Abstract
Daidzein isolated from soybean (Glycine max) has been widely studied for its antioxidant and anti-inflammatory activities. However, the protective effects of 7,8,4′-trihydroxyisoflavone (THIF), a major metabolite of daidzein, on 6-hydroxydopamine (OHDA)-induced neurotoxicity are not well understood. In the current study, 7,8,4′-THIF significantly inhibited neuronal cell death and lactate dehydrogenase (LDH) release induced by 6-OHDA in SH-SY5Y cells, which were used as an in vitro model of Parkinson’s disease (PD). Moreover, pretreatment with 7,8,4′-THIF significantly increased the levels of superoxide dismutase (SOD), catalase (CAT), and glutathione (GSH) and decreased malondialdehyde (MDA) activity in 6-OHDA-induced SH-SY5Y cells. In addition, 7,8,4′-THIF significantly recovered 6-OHDA-induced cleaved caspase-3, cleaved caspase-9, cleaved poly-ADP-ribose polymerase (PARP), increased Bax, and decreased Bcl-2 levels. Additionally, 7,8,4′-THIF significantly restored the expression levels of phosphorylated c-Jun N-terminal kinase (JNK), p38 mitogen-activated protein kinase (MAPK), extracellular signal-regulated kinase 1/2 (ERK 1/2), phosphatidylinositol 3-kinases (PI3K)/Akt, and glycogen synthase kinase-3 beta (GSK-3β) in 6-OHDA-induced SH-SY5Y cells. Further, 7,8,4′-THIF significantly increased the reduced tyrosine hydroxylase (TH) level induced by 6-OHDA in SH-SY5Y cells. Collectively, these results suggest that 7,8,4′-THIF protects against 6-OHDA-induced neuronal cell death in cellular PD models. Also, these effects are mediated partly by inhibiting activation of the MAPK and PI3K/Akt/GSK-3β pathways.
Keywords: 7,8,4′-Trihydroxyisoflavone; 6-Hydroxydopamine; Neurotoxicity; Apoptosis; Parkinson’s disease
INTRODUCTION
Black soybeans (Glycine max) have been used for hundreds of years in Oriental medicine as a food source to promote human health and protect against numerous diseases (Lee and Chou, 2006). In particular, black soybeans have a variety of beneficial properties such as antioxidant and anti-aging effects (Xu and Chang, 2008). As one of the important components of black soybeans along with genistein, daidzein has been mainly investigated for its antioxidant and anti-inflammatory activities (Li et al., 2014; Eren-Guzelgun et al., 2018). This isoflavone is readily bioconverted to various metabolized forms, such as 7,8,4′-trihydroxyisoflavone (7,8,4′-THIF, Fig. 1) and 6,7,4′-THIF, in the human body (Heinonen et al., 2003). Among these metabolized products derived from daidzein, 7,8,4′-THIF possesses beneficial properties for human health, including anti-atopic and antioxidant effects (Kim et al., 2014), as well as anti-neuroinflammatory activity, in lipopolysaccharide (LPS)-stimulated BV-2 microglial cells (Wu et al., 2018). Moreover, 7,8,4′-THIF could be a potential functional food source due to its prevention effect on the risk of cardiovascular diseases (Lee et al., 2018). However, the effects of 7,8,4′-THIF on neurotoxin-induced oxidative stress and neuronal cell death are poorly understood.
Fig. 1.
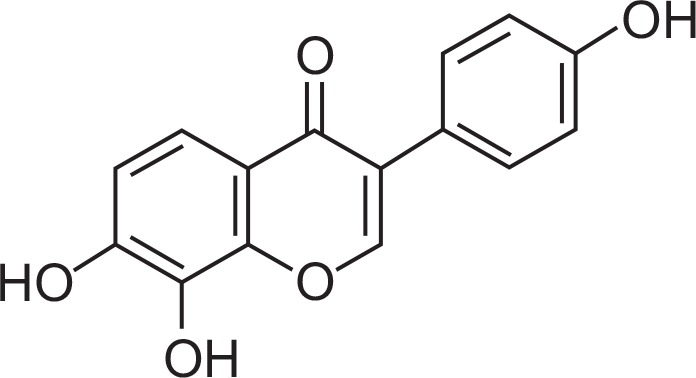
Chemical structure of 7,8,4′-THIF.
Parkinson’s disease (PD) is a progressive nervous system disorder that affects approximately 1% of the population by age 65 (Eriksen et al., 2003). PD is characterized by loss of dopaminergic neurons in the substantia nigra pars compacta, leading to a significant reduction in dopamine level in the striatum (Rodriguez-Oroz et al., 2009). The major motor symptoms of PD are tremors, rigidity, bradykinesia, and impaired balance (Yu et al., 2016), and many studies have demonstrated that oxidative stress may be closely related to the pathogenesis and aggravation of motor decline in PD (Yuan et al., 2007). In particular, increased oxidative stress, dysfunction of the anti-oxidant system, and mitochondrial damage have been shown to induce apoptotic processes in various cellular systems (Blum et al., 2001). Therefore, attenuation of oxidative stress may be an important strategy for treatment and/or prevention of PD.
6-Hydroxydopamine (OHDA) has been widely used to produce oxidative stress associated with damage to dopaminergic neurons. Therefore, 6-OHDA is a well-known neurotoxin for inducing PD in vitro and in vivo (Kopalli et al., 2013) including in the human neuroblastoma SH-SY5Y cell line (Guo et al., 2005). 6-OHDA induces neuronal cell death by inhibiting antioxidant systems including reducing the levels of glutathione (GSH), catalase (CAT), and superoxide dismutase (SOD) and inducing mitochondrial deficits (Kwon et al., 2012; Park et al., 2017). In addition, the neurotoxin 6-OHDA stimulates several pro-apoptosis molecular factors for mitogen-activated protein kinases (MAPKs) including extracellular signal-regulated kinase 1/2 (ERK1/2), p38, c-Jun N-terminal kinase (JNK), phosphatidylinositol 3-kinases (PI3K)/Akt, and glycogen synthase kinase-3 beta (GSK-3β) (Kim and Choi, 2010; Kwon et al., 2014).
In the present study, the effects of 7,8,4′-THIF, a metabolic product of daidzein, on 6-OHDA-induced neurotoxicity and cell viability were investigated in human neuroblastoma SH-SY5Y cells as a model of PD. To evaluate the possible mechanism(s) underlying the effects of 7,8,4′-THIF against 6-OHDA-induced apoptotic cell death, we measured the levels of SOD, CAT, GSH, and malondialdehyde (MDA), as well as lactate dehydrogenase (LDH) release, in SH-SY5Y cells. To determine the effects of 7,8,4′-THIF on 6-OHDA-induced apoptosis pathways, we assessed the expression levels of Bax, Bcl-2, cleaved caspase-3, cleaved caspase-9, and cleaved poly-ADP-ribose polymerase (PARP), as well as the activation of MAPK and PI3K/Akt/GSK-3β cascades, using Western blotting. Finally, we determined the level of tyrosine hydroxylase (TH), an important rate-limiting enzyme in dopamine metabolism, in 6-OHDA-stimulated SH-SY5Y cells.
MATERIALS AND METHODS
Chemicals and reagents
7,8,4′-THIF was purchased from Indofine Chemical Company (San Mateo, CA, USA). 3-(4,5-Dimethyl thiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT), anti-β-actin antibody, dimethyl sulfoxide (DMSO), 6-OHDA, and Tween 20 were purchased from Sigma Chemicals (St. Louis, MO, USA). Dulbecco’s modified Eagle’s medium (DMEM) was obtained from HyClone (Logan, UT, USA). Fetal bovine serum (FBS), 0.25% trypsin-EDTA, and penicillin/streptomycin were obtained from Gibco–BRL (Grand Island, NY, USA). Dulbecco’s phosphate-buffered saline (D-PBS) was obtained from Wel-gene (Gyeongsan, Korea). Rabbit anti-Bax, rabbit anti-Bcl-2, rabbit anti-caspase-3, rabbit anti-caspase-9, rabbit anti-PARP, rabbit anti-phospho Erk1/2 (Thr202/Tyr204), rabbit anti-Erk1/2 (Thr202/Tyr204), rabbit anti-phospho JNK (Thr183/Tyr185), rabbit anti-phospho GSK-3β (D75D3), and rabbit anti-GSK-3β antibodies were purchased from Cell Signaling Technology (Boston, MA, USA). Rabbit anti-JNK, rabbit anti-phospho p38 MAPK (Thr180/Tyr182), and rabbit anti-p38 MAPK antibodies were purchased from Epitomics (Burlingame, CA, USA). Rabbit anti-TH antibody was purchased from Merck Millipore (Darmstadt, Germany). Secondary antibodies were purchased from Jackson ImmunoResearch Laboratories (West Grove, PA, USA). All other chemicals were of analytical grade.
