Abstract
INTRODUCTION:
Currently, only topical minoxidil (MNX) and oral finasteride (FNS) are approved by the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for the treatment of androgenetic alopecia. Although FNS is efficacious for hair regrowth, its systemic use is associated with side effects limiting long-term utilization. Exploring topical FNS as an alternative treatment regimen may prove promising.
METHODS:
A search was conducted to identify studies regarding human in vivo topical FNS treatment efficacy including clinically relevant case reports, randomized controlled trials (RCTs), and prospective studies.
RESULTS:
Seven articles were included in this systematic review. In all studies, there was significant decrease in the rate of hair loss, increase in total and terminal hair counts, and positive hair growth assessment with topical FNS. Both scalp and plasma DHT significantly decreased with application of topical FNS, however no changes in serum testosterone were noted.
CONCLUSION:
Preliminary results on the use of topical FNS are limited but safe and promising. Continued research into drug-delivery, ideal topical concentration and application frequency, side effects and use for other alopecias will help to elucidate the full extent of topical FNS’ use.
Keywords: topical finasteride, androgenetic alopecia, efficacy, adverse events
INTRODUCTION
Androgenetic alopecia (AGA) is a common chronic, cutaneous condition encountered by dermatologists globally. AGA is androgen-dependent and characterized by an hereditary inheritance pattern, beginning with the advent of puberty; in predisposed males and females scalp hair progressively thins in a defined pattern, most often at the vertex, with non-scarring, progressive miniaturization of the hair follicle and shaft.1 Unfortunately, AGA is often accompanied by low self-esteem and negatively impacts quality of life. Despite its prevalence and patient morbidity, Food and Drug Administration (FDA) and the European Medicines Agency (EMA)-approved therapeutic options for AGA are limited to oral finasteride (FNS; Propecia®, Merck Pharmaceuticals, for men only) and topical minoxidil (MNX; Rogaine®, Johnson and Johnson Healthcare Products, for men and women).2,8 In the absence of other therapeutic modalities, practitioners may use surgical hair transplant; however, patients often encounter increased cost because most insurance plans do not cover the procedure. In addition, transplants are associated with risks such as bleeding and infection.3
Pathogenesis of AGA is related to the purported binding of dihydrotestosterone (DHT) to androgen receptors (AR) located at the hair follicle. DHT is produced by conversion of testosterone using 5-ɑ-reductase type 2, an enzyme located in the follicle dermal papilla. DHT levels are affected by factors including the abundance of weak androgens, testosterone conversion, activity of androgen inactivating enzymes, and abundance of AR.4˒5 AGA predisposed dermis exhibits high levels of DHT and increased expression of AR.6
Systemic FNS, a 5ɑ-reductase inhibitor 4-aza-3-oxosteroid compound, has been extensively studied and is clinically used for the treatment of benign prostate hyperplasia (BPH) and AGA.7 FNS works by competitively inhibiting 5ɑ-reductase type 2, resulting in the inhibition of the conversion of testosterone to DHT, markedly suppressing serum DHT levels. The mean terminal half-life of FNS is approximately five to six hours in men 18–60 years, and eight hours in men greater than 70 years of age. DHT levels return to normal within 14 days of treatment discontinuation. It is expected that after systemic FNS use for the treatment of AGA is stopped, reversal of hair regrowth occurs within 12 months.8 In its systemic form, various side effects such as gynecomastia, breast tenderness, malignant neoplasms of the male breast, decreased ejaculate volume, decrease in testicular size, testicular pain, reduction in penile curvature, reduction in penile size, sexual disorder, male infertility, high grade prostate cancer, and prostatitis have been reported.8 These side effects are often prohibitive as male patients are sensitive to sexual side effects.
Animal studies have shown that topical FNS may have protective effects against AGA. Comparing topical FNS 2% solution to a fern extract (Adiantum capillus-veneris) in a testosterone-induced alopecia albino mouse model demonstrated higher follicular density and anagen:telogen ratios in groups treated with topical FNS.9 In humans, topical FNS application for the treatment of AGA was first conducted twenty years ago by Mazarella et al. in an attempt to analyze its efficacy and safety.10 In the past five years, emerging evidence suggests that topical FNS may be a promising treatment with a less severe side effect profile compared to systemic therapy. This review will provide a summary of past and current clinical studies investigating topical FNS therapy for AGA.
