Abstract
Context
Dietary intake research has increasingly focused on improving diet quality in low- and middle-income countries (LMICs). Accompanying this is the need for sound metrics to assess diet quality.
Objective
This systematic literature review aims to describe existing diet quality indices for general populations and highlights recommendations for developing such indices for food system research in LMICs.
Data sources
Three electronic databases were searched for papers published between January 2008 and December 2017.
Data extraction
Articles published in English and describing the development of an index to measure overall diet quality, irrespective of whether they were for high-income countries or LMICs, were included.
Data analysis
Eighty-one indices were identified, over two thirds were based on national dietary guidelines from high-income countries. Of the 3 key diet quality dimensions, “diversity” was included in all 18 indices developed for LMICs, “moderation” was captured by most, and “nutrient adequacy” was included 4 times.
Conclusions
Indices need to be developed that include all dimensions, include foods and/or food groups rather than nutrients, use an optimal range for individual components in the score, and express the intake of healthy and unhealthy components separately. Importantly, validation of the index should be part of its development.
Keywords: diet index, diet quality, dietary assessment, food systems research, low- and middle-income countries
INTRODUCTION
Food systems should provide year-round access to foods that cover people’s nutrient needs and promote healthy dietary practices.1 However, they are increasingly under pressure to improve and accelerate impacts on nutritional outcomes,2 especially in low- and middle-income countries (LMICs). Diets of poor quality are the main contributors to the multiple burdens of malnutrition (stunting, wasting, micronutrient deficiencies, overweight, obesity, and nutrition-related noncommunicable diseases [NCDs]),3,4 and promoting healthy diets can help prevent undernutrition and micronutrient deficiencies and mitigate the rise of overnutrition and diet-related noncommunicable diseases among poor and vulnerable populations.3,5 Food systems, including all components and activities related to production, processing, distribution, preparation, and consumption, and the outputs of these activities,1,6 have a key role in delivering high-quality diets but are presently failing to deliver healthy diets to people in LMICs. It is generally recognized that food systems need to be repositioned away from a strong focus on increasing food quantity toward more diversified systems capable of supplying the essential dietary components that can reduce the high prevalence of micronutrient deficiencies among women and children and high stunting rates (growth retardation) of children.7 At the same time, food systems should provide dietary options that can diminish the growing burden of overweight, obesity, and diet-related NCDs, such as diabetes, cancer, and cardiovascular diseases (CVD).4
Although a universal definition of the concept of diet quality is lacking, there is general agreement that it comprises 3 main dimensions: 1) nutrient adequacy, 2) food variety or food diversity, and 3) moderation of foods, food groups, or energy and nutrients.8,9 Adequacy refers to the provision of levels of dietary energy and macro- and micronutrients appropriate to age, sex, disease status, and physical activity for a healthy life. Diversity refers to the consumption of a variety of desirable foods or food groups (eg, whole grains, fruits, vegetables, fish, meat, nuts and seeds, beans and legumes, milk and eggs).9 Moderation refers to the avoidance or limited consumption of foods, food groups, and nutrients that can be unhealthy if consumed in excess, such as food high in fats (especially saturated and trans fat), sugar, (including sugar-sweetened beverages [SSBs]), and sodium.8,10 Food safety is another important dimension of high-quality diets but will not be addressed in this paper. Monotonous staple-based diets and lack of dietary diversity, both often observed in dietary surveys in LMICs, are strongly associated with inadequate intake and risks of deficiencies of essential micronutrients.11 In addition, many LMICs are currently undergoing a nutrition transition, which is marked by an increased intake of unhealthy fats, refined carbohydrates, added sugar, animal source foods, and low consumption of legumes, fruits, and vegetables.12–14
With this transformation of food systems to a focus on healthy diets comes the need for sound metrics to measure the quality of such diets in LMICs. The quality of a diet depends on the existing dietary patterns, and in general, 2 approaches to assessing dietary patterns are used: a priori, based on prior nutrition knowledge translated into dietary guidelines; and a posteriori, where patterns are defined once the dietary intake data are collected.15 A priori assessed dietary patterns are used to construct diet quality indices that quantify the healthiness of the dietary pattern based on existing scientific knowledge and, when international dietary guidelines are used, allow for cross-country comparisons. In LMIC settings the use of dietary diversity scores is common because they are relatively easy to administer with limited resources,16 but the scores presently used do not capture the 3 important dimensions of diet quality (see above); in particular, the moderation dimension is often missing. Therefore, additional diet quality indices need to be identified for use in LMICs to complement dietary diversity scores. This systematic review aims to present a state-of-the-art inventory of diet quality indices developed for both LMICs and high-income countries by systematically searching the literature for articles listing the diet quality indices published since a previous review was published in 2009 by Wirt and Collins.17 Furthermore, the authors highlight priorities and recommendations on the applicability and further development of such indices for food system research in LMICs.
METHODS
Literature search strategy
A systematic search of English-language articles published in peer-reviewed journals between January 2008 and December 2017 and review articles from before 2008 was performed using the electronic databases Scopus, CAB abstracts, and MEDLINE. These 3 databases are the most relevant in nutrition research, and therefore the authors feel confident that this search provided comprehensive coverage of the published literature. The starting date of this systematic review was chosen based on the timeframe of the most recent systematic review on diet quality indices in all age groups by Wirt and Collins.17 Title-abstract-keywords were included in three different search strings: 1) (Diet* OR food* OR nutrient* OR meal* OR nutrition*), 2) (index OR determinant* OR indicator* OR score* OR indices OR measure* OR asses* OR approach), and 3) (quality OR adequacy OR variety OR diversity OR health*) using an adjacency operator when combining the 3 searches. Relevant studies might have been missed when the words used in the search were not mentioned in the title, abstract, or keywords. Therefore, the literature list of the included publications was checked, and the gray literature was searched in order to be as comprehensive as possible. Another limitation inherent to systematic literature review is publication bias, which refers to the possibility that newly developed indices have not been published and could therefore not be included in this review.
Some diet quality indices are more extensively evaluated and described in additional publications (eg, the Healthy Eating Index [HEI] 200518,19 and 201020,21 and the World Health Organization’s Infant and Young Children Feeding Indicators [IYCFI]22); however this review focuses on articles that describe the development of indices, thus additional articles that describe the validation of a certain index are not included in this review.