Cell culture and treatment
Human neuroblastoma SH-SY5Y cells (catalog #CRL-2266, RRID: CVCL_0019) were obtained from the ATCC (Manassas, VA, USA) and were maintained in DMEM supplemented with 10% heat-inactivated FBS and 0.1% penicillin/streptomycin at 37°C in a humidified atmosphere of 5% CO2 and 95% air. The medium was replaced every 3 days until the cells reached 80–90% confluency in 100-mm2 cell culture dishes. For subcultures, SH-SY5Y cells were dissociated with trypsin-EDTA and subcultured in culture dishes. 6-OHDA was prepared as a 20 mM stock solution immediately before use and diluted in PBS to the final concentration. The test compound was dissolved in DMSO, and the stock solution was added to the culture media to a final concentration of 0.1% (v/v) DMSO.
Measurement of cell viability
SH-SY5Y cells were plated in 96-well plates (2.5×104 cells/well). After pretreatment with either 7,8,4′-THIF (1, 2.5, 5, 10, or 20 μM) or vehicle (0.1% v/v DMSO) for 30 min, the cells were incubated with 200 μM 6-OHDA for 24 h and subsequently treated with MTT solution (5 mg/ml). In addition, in order to avoid the direct molecular reaction of 7,8,4′-THIF with 6-OHDA present in the cell culture medium, the cells were pre-treated with 7,8,4′-THIF for 1 h, washed three times with PBS, and then incubated with 6-OHDA for 24 h in another group of experiments (Tian et al., 2007). The dark blue formazan crystals formed in the viable cells were dissolved in DMSO, and the absorbances at 540 nm were measured with a microplate reader (SpectraMax 250, Molecular Device, Sunnyvale, CA, USA).
Measurement of LDH release
LDH release was spectrophotometrically measured using a Cytotoxicity Cell Death kit (Takara Bio, Shiga, Japan) according to the manufacturer’s instructions. SH-SY5Y cells (2.5×104 cells/well in 96-well plates) with or without 7,8,4′-THIF pre-treatment were incubated at 37°C with 200 μM 6-OHDA for 24 h, and the cell supernatant was collected and assayed. Then, the total protein amounts were normalized using a protein assay kit (Thermo Scientific, Rockford, IL, USA). The reaction mixture (100 μl) was added to each well and incubated for 30 min at room temperature. The absorbance at 490 nm was measured using a microplate reader, and the LDH expressed due to cytotoxicity (%) was calculated using the following formula: % of LDH release=[(LDH activity in the medium)/(LDH activity in the medium+LDH activity in the cell)]×100.
Measurement of SOD and CAT activities and GSH content
SOD and CAT activities and GSH content were measured using commercial assay kits (BioVision, Milpitas, CA, USA). SH-SY5Y cells (5×105 cells/well in 6-well plates) with or without 7,8,4′-THIF pretreatment were incubated at 37°C with 200 μM 6-OHDA for 24 h. The medium was then removed, and the cells were harvested. The cells were washed with ice-cold PBS, dissociated with cell lysis buffer, and centrifuged for 5 min (15,000×g). The cell pellet was resuspended in 500 μl of ice-cold buffer and lysed via vortexing. The cell suspension was then used for assays according to the manufacturer’s protocols (BioVision). The total protein amounts were normalized for avoiding the pure cell-killing toxic effect of 6-OHDA. The absorbance of all samples was measured using a microplate reader (SpectraMax 250, Molecular Device) at 450 nm for SOD, 570 nm for CAT, and 405 nm for GSH.
Measurement of MDA level
SH-SY5Y cells (5×105 cells/well in 6-well plates) were incubated at 37°C with 200 μM of 6-OHDA for 6 h with or without 7,8,4′-THIF pretreatment. The medium was then removed, and the cells were harvested. The cells were washed with ice-cold PBS, dissociated with cell lysis buffer, and centrifuged for 5 min (15,000×g). The total protein amounts were quantified using a protein assay kit (Thermo Scientific). The MDA level in the supernatant was measured using a specific assay kit (Nanjing Jiancheng Bioengineering Institute, Nanjing, China) based on the manufacturer’s instructions.
Western blot analysis
Western blotting was conducted as previously described (Ko et al., 2018b). Briefly, SH-SY5Y cells (5×105 cells/well in 6-well plates) were incubated at 37°C with 200 μM of 6-OHDA for 1 or 6 h with or without 7,8,4′-THIF pretreatment. The cells were then washed, harvested with ice-cold PBS, and centrifuged at 400×g for 3 min. The cell pellet was resuspended in 100 μl of ice-cold T-PER tissue protein extraction buffer (Thermo Scientific) containing protease and phosphatase inhibitor cocktails (Roche Diagnostics, GmbH, Berlin, Germany) and incubated on ice for 30 min. Following centrifugation at 10,000×g for 15 min, the supernatant was isolated and stored at −70°C. The protein concentration was calculated using a protein assay kit (Thermo Scientific). The protein samples were separated using 8–12.5% sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and then transferred onto polyvinylidene difluoride (PVDF) membranes (Pall Corporation, Pensacola, FL, USA) using transfer buffer (25 mM Tri-HCl buffer, pH 7.4, containing 192 mM glycine and 20% v/v methanol) and blocked with 5% non-fat milk in 0.5 mM Tris-HCl (pH 7.5) containing 150 mM NaCl and 0.1% Tween 20 for 1 h at room temperature. Each membrane was incubated in a primary antibody overnight at 4°C. These primary antibodies comprised anti-Bax (1:1000 dilution), anti-Bcl-2 (1:1000), anti-caspase-3 (1:1000), anti-caspase-9 (1:1000), anti-PARP (1:1000), anti-phospho JNK (1:1000), anti-JNK (Thr183/Tyr185) (1:1000), anti-phospho p38 (Thr180/Tyr182) (1:1000), anti-p38 (1:1000), anti-phospho ERK1/2 (Thr202/Tyr204) (1:2000), anti-ERK1/2 (1:2000), anti-phospho Akt (Ser473) (1:1000), anti-Akt (1:1000), anti-phospho GSK-3β (D75D3) (1:1000), anti-GSK-3β (1:1000), and anti-TH (1:1000). After washing the membranes with TBST (Tris-buffered saline with 0.1% Tween 20), the blots were incubated in horseradish-peroxidase-conjugated secondary antibodies (Jackson ImmunoResearch Laboratories, West Grove, PA, USA) for 1 h at room temperature. The band density was determined with enhanced chemiluminescence (ECL) by immersing the probed membrane in a 1:1 mixture of ECL reagents A and B (Animal Genetics, Suwon, Republic of Korea) for 5 min. The membranes were then exposed to photographic film for several minutes. The protein bands were quantified using densitometric analysis with ImageJ software (National Institutes of Health, Bethesda, MD, USA).
Statistical analysis
All data are presented as mean ± SEM and were analyzed using Prism software, version 6.0 (GraphPad Software, San Diego, CA, USA). Statistical analyses were performed using one-way analysis of variance (ANOVA) following by the Newman–Keuls post hoc test for multiple comparisons. Statistical significance was defined as p<0.05.
