treated as chronic diseases in primary care settings [62]. The policy stemmed in part from evidence that neglect of depression in the general hospital was a serious issue in central China [63]. Although clinicians must improve the identification of depression in the primary care setting, ICM has not been practiced clinically in China. Nonetheless, a 2015 randomized trial study has tested the effectiveness of an ICM model among Chinese patients 50 years and older with major depressive disorders; its results demonstrate that ICM contributes to reducing depressive symptoms and patient-reported stigma and improving QOL [64]. More evidence-based studies of ICM of this type must be conducted in China to promote the well-being of individuals living with depression and chronic disease.
4.5. Implications for nurses
The prevalence of depression and anxiety are high among patients with chronic diseases in both the United States and China. The depression of many of these patients remains under-recognized and under-treated—especially in China. Therefore, nurses caring for these patients should be knowledgeable and alert regarding the signs of depression and anxiety. Proactive actions can be taken to screen for mental health symptoms using valid tools such as the Beck Depression Inventory [65] and the Hospital Anxiety and Depression Scale [66]. Moreover, nurses can provide patients presenting chronic diseases with useful resources and strategies to effectively manage mental health symptoms. Whether in China or the United States, advanced practice mental health nurses will play an important role in the future with the adaption of ICM [67].
The complexity of chronic illnesses presented by patients can occupy the attention of nurses, which can hamper their ability to notice and assess anxiety among the patients. Therefore, nurses must be equipped with a heightened awareness of the symptoms of anxiety and depression when caring for patients suffering chronic illnesses. Moreover, nurses should be able to differentiate the symptoms of depression or anxiety from those of chronic illness, as the two can be similar. As such, nurses should place emphasis on assessing patients who present a new diagnosis of chronic illness or who are in an advanced stage of chronic illness because patients such as these are more likely to suffer depression [68]. In addition, the time of occurrence of depressive symptoms is important for nurses to know. For example, nurses should assess for depressive symptoms among cancer patients at the time of diagnosis. Furthermore, when taking care of patients who have suffered a stroke, nurses should assess for depressive symptoms both at the time of the acute stroke and weeks after the stroke. Nurses also should assess for depressive symptoms among patients who have suffered MI.
Nurses should be aware that untreated depression or anxiety among individuals suffering chronic illnesses can result in medication non-adherence, more rapid disease progression, and poor treatment outcomes. For example, when caring for patients with diabetes, nurses should pay close attention to the patients’ disease self-management—especially if the patients suffer depressive symptoms. Moreover, follow-up phone calls can be used to improve the poor self-care of the patients. In addition to pharmacological interventions, nurses should be knowledgeable about psychoeducational and psychosocial interventions to treat depression as they have been found to be effective in the treatment of depression among patients with different types of cancer [69]. Furthermore, a combined therapy comprising both psychological and antidepressant therapy to manage depression has been found to be more effective than medications alone [70]. Therefore, a combined therapy of this sort should be considered as a treatment approach for patients presenting both depression and/or anxiety and chronic illnesses. In particular, the primary care nurses—whether in the United States or China—can play a key role in not only the identification of depression and/or anxiety among patients presenting chronic diseases, but also the education of at-risk patients concerning the value of treatment for depression and/or anxiety in maintaining and improving QOL.
Conflicts of interest
No conflict of interest is declared by the authors.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Ethical approval
N/A.