Selection of studies and data synthesis
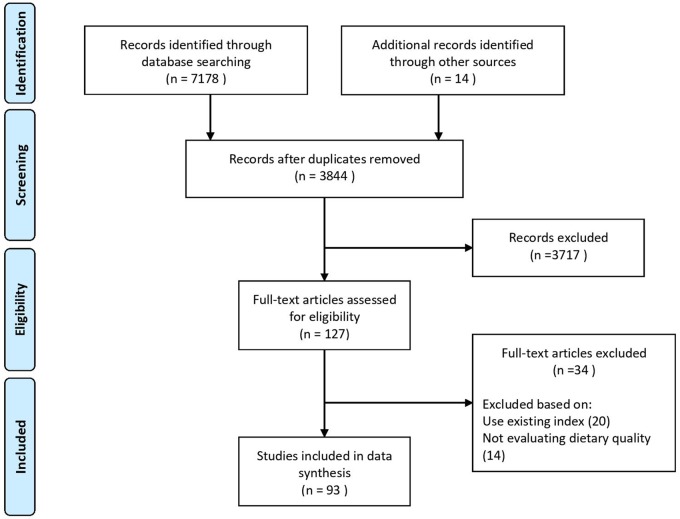
The database search resulted in 7178 articles. An additional 14 publications were included from the gray literature and by screening the references of eligible articles. After removal of the duplicates, 3844 articles were left. The initial title-abstract screening resulted in 127 eligible articles, and after reading the full texts an additional 34 articles were excluded, resulting in 78 original articles and 15 review articles included in this review (see Figure 1 for the flow diagram).
Figure 1.
Flow diagram of the literature search process.
The PICOS criteria for inclusion and exclusion are described in Table 1. Inclusion criteria for title, abstract, and full-text screening were articles describing the development of an index (or a new index that was adapted from a former index) to measure diet quality in all population groups. Exclusion criteria were nonhuman studies or studies using an existing diet quality index or associating such an existing index to a health outcome or biomarker. Also, articles not evaluating dietary quality (eg, indices assessing environmental impacts, food labeling, and advertisement influences or indices dealing with food safety issues) were not included. Indices solely describing the meal intake pattern (eg, number of meals, frequency of eating pattern, or snack intake) or the quality of a single meal, which are extensively described in a review done by Gorgulho et al,23 were not included in this review. Likewise, scores for single nutrient quality (including protein quality and the glycemic load and index)24 or nutrient profiling of single foods (where single foods are profiled according to their nutrient content [eg, the Nutrient Rich Foods {NRF} 9.3])25–28 are beyond the scope of this review.
Table 1.
PICOS criteria for inclusion and exclusion of studies
| PICOS criteria | Inclusion | Exclusion |
|---|---|---|
| Population | All population groups | Nonhuman studies |
| Intervention | Measure of diet quality | Articles not evaluating dietary quality (eg, assessing environmental impacts, food labeling, influence of advertisements, or food safety issues) |
| Comparator | No comparator, descriptive systematic review | |
| Outcome | New or updated diet quality index | Studies using an existing index |
| Setting | All settings |
Title-abstract eligibility assessment of the articles for inclusion in the systematic review was performed by 1 reviewer and afterwards checked, in an unblinded manner, by another reviewer. Disagreements between reviewers were resolved by consensus. Subsequently 1 reviewer extracted the data from the included studies (n = 127 articles) and discussed it with the second reviewer, leading to the exclusion of another 34 articles, resulting in a total of 93 studies (78 original articles and 15 review articles) included in the analysis. Information was extracted from each study on the developed index (age group for whom the index is intended, guideline(s) used to develop the index, components of the index, scoring system), the pilot/evaluation study (country, sample size, study type, objective), dietary assessment method used, and the initial evaluation method used to validate the index.
The authors evaluated the different indices on a qualitative and descriptive basis rather than a quantitative basis because the development, assessment, and evaluation of the listed diet quality indices show a great deal of variety.
RESULTS
Of the 93 included articles, a total of 78 original articles listing 81 different diet quality indices were identified in this systematic literature review. Additionally, 15 reviews of such indices were found.17,24,29–41 These reviews were used as background reading and to check the completeness of the list of diet quality indices but are not discussed in the article. The 81 diet quality indices identified are listed in Table 2 (indices developed for global/multiple region use, n = 5),11,42–46Table 3 (indices developed for LMICs, n = 14),47–58 and Table 4 (indices developed for high-income countries, n = 62).59–119 Sixty-one of the diet quality indices have been developed for countries in Europe (n = 33), Australia and New Zealand (n = 15), and North America (n = 13) (Tables 3 and 4). This review identified 14 indices developed for countries classified as LMICs47–58 (Table 3, based on the World Bank country classification by income). Another 5 indices were developed for cross-regional comparison (Table 2), of which 3 have global applicability,42,43,45 and the other 2 have been applied on 2 different continents, the PANDiet score44 in high income countries and the Food Group Diversity Indicators (FGI)11 in LMICs in Africa and Asia. Research on the development of the FGI was used for the development of the Minimum Dietary Diversity for Women (MDD-W).42 Thus various forms of diet quality indices have been tested for LMICs, although the question remains whether these country-specific and cross-regional indices capture all dimensions of diet quality.
Table 2.
Identified diet quality indices from the literature for global/multiple regions
| Reference | Index | Theoretical basis | Country and target group | Components | Scoring system | Evaluationa |
|---|---|---|---|---|---|---|
| FAO and FHI 360 (2016)42 | Minimum Dietary Diversity for Women (MDD-W) | Scientific literature, expert group | Global; women | Grains, white roots and tubers, plantains, pulses (beans, peas, and lentils), nuts and seeds, dairy, meat/poultry/fish, eggs, dark green leafy vegetables, other vitamin A–rich fruits and vegetables, other vegetables, other fruits | 10 food groups, score based on consumption, range 0–10 | Not described in this publication, but it is based on the findings from the FGI11 research and further elaborated on Martin-Prével et al46 |
| Arimond et al (2010)11 | Food Group Diversity Indicators (FGI) | Scientific literature | Burkina Faso, Mali, Mozambique, Bangladesh, Philippines; women | All starchy staples, all legumes and nuts, all dairy, other animal source foods, vitamin A–rich fruits and vegetables, other fruits and vegetables (or split up in a higher aggregation level) | 8 different FGIs, varying in amount of food groups and minimum quantities consumed | Sociodemographic factors, anthropometrics, mean probability of adequacy, se/sp analysis |
| Imamura et al (2015)43 | 3 scores: healthy items, unhealthy items, combined items | Scientific literature | 187 countries; adults | Healthy: fruits, vegetables, beans/legumes, nuts/seeds, whole grains, milk, PUFA, fish, plant n-3, dietary fiberUnhealthy: unprocessed red meats, processed meats, SSBs, saturated fat, trans fat, cholesterol, sodium | 17 components, score based on quintiles, range 0–100 | Scores are compared among countries, age, and sex |
| Verger et al (2012)44 | Probability of Adequate Nutrient Intake (PANDiet) score | Nutritional recommendations for French and US adults | France and USA; adults | Protein, total carbohydrates, fiber, total fat, SFAs, PUFAs, cholesterol, thiamin, riboflavin, niacin, folate, vitamin A, vitamin B6, vitamin B12, vitamin C, vitamin D, vitamin E, calcium, magnesium, zinc, phosphorus, potassium, iron, sodium | 24 components, scored based on adequacy probability, range 0–100 | Sociodemographic factors, nutrient intakes, food groups, biomarkers of exposure |
| WHO (2008)45 | Indicators for infant and young child feeding | Scientific literature | Global; infants and young child | Summary score: breastfeeding practices, dietary diversity, meal frequency | 3 components, score based on consumption and frequency, range 0–1 | Not described in this publication but for evaluation see, for example, Jones et al22 |
Abbreviations: FGI, food group diversity indicators; PUFA, polyunsaturated fatty acids, se/sp analysis; sensitivity/specificity analysis; SFA, saturated fatty acid; SSB, sugar-sweetened beverages.