RESULTS
Effects of 7,8,4′-THIF on 6-OHDA-induced cell viability and LDH release in SH-SY5Y cells
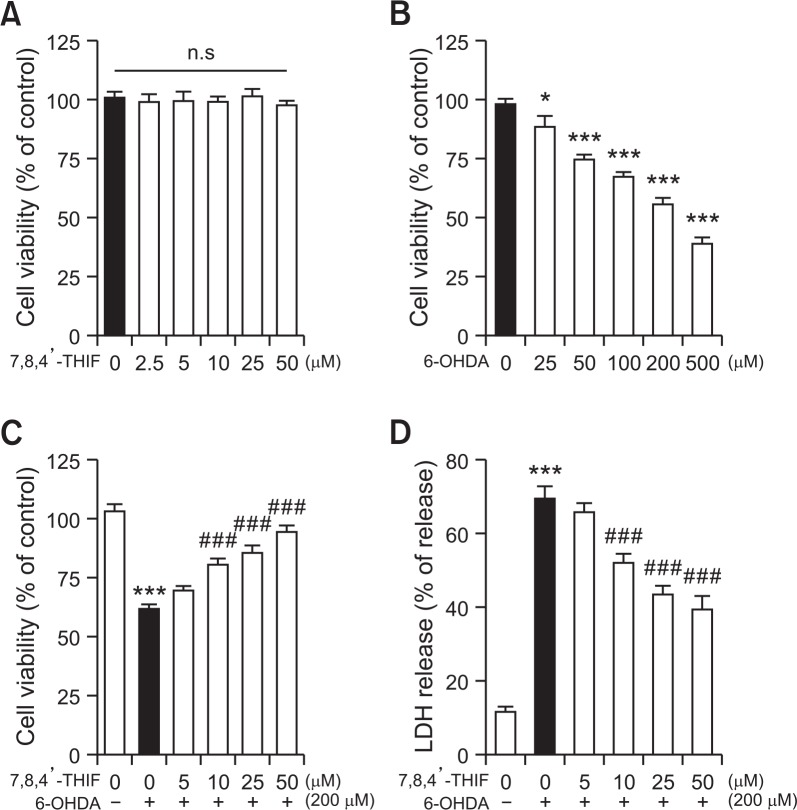
Pretreatment with 7,8,4′-THIF (2.5, 5, 10, 25, or 50 μM) alone did not affect cytotoxicity in SH-SY5Y cells (Fig. 2A). In addition, SH-SY5Y cells were treated with varying doses of 6-OHDA (25, 50, 100, 200, or 500 μM) for 24 h, and the viability of the cells was determined using the MTT formazan assay. As shown in Fig. 2B, all concentrations of 6-OHDA induced significant neuronal cell death in a dose-dependent manner (Fig. 2B, F(5, 30)=52.60, p<0.05 and p<0.001, respectively). Only 55.8% of the cells exposed to 200 μM 6-OHDA remained viable compared with the control group. Therefore, 200 μM 6-OHDA was selected for all subsequent experiments. To assess the effects of 7,8,4′-THIF on neuronal injury, 6-OHDA-induced SH-SY5Y cells were treated with various concentrations of 7,8,4′-THIF. 6-OHDA (200 μM) significantly decreased cell viability (Fig. 2C, F(5, 30)=31.82, p<0.001) and increased LDH release compared with the control group (Fig. 2D, F(5, 30)=59.86, p<0.001). However, pretreatment with 7,8,4′-THIF (10, 25, or 50 μM) significantly ameliorated 6-OHDA-induced cell death (Fig. 2C, p<0.001, p<0.001, and p<0.001, respectively) and LDH release in SH-SY5Y cells (Fig. 2D, p<0.001, p<0.001, and p<0.001, respectively).
Fig. 2.
Effects of 7,8,4′-THIF on viability (A) of SH-SY5Y cells. Dose-dependent cytotoxic effects of 6-OHDA on viability (B) of SH-SY5Y cells. Protective effects of 7,8,4′-THIF on 6-OHDA-induced neuronal cell death (C) and LDH release (D) in SH-SY5Y cells. The cells were pretreated with 7,8,4′-THIF (2.5, 5, 10, 25, or 50 μM) for 30 min followed by exposure to 200 μM 6-OHDA for 24 h. The viability of the cells and LDH release were assessed using MTT and LDH assays, respectively, and are expressed as a percentage of the corresponding values for the control group.The data are presented as mean ± SEM (n=6). *p<0.05 and ***p<0.001 compared with the control group. ###p<0.001 compared with the 6-OHDA-treated group.
Effects of 7,8,4′-THIF on 6-OHDA-induced SOD and CAT activities, GSH content, and MDA level in SH-SY5Y cells
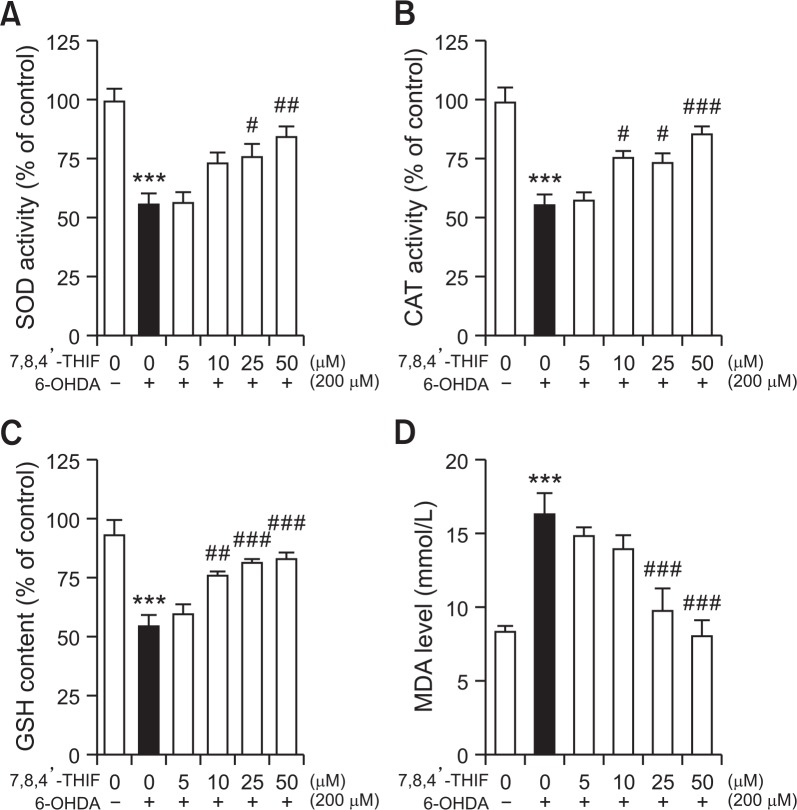
To investigate the effects of 7,8,4′-THIF on 6-OHDA-induced antioxidant enzymes, we assessed the activities of SOD, CAT, and GSH in SH-SY5Y cells. A marked reduction in the activities of SOD (55.4% decrease) (Fig. 3A, F(5, 30)=11.06, p<0.001) and CAT (in 55.1% decrease of the control level) (Fig. 3B, F(5, 30)=14.35, p<0.001), as well as the GSH content (54.1% decrease) (Fig. 3C, F(5, 30)=13.38, p<0.001), were seen after treatment with 6-OHDA (200 μM) compared with the control group. However, the reductions in CAT and GSH levels were significantly restored by 7,8,4′-THIF (10 μM) to 75.1% and 75.6% of the control level, respectively (p<0.05 and p<0.01). In addition, pretreatment with 25 μM 7,8,4′-THIF significantly increased SOD, CAT, and GSH levels to 75.5%, 73.1%, and 81.3% of the control level, respectively (p<0.05, p<0.05, and p<0.001). Pretreatment with 50 μM 7,8,4′-THIF also resulted in significant increases in SOD, CAT, and GSH to 84.0%, 85.1%, and 82.8% of the control level, respectively (p<0.01, p<0.001, and p<0.001). When cells were incubated with 200 μM of 6-OHDA in the absence of 7,8,4′-THIF pretreatment, the MDA level was significantly increased compared with the control cells (Fig. 3D, F(5, 30)=11.14, p<0.001). However, pre-treatment with 7,8,4′-THIF (25 or 50 μM) markedly decreased the level of MDA compared with the 6-OHDA-treated cells (Fig. 3D, p<0.001 and p<0.001, respectively). These results indicate that 7,8,4′-THIF might improve 6-OHDA-induced dysfunction of the antioxidant system in SH-SY5Y cells.
Fig. 3.
Effects of 7,8,4′-THIF on 6-OHDA-induced SOD (A) and CAT (B) activities, GSH content (C), and MDA level (D) in SH-SY5Y cells. The cells were pretreated with 7,8,4′-THIF (5, 10, 25, or 50 μM) for 30 min followed by exposure to 200 μM 6-OHDA for 6 or 24 h. SOD and CAT activities, GSH content, and MDA level were assessed using commercial assay kits and are expressed as a percentage of the corresponding values for the control group. The data are presented as mean ± SEM (n=6). ***p<0.001 compared with the control group. #p<0.05, ##p<0.01, and ###p<0.001 compared with the 6-OHDA-treated group.