Acknowledgements
N/A.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2018.11.007.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization Depression and other common mental disorders: global health estimates. 2017. http://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf;jsessionid=AF90F1082645C497062D5FD9650888CE?sequence=1
- 2.Gu L., Xie J., Long J., Chen Q., Chen Q., Pan R. Epidemiology of major depressive disorder in mainland China: a systematic review. PloS One. 2013;8(6) doi: 10.1371/journal.pone.0065356. e65356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine . The National Academies Press; Washington, DC: 2012. Living well with chronic illness: a call for public health action.http://www.nationalacademies.org/hmd/∼/media/Files/Report Files/2012/Living-Well-with-Chronic-Illness/livingwell_chronicillness_reportbrief.pdf [Google Scholar]
- 4.Xu . 2018. national vital statistics reports volume 67, number 5 july 26, 2018, deaths final data for 2016. [PubMed] [Google Scholar]
- 5.National Health and Family Planning Commission of the PRC Report on Chinese resident's chronic disease and nutrition. 2014. http://www.chinadaily.com.cn/m/chinahealth/2015 06/15/content_21008408.htm
- 6.Kong L.-Z. China's medium-to-long term plan for the prevention and treatment of chronic diseases (2017–2025) under the Healthy China Initiative. Chronic Dis Transl Med. 2017;3(3):135–137. doi: 10.1016/j.cdtm.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clarke D.M., Currie K.C. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Aust. 2009;190(7):S54–S60. doi: 10.5694/j.1326-5377.2009.tb02471.x. [DOI] [PubMed] [Google Scholar]
- 8.DeJean D., Giacomini M., Vanstone M., Brundisini F. Patient experiences of depression and anxiety with chronic disease: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser. 2013;13(16):1–33. [PMC free article] [PubMed] [Google Scholar]
- 9.Craven M.A., Bland R. Depression in primary care: current and future challenges. Can J Psychiatr. 2013;58(8):442–448. doi: 10.1177/070674371305800802. [DOI] [PubMed] [Google Scholar]
- 10.Žikić T.R., Divjak I., Jovićević M., Semnic M., Slankamenac P., Žarkov M. The effect of post stroke depression on functional outcome and quality of life. Acta Clin Croat. 2014;53(3):294–301. [PubMed] [Google Scholar]
- 11.Salte K., Titlestad I., Halling A. Depression is associated with poor prognosis in patients with chronic obstructive pulmonary disease-a systematic review. Dan Med J. 2015;62(10):A5137. [PubMed] [Google Scholar]
- 12.Satin J.R., Linden W., Phillips M.J. Depression as a predictor of disease progression and mortality in cancer patients. Cancer. 2009;115(22):5349–5361. doi: 10.1002/cncr.24561. [DOI] [PubMed] [Google Scholar]
- 13.Krebber A., Buffart L., Kleijn G., Riepma I., Bree R., Leemans C. Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments. Psycho Oncol. 2014;23(2):121–130. doi: 10.1002/pon.3409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Linden W., Vodermaier A., MacKenzie R., Greig D. Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord. 2012;141(2):343–351. doi: 10.1016/j.jad.2012.03.025. [DOI] [PubMed] [Google Scholar]
- 15.Kissane D.W., Maj M., Sartorius N. John Wiley & Sons; 2011. Depression and cancer. [Google Scholar]
- 16.Hong J.S., Tian J. Prevalence of anxiety and depression and their risk factors in Chinese cancer patients. Support Care Canc. 2014;22(2):453–459. doi: 10.1007/s00520-013-1997-y. [DOI] [PubMed] [Google Scholar]
- 17.Ayerbe L., Ayis S., Wolfe C.D., Rudd A.G. Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis. Br J Psychiatry. 2013;202(1):14–21. doi: 10.1192/bjp.bp.111.107664. [DOI] [PubMed] [Google Scholar]
- 18.Kouwenhoven S.E., Kirkevold M., Engedal K., Kim H.S. Depression in acute stroke: prevalence, dominant symptoms and associated factors. A systematic literature review. Disabil Rehabil. 2011;33(7):539–556. doi: 10.3109/09638288.2010.505997. [DOI] [PubMed] [Google Scholar]