METHODS
A primary literature search was conducted using PubMed/MEDLINE, Embase, PsycINFO, TRIP Cochrane Library, and Cochrane Skin databases with search terms”[topical finasteride], [finasteride solution], [finasteride liquid], [finasteride foam], and [finasteride cream]”. Given the focus of this article is the clinical application of topical FNS in humans, only studies regarding human in vivo topical FNS treatment efficacy were reviewed for inclusion; clinically relevant systematic reviews, randomized controlled trials, and open studies were considered. Inclusion criteria were studies involving at least one treatment group with topical FNS, inclusion of results regarding efficacy of topical FNS, and the use of in vivo treatment only. Excluded studies included those that were not written in English, involved treatment with oral FNS only, and those that addressed only the mechanism or pharmacodynamics of the topical FNS. Included studies were graded using the Oxford Center for Evidence-Based Medicine 2011 Levels of Evidence.
RESULTS
119 articles were found using the methodology outlined above. Of these, 67 records were identified by title, and further narrowed to seven records after inclusion criteria were applied and duplicates were removed. Of the reviewed articles, six were published in the last eight years, while one was published 20 years ago, and include five RCTs and two prospective studies. Three studies compare topical to oral FNS, two compare topical MNX to a topical combination of MNX and FNS, one compares combination topical treatments containing FNS, and one compares varying doses and frequencies of topical FNS application. A total of 256 (24 female, 232 male) human subjects were studied (Figure 1, Table 1).
Figure 1:
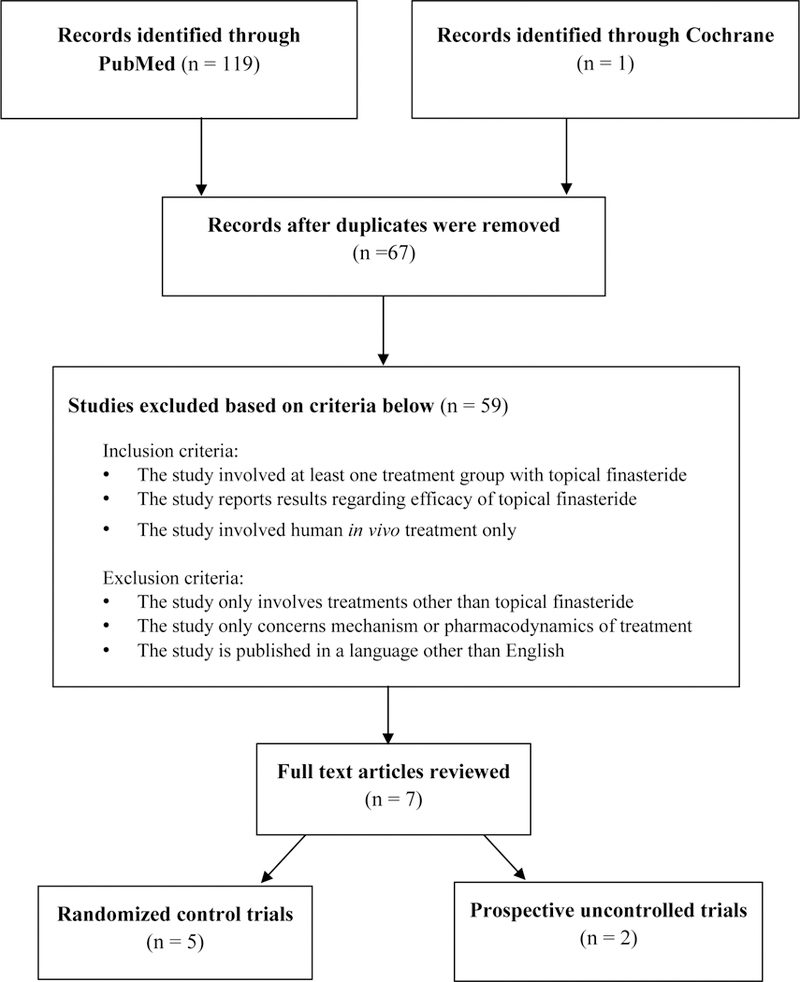
Selecting clinically relevant articles on the use of topical FNS in human subjects with AGA.