Effects of 7,8,4′-THIF on 6-OHDA-induced increased Bax and decreased Bcl-2 expression levels in SH-SY5Y cells
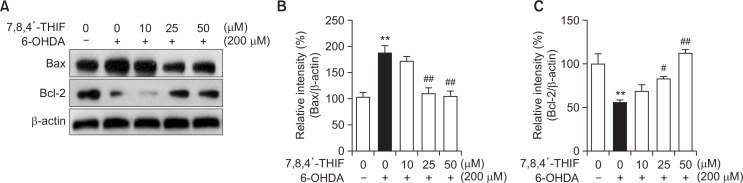
To explore the effects of 7,8,4′-THIF on 6-OHDA-induced Bax and Bcl-2 expression levels, we performed Western blotting on SH-SY5Y cells (Fig. 4A). Treatment of cells with 200 μM 6-OHDA resulted in a significant increase in the level of Bax to 187.5% of the control level (Fig. 4B, F(4, 10)=14.57, p<0.01). In contrast, 6-OHDA treatment significantly decreased the level of Bcl-2 to 55.4% of the control value (Fig. 4C, F(4, 10)=11.07, p<0.05). However, pretreatment with 25 or 50 μM 7,8,4′-THIF significantly recovered the levels of Bax to 109.5% (Fig. 4B, p<0.01) and 105.0% (Fig. 4B, p<0.01) of the control value, respectively. In addition, pretreatment with 25 or 50 μM 7,8,4′-THIF dramatically restored the levels of Bcl-2 to 82.7% (Fig. 4C, p<0.05) and 112.1% (Fig. 4C, p<0.01) of the control group.
Fig. 4.
Effects of 7,8,4′-THIF on 6-OHDA-induced increased Bax and decreased Bcl-2 expression levels in SH-SY5Y cells. The cells were pretreated with 7,8,4′-THIF (10, 25, or 50 μM) for 30 min followed by exposure to 200 μM 6-OHDA for 6 h (A). The expression levels of Bax (B) and Bcl-2 (C) were evaluated using Western blot analysis. The densitometric data are expressed as mean ± SEM (n=3). **p<0.01 compared with the control group. #p<0.05 and ##p<0.01 compared with the 6-OHDA-treated group.
Effects of 7,8,4′-THIF on 6-OHDA-induced expression levels of cleaved caspase-9, cleaved caspase-3, and cleaved PARP in SH-SY5Y cells
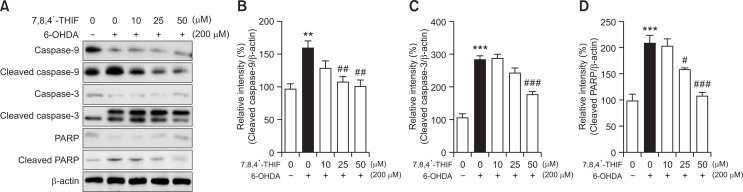
To assess the effects of 7,8,4′-THIF on the underlying apoptotic pathway, we verified the regulation of caspase and PARP proteins using Western blot analysis in 6-OHDA-stimulated SH-SY5Y cells (Fig. 5A). Treatment with 200 μM 6-OHDA resulted in increased expression levels of cleaved caspase-9, cleaved casepase-3, and cleaved PARP to 159.8% (Fig. 5B, F(4, 10)=7.06, p<0.01), 283.0% (Fig. 5C, F(4, 10)=36.88, p<0.001), and 208.5% (Fig. 5D, F(4, 10)=21.35, p<0.001) of the control values, respectively. However, treatment of SH-SY5Y cells with 25 μM 7,8,4′-THIF significantly decreased the levels of cleaved caspase-9 and cleaved PARP to 107.4% (Fig. 5B, p<0.01) and 158.8% (Fig. 5D, p<0.05) compared with the 6-OHDA-treated group, respectively. In addition, treatment with 50 μM 7,8,4′-THIF significantly reduced the 6-OHDA-induced levels of cleaved caspase-9, cleaved caspase-3, and cleaved PARP to 100.7% (Fig. 5B, p<0.01), 176.2% (Fig. 5C, p<0.001), and 107.1% (Fig. 5D, p<0.001) of the control values, respectively. These results indicate that 7,8,4′-THIF effectively inhibits events downstream of the apoptotic pathway, including caspase-9, caspase-3, and PARP activation, in SH-SY5Y cells.
Fig. 5.
Effects of 7,8,4′-THIF on 6-OHDA-induced cleaved caspase-9, cleaved caspase-3, and cleaved PARP expression levels in SH-SY5Y cells. The cells were pretreated with 7,8,4′-THIF (10, 25, or 50 μM) for 30 min followed by exposure to 200 μM 6-OHDA for 6 h (A). The expression levels of cleaved caspase-9 (B), cleaved caspase-3 (C), and cleaved PARP (D) were evaluated using Western blot analysis. Densitometric data are expressed as mean ± SEM (n=3). **p<0.01 and ***p<0.001 compared with the control group. #p<0.05, ##p<0.01, and ###p<0.001 compared with the 6-OHDA-treated group.
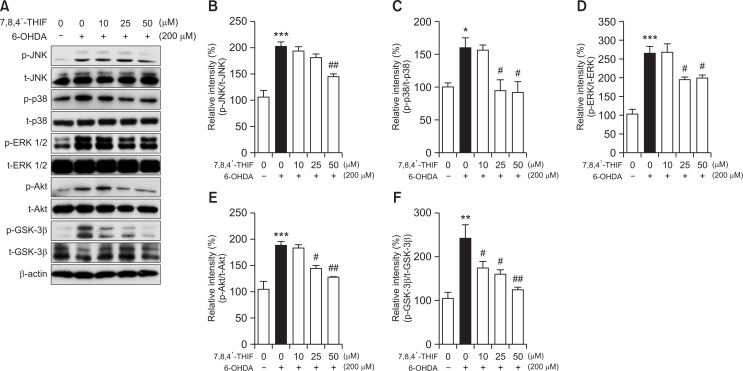
Effects of 7,8,4′-THIF on 6-OHDA-induced expression levels of phosphorylated JNK, p38, ERK 1/2, Akt, and GSK-3β in SH-SY5Y cells
As shown in Fig. 6A, the effects of 7,8,4′-THIF on the 6-OHDA-induced expression levels of phosphorylated JNK, p38, ERK 1/2, Akt, and GSK-3β were assessed using Western blot analysis in SH-SY5Y cells. Treatment with 200 μM 6-OHDA significantly increased the expression of phosphorylated JNK, p38, ERK 1/2, Akt, and GSK-3β to 202.4% (Fig. 6B, F(4, 10)=20.45, p<0.001), 160.4% (Fig. 6C, F(4, 10)=6.98, p<0.05), 265.3% (Fig. 6D, F(4, 10)=19.81, p<0.001), 188.3% (Fig. 6E, F(4, 10)=16.74, p<0.001), and 242.3% (Fig. 6F, F(4, 10)=9.42, p<0.01) of the control values, respectively. However, 10 μM 7,8,4′-THIF recovered the increases in phospho GSK-3β caused by 6-OHDA to 174.6% (Fig. 6F, p<0.05) of the control value. In addition, 25 μM 7,8,4′-THIF significantly reversed the increased expression of phosphorylated p38, ERK 1/2, Akt, and GSK-3β to 94.7% (Fig. 6C, p<0.05), 194.1% (Fig. 6D, p<0.05), 145.0% (Fig. 6E, p<0.05), and 161.3% (Fig. 6F, p<0.05), respectively. Pretreatment with 50 μM 7,8,4′-THIF also significantly reduced the elevated expression of phosphorylated JNK, p38, ERK 1/2, Akt, and GSK-3β to 145.1% (Fig. 6B, p<0.01), 92.2% (Fig. 6C, p<0.05), 199.7% (Fig. 6D, p<0.05), 126.5% (Fig. 6E, p<0.01), and 124.7% (Fig. 6F, p<0.01), respectively, in SH-SY5Y cells. Taken together, these data show that 7,8,4′-THIF effectively attenuates 6-OHDA-induced activation of the MAPK and PI3K/Akt/GSK-3β cascades.
Fig. 6.
Effects of 7,8,4′-THIF on 6-OHDA-induced expression of phosphorylated JNK, p38, ERK 1/2, Akt, and GSK-3β in SH-SY5Y cells. The cells were pretreated with 7,8,4′-THIF (10, 25, or 50 μM) for 30 min followed by exposure to 200 μM 6-OHDA for 1 h (A). The expression levels of phospho JNK (B), phospho p38 (C), phospho ERK 1/2 (D), phospho Akt (E), and phospho GSK-3β (F) were evaluated using Western blot analysis. Densitometric data are expressed as mean ± SEM (n=3). *p<0.05, **p<0.01, and ***p<0.001 compared with the control group. #p<0.05 and ##p<0.01 compared with the 6-OHDA-treated group.