Some diet quality indices are more extensively evaluated and described in additional publications; however, our review search was not specifically set up for such validation studies, and thus articles describing such validation studies are not included in our review.
Table 3.
Identified diet quality indices from the literature for low- and middle-income countries, organized by region and country
| Reference | Index | Theoretical basis | Country and target group | Components | Scoring system | Evaluationa |
|---|---|---|---|---|---|---|
| AFRICA | ||||||
| Bork et al (2012)47 | Infant and Young Child Feeding Index (ICFI) | Scientific literature and available data | Senegal; infants and toddlers | Dietary diversity index, food variety index, meal frequency index, breastfeeding | 4 components, score based on tertiles and breastfeeding, range 0–7 | Anthropometrics, reliability |
| ASIA | ||||||
| Yuan et al (2017)48 | Chinese Healthy Eating Index (CHEI) | Chinese Dietary Guidelines 2016 | China; children, adolescents, adults | Adequacy: total grains, whole grains/mixed beans, tubers, total vegetables, dark vegetables, fruits, dairy, soybeans, fish/seafood, poultry, eggs, seeds/nuts Limiting: red meat, cooking oils, sodium, added sugars, alcohol | 17 components including weighing factor, score based on standard portion size per 1000 kcal, range 0–100 | Sociodemographic factors, BMI |
| Cheng et al (2016)49 | Chinese Children Dietary Index (CCDI) | Chinese Dietary Guidelines 2007 and Chinese DRIs 2013 | China; children and adolescents | Grains, vegetables, fruits, dairy/dairy products, soybean and its products, fish/shrimp, meat, eggs, water, SSB, vitamin A, ratio UFA to SFA, fiber, diet variety (5 food groups), eating breakfast/dinner, energy balance metric | 16 components, score based on food densities (g/kcal), meeting recommendations or servings, range 0–160 | Sociodemographic factors, BMI, nutrient adequacy ratios, mean adequacy ratio, foods/food groups |
| Xu et al (2015)50 | Chinese Food Pagoda Score (CFPS) | Chinese Food Pagoda (CFP) | China; adults | Grains/potatoes/beans, vegetables, fruits, meat, eggs, fish/shrimp, dairy, nuts/soybean products, cooking oil, salt | 10 components, gram intake per energy level, range 0–10 | Sociodemographic factors |
| Hardiansyah et al (2015)51 | Balanced Diet Index (BDI) | Not mentioned | Indonesia; children | Adequacy: carbohydrate foods, vegetables, fruits, animal foods, milk, plant protein foods Limiting: fat, salt/sodium, added sugar | 12 BDIs are discussed, based on servings, different ranges for the 12 BDIs | Nutrient adequacy |
| Chiplonkar and Rama (2010)52 | Adolescent Micronutrient Quality Index (AMQI) | Indian and US dietary guidelines | India; adolescents | Cereals and millets, legumes, milk and milk products, vegetables (green leafy, other, roots and tubers), fruits, sugar, fats/oils, at least 50% grains as whole grains, at least 50% legumes being micronutrient dense, food variety, sprouts/fermented foods/salads, tea/coffee with meals, fried foods | 13 components, score based on servings, range 0–100 | Sociodemographic factors, nutrient intake, biomarker of exposure, micronutrient adequacy ratio, physical activity |
| Taechangam et al (2008)53 | Healthy Eating Index for Thais (THEI) | Food Guide Thailand Nutrition Flag | Thailand; adults | Rice/starch, vegetables, fruits, milk/ milk products, meat/poultry/fish/dry beans/eggs/nuts, total fat, saturated fat, added sugar, total cholesterol, Na, variety score | 11 components, score based on amounts consumed, servings and E%, range 0–110 | Anthropometrics, expert panel, nutrient intakes |
| SOUTH AMERICA | ||||||
| Molina et al (2010)54 | Indice de Alimentacao do Escolar (ALES; School Child Diet Index) | Nutritional recommendations for the Brazilian population | Brazil; children | Fruits, raw vegetables, cooked vegetables, beans, milk, fish, candies, cookies, soft drinks, hamburgers, fried snacks, French fries/fried cassava/ fried bananas, mayonnaise, instant noodles, breakfast, natural juice | 16 components, score based on frequency, range 15–16 | Sociodemographic factors |
| Jaime et al (2010)55 | Diet Quality Index (DQI-a) | HEI-1995 | Brazil; adults | Grains, vegetables, fruit, milk/dairy products, meats, legumes, total fat, saturated fat, sodium, diet variety | 10 components, score based on servings and grams and E%, range 0–100 | Sociodemographic factors, BMI, food groups, nutrient intakes, se/sp analysis |
| CENTRAL AMERICA | ||||||
| Enneman et al (2009)56 | Dietary Diversity Score (DDS) | USAID | Guatemala; infants | Grains/roots/ tubers, legumes/nuts, dairy products, flesh foods, eggs, vitamin A–rich fruits and vegetables, other fruits and vegetables, fats/oils | 8 components, score based on consumption, range 0–8 | Day-to-day variation, sociodemographic factors |
| Enneman et al (2009)56 | Dietary Diversity Score (DDS) | Guatemalan dietary guide | Guatemala; infants | Grains (legumes) cereals/potatoes, herbs/vegetables, fruits, meat, milk/ milk products, sugar/fats | 6 components, score based on consumption, range 0–6 | Day-to-day variation, sociodemographic factors |
| Enneman et al (2009)56 | Dietary Diversity Score (DDS) | Institute of Nutrition of Central America and Panama (INCAP) | Guatemala; infants | Corn/corn tortilla/corn gruel, corn tamales, beans, rice, bread, breakfast cereals, other cereals, milk/dairy products/egg, meat/ beef/pork, game meat, chicken/turkey, fish/shellfish, green leaves, green/yellow vegetables, other vegetables, potatoes/root crops/ plantain, fruit, fats/oils, sugar, beverages, snacks, desserts, soups, other mixed dishes with meat, miscellaneous | 25 components, score based on consumption, range 0–25 | Day-to-day variation, sociodemographic factors |
| NORTH AMERICA | ||||||
| Macedo-Ojeda et al (2016)57 | Mexican Diet Quality Index (ICDMx) | Recommendations for food and nutrient intake issued by Mexican experts | Mexico; adults | Energy requirements, iron, calcium, fiber, water, protein, lipids, carbohydrates, vegetables and fruits, cereals, legumes and animal products, food variety (vegetables and fruits, cereals, legumes and animal product), SFA, PUFA, sodium, alcohol | 17 components, % of recommended (energy) intake or gram, range 0–100 | Reproducibility, relative validity, biomarkers, nutrient intake |