- 19.Poynter B., Hon M.S., Diaz-Granados N., Kapral M., Grace S.L., Stewart D.E. Sex differences in the prevalence of post-stroke depression: a systematic review. Psychosomatics. 2009;50(6):563–569. doi: 10.1176/appi.psy.50.6.563. [DOI] [PubMed] [Google Scholar]
- 20.Zhang W.-N., Pan Y.-H., Wang X.-Y., Zhao Y. A prospective study of the incidence and correlated factors of post-stroke depression in China. PloS One. 2013;8(11) doi: 10.1371/journal.pone.0078981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang N., Wang C.X., Wang A.X., Bai Y., Zhou Y., Wang Y.L. Time course of depression and one-year prognosis of patients with stroke in mainland China. CNS Neurosci Ther. 2012;18(6):475–481. doi: 10.1111/j.1755-5949.2012.00312.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yohannes A., Willgoss T., Baldwin R., Connolly M. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: prevalence, relevance, clinical implications and management principles. Int J Geriatr Psychiatr. 2010;25(12):1209–1221. doi: 10.1002/gps.2463. [DOI] [PubMed] [Google Scholar]
- 23.Sullivan M.D., Levy W.C., Crane B.A., Russo J.E., Spertus J.A. Usefulness of depression to predict time to combined end point of transplant or death for outpatients with advanced heart failure. Am J Cardiol. 2004;94(12):1577–1580. doi: 10.1016/j.amjcard.2004.08.046. [DOI] [PubMed] [Google Scholar]
- 24.Rudisch B., Nemeroff C.B. Epidemiology of comorbid coronary artery disease and depression. Biol Psychiatry. 2003;54(3):227–240. doi: 10.1016/s0006-3223(03)00587-0. [DOI] [PubMed] [Google Scholar]
- 25.Ren Y., Yang H., Browning C., Thomas S., Liu M. Prevalence of depression in coronary heart disease in China: a systematic review and meta-analysis. Chin Med J. 2014;127(16):2991–2998. [PubMed] [Google Scholar]
- 26.Kala P., Hudakova N., Jurajda M., Kasparek T., Ustohal L., Parenica J. Depression and anxiety after acute myocardial infarction treated by primary PCI. PloS One. 2016;11(4) doi: 10.1371/journal.pone.0152367. e0152367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Suzuki T., Shiga T., Kuwahara K., Kobayashi S., Suzuki S., Nishimura K. Prevalence and persistence of depression in patients with implantable cardioverter defibrillator: a 2-year longitudinal study. Pacing Clin Electrophysiol. 2010;33(12):1455–1461. doi: 10.1111/j.1540-8159.2010.02887.x. [DOI] [PubMed] [Google Scholar]
- 28.Holt R.I., Katon W.J. Dialogue on diabetes and depression: dealing with the double burden of co-morbidity. J Affect Disord. 2012;142:S1–S3. doi: 10.1016/S0165-0327(12)00632-5. [DOI] [PubMed] [Google Scholar]
- 29.Gonzalez J.S., Safren S.A., Cagliero E., Wexler D.J., Delahanty L., Wittenberg E. Depression, self-care, and medication adherence in type 2 diabetes. Diabetes Care. 2007;30(9):2222–2227. doi: 10.2337/dc07-0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De Groot M., Anderson R., Freedland K.E., Clouse R.E., Lustman P.J. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001;63(4):619–630. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 31.Roy T., Lloyd C.E. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. 2012;142:S8–S21. doi: 10.1016/S0165-0327(12)70004-6. [DOI] [PubMed] [Google Scholar]
- 32.Zhang Y., Ting R.Z., Yang W., Jia W., Li W., Ji L. Depression in Chinese patients with type 2 diabetes: associations with hyperglycemia, hypoglycemia, and poor treatment adherence. J Diabetes. 2015;7(6):800–808. doi: 10.1111/1753-0407.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sode B.F., Dahl M., Nordestgaard B.G. Myocardial infarction and other co-morbidities in patients with chronic obstructive pulmonary disease: a Danish nationwide study of 7.4 million individuals. Eur Heart J. 2011;32(19):2365–2375. doi: 10.1093/eurheartj/ehr338. [DOI] [PubMed] [Google Scholar]