Table 1:
Summarizing the use of topical FNS in animal models.
| Author | Sample size | Treatment(s) | Assessments | Study Outcome |
|---|---|---|---|---|
| Noubarani et al. (2014) | 26 male albino mice (ages 2–3 mo) |
Topical testosterone solution only vs. testosterone + FNS 2% vs. testosterone + A. capillus-veneris extract 1% vs. control for 21 days | Number of follicles/mm Anagen:telogen ratio | Mice treated with topical testosterone + A. capillus veneris demonstrated less hair loss compared to those treated with testosterone only. Follicular density and anagen:telogen ratio was highest in topical testosterone + FNS treated animals. |
Assessing systemic pharmacodynamics of topical finasteride
The first study on topical finasteride in humans was completed in 1997 by Mazarella et al.as a single-blind, placebo-controlled study, including 28 males and 24 females patients with AGA. Subjects were randomized to receive either 1.0 mL topical FNS 0.005% solution or placebo twice daily to the affected scalp for 16 months. Pharmacodynamic data revealed no significant change in plasma levels of total testosterone, free testosterone, and DHT between the groups. At sixth months, researchers observed a significant decrease in the rate of hair loss in the topical FNS compared to the placebo group. Patients’ opinion on the effectiveness of treatment was generally positive among the FNS group, with 73% of treated patients reporting “high effectiveness”, compared to 60% of placebo patients reporting “no effect”.10
Five years later, a double-blind, randomized clinical trial with 45 AGA male patients compared topical FNS gel 1% to the scalp twice daily with oral placebo tablets to oral FNS 1 mg daily with a control vehicle applied to the scalp twice daily. In A group (FNS gel and placebo tablet), increased terminal hair counts were observed at the third month of treatment (p = 0.001); however, increased hair counts were noted one month earlier in the B group (FNS tablet and placebo gel). During the therapeutic period, the size of alopecia area(s) was not significantly altered in group A, but in group B the change in alopecia area was significant at the fourth month of treatment and both groups demonstrated increased hair counts with moderate therapeutic response with no difference noted between treatment groups. 11
Studies comparing topical FNS 0.25% (2.275 mg/mL) (P-3074) to systemic FNS 1 mg tablets for AGA therapy have shown that both therapies significantly suppress plasma DHT levels. Caserini et al. randomized 24 male patients in a single-center, open-label, parallel-group, exploratory study with subjects either applying topical solution to their shaved scalp twice daily, or taking a tablet once daily for seven days. Although there is decreased absorption of topical FNS compared to oral, the authors noted a decrease in plasma DHT levels after one week of treatment with either topical or oral formulations. This study provides the first evidence that topical FNS slows AGA-associated hair loss by modulating DHT levels, while also reducing systemic exposure to the medication.12
A follow-up study also by Caserini et al. further examined the dose-dependent effects of topical FNS using a randomized, parallel-group design. The first part of this study examined 18 male patients applying 1 mL of topical FNS 0.25% solution to the scalp once or twice daily, versus administration of oral FNS 1 mg tablet once daily for seven days. There were an increase in alanine aminotransferase, pollakiuria, and testicular pain reported in two participants. In the second part, a group of 32 men received either placebo, or 100 μL (0.2275mg), 200 μL (0.455 mg), 300 μL (0.6285 mg) or 400 μL (0.91 mg) topical FNS 0.25% solution to apply to the scalp once daily for seven days. Interestingly, the results suggest that once daily application of topical FNS is more efficacious at decreasing scalp and plasma DHT levels than twice daily application, and is non-inferior to oral FNS administration. There was no significant differences noted between the varying concentrations of topical FNS, however 300 and 400 μL doses are associated with higher plasma concentrations of FNS, and therefore at greater risk for systemic side effects. Presyncope, conjunctivitis, headache, and oropharyngeal pain were rarely reported. The authors concluded that 100 and 200 μL doses of topical FNS applied daily may be the most effective treatment regimen for AGA.13
Combining topical finasteride with other agents
Research has also been completed to demonstrate the efficacy of topical FNS for AGA in comparison to topical combination therapies. A novel combination topical treatment by the name NuH Hair [topical FNS, dutasteride and minoxidil (MNX)], was formulated by Rafi and Katz (2011). 15 male patients were asked to apply the solution daily for nine months and were given the option of adding three further components to their treatment protocol: 1) oral FNS 1 mg daily 2) topical MNX 5% foam applied at least once per day, and/or 3) topical ketoconazole 2% shampoo applied 2–3 times per week. Eight subjects chose aggressive treatment with all four treatment modalities simultaneously. While all 15 patients demonstrated significant growth of hair by the end of the treatment period, the eight patients who utilized all four treatment options experienced significant growth in as little as 30 days; for the patients using topical FNS/dutasteride/MNX alone, significant hair growth was experienced after three months. The topical FNS/dutasteride/MNX was formulated as a hypoallergenic lotion and found to be safe even in subjects with atopy.14