| Monterrosa et al (2015)58 | Infant and Young Child Feeding (IYCF) index | WHO dietary diversity indicator | Mexico; infants | Breastfeeding, use of bottles, sweetened and carbonated beverages, dietary diversity score (grains/tubers, fruits, vegetables, legumes/nuts, egg, flesh foods, dairy) | 4 components, score based on consumption, range 0–10 | Prepregnancy BMI |
Abbreviations: BDI, Balanced Diet Index; BMI, body mass index; E%, percentage of energy; HEI, Healthy Eating Index; PUFA, polyunsaturated fatty acid; se/sp analysis, sensitivity/specificity analysis; SFA, saturated fatty acid; SSB, sugar-sweetened beverage; UFA, unsaturated fatty acid; USAID, United States Agency for International Development; WHO, World Health Organization of the United Nations.
Some diet quality indices are more extensively evaluated and described in additional publications; however, our review search was not specifically set up for such validation studies, and thus articles describing such validation studies are not included in our review.
Table 4.
Identified diet quality indices from the literature for high-income countries, organized by region and country
| Reference | Index | Theoretical basis | Country and target group | Components | Scoring system | Evaluationa |
|---|---|---|---|---|---|---|
| ASIA | ||||||
| Nishimura et al (2015)96 | Food-based diet quality score for Japanese | Japanese food guide Spinning Top (2005) | Japan; adults | Grain dishes, vegetable dishes, fish and meat, milk, fruits, snacks and alcoholic beverages | 6 components, servings or energy, range 0–60 | Sociodemographic factors, nutrient intakes, metabolic risk factors, BMI, anthropometrics |
| Kuriyama et al (2016)81 | Modified food-based diet quality score for Japanese | Japanese food guide Spinning Top (2005) | Japan; adults | Grain dishes, vegetable dishes, fish and meat, milk, fruits, snacks and alcoholic beverages, seasonings | 7 components, servings or energy, range 0–70 | Sociodemographic factors, nutrient intakes, food groups, original food-based diet quality score for Japanese |
| Lee et al (2008)84 | Overall Dietary Index Revised (ODI-R) | Taiwanese Dietary Recommendations | Taiwan; adults | Grains/starchy tubers (whole grains), vegetables, fruits, eggs/soy/fish/meat (soybean, fish), dairy products, K/Na ratio, cholesterol, dietary moderation (refined sugars, Na, alcohol), dietary diversity. | 9 components, score based on servings, E%, or amounts consumed, range 0–100 | Nutrient intakes, other DQ score (ODI) |
| NORTH AMERICA | ||||||
| Jessri et al (2017)75 | Healthy Eating Index–Canada 2010 (HEI-C 2010) | HEI-2010 and Canada’s Food Guide (CFG) 2007 | Canada; children, adolescents, adults | Total fruit and vegetables, whole fruit, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, FAs, refined grains, Na, empty calories | 11 components, amount intake per 1000 kcal and E%, range 0–100 | Sociodemographic factors, nutrient intakes, food groups, reliability, BMI |
| Woodruff and Hanning (2010)117 | Canadian Healthy Eating Index (HEIC-2009) | Canada’s Food Guide recommendations (HEIC-2009) | Canada; children, adolescents | Grains, vegetables/fruits, milk, meat, other, total fat, saturated fat, cholesterol, dietary variety | 9 components, score based on servings and E%, range 0–100 | Other DQ index (HEI-C) |
| Sharafi et al (2015)105 | Healthy Eating Preference Index (HEPI) | Dietary Guidelines for Americans 2010 | USA; preschool children | High-fat/sweet/salty foods, fruits and vegetables, variety score | 6 components, score based on liking scores, range −250 to 250 | Sociodemographic factors, BMI, biomarker, other DQ score (HEI 2010), reliability |
| Anderson et al (2015)59 | Healthy score and unhealthy score | Not specified | USA; preschool children | Healthy: fruits, vegetables, milk Unhealthy: SSB, fast food, sweets, salty snacks | Healthy/unhealthy score: 3 components / 4 components, both scores based on frequency, range 0–18/range 0–24 | Food groups |
| Vadiveloo et al (2014)109 | US Healthy Food Diversity (HFD) Index | 2010 Dietary Guidelines for Americans and German algorithm | USA; adults | 26 food groups, not specified | 26 components, score based on proportion of the food eaten and a health factor, range 0–1 | Sociodemographic factors, food groups, (mean) probability of nutrient adequacy, other DQ score (DASH diet score) |
| Guenther et al (2013)71 | Healthy Eating Index (HEI) 2010 | 2010 Dietary Guidelines for Americans | USA; children, adolescents, adults | Total fruit, whole fruit, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, FAs, refined grains, Na, empty calories | 12 components, amount intake per 1000 kcal and E%, range 0–100 | Not described in this publication but for evaluation, see, for example, Guenther et al20 and Anic et al21 |
| Lipsky et al (2012)87 | Whole Plant Foods (WPF) | MyPyramid and Center for Nutrition Policy and Promotion of Fruit and Fruit Juice | USA; children, adolescents, adults | Whole fruit, vegetables, whole grains, legumes, nuts, seeds | 6 compounds, score based on amounts, or proportion of intake | Biomarker, biomarkers for CVD, diabetes, and inflammation, other DQ score (HEI-2005) |
| Rumawas et al (2009)103 | Mediterranean-Style Dietary Pattern Score (MSDPS) | Mediterranean diet pyramid | USA; adults | Whole-grain cereals, fruits, vegetables, dairy, wine, fish, poultry, olives/ legumes, nuts/potatoes, eggs, sweets, meats, olive oil | 13 components, score based on servings, range 1–100 | Sociodemographic factors, anthropometrics, nutrient intakes, food groups |
| Falciglia et al (2009)65 | Dietary variety score | US MyPyramid (2005) | USA; children | Number of foods and beverages consumed in 1 day based on servings | All foods and drinks consumed, score based on prediction equation | Reproducibility (3-day recall vs 15-day recall) |