- 34.Doyle T., Palmer S., Johnson J., Babyak M.A., Smith P., Mabe S. Association of anxiety and depression with pulmonary-specific symptoms in chronic obstructive pulmonary disease. Int J Psychiatr Med. 2013;45(2):189–202. doi: 10.2190/PM.45.2.g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsai T.-Y., Livneh H., Lu M.-C., Tsai P.-Y., Chen P.-C., Sung F.-C. Increased risk and related factors of depression among patients with COPD: a population-based cohort study. BMC Publ Health. 2013;13(1):976. doi: 10.1186/1471-2458-13-976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lou P., Zhu Y., Chen P., Zhang P., Yu J., Zhang N. Prevalence and correlations with depression, anxiety, and other features in outpatients with chronic obstructive pulmonary disease in China: a cross-sectional case control study. BMC Pulm Med. 2012;12(1):53. doi: 10.1186/1471-2466-12-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mitchell A.J., Vaze A., Rao S. Clinical diagnosis of depression in primary care: a meta-analysis. Lancet. 2009;374(9690):609–619. doi: 10.1016/S0140-6736(09)60879-5. [DOI] [PubMed] [Google Scholar]
- 38.Pratt L.A., Brody D.J. Depression in the US household population, 2009-2012. NCHS Data Brief. 2014;(172):1–8. [PubMed] [Google Scholar]
- 39.Menear M., Doré I., Cloutier A.-M., Perrier L., Roberge P., Duhoux A. The influence of comorbid chronic physical conditions on depression recognition in primary care: a systematic review. J Psychosom Res. 2015;78(4):304–313. doi: 10.1016/j.jpsychores.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 40.China - World Health Survey [Internet] World health organization. 2003. http://apps.who.int/healthinfo/systems/surveydata/index.php/catalog/78 [cited May 2018]. Available from:
- 41.Zhao L., Li X., Zhang Z., Song C., Guo C., Zhang Y. Prevalence, correlates and recognition of depression in Chinese in patients with cancer. Gen Hosp Psychiatr. 2014;36(5):477–482. doi: 10.1016/j.genhosppsych.2014.05.005. [DOI] [PubMed] [Google Scholar]
- 42.Chen S., Conwell Y., Vanorden K., Lu N., Fang Y., Ma Y. Prevalence and natural course of late-life depression in China primary care: a population based study from an urban community. J Affect Disord. 2012;141(1):86–93. doi: 10.1016/j.jad.2012.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Katon W.J. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci. 2011;13(1):7–23. doi: 10.31887/DCNS.2011.13.1/wkaton. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hare D.L., Toukhsati S.R., Johansson P., Jaarsma T. Depression and cardiovascular disease: a clinical review. Eur Heart J. 2014;35(21):1365–1372. doi: 10.1093/eurheartj/eht462. [DOI] [PubMed] [Google Scholar]
- 45.Sotelo J.L., Musselman D., Nemeroff C. The biology of depression in cancer and the relationship between depression and cancer progression. Int Rev Psychiatr. 2014;26(1):16–30. doi: 10.3109/09540261.2013.875891. [DOI] [PubMed] [Google Scholar]
- 46.Lu Y., Feng L., Feng L., Nyunt M.S., Yap K.B., Ng T.P. Systemic inflammation, depression and obstructive pulmonary function: a population-based study. Respir Res. 2013;14(1):53. doi: 10.1186/1465-9921-14-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu Q., Cai H., Yang L.H., Xiang Y.-B., Yang G., Li H. Depressive symptoms and their association with social determinants and chronic diseases in middle-aged and elderly Chinese people. Sci Rep. 2018;8(1):3841. doi: 10.1038/s41598-018-22175-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Naghavi M., Abajobir A.A., Abbafati C., Abbas K.M., Abd-Allah F., Abera S.F. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang Y-c, Wei L-j, Liu J-t, Li S-x, Wang Q-s. Comparison of cancer incidence between China and the USA. Cancer Biol Med. 2012;9(2):128–132. doi: 10.3969/j.issn.2095-3941.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zou X., Chen G. The epidemiology of cancers of stomach and esophagus in China. J Gastrointest Dig Syst. 2013;3:137. [Google Scholar]
- 51.Parker G., Gladstone G., Chee K.T. Depression in the planet's largest ethnic group: the Chinese. Am J Psychiatry. 2001;158(6):857–864. doi: 10.1176/appi.ajp.158.6.857. [DOI] [PubMed] [Google Scholar]
- 52.Yang L. Application of mental illness stigma theory to Chinese societies: synthesis and new directions. Singap Med J. 2007;48(11):977–985. [PubMed] [Google Scholar]
- 53.He W. Challenges facing China and harmony as a state strategy. Cult Dynam. 2015;27(2):301–310. [Google Scholar]