A randomized, double-blind, comparative study assessed the efficacy and safety of twice daily topical MNX 3% versus topical combined MNX 3%/FNS 0.1% in 40 men with AGA for 24 weeks. Both groups demonstrated increased hair counts from baseline with the MNX 3%/FNS 0.1% group showed statically superior improvement compared to the MNX group.15 Further studies with retrospective assessment and prospective cohort tested a higher concentration of topical MNX 5%/FNS 0.1% for one year on 50 AGA men who were previously treated with oral FNS 1 mg daily and topical MNX 5% twice a day for two years. Approximately 80% of patients either maintained or improved their baseline hair density using topical combination therapy.16
DISCUSSION
Topical application of FNS in the treatment of AGA is an area of research in its infancy and limited to a small number of randomized-controlled trials, prospective studies, and retrospective medical record review. Overall data from the studies on investigating the efficacy and safety of topical FNS in the AGA show promising results and non-inferiority compared to systemic delivery.
Although preliminary results on the use of topical FNS are limited, the studies reviewed demonstrate that topical FNS may be safe for use in patients wishing to avoid systemic side effects. This may be especially important for the AGA population in female, in which systemic FNS is not approved due to hormonal suppression, considering that it is a category X drug during pregnancy.8 It is possible that topical FNS will follow the same path as topical retinoid derivatives (category C)17 and their parent systemic drug isotretinoin (category X),18 with the topical formulation of FNS considered relatively safe for use in pregnant females if the benefits outweigh the risk.
With consistent inhibitory effects on scalp DHT levels while minimizing the systemic effects on serum DHT, doses of 100 μL (0.2275mg) and 200 μL (0.455 mg) topical FNS 0.25% solution applied daily appears to be the most efficacious concentration and frequency at this time.13 The use of topical FNS has not resulted in the report of serious side effects; however, there are reports of scalp irritation manifesting as erythema and contact dermatitis, as well as cases of increased liver enzymes, bed-wetting, testicular pain, headaches, presyncope and oropharyngeal pain (Table 1).11,13,15 Although current evidence suggests that patients are satisfied and that the drug is well-tolerated, we believe large cohort studies examining the potential adverse effect profile of the drug are warranted.
Several challenges arise from the available studies on topical FNS including the vehicle, concentration, as well as application regimen and frequency. The delivery of topical pharmacologic drug to any dermatologic disease state is a heavily studied and debated subject; pharmacokinetic and -dynamic properties, solubility, concentration, potency, drug-drug interactions, absorption, and degradation are dependent on the exact formulation of the vehicle. For the treatment of AGA, the variable efficacy of topical FNS formulations likely depends on the composition of the vehicle.19 Currently, topical formulations of FNS have been tested as gels and solutions at varying concentrations; all of which have resulted in improved hair growth.10, 11, 12, 13, 14, 15, 16
There is no study comparing vehicle delivery (gel vs. solution), and it is unknown which formulation is the most effective at penetrating the scalp, stabilizing FNS over a period of time (i.e. prolonging shelf-life), delivering drug and producing hair regrowth. Combining topical FNS with MNX and/or dutasteride has shown greater efficacy at hair regrowth than topical MNX alone14 and also allowed for the maintenance of hair density. Researchers have optimized the penetration of FNS into the dermis by modulating the type and size of particles transporting the medication across the skin. Studies evaluating the efficacy of nanoparticle delivery have shown enhanced absorption of FNS with smaller particles, particularly with the liquid crystalline variation.20,21 Liposomes and microplated films are also successful delivery methods, as well as the use of absorption enhancers, such as ethanol and propylene glycol.22,23,24A head-to-head comparison of compounds used to deliver nanoparticles has yet to be done, and no conclusions can be drawn at this time regarding which will be most efficacious, with the least amount of adverse events, and the most cost-effective. Although most studies apply topical solution twice daily, once daily application of topical FNS is more effective at decreasing scalp DHT levels. 13 Other studies revealed that combination of topical medications such as MNX 5% with FNS 0.1% may have synergistic and additive effects compared to single agent usage.14, 15, 16
In the future, further research clarifying an optimal drug-delivery system, ideal concentration and frequency of the drug application, the adverse effect profile, as well as use in other hair loss disorders is required to determine the full extent to which topical FNS may be used.