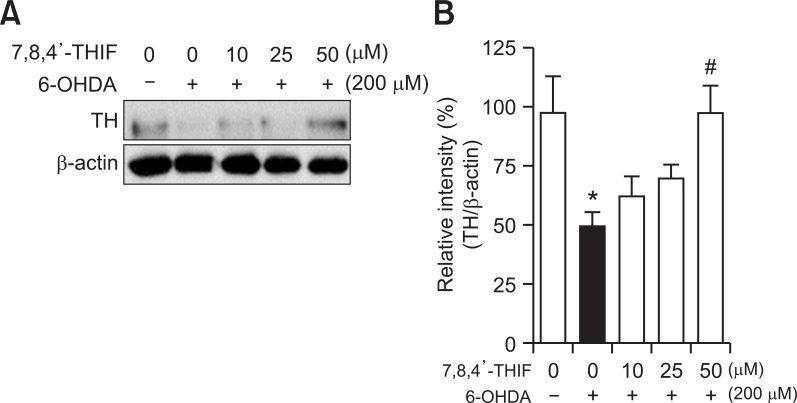
Effects of 7,8,4′-THIF on 6-OHDA-induced TH expression level in SH-SY5Y cells
TH is a rate-limiting enzyme in dopamine metabolism and has been found to be downregulated in many studies using in vitro and in vivo PD models (Jing et al., 2015). Therefore, we further evaluated the effects of 7,8,4′-THIF on TH expression level in SH-SY5Y cells (Fig. 7A). In 6-OHDA-induced cells, the expression level of TH was significantly downregulated to 49.7% of the control values (Fig. 7B, F(4, 10)=4.51, p<0.05). However, 50 μM 7,8,4′-THIF significantly increased the TH level to 97.6% (Fig. 7B, p<0.05), suggesting a positive effect of 7,8,4′-THIF against 6-OHDA-induced dopaminergic cell damage.
Fig. 7.
Effects of 7,8,4′-THIF on 6-OHDA-induced TH expression level in SH-SY5Y cells. The cells were pretreated with 7,8,4′-THIF (10, 25, or 50 μM) for 30 min followed by exposure to 200 μM 6-OHDA for 6 h (A). The expression level of TH (B) was evaluated using Western blot analysis. Densitometric data are expressed as mean ± SEM (n=3). *p<0.05 compared with the control group. #p<0.05 compared with the 6-OHDA-treated group.
DISCUSSION
In the current study, we evaluated the effects of 7,8,4′-THIF (8-hydroxydaidzein), one of the metabolites of daidzein isolated from soybean (Glycine max) products, on neurotoxicity in SH-SY5Y cells stimulated by 6-OHDA. It has been previously reported that 7,8,4′-THIF possesses several biological activities associated with the benefits of human health. In particular, the anti-inflammatory effect of 7,8,4′-THIF in LPS-induced models was exerted by inhibiting Akt/nuclear factor (NF)-κB and activator protein 1 (AP-1) signaling, as well as pro-inflammatory cytokines, inducible nitric oxide synthase (iNOS), and cyclooxygenase-2 (COX-2) activity (Kim et al., 2018; Wu et al., 2018). Also, the antioxidant property of 7,8,4′-THIF was proved by investigating its effects on reactive oxygen species (ROS), free radical scavenging, and cellular activity (Rimbach et al., 2003) and may be affected by nuclear factor E2-related factor 2 (Nrf2) (Wu et al., 2018). However, the anti-apoptotic effects of 7,8,4′-THIF on neuronal cell death have not been investigated in 6-OHDA-induced cellular PD models until now. In addition, the possible mechanisms of 7,8,4′-THIF were studied by evaluating the underlying intracellular signaling pathways in human neuronal SH-SY5Y cells.
Many studies have demonstrated that damage from 6-OHDA-induced oxidative stress can cause cell toxicity and impair the antioxidant defense system, which eventually leads to apoptotic processes associated with PD (Chen et al., 2012). Therefore, suppression of oxidative stress, subsequent dopaminergic neuronal loss, and apoptosis are considered possible therapeutic strategies for treating PD. As provided above, 6-OHDA, a selective neurotoxin, could induce dopaminergic neuronal cell death through the several molecular mechanisms. For example, this neurotoxin inhibits antioxidant system, including the decreases in SOD and GSH contents and increases ROS levels (Kwon et al., 2012). Moreover, 6-OHDA-induced lesion could change the ratio of Bax/Bcl-2 proteins associated with mitochondrial function and activate MAPK and PI3K/Akt/NF-κB molecular pathways related to the processes of cell survival or apoptosis caused by oxidative stress (Zhang et al., 2012; Kim et al., 2017). These changes in mechanisms induced by 6-OHDA may cause neurodegenerative lesion such as PD and Alzheimer’s disease (AD). In this study, we found that cells treated with 200 μM 6-OHDA showed a significant decrease in cell viability and elevated LDH release as determined using MTT and LDH assays, respectively. LDH is another marker for cell toxicity and is released into the extracellular membrane due to damage to neuronal cells caused by neurotoxin such as 6-OHDA or H2O2 (Tan and Kim, 2016). Our results showed that various concentrations of 7,8,4′-THIF significantly inhibited the decreased cell viability and increased LDH release due to 6-OHDA. In addition, in another group of experiments avoiding the direct reaction of 7,8,4′-THIF with 6-OHDA, the MTT and LDH as-says indicated that 7,8,4′-THIF also has a protective effect on 6-OHDA-induced neurotoxicity like the results above (data not shown). Thus, the protective activity of 7,8,4′-THIF may be not related to the direct interaction with 6-OHDA or the quenching effect on the toxicity of 6-OHDA. Moreover, we examined the levels of antioxidant enzymes (SOD, CAT, and GSH) and MDA content after 6-OHDA treatment, and the results indicate that the neurotoxin changed the activities of these products. In cells, these antioxidant enzymes prevent the production of free radicals from peroxides or superoxides (Jin et al., 2015). In addition, 6-OHDA increases the level of MDA, an end-product of lipid peroxidation, in neuronal cells under conditions of oxidative stress (Porres-Martínez et al., 2015). Thus, the increased MDA content is closely associated with oxidative damage to the cell membrane, which can result in cellular damage (Xiao et al., 2008). In our results, pretreatment with 7,8,4′-THIF normalized these changes, demonstrated by elevation of the SOD, CAT, and GSH contents the reduction of MDA activity. Thus, our data indicate that 7,8,4′-THIF is effective in preventing neuronal cell death, which may be partly mediated by recovery of the antioxidant defense system and inhibition of MDA level involved in oxidative stress in neuronal cells.
The main members of the Bcl-2 mitochondrial protein family, including Bcl-2 and Bax, are associated with apoptosis regulation during mitochondrial membrane dysfunction (Kwon et al., 2011). Translocation of the pro-apoptotic protein Bax to the mitochondrial membrane enhances the progression of apoptosis by changing membrane permeability (Vander Heiden and Thompson, 1999). In contrast, Bcl-2, an integral membrane protein located in the outer membrane, has anti-apoptotic activity and protects neuronal cells from oxidative injury and early apoptosis caused by various factors such as 6-OHDA (Tortosa et al., 1997). Thus, the balance of Bcl-2 family proteins (i.e., pro- and anti-apoptotic molecules) likely plays an important role in apoptosis and neuronal cell survival. In addition, 6-OHDA activates caspase-9 and caspase-3, which are primarily associated with neuronal apoptosis (Lee et al., 2005). These activated caspase proteins are also mediated by upregulation of cleavage of the DNA repair enzyme PARP (Grütter, 2000). Thus, inhibition of caspase-3 and caspase-9 may contribute to protection against neuronal cell loss. Our present results reveal that 6-OHDA induced increased Bax and decreased Bcl-2 expression levels, which were ameliorated by pretreatment with 7,8,4′-THIF in SH-SY5Y cells. Moreover, 6-OHDA-mediated increases in the caspase cascade, including increased levels of cleaved caspase-9, cleaved caspase-3, and cleaved PARP, were inhibited by 7,8,4′-THIF. These findings suggest that 7,8,4′-THIF can inhibit 6-OHDA-stimulated apoptotic cell death processes by regulating the expression of Bax and Bcl-2, as well as caspase proteins.