| Guenther et al (2008)72 | Healthy Eating Index–2005 (HEI-2005) | Dietary Guidelines for Americans 2005 | USA; children, adolescents, adults (not pregnant) | Total fruit, whole fruit, total vegetables, dark green and orange vegetables and legumes, total grains, whole grains, milk, meat and beans, oils, saturated fat, Na, calories from solid fats/alcoholic beverages/added sugars | 12 components, score based on amounts consumed /1000 kcal, range 0–100 | Not described in this article but for evaluation see, for example, Guenther et al18 and Grimstvedt et al19 |
| Fung et al (2008)67 | DASH-style diet | DASH diet | USA; women | Fruits, vegetables, whole grains, nuts and legumes, low-fat dairy, red and processed meats, sweetened beverages, and Na | 8 components, score based on quintiles of intake, range 8–40 | Sociodemographic factors, nutrient intakes, food group, CHD, stroke, BMI |
| AUSTRALIA/NEW ZEALAND | ||||||
| Gasser et al (2017)68 | Dietary score | Australian Dietary Guidelines 2013 | Australia; children | Fruits, vegetables, water, fatty foods, sugary foods, SSB, milk products or alternatives | 7 components, frequency, range 0–14 | Dietary patterns, change of food group trajectories over age |
| Roy et al (2016)101 | Healthy Eating Index for Australian Adults (HEIF-2013) | Australian Dietary Guidelines 2013 | Australia; young adults | Adequacy: vegetables, fruits, grain (cereal) foods, milk and milk alternatives, meat and protein food alternatives, water | 11 components, score based on servings, range 0–100 | Nutrient intakes, food groups, relative validity |
| Limitation: discretionary foods high in saturated fat or added sugars, added salt, alcohol | ||||||
| Thorpe et al (2016)108 | Dietary Guideline Index 3013 (DGI-2013) | Australian Dietary Guidelines 2013 | Australia; adults | Adequacy: Food variety, vegetables, fruits, grain (cereal) foods, lean meat and poultry/fish/eggs/nuts/seeds/legumes/beans, milk/yogurt/cheese and alternatives, water | 13 components, score based on servings or type of product, range 0–130 | Sociodemographic factors, health behaviors, BMI |
| Limitation: foods containing SFA/salt/sugars/alcohol, foods high in SFA, fatty foods, salty foods, sugary foods, alcohol | ||||||
| Taylor et al (2015)107 | Healthy trolley index (HETI) | Australian Guide to Healthy Eating | Australia; adults | Grains/cereals, meat and alternatives, dairy foods and alternatives, fruit, vegetables, discretionary (eg, savory snacks, confectionery, SSB, alcohol, processed meat, baked goods) | 6 components, score based on monthly food expenditure, range 0–100 | Sociodemographic factors, foods/food groups, overweight/obesity |
| Zarrin et al (2013)118 | Aussie_DQI | National dietary guidelines linked to the Australia National Health Priority Areas | Australia; adults | Vegetables, fruit, dairy products, meat and alternatives, cereals, E% SFA, E% sugar, alcohol, processed meat, added salt/Na, dietary variety (vegetables, fruits, wholegrain, fish) | 11 components, score based on servings, E%, and amounts, range 0–120 | Sociodemographic factors, nutrient intakes, food groups, BP, all-cause and cancer mortality, overweight, obesity |
| Spence et al (2013)106 | Obesity Protective Dietary Index (OPDI) | Based on the intended trial outcomes | Australia; toddlers | Fruits, vegetables, noncore foods | 3 components, score based on grams and KJ, range 0–30 | Nutrient intakes, intervention vs control group of intervention |
| Scott et al (2012)104 | Fruit and Vegetable Variety Score (FVVS) | Australian Guide to Healthy Eating | Australia; children | Vegetables, fruits | 16 components, score based on consumption, range 0–16 | Sociodemographic factors, breastfeeding |
| Scott et al (2012)104 | Core Food Variety Score (CFVS) | Australian Guide to Healthy Eating | Australia; children | Milk/dairy, grains and grain products, vegetables, fruits, meat or other nondairy protein sources | 34 components, score based on consumption, range 0–34 | Sociodemographic factors, breastfeeding |
| Marshall et al (2012)93 | Australian Child and Adolescent Recommended Food Score (ACARFS) | Dietary Guidelines for Children and Adolescents in Australia and US Recommended Food Score | Australia; children and adolescents | Vegetables, fruit, protein foods (meat/flesh), protein foods (meat/flesh alternatives), grains, dairy, water, extras | 8 components, score based on frequency and servings, range 0–73 | Sociodemographic factors, BMI, nutrient intakes, nutrient reference values |
| Li et al (2012)86 | Index of Diet Quality | Scientific literature and Australian recommendations | Australia; adolescents | Breads/cereals/rice/pasta/noodles, vegetables, fruit, milk/yoghurt/cheese, meat/fish/poultry/eggs/nuts/legumes, extra foods (soft drinks, chips etc.), vitamin C, vitamin A, dietary fiber, Fe, Ca, protein, total fat (%KJ), saturated fat (%KJ), n-6/n-3 FA ratio | 15 components, score based on amounts consumed and E%, range 20–150 | Sociodemographic factors |
| Golley et al (2011)69 | Dietary Guideline Index for Children and Adolescents (DGI-CA) | Australian Dietary Guidelines 2003 for children and adolescents | Australia; children and adolescents | Fruit, vegetables, bread and cereals, whole-grain cereals, meat and alternatives, dairy foods, reduced-fat dairy, fluids, extra foods (nutrient poor and high in fat, salt, and added sugar), healthy fats/oils, diet variety | 11 components, score based on servings, range 0–100 | Sociodemographic factors, anthropometrics, food groups, nutrient intakes |
| McNaughton et al (2008)94 | Dietary Guideline Index (DGI) | Australian Guide to Healthy Eating | Australia; adults | Vegetables/legumes, fruit, total cereals, meat and alternatives, total dairy, beverages, Na, saturated fat, alcoholic beverages, added sugars, whole-grain cereals, lean meat, reduced/low fat dairy, dietary variety, extra foods | 15 components, score based on servings, type or frequency, range 0–150 | Sociodemographic factors, anthropometrics, nutrient intakes, BP |