CONCLUSION
AGA is a debilitating chronic condition, causing a great deal of psychological patient morbidity and decreased patient quality of life. Preliminary results regarding the application of topical FNS for the treatment of AGA are promising. Current data suggests that there may be a therapeutic potential for topical FNS in the treatment of AGA, while minimizing unwanted systemic side effects associated with oral use. Topical FNS appears to be non-inferior for hair regrowth when compared to systemic FNS. Combination therapies including topical FNS, as well as MNX or dutasteride, may be more effective than topical FNS alone. Topical FNS is not widely used despite its proven efficacy and lack of side effects, most likely due to the lack of evidence-based research. At this time it is unknown whether the cost of compounding topical FNS is a barrier to treatment. Given the benefits of topical FNS in both male and female AGA patients, further studies are warranted to determine the efficacy of long-term hair regrowth, therapeutic safety, cost-effectiveness, patient tolerability and satisfaction.
Table 2:
Summarizing the results of studies demonstrating the use of topical FNS for the treatment of AGA.
| Author | Level of Evidence |
Sample size |
Study Design |
Treatment(s) | Assessments | Study Outcome and Adverse Events |
|---|---|---|---|---|---|---|
| Mazarella et al. (1997) | 2 | 52 subjects total: 28 male, 24 female, age range 18–38 y/o |
RCT | Topical FNS 0.005% vs. placebo for 16 months |
Physician
Assessments: Photograph 6 point hair regrowth scale “Wash test” Subject Assessments: Subjective four-point scale of effectiveness (0 to 3, with 0 being no effect, and 3 being high effectiveness) |
Significant decrease in rate of hair loss in FNS group after 6 months of treatment. Slight to marked reduction in balding areas in all FNS patients compared to baseline; placebo patients experienced no reduction. 73% of patients in FNS group reported moderate treatment effectiveness, 70% of the placebo group reported no to slight treatment effectiveness. Adverse Events: 30% subjects withdrew from the placebo group due to treatment non-efficacy. No reported local or systemic effects in treatment or placebo groups. |
| Hajheydari et al. (2009) |
2 | 38 male subjects, mean age 22.8 +/− 3 years | RCT | Topical FNS 1% with placebo oral tablet vs. oral FNS 1 mg with placebo gel for 6 months | Size of bald area Total hair count Terminal hair count |
Statistically significant increase in total and terminal hair count compared to baseline in both groups after 4 months. Significant size decrease of bald area compared to baseline in oral FNS group only. No significant difference between the two groups in hair thickness, total hair counts and the size of bald area. Adverse Events: Erythema of scalp after application of topical FNS (n = 1). Decreased libido with use of systemic FNS (n= 1). |
| Rafi and Katz(2011) | 3 | 15 male subjects, age range 24–72 y/o | Prospective cohort | NuH hair (topical FNS, dutasteride, MNX) with the option to add oral FNS, MNX, and/or ketoconazole shampoo for 9 months |
Photographs | All patients demonstrated significant growth of hair compared to baseline. In those patients who utilized all 4 components, significant growth compared to baseline was achieved in as little as 30 days. In those patients who chose to apply NuH Hair only, significant growth compared to baseline was demonstrated after 3 months. Adverse Events: No report of contact or irritant dermatitis were reported with the use of NuH Hair. |
| Tanglertsampan (2012) | 2 | 33 male subjects, age range 27–49 y/o | RCT | Topical MNX 3% alone vs. MNX 3% + FNS 0.1% (MFX) for 24 weeks | Hair count Photographs |
Hair count increased in both groups, but was only significantly improved from baseline in the MFX group. MFX showed significantly higher efficacy by global photographic assessment compared to MNX. Adverse Events: Contact dermatitis experienced in MNX group n = 6 (38%), MFX group n = 4 (24%). |