To evaluate the effects of 7,8,4′-THIF on the 6-OHDA-stimulated MAPK cascade, we next performed Western blot analysis on SH-SY5Y cells. The MAPK cascade is activated by major stimuli, such as oxidative stress, and is mainly involved in cell survival and death (Xia et al., 1995). The MAPK pathway, including JNK, p38, and ERK 1/2, regulates various cellular events such as differentiation, proliferation, and apoptosis (Lewis et al., 1998). In addition, PI3K/Akt and its downstream molecule GSK-3β are necessary for diverse cellular processes such as proliferation, growth, survival, and apoptosis (Chen et al., 2004). Thus, the MAPK and PI3K/Akt/GSK-3β signaling pathways are closely associated with pathological aspects of PD. Specifically, increased the expression levels of phosphorylated MAPKs, PI3K/Akt, and GSK-3β were found in the postmortem brain of patients with PD (Dzamko et al., 2014). In addition, 6-OHDA-induced PD exhibits increased levels of phospho MAPKs and PI3K/Akt/GSK-3β in both in vitro and in vivo models (Xie et al., 2016). These inhibitions of the MAPK and PI3K/Akt molecular cascades may be targets for treatment of neurodegenerative diseases such as PD. Previous studies have reported that several therapeutic natural sources and their major compounds were able to inhibit neurotoxin-induced cell death by blocking the abovementioned apoptotic signaling in cellular PD models (Kwon et al., 2012; Kim et al., 2017). Consistent with previous studies using other therapeutic candidate compounds, we found that pretreatment with 7,8,4′-THIF significantly suppressed the 6-OHDA-induced increases in the expression of phosphorylated JNK, p38, and ERK 1/2, as well as PI3K/Akt. Thus, these results obtained from Western blot analyses demonstrate that 7,8,4′-THIF may prevent 6-OHDA-induced neuronal cell death by blocking apoptotic signaling pathways in SH-SY5Y cells. In addition, there is a possibility that 7,8,4′-THIF probably affects Nrf2 involved in the protection of cells from oxidative stress. Many previous studies have indicated that Nrf2, a redox-sensitive transcription factor, is stimulated by the neurotoxin and ROS, which lead to the translocation of Nrf2 into the nucleus where it binds to promoter sequence known as antioxidant response elements (AREs) and could increase a series of antioxidant genes, including heme oxygenase-1 (HO-1) (Keum, 2012; Kwon et al., 2015). Nrf2-dependent pathway has also been reported to be associated with MAPKs and PI3K/Akt signaling. Thus, 7,8,4′-THIF may increase antioxidant genes, such as HO-1, and show cytoprotective effects on 6-OHDA-induced neurotoxicity through, at least in part, the activation of the PI3K/Akt/Nrf2 signaling cascade. Although we did not evaluate the remaining markers such as Nrf2 or HO-1, it is indirectly predicted that 7,8,4′-THIF could increase the anti-oxidant genes through the evaluation of MAPKs and PI3K/Akt pathways as well as the assessment of antioxidant enzymes associated with ROS.
Finally, to explore whether TH expression level was changed following treatment with 7,8,4′-THIF, we conducted Western blotting on SH-SY5Y cells exposed to 6-OHDA. TH is a key enzyme for dopamine metabolism and converts tyrosine to the dopamine precursor dihydroxyphenylalanine in dopaminergic neurons (Pišlar et al., 2014). The decreased TH level leads to dopamine deficits and eventually to the neuropathological features of PD (Simola et al., 2007). Thus, treatment with 6-OHDA markedly reduces the level of TH in neuronal cell models (Shukla et al., 2014). Previous studies have indicated that α-synuclein, a protein marker for the pathogenesis of PD, is the major component of Lewy bodies and could decrease the expression of TH in dopaminergic cells (Kirik et al., 2002). This overexpression of α-synuclein could be up-regulated by some Parkinsonism-inducing neurotoxins such as 6-OHDA and 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) (Yu et al., 2004). Furthermore, there is a possibility that the reduction of TH level may be associated with the transcriptional inhibition of the TH gene (Yu et al., 2004). However, the detailed molecular mechanisms for the suppression of the TH gene expression in dopaminergic cells are not clear. Similarly, our study showed that exposure of SH-SY5Y cells to 6-OHDA significantly reduced the expression of TH. However, this reduction was normalized by pretreatment with 7,8,4′-THIF. As described above, 6-OHDA could destroy dopaminergic neurons normally expressing TH and could induce cell death. 7,8,4′-THIF may increase the survivability of dopaminergic cells against 6-OHDA-induced injury, and thus could also reverse the levels of TH expression. Also, another possibility is that the strong antioxidant effect of 7,8,4′-THIF may protect the reduction of TH expression in SH-SY5Y cells. A previous study has been reported that SH-SY5Y cells with increased TH level have the resistance on oxidative stress induced by 6-OHDA or H2O2 (Franco et al., 2010). Therefore, there may be a correlation between the antioxidant activity of 7,8,4′-THIF and TH expression level. Taken together, these results demonstrate the possible neuroprotective profile of 7,8,4′-THIF in cellular PD models.
In conclusion, we found that 7,8,4′-THIF, a metabolite of daidzein, protects against 6-OHDA-induced neurotoxicity in SH-SY5Y cells. Its mechanism of action is likely associated with its antioxidant activities, as demonstrated by its ability to inhibit LDH and MDA activities as well as increase the levels of antioxidant enzymes such as SOD, CAT, and GSH. In addition to the antioxidant activities of 7,8,4′-THIF, its protective effects against apoptosis caused by 6-OHDA are likely related to it decreasing the activation of the MAPK and PI3K/Akt/GSK-3β pathways, as well as reducing the expression of cleaved caspase-3, cleaved caspase-9, and cleaved PARP, upregulating Bax, and downregulating Bcl-2. These effects may be a direct activity on the processes of apoptosis in SH-SY5Y cells. 7,8,4′-THIF could modulate the apoptotic modulator (Bax and Bcl-2) and apoptotic proteins (caspase-9, caspase-3, and PARP) as well as inhibit the MAPK signaling molecules deeply involved in the process of apoptosis at the molecular levels. However, there is also a possibility that the potential anti-apoptotic activity of 7,8,4′-THIF is mediated partly by changing SOD or GSH directly related to the antioxidant function. Therefore, these results indicate that 7,8,4′-THIF may provide protection by both direct and indirect anti-apoptotic activities against 6-OHDA-induced neurotoxicity. Finally, pretreatment with 7,8,4′-THIF restores the decreased expression of TH, an enzyme responsible for dopamine synthesis, in 6-OHDA-stimulated SH-SY5Y cells. As mentioned above, our previous studies and other studies have indicated that the metabolites of daidzein, including 7,8,4′-THIF and 6,7,4′-THIF, have positive effects on brain-related disorders such as cognitive impairment and neuroinflammation (Ko et al., 2018a; Wu et al., 2018). Although the exact mechanisms involved in the effects of 7,8,4′-THIF remain unclear, this molecule has potential therapeutic value in the treatment of neurodegenerative diseases such as PD. Furthermore, 7,8,4′-THIF is a metabolite of daidzein and is found only in fermented soybean-based foods (Wu et al., 2018). Therefore, it is produced by the fermentation process and may have positive effects on human health. In addition, in our results, 50 μM of 7,8,4′-THIF showed a sufficient effect to block the toxicity of 6-OHDA. Recent published pharmaco-kinetics (PK) results showed the changes in the amounts of 7,8,4′-THIF and its maximum value in soybean extract-fed rat plasma within a specific time range (Lee et al., 2018). Thus, the possibility of achieving 50 μM of 7,8,4′-THIF concentration in vivo may be predicted with reference to this result. Collectively, these data indicate that 7,8,4′-THIF is a potentially therapeutic compound for treating PD and developing functional food or medicine. However, the improving effect of 7,8,4′-THIF in PD is required to be further investigated in vivo.
Acknowledgments
This research was supported by a grant (NRF-2012R1A 5A2A28671860) from the Basic Science Research Program through the National Research Foundation of Korea.