| Wong et al (2017)115 | Healthy Dietary Habits Index (HDHI) | New Zealand Food and Nutrition Guidelines for Healthy Adults 2003 | New Zealand; adults | Red meat, chicken, fish/shellfish, milk, spread, low-fat foods, fries, bread, fruit, vegetables, soft drinks, breakfast, fast foods, added salt, low-salt foods. | 15 components, score based on frequencies, servings or type of product, range 0–60 | Sociodemographic factors, BMI, nutrient intakes, nutritional biomarkers |
| Wong et al (2014)114 | Healthy Dietary Habits Score for Adolescents (HDHS-A) | Scientific literature and New Zealand Food and Nutrition Guidelines for Healthy Children and Young people | New Zealand; adolescents | Fat from meat/poultry/fish, other fats, fruit, vegetables and bread, sugar sources, meal habits | 17 components grouped in 5 clusters, score based on frequency and servings, range 0–68 | Sociodemographic factors, BMI, nutrient intakes, biomarker, expert review, reliability |
| Wong et al (2013)116 | New Zealand Diet Quality Index for Adolescents (NZDQI-A) | New Zealand Food and Nutrition Guidelines for Healthy Adolescents | New Zealand; adolescents | Fruits, vegetables, bread and cereals, milk and milk products, meat and alternatives | 5 components, score based on servings and frequency, range 0–100 | Nutrient intakes, reproducibility, reliability, relative validity |
| EUROPE | ||||||
| Freisling et al (2009)66 | Food frequency index (FFI) | Austrian Food Based Dietary Guidelines | Austria; adults | Vegetables, fruits, whole-meal bread, pasta/rice, pulses, nuts, milk products, beef/pork, processed meats, poultry | 10 components, score based on frequency, range 0–70 | Sociodemographic factors, BMI, nutrient intakes, biomarker, cholesterol |
| Vandevijvere et al (2010)110 | Dietary diversity, dietary adequacy, dietary moderation, and dietary balance scores | Food-based dietary guidelines (FBDG) | Belgium; adults | Water (including coffee, tea and broth), bread/cereals, grains and potatoes, vegetables, fruits, dairy products (including Ca-enriched soy products, excluding cheese), cheese, meat/fish/eggs/legumes/nuts/meat substitutes, spreadable fats, energy-dense nutrient-poor foods | 4 scores, based on servings | Sociodemographic factors, BMI, scores are compared among each other |
| Huybrechts et al (2010)74 | Diet Quality Index (DQI) | Flemish Dietary gGidelines 2004 | Belgium; preschool children | Dietary diversity, dietary quality, dietary moderation, dietary adequacy, dietary equilibrium, meal index | 6 components, score based on amounts and recommendations, range 25%–100% | Nutrient intakes, reproducibility, relative validity |
| Lazarou et al (2009)82 | E-KINDEX | Not mentioned | Cyprus; children | Bread, cereals, and grain foods (excluding bread), fruit and fruit juices, vegetables, legumes, milk, fish and seafood, meat, salted and smoked meat food, sweets and snack items, soft drinks, fried food, grilled food | 13 components, Score based on frequency, range 0–37 | BP |
| Biltoft-Jensen et al (2008)60 | Simple Diet Quality Index (SDQI) | Danish Dietary Guidelines, NNR 2004 | Denmark; adults | Saturated fat, fiber | 2 components, score based recommended intake, range 0–100 | Sociodemographic factors, nutrient intakes, food groups, obesity, overweight |
| Meinilä et al (2016)95 | Healthy Food Intake Index (HFII) | Nordic Nutrition Recommendations (NNR) | Finland; pregnant women | Vegetables, fruits/berries, high-fiber grains, fish, low-fat milk, low-fat cheese, cooking fat, fat spread, snacks, SSB, fast food | 11 components, frequencies, range 0–17 | Sociodemographic factors, BMI, nutrient intakes, reproducibility |
| Roytio et al (2015)102 | Children’s Index of Diet Quality (CIDQ) | Nordic Nutrition Recommendations | Finland; children | Fiber, vegetables, fruits and berries, SFA, PUFA, saccharose, Ca | 6 components, score based on E% and gram intake, range 0–21 | BMI, nutrient intakes, biomarker, se/sp analysis |
| Kanerva et al (2014)77 | Baltic Sea Diet Score (BSDS) | Baltic Sea Diet Pyramid | Finland; adults | Fruits and berries, vegetables, cereals, low-fat milk, fish, meat products, total fat, fat ratio (PUFA to SFA + trans fatty acids), alcohol. | 9 components, score based on quartiles, range 0–25; or score based on median, range 0–9 | Sociodemographic factors, BMI, nutrient intakes |
| Leppala et al (2010)85 | Index of Diet Quality (IDQ) | Nordic Nutrition Recommendations and Finish Nutrition Recommendations | Finland; adults | Whole-grain products, fat-containing foods, dairy products, vegetables/ fruits/berries, sugar, meal pattern | 6 components, score based on frequency, range 0–15 | Nutrient intakes, se/sp analysis, BMI |
| Estaquio et al (2008)64 | French Score of Indicators of the PNNS Objectives (FSIPO) | Program Nutritional Nutrition Santé | France; adults | Fruits/vegetables, Ca, total fat, saturated fat, carbohydrate consumption, complex carbohydrates, simple sugars, fiber, alcohol, cholesterol level, SBP, BMI, physical activity | 13 components, score based on servings or RDA or %E intake, range 0–17.5 | Sociodemographic factors, nutrient intakes, biomarkers, NCDs |
| Kleiser et al (2009)78 | Healthy Nutrition Score for Kids and Youth (HuSKY) | OMD recommendations | Germany; children and adolescents | Beverages, vegetables, fruit, fish, bread/ cereals, pasta/rice/potatoes, milk/dairy products, eggs, fats, meat/ sausages, sweets/fatty snacks/soft drinks | 11 components, score based on the proportion to recommended intake, range 0–100 | Sociodemographic factors, biomarkers |
| Manios et al (2015)91 | Revised Healthy Lifestyle-Diet Index (R-HLD-Index) | USDA’s Choose My Plate recommendations | Greece; children and adolescents | Fruits, vegetables, grains, milk/dairy products, meat/meat products, fish/seafood, legumes, eggs, soft drinks, sweets, physical activity status, time spend on moderate to vigorous physical activity | 12 components, score based on servings and time spent on activity, range 0–48 | overweight, obesity, iron deficiency |