| Caserini et al. (2014) | 2 | 23 male subjects, age range 18–65 y/o | RCT | Topical FNS 0.25% twice daily vs. oral FNS 1 mg once daily for 7 days | DHT and testosterone levels in plasma | Plasma DHT was reduced by 68–75% with use of topical FNS and by 62–72% with systemic administration. No relevant changes occurred for plasma testosterone with either treatment. Adverse Events: No clinically significant adverse events occurred. |
| Caserini et al. (2015) |
2 | 50 male subjects, age range 18–65 y/o | RCT |
Study 1: 1 mL topical FNS 0.25% daily vs. 1 mL topical FNS 0.25% twice daily vs. oral FNS 1 mg daily for 7 days Study 2: Placebo vs topical FNS 0.25% twice daily in varying quantities 100 μl vs. 200 μl vs. 300 μl vs. 400 μl for 7 days |
DHT concentration in scalp and plasma Testosterone levels in plasma FNS levels in plasma |
Study 1: 70% decrease from baseline in scalp DHT after application of 1 mL topical FNS daily compared to 50% decrease from baseline for both 1 mL topical FNS twice daily or oral FNS. Study 2: Scalp DHT reduction was decreased by 47–52% using 100 μl and 200 μl of topical FNS, which was similar to the 37% and 54% reduction seen with 300 μl and 400 μl respectively. Serum DHT was reduced by 24%, 26%, 44%, and 48% by 100 μl, 200 μl, 300 μl, and 400 μl respectively. No significant changed occurred in serum testosterone levels. Adverse Events: Study 1: Increased alanine aminotransferase, pollakiuria and testicular pain (n = 2, 11.1%) Study 2: Presyncope, conjunctivitis, headache, oropharyngeal pain (n = 5, 15.6%) |
| Chandrashekar et al. (2017) | 3 | 50 male subjects, age range 20–40 y/o | Retrospec-tive assessment and Prospective cross-over cohort | Topical MNX 5% and oral FNS 1 mg for 2 years, followed by either topical MNX 5% + FNS 0.1% (MFX) for 1 year either immediately or after 8–12 months without treatment | Photographs | 45 subjects underwent continuous treatment with MNX and oral FNS for 2 years and then treatment was continued with MFX. –Of these patients, 84.4% maintained good hair density while on MFX. 5 subjects underwent continuous treatment with MNX and oral FNS for 2 years, were discontinued from all treatments for 8–12 months, and then treatment was continued with MFX. –Of these patients 80% maintained good hair density while on MFX. Adverse Events: No adverse events were reported with either treatment. Patient compliance was good with topical finasteride. |
Acknowledgments
The authors received no financial support for this research.
Abbreviations:
- AGA
Androgenetic alopecia
- AR
androgen receptors
- DHT
dihydrotestosterone
- EMA
European Medicines Agency
- FDA
Food and Drug Administration
- FNS
finasteride
- MNX
minoxidil
- RCT
randomized controlled trial
Footnotes
Disclosure:
The authors have no conflicts of interest to disclose.
References
- 1.Lolli F, Pallotti F, Rossi A, Fortuna MC, et al. Androgenetic alopecia: a review. Endocrine. 2017;57(1):9–17. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Food & Drug Administration: Drug Databases. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2006/021812s000TOC.cfm. Accessed July 07, 2017.
- 3.Robinson J Hair transplants: what to expect. WebMD. https://www.webmd.com/skin-problems-and-treatments/hair-loss/men-hair-loss-17/hair-transplants. Published December 18, 2016. Accessed July 04, 2017. [Google Scholar]
- 4.Inui S, Itami S. Androgen actions on the human hair follicle: perspectives. ExpDermatol.2012. doi: 10.1111/exd.12024. [DOI] [PubMed] [Google Scholar]
- 5.El-Domyati M, Attia S, Saleh F, et al. Androgenetic alopecia in males: a histopathological and ultrastructural study. J CosmetDermatol. 2009;8(2)83–91. [DOI] [PubMed] [Google Scholar]
- 6.Trueb RM. Molecular mechanisms of androgenetic alopecia.TherUmsch. 2002;59(5)211–6. [Google Scholar]
- 7.Finn DA, Beadles-Bohling AS, Beckley EH, et al. A new look at the 5alpha-reductase inhibitor finasteride. Cns Drug Rev. 2006;12:53–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S. Food & Drug Administration: Drug Databases. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/020788s018lbl.pdf Accessed July 07, 2017.