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
REFERENCES
- Blum D, Torch S, Lambeng N, Nissou M, Benabid AL, Sadoul R, Verna JM. Molecular pathways involved in the neurotoxicity of 6-OHDA, dopamine and MPTP: contribution to the apoptotic theory in Parkinson’s disease. Prog Neurobiol. 2001;65:135–172. doi: 10.1016/S0301-0082(01)00003-X. [DOI] [PubMed] [Google Scholar]
- Chen G, Bower KA, Ma C, Fang S, Thiele CJ, Luo J. Glycogen synthase kinase 3beta (GSK3beta) mediates 6-hydroxydopamine-induced neuronal death. FASEB J. 2004;18:1162–1164. doi: 10.1096/fj.04-1551fje. [DOI] [PubMed] [Google Scholar]
- Chen JH, Ou HP, Lin CY, Lin FJ, Wu CR, Chang SW, Tsai CW. Carnosic acid prevents 6-hydroxydopamine-induced cell death in SH-SY5Y cells via mediation of glutathione synthesis. Chem Res Toxicol. 2012;25:1893–1901. doi: 10.1021/tx300171u. [DOI] [PubMed] [Google Scholar]
- Dzamko N, Zhou J, Huang Y, Halliday GM. Parkinson’s disease-implicated kinases in the brain; insights into disease pathogenesis. Front Mol Neurosci. 2014;7:57. doi: 10.3389/fnmol.2014.00057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eren-Guzelgun B, Ince E, Gurer-Orhan H. In vitro antioxidant/prooxidant effects of combined use of flavonoids. Nat Prod Res. 2018;32:1446–1450. doi: 10.1080/14786419.2017.1346637. [DOI] [PubMed] [Google Scholar]
- Eriksen JL, Dawson TM, Dickson DW, Petrucelli L. Caught in the act: alpha-synuclein is the culprit in Parkinson’s disease. Neuron. 2003;40:453–456. doi: 10.1016/S0896-6273(03)00684-6. [DOI] [PubMed] [Google Scholar]
- Franco JL, Posser T, Gordon SL, Bobrovskaya L, Schneider JJ, Farina M, Dafre AL, Dickson PW, Dunkley PR. Expression of tyrosine hydroxylase increases the resistance of human neuroblastoma cells to oxidative insults. Toxicol Sci. 2010;113:150–157. doi: 10.1093/toxsci/kfp245. [DOI] [PubMed] [Google Scholar]
- Grütter MG. Caspases: key players in programmed cell death. Curr Opin Struct Biol. 2000;10:649–655. doi: 10.1016/S0959-440X(00)00146-9. [DOI] [PubMed] [Google Scholar]
- Guo S, Bezard E, Zhao B. Protective effect of green tea polyphenols on the SH-SY5Y cells against 6-OHDA induced apoptosis through ROS-NO pathway. Free Radic Biol Med. 2005;39:682–695. doi: 10.1016/j.freeradbiomed.2005.04.022. [DOI] [PubMed] [Google Scholar]
- Heinonen SM, Hoikkala A, Wähälä K, Adlercreutz H. Metabolism of the soy isoflavones daidzein, genistein and glycitein in human subjects. Identification of new metabolites having an intact isoflavonoid skeleton. J Steroid Biochem Mol Biol. 2003;87:285–299. doi: 10.1016/j.jsbmb.2003.09.003. [DOI] [PubMed] [Google Scholar]
- Jin X, Liu Q, Jia L, Li M, Wang X. Pinocembrin attenuates 6-OHDA-induced neuronal cell death through Nrf2/ARE pathway in SH-SY5Y cells. Cell Mol Neurobiol. 2015;35:323–333. doi: 10.1007/s10571-014-0128-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jing X, Shi H, Zhang C, Ren M, Han M, Wei X, Zhang X, Lou H. Dimethyl fumarate attenuates 6-OHDA-induced neurotoxicity in SH-SY5Y cells and in animal model of Parkinson’s disease by enhancing Nrf2 activity. Neuroscience. 2015;286:131–140. doi: 10.1016/j.neuroscience.2014.11.047. [DOI] [PubMed] [Google Scholar]
- Keum YS. Regulation of Nrf2-mediated phase II detoxification and anti-oxidant genes. Biomol. Ther (Seoul) 2012;20:144–151. doi: 10.4062/biomolther.2012.20.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E, Kang YG, Kim JH, Kim YJ, Lee TR, Lee J, Kim D, Cho JY. The antioxidant and anti-inflammatory activities of 8-hydroxydaidzein (8-HD) in activated macrophage-like RAW264.7 cells. Int. J. Mol. Sci. 2018;19:E1828. doi: 10.3390/ijms19071828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim EK, Choi EJ. Pathological roles of MAPK signaling pathways in human diseases. Biochim. Biophys. Acta. 2010;1802:396–405. doi: 10.1016/j.bbadis.2009.12.009. [DOI] [PubMed] [Google Scholar]
- Kim H, Kim JR, Kang H, Choi J, Yang H, Lee P, Kim J, Lee KW. 7,8,4′-Trihydroxyisoflavone attenuates DNCB-induced atopic dermatitis-like symptoms in NC/Nga mice. PLoS ONE. 2014;9:e104938. doi: 10.1371/journal.pone.0104938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SM, Park YJ, Shin MS, Kim HR, Kim MJ, Lee SH, Yun SP, Kwon SH. Acacetin inhibits neuronal cell death induced by 6-hydroxydopamine in cellular Parkinson’s disease model. Bioorg Med Chem Lett. 2017;27:5207–5212. doi: 10.1016/j.bmcl.2017.10.048. [DOI] [PubMed] [Google Scholar]
- Kirik D, Rosenblad C, Burger C, Lundberg C, Johansen TE, Muzyczka N, Mandel RJ, Björklund A. Parkinson-like neurodegeneration induced by targeted overexpression of alpha-synuclein in the nigrostriatal system. J Neurosci. 2002;22:2780–2791. doi: 10.1523/JNEUROSCI.22-07-02780.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko YH, Kim SY, Lee SY, Jang CG. 6,7,4′-Trihydroxyisoflavone, a major metabolite of daidzein, improves learning and memory via the cholinergic system and the p-CREB/BDNF signaling pathway in mice. Eur J Pharmacol. 2018a;826:140–147. doi: 10.1016/j.ejphar.2018.02.048. [DOI] [PubMed] [Google Scholar]
- Ko YH, Kwon SH, Hwang JY, Kim KI, Seo JY, Nguyen TL, Lee SY, Kim HC, Jang CG. The memory-enhancing effects of liquiritigenin by activation of NMDA receptors and the CREB signaling pathway in mice. Biomol. Ther. (Seoul) 2018b;26:109–114. doi: 10.4062/biomolther.2016.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopalli SR, Noh SJ, Koppula S, Suh YH. Methylparaben protects 6-hydroxydopamine-induced neurotoxicity in SH-SY5Y cells and improved behavioral impairments in mouse model of Parkinson’s disease. Neurotoxicology. 2013;34:25–32. doi: 10.1016/j.neuro.2012.10.003. [DOI] [PubMed] [Google Scholar]
- Kwon SH, Hong SI, Jung YH, Kim MJ, Kim SY, Kim HC, Lee SY, Jang CG. Lonicera japonica THUNB. protects 6-hydroxydopamine-induced neurotoxicity by inhibiting activation of MAPKs, PI3K/Akt, and NF-κB in SH-SY5Y cells. Food Chem Toxicol. 2012;50:797–807. doi: 10.1016/j.fct.2011.12.026. [DOI] [PubMed] [Google Scholar]
- Kwon SH, Kim JA, Hong SI, Jung YH, Kim HC, Lee SY, Jang CG. Loganin protects against hydrogen peroxide-induced apoptosis by inhibiting phosphorylation of JNK, p38, and ERK 1/2 MAPKs in SH-SY5Y cells. Neurochem Int. 2011;58:533–541. doi: 10.1016/j.neuint.2011.01.012. [DOI] [PubMed] [Google Scholar]
- Kwon SH, Ma SX, Hong SI, Kim SY, Lee SY, Jang CG. Eucommia ulmoides Oliv. bark. attenuates 6-hydroxydopamine-induced neuronal cell death through inhibition of oxidative stress in SH-SY5Y cells. J Ethnopharmacol. 2014;152:173–182. doi: 10.1016/j.jep.2013.12.048. [DOI] [PubMed] [Google Scholar]
- Kwon SH, Ma SH, Hwang JY, Lee SY, Jang CG. Involvement of the Nrf2/HO-1 signaling pathway in sulfuretin-induced protection against amyloid beta25-35 neurotoxicity. Neuro-science. 2015;304:14–28. doi: 10.1016/j.neuroscience.2015.07.030. [DOI] [PubMed] [Google Scholar]