- 54.Zeng Q., Wang W.C., Fang Y., Mellor D., Mccabe M., Byrne L. Evaluations of treatment efficacy of depression from perspective of both patients' symptoms and general sense of mental health and wellbeing: a large scale, multi-centered, longitudinal study in China. Psychiatr Res. 2016;241:55–60. doi: 10.1016/j.psychres.2016.04.111. [DOI] [PubMed] [Google Scholar]
- 55.Wang X., Pi Y., Chen B., Chen P., Liu Y., Wang R. Effect of traditional Chinese exercise on the quality of life and depression for chronic diseases: a meta-analysis of randomised trials. Sci Rep. 2015;5:15913. doi: 10.1038/srep15913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang T., Wang L., Tao W., Chen L. Acupuncture combined with an antidepressant for patients with depression in hospital: a pragmatic randomised controlled trial. Acupunct Med. 2014;32(4):308–312. doi: 10.1136/acupmed-2013-010469. [DOI] [PubMed] [Google Scholar]
- 57.Wang L., Zhong Z., Hu J., Rong X., Liu J., Xiao S. Sertraline plus deanxit to treat patients with depression and anxiety in chronic somatic diseases: a randomized controlled trial. BMC Psychiatr. 2015;15(1):84. doi: 10.1186/s12888-015-0449-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Smits F., Huijts T. Treatment for depression in 63 countries worldwide: describing and explaining cross-national differences. Health Place. 2015;31:1–9. doi: 10.1016/j.healthplace.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 59.Goodrich D.E., Kilbourne A.M., Nord K.M., Bauer M.S. Mental health collaborative care and its role in primary care settings. Curr Psychiatr Rep. 2013;15(8):383. doi: 10.1007/s11920-013-0383-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Unützer J., Katon W., Callahan C.M., Williams J.W., Jr., Hunkeler E., Harpole L. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. J Am Med Assoc. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 61.Butler M., Kane R.L., McAlpine D., Kathol R., Fu S.S., Hagedorn H. Does integrated care improve treatment for depression? a systematic review. J Ambul Care Manag. 2011;34(2):113–125. doi: 10.1097/JAC.0b013e31820ef605. [DOI] [PubMed] [Google Scholar]
- 62.Wang J., Kushner K., Frey J.J., Du X.P., Qian N. Primary care reform in the Peoples' Republic of China: implications for training family physicians for the world's largest country. Fam Med. 2007;39(9):639–643. [PubMed] [Google Scholar]
- 63.Zhong B-l, Chen H-h, Zhang J-f, Xu H-m, Zhou C., Yang F. Prevalence, correlates and recognition of depression among inpatients of general hospitals in Wuhan, China. Gen Hosp Psychiatr. 2010;32(3):268–275. doi: 10.1016/j.genhosppsych.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 64.Chen S., Conwell Y., He J., Lu N., Wu J. Depression care management for adults older than 60 years in primary care clinics in urban China: a cluster-randomized trial. Lancet Psychiatry. 2015;2(4):332–339. doi: 10.1016/S2215-0366(15)00002-4. [DOI] [PubMed] [Google Scholar]
- 65.Beck A.T., Steer R.A., Brown G.K. Beck depression inventory-II. San Antonio. 1996;78(2):490–498. [Google Scholar]
- 66.Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 67.Delaney K.R., Robinson K.M., Chafetz L. Development of integrated mental health care: critical workforce competencies. Nurs Outlook. 2013;61(6):384–391. doi: 10.1016/j.outlook.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 68.Simon G.E. Treating depression in patients with chronic disease. West J Med. 2001;175(5):292–293. doi: 10.1136/ewjm.175.5.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li M., Fitzgerald P., Rodin G. Evidence-based treatment of depression in patients with cancer. J Clin Oncol. 2012;30(11):1187–1196. doi: 10.1200/JCO.2011.39.7372. [DOI] [PubMed] [Google Scholar]
- 70.Pampallona S., Bollini P., Tibaldi G., Kupelnick B., Munizza C. Combined pharmacotherapy and psychological treatment for depression: a systematic review. Arch Gen Psychiatr. 2004;61(7):714–719. doi: 10.1001/archpsyc.61.7.714. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.