| Manios et al (2010)90 | Healthy Lifestyle-Diet Index (HLD-Index) | MyPyramid, American Academy of Pediatrics | Greece; children | Fruits, vegetables, grains, dairy products, meat, fish/seafood, soft drinks, sweets, physical activity, screen time | 10 components, score based on servings and time spent on activity, range 0–40 | Nutrient intakes, insulin resistance, estimated average requirements |
| Manios et al (2010)89 | Preschoolers Diet-Lifestyle Index (PDL-Index) | USDA food guide pyramid, Canada’s Food Guide, American Heart Association, American Academy of Pediatrics | Greece; preschool children | Fruits, vegetables, total grains, dairy products, red meat, white meat/ legumes, fish/seafood, unsaturated fats, sweets, physical activity, screen time | 11 components, score based on servings and time spent on activity, range 0–44 | Nutrient intakes, food groups, estimated average requirements, obesity, overweight |
| Kourlaba et al (2009)80 | Elderly Dietary Index (EDI) | Modified MyPyramid for Older Adults and features of the Mediterranean diet | Greece; elderly | Meat, fish, fruits, vegetables, cereals, legumes, olive oil, alcohol, type of bread, dairy products | 10 components, score based on frequency, range 10–40 | Sociodemographic factors, food groups, obesity, hypertension, hypercholesterolemia, diabetes |
| Kosti et al (2009)79 | Diet-Lifestyle Index | Scientific literature | Greece; adolescents | Vegetables, fruits, whole grains, sweets/added sugars, breakfast cereals, dairy products, sports activities, sedentary behavior, consumption of breakfast, eating away from home, number of eating episodes a day, visible fat consumption, obesity status of parents | 13 components, score based on servings, type or behavior, range 11–57 | Sociodemographic factors, obesity, overweight |
| Perry et al (2015)98 | Diet Quality Score (DQS) | Irish guidelines | Ireland; children | Fruit, fruit juice, meat/chicken/fish, eggs, cooked vegetables, raw vegetables, meat pie/hamburger/hot dog/sausage, hot chips or french fries, crisps/savory snacks, bread, potatoes/pasta/rice, cereals, biscuits/doughnut/cake/pie/chocolate, cheese/yoghurt/fromage frais, low fat cheese/low fat yogurt, water, soft drinks (not diet), soft drinks (diet), full-cream milk and products, skimmed milk and products | 20 components, score based on frequency, range 12–28 | Sociodemographic factors, food groups, obesity/ overweight |
| Looman et al (2017)88 | Dutch Healthy Diet Index 2015 (DHD15-Index) | Dutch Dietary Guidelines 2015 | The Netherlands; adults | Vegetables, fruit, whole-grain products, legumes, nuts, dairy, fish, tea, fats and oils, coffee, red meat, processed meat, SSsB and fruit juices, alcohol, salt | 15 components, grams per day, range 0–150 | Sociodemographic factors, nutrient intakes, relative validity |
| Lee et al (2012)83 | Dutch Healthy Diet Index (DHD-Index) | Dutch Guidelines for a Healthy Diet 2006 | The Netherlands; adults | Physical activity, vegetables, fruit / fruit juices, fiber, fish, SFA, TFA, acid drinks and foods, Na, alcohol | 10 components, score based on activities, grams or E%, range 0–100 | Sociodemographic factors, BMI, food groups, nutrient intakes |
| Voortman et al (2015)113 | Diet Quality Score (DQS) | National and international guidelines and scientific literature | The Netherlands; toddlers | Vegetables, fruit, bread/cereals, rice/ pasta/potatoes/ legumes, dairy, meat/ eggs, fish, oils/fats, candy/snacks, SSBs | 10 components, score based on intake in grams and adjusted for energy intake, range 0–10 | Sociodemographic factors, anthropometrics, BMI (NS), nutrient intakes |
| Jonge et al (2015)76 | Bone Mineral Density (BMD) diet score | Scientific literature | The Netherlands; elderly | Vegetables, fruits, dairy products, whole grain products, fish/seafood, legumes/ beans, meat, confectionary | 8 components, score based on quartiles, range 8–24 | Sociodemographic factors, biomarker, anthropometrics, NCDs, bone mineral density, other DQ score (HDI) |
| Jonge et al (2015)76 | Healthy Diet Indicator (HDI) (adapted from Jankovic et al119) | WHO dietary guidelines 2003 | The Netherlands; elderly | SFA, mono- and disaccharides, cholesterol, trans fat, Na, PUFA, protein, total fat, n-6 PUFA, n-3 PUFA, dietary fiber, fruits/vegetables | 12 components, score based on grams intake, range 0–120 | Bone Mineral Density |
| Hillesund et al (2014)73 | New Nordic Diet (NND) Score | Guidelines of the NND | Norway; women (mothers) | Meal pattern, Nordic fruit consumption, root vegetables, cabbages, potatoes, whole grain breads, oatmeal porridge, food from the wild countryside, milk, water | 10 components, score based on frequency and type, range 0–10 | Sociodemographic factors, food groups, nutrient intakes, BMI, pregnancy outcomes |
| Rodríguez-Martin et al (2017)100 | EVIDENT diet quality index | Scientific literature | Spain; adults | Adequacy: Low-fat dairy, poultry, rabbit, fish, dark-yellow vegetables, green leafy vegetables, cruciferous vegetables, other vegetables, gazpacho, potatoes, fruits, fresh fruit juice, beans/lentils/chickpeas, whole-grain bread/rice/cereal/pasta, olive oil, green/black tea, red wine, beer | 36 components, frequency per week/day, range 0–100 | Sociodemographic and lifestyle factors, nutrient intake, food groups, Mediterranean diet, CVD risk, BP, anthropometrics, pulse wave velocity |
| Limiting: whole-fat dairy, ice cream, red meat, processed meat, pizza, fried potatoes, salty snack foods, added fats/ oils, butter, sweet breads, desserts, added sweets, precooked meals, sauce (ketchup, mayonnaise), honey, jam, soda, bottled juices | ||||||
| Mariscal-Arcas et al (2009)92 | Mediterranean Diet Index for pregnant women (MDS-P) | Mediterranean diet and specific needs during pregnancy based on scientific literature | Spain; pregnant women | Vegetables, fruits/nuts, pulses, cereals, fish, MUFA/SFA ratio, meat, dairy products, Fe, Ca, folic acid | 11 components, scored based on RDI, range 0–11 | Anthropometrics, nutrient intakes, food groups, pregnancy outcomes |