- Lee CC, Dudonné S, Kim JH, Kim JS, Dubé P, Kim JE, Desjardins Y, Park JHY, Lee KW, Lee CY. A major daidzin metabolite 7,8,4′-trihydroxyisoflavone found in the plasma of soybean extract-fed rats attenuates monocyte-endothelial cell adhesion. Food Chem. 2018;240:607–614. doi: 10.1016/j.foodchem.2017.08.002. [DOI] [PubMed] [Google Scholar]
- Lee HJ, Noh YH, Lee DY, Kim YS, Kim KY, Chung YH, Lee WB, Kim SS. Baicalein attenuates 6-hydroxydopamine-induced neurotoxicity in SH-SY5Y cells. Eur J Cell Biol. 2005;84:897–905. doi: 10.1016/j.ejcb.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Lee IH, Chou CC. Distribution profiles of isoflavone isomers in black bean kojis prepared with various filamentous fungi. J Agric Food Chem. 2006;54:1309–1314. doi: 10.1021/jf058139m. [DOI] [PubMed] [Google Scholar]
- Lewis TS, Shapiro PS, Ahn NG. Signal transduction through MAP kinase cascades. Adv Cancer Res. 1998;74:49–139. doi: 10.1016/S0065-230X(08)60765-4. [DOI] [PubMed] [Google Scholar]
- Li HY, Pan L, Ke YS, Batnasan E, Jin XQ, Liu ZY, Ba XQ. Daidzein suppresses pro-inflammatory chemokine Cxcl2 transcription in TNF-α-stimulated murine lung epithelial cells via depressing PARP-1 activity. Acta Pharmacol Sin. 2014;35:496–503. doi: 10.1038/aps.2013.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park HJ, Lee KS, Zhao TT, Lee KE, Lee MK. Effects of asarinin on dopamine biosynthesis and 6-hydroxydopamine-induced cytotoxicity in PC12 cells. Arch Pharm Res. 2017;40:631–639. doi: 10.1007/s12272-017-0908-z. [DOI] [PubMed] [Google Scholar]
- Pišlar AH, Zidar N, Kikelj D, Kos J. Cathepsin X promotes 6-hydroxydopamine-induced apoptosis of PC12 and SH-SY5Y cells. Neuropharmacology. 2014;82:121–131. doi: 10.1016/j.neuropharm.2013.07.040. [DOI] [PubMed] [Google Scholar]
- Porres-Martínez M, González-Burgos E, Carretero ME, Gómez-Serranillos MP. Protective properties of Salvia lavandulifolia Vahl. essential oil against oxidative stress-induced neuronal injury. Food Chem Toxicol. 2015;80:154–162. doi: 10.1016/j.fct.2015.03.002. [DOI] [PubMed] [Google Scholar]
- Rimbach G, De Pascual-Teresa S, Ewins BA, Matsugo S, Uchida Y, Minihane AM, Turner R, VafeiAdou K, Weinberg PD. Antioxidant and free radical scavenging activity of isoflavone metabolites. Xenobiotica. 2003;33:913–925. doi: 10.1080/0049825031000150444. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Oroz MC, Jahanshahi M, Krack P, Litvan I, Macias R, Bezard E, Obeso JA. Initial clinical manifestations of Parkinson’s disease: features and pathophysiological mechanisms. Lancet Neurol. 2009;8:1128–1139. doi: 10.1016/S1474-4422(09)70293-5. [DOI] [PubMed] [Google Scholar]
- Shukla A, Mohapatra TM, Parmar D, Seth K. Neuroprotective potentials of neurotrophin rich olfactory ensheathing cell’s conditioned media against 6OHDA-induced oxidative damage. Free Radic Res. 2014;48:560–571. doi: 10.3109/10715762.2014.894636. [DOI] [PubMed] [Google Scholar]
- Simola N, Morelli M, Carta AR. The 6-hydroxydopamine model of Parkinson’s disease. Neurotox Res. 2007;11:151–167. doi: 10.1007/BF03033565. [DOI] [PubMed] [Google Scholar]
- Tan JW, Kim MK. neuroprotective effects of biochanin A against β-amyloid-induced neurotoxicity in PC12 cells via a mitochondrial-dependent apoptosis pathway. Molecules. 2016;21:548. doi: 10.3390/molecules21050548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian LL, Zhou Z, Zhang Q, Sun YN, Li CR, Cheng CH, Zhong ZY, Wang SQ. Protective effect of (+/−) isoborneol against 6-OHDA-induced apoptosis in SH-SY5Y cells. Cell Physiol Biochem. 2007;20:1019–1032. doi: 10.1159/000110682. [DOI] [PubMed] [Google Scholar]
- Tortosa A, López E, Ferrer I. Bcl-2 and Bax proteins in Lewy bodies from patients with Parkinson’s disease and Diffuse Lewy body disease. Neurosci Lett. 1997;238:78–80. doi: 10.1016/S0304-3940(97)00837-9. [DOI] [PubMed] [Google Scholar]
- Vander Heiden MG, Thompson CB. Bcl-2 proteins: regulators of apoptosis or of mitochondrial homeostasis? Nat Cell Biol. 1999;1:E209–E216. doi: 10.1038/70237. [DOI] [PubMed] [Google Scholar]
- Wu PS, Ding HY, Yen JH, Chen SF, Lee KH, Wu MJ. Anti-inflammatory activity of 8-hydroxydaidzein in LPS-stimulated BV2 microglial cells via activation of Nrf2-antioxidant and attenuation of Akt/NF-κB-inflammatory signaling pathways, as well as inhibition of COX-2 activity. J Agric Food Chem. 2018;66:5790–5801. doi: 10.1021/acs.jafc.8b00437. [DOI] [PubMed] [Google Scholar]
- Xia Z, Dickens M, Raingeaud J, Davis RJ, Greenberg ME. Opposing effects of ERK and JNK-p38 MAP kinases on apoptosis. Science. 1995;270:1326–1331. doi: 10.1126/science.270.5240.1326. [DOI] [PubMed] [Google Scholar]
- Xiao X, Liu J, Hu J, Zhu X, Yang H, Wang C, Zhang Y. Protective effects of protopine on hydrogen peroxide-induced oxidative injury of PC12 cells via Ca(2+) antagonism and antioxidant mechanisms. Eur J Pharmacol. 2008;591:21–27. doi: 10.1016/j.ejphar.2008.06.045. [DOI] [PubMed] [Google Scholar]
- Xie CL, Lin JY, Wang MH, Zhang Y, Zhang SF, Wang XJ, Liu ZG. Inhibition of glycogen synthase kinase-3β (GSK-3β) as potent therapeutic strategy to ameliorates L-dopa-induced dyskinesia in 6-OHDA parkinsonian rats. Sci Rep. 2016;6:23527. doi: 10.1038/srep23527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu B, Chang SK. Antioxidant capacity of seed coat, dehulled bean, and whole black soybeans in relation to their distributions of total phenolics, phenolic acids, anthocyanins, and isoflavones. J Agric Food Chem. 2008;56:8365–8373. doi: 10.1021/jf801196d. [DOI] [PubMed] [Google Scholar]
- Yu G, Deng A, Tang W, Ma J, Yuan C, Ma J. Hydroxytyrosol induces phase II detoxifying enzyme expression and effectively protects dopaminergic cells against dopamine- and 6-hydroxydopamine induced cytotoxicity. Neurochem Int. 2016;96:113–120. doi: 10.1016/j.neuint.2016.03.005. [DOI] [PubMed] [Google Scholar]
- Yu S, Zuo X, Li Y, Zhang C, Zhou M, Zhang YA, Uéda K, Chan P. Inhibition of tyrosine hydroxylase expression in alpha-synuclein-transfected dopaminergic neuronal cells. Neurosci Lett. 2004;367:34–39. doi: 10.1016/j.neulet.2004.05.118. [DOI] [PubMed] [Google Scholar]
- Yuan H, Zheng JC, Liu P, Zhang SF, Xu JY, Bai LM. Pathogenesis of Parkinson’s disease: oxidative stress, environmental impact factors and inflammatory processes. Neurosci Bull. 2007;23:125–130. doi: 10.1007/s12264-007-0018-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang LJ, Xue YQ, Yang C, Yang WH, Chen L, Zhang QJ, Qu TY, Huang S, Zhao LR, Wang XM, Duan WM. Human albumin prevents 6-hydroxydopamine-induced loss of tyrosine hydroxylase in in vitro and in vivo. PLoS ONE. 2012;7:e41226. doi: 10.1371/journal.pone.0041226. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.