- 9.Noubarani M, Rostamkhani H, Erfan M, Kamalinejad M, Eskandari MR, Babaeian M, Salamzadeh J. Effect of adiantum capillus veneris linn on an animal model of testosterone-induced hair loss. Iran J Pharm Red. 2014. Winter; 13(Suppl): 113–118. [PMC free article] [PubMed] [Google Scholar]
- 10.Mazzarella GF, Loconsole GF, Cammisa GA, Mastrolonardo GM, Vena G. Topical finasteride in the treatment of androgenic alopecia. Preliminary evaluations after a 16-month therapy course. J of Derm Tr. 1997;8(3):189–92. DOI: 10.3109/09546639709160517. [DOI] [Google Scholar]
- 11.Hajheydari Z, Akbari J, Saeedi M, Shokoohi L. Comparing the therapeutic effects of finasteride gel and tablet in treatment of the androgenetic alopecia. Exp Gerontol. 2002;37(9–0)981–90. [DOI] [PubMed] [Google Scholar]
- 12.Caserini M1, Radicioni M, Leuratti C, et al. A novel finasteride 0.25% topical solution for androgenetic alopecia: pharmacokinetics and effects on plasma androgen levels in healthy male volunteers. Int J Clin Pharmacol Ther. 2014;52(10):842–9. [DOI] [PubMed] [Google Scholar]
- 13.Caserini M, Radicioni M, Leuratti C, et al. Effects of a novel finasteride 0.25% topical solution on scalp and serum dihydrotestosterone in healthy men with androgenetic alopecia. Int J ClinPharmacolTher. 2016;54(1):19–27. [DOI] [PubMed] [Google Scholar]
- 14.Rafi AW, Katz RM. Pilot study of 15 patients receiving a new treatment regimen for androgenic alopecia: the effects of atopy on AGA. ISRN Dermatol. 2011; 2011: 241953 Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tanglertsampan C Efficacy and safety of 3% minoxidil versus combined 3% minoxidil/0.1% finasteride in male pattern hair loss: a randomized, double-blind, comparative study. J Med Assoc Thai. 2012;95(10):1312–6. [PubMed] [Google Scholar]
- 16.Chandrashekar BS, Nandhini T, Sriram R, Navale S. Topical minoxidil fortified with finasteride: An account of maintenance of hair density after replacing oral finasteride. Indian Dermatol Online J. 2015. Jan-Feb; 6(1): 17–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.U.S. Food & Drug Administration: Drug Databases. https://www.fda.gov/ohrms/dockets/dockets/05p0417/05p-0417-sup0001-03-Retin-A-Labeling-vol2.pdf Accessed October 04, 2017
- 18.U.S. Food & Drug Administration: Drug Databases https://www.accessdata.fda.gov/drugsatfda_docs/label/2002/18662s051lbl.pdf Accessed July 04, 2017
- 19.Sintov A, Serafimovich S, Gilhar A. New topical antiandrogenic formulations can stimulate hair growth in human bald scalp grafted onto mice. Int J of Pharmaceutics 194 (2000) 125–134. [DOI] [PubMed] [Google Scholar]
- 20.Roque LV, Dias IS, Cruz N, Rebelo A, Robert A, Rijo P, Reis CP. Design of Finasteride-loaded nanoparticles for potential treatment of alopecia. Skin Pharmacol Physiol. 2017. July 8: 30 (4): 197–204. [DOI] [PubMed] [Google Scholar]
- 21.Gomes MJ, Martins S, Ferreira D, Segundo M, Reis S. Lipid nanoparticles for topical and transdermal application for alopecia treatment: development, physiochemical characterization, and in vitro release and penetration studies. Skin Pharmacol Physiol. 2017. July 8; 30 (4): 197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumar R, Singh B, Bakshi G, Katare OP. Development of liposomal systems of finasteride for topical applications: designs, characterization, and in vitro evaluation. Pharm Dev Technol. 2007; 12(6):591–601. [DOI] [PubMed] [Google Scholar]
- 23.Ahmed TA, El-Say KM. Transdermal film-loaded finasteride microplates to enhance drug skin permeation: two-step optimization study. Eur J Pharm Sci. 2016. June 10; 88: 246–56. [DOI] [PubMed] [Google Scholar]
- 24.Tabbakhian M, Tavakoli N, Jaafari MR, Daneshamouz S. Enhancement of follicular delivery of finasteride by liposomes and niosomes 1. In vitro permeation and in vivo deposition studies using hamster flank and ear models. Int. J Pharm 2006. October 12; 323(1–2):1–10. [DOI] [PubMed] [Google Scholar]