| Drake et al (2011)63 | Diet Quality Index–Swedish Nutrition Recommendations (DQI-SNR) | Swedish Nutrition Recommendations (SNR) and the Swedish Dietary Guidelines (SDG) | Sweden; adults | SFA, PUFA, fish and shellfish, dietary fiber, fruit and vegetables, sucrose | 6 components, score based on intake in weights and E%, range 0–6 | Sociodemographic factors, anthropometrics, food groups, nutrient intakes, BP and NCDs |
| Cleghorn et al (2016)61 | Dietary quality score (DQS) | WHO/FAO expert consultation group 2003 | UK; adults | Fruit, vegetable, oily fish, nonmilk extrinsic sugar, fat | 5 components, servings or gram per day, range 0–15 | Relative validity, foods |
| Verger et al (2015)112 | Probability of Adequate Nutrient Intake (PANDiet) score (updated) | United Kingdom nutritional recommendations | UK; young children | Protein, total carbohydrates, non-milk extrinsic sugars, total fat, SFA, PUFA, thiamin, riboflavin, niacin, folate, vitamin A, vitamin B6, vitamin B12, vitamin C, vitamin D, Ca, magnesium, zinc, phosphorus, potassium, Fe, copper, selenium, iodine, Na | 25 nutrients, scored based on adequacy probability, range 0–100 | Sociodemographic factors, food groups, consumption of infant formula/foods |
| Pot et al (2014)99 | Eating Choices Index (ECI) | Based on NSHD consumption data and discussion with researchers | UK; adults | Consumption of breakfast, consumption of 2 portions of fruit per day, type of milk consumed, type of bread consumed | 4 components, score based on frequency and type, range 4–20 | Sociodemographic factors, nutrient intakes, overweight, obesity |
| Golley et al (2012)70 | Complementary Feeding Utility Index (CFUI) | Complementary feeding guidelines of Australia, New Zealand, USA, and UK | UK; infants | Breastfeeding duration, feeding on demand, timing of introduction to solids, exposure to Fe-rich cereals, fruit, vegetables, protein foods variety, exposure to sugary drinks, exposure to confectionary, cakes, savory snacks, cow milk introduction, exposure to tea, timing of lumpy food intro, exposure to commercial infant foods, daily meal/snack frequency. | 14 components, score based on probability function, range 0–1 | Sociodemographic factors, BMI, food group, nutrient intake, feeding behavior |
| Crombie et al (2009)62 | Diet quality score | Caroline Walker Trust, Eat Well plate | UK; women (mothers) | Bread/other cereals/potatoes, fruit/ vegetables, dairy products, meat/ fish/ alternatives, high-fat/ high-sugar snacks | 5 components, score based on daily portions, range 0–5 | Maternal knowledge and views |
| Oliveira et al (2015)97 | Healthy Plate Variety Score | Modified version of food variety index for toddlers | Portugal, UK, France; children | Starchy foods (including potatoes), fruits, vegetables, meat/fish/alternatives, dairy foods | 5 components, score based on servings, range 0–5 | Children’s eating behavior |
| Vereecken et al (2008)111 | Fruit and vegetable index, fiber index, calcium index, variety index, excess index, short excess index | Not mentioned | Belgium and Italy; children | Fruit and vegetable index, fiber index (FV and brown bread), Ca index (whole-fat milk, semi-skimmed milk, cheese, and other milk products), variety index (combination of fiber index and Ca index), excess index (carbonated sugared soft drinks, sweets, chips, crisps), short excess index (soft drinks, sweets) | Not specified | Nutrient intakes, reproducibility, relative validity |
Abbreviations: BMI, body mass index; BP, blood pressure; Ca, calcium; CHD, coronary heart disease; CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension; DQ, diet quality; EVIDENT, Estilos de vida y disfunción endotelial; E%, percentage of energy; FA, fatty acid; FAO, Food and Agricultural Organization of the United Nations; Fe, iron; FV, food variety; HEI, Healthy Eating Index; K, potassium; %KJ, percentage of kilojoule; MUFA, monounsaturated fatty acid; Na, sodium; NCD, noncommunicable disease; NS, not significant; NSHD, The Medical Research Council National Survey of Health and Development; OMD, optimized mixed diet; PNNS, Program Nutritional Nutrition Santé; PUFA, polyunsaturated fatty acid; RDA, Recommended Dietary Allowance; RDI, Recommended Dietary Intake; SBP, systolic blood pressure; se/sp analysis, sensitivity/specificity analysis; SFA, saturated fatty acids; SSB, sugar-sweetened beverage; TFA, total fatty acid; USDA, United States Agency for International Development; WHO, World Health Organization of the United Nations.
Some diet quality indices are more extensively evaluated and described in additional publications; however, our review search was not specifically set up for such validation studies, and thus articles describing such validation studies are not included in our review.
Theoretical basis of the index
The majority of the indices are based on national dietary recommendations (n = 54) originating from the country where the index was developed. These national guidelines are often established by an expert group based on scientific literature. For some indices, such as the Bone Mineral Density (BMD) Diet score76 and the Diet-Lifestyle Index79 the authors of the paper performed a scientific literature search. Nine of the 14 indices developed for LMICs use national dietary guidelines48–50,52–57; 3 use recommendations by internationally oriented organizations56,58; the Infant and Young Child Feeding Index (ICFI)47 is based on scientific literature; and Hardiansyah et al do not mention their source.51 Indices based on national dietary recommendations might be useful for in-country comparison and trend analysis, and they take into consideration the availability of foods and cultural dietary preferences. However, such indices should be used carefully for cross-country comparisons because their generalizability might be limited, especially regarding the foods or food groups included in the index. Indices that can be applied globally, allowing for cross-country comparison, include those based on assessing the adherence to a specific health-improving diet, such as the Mediterranean diet,80,92,103 the DASH (Dietary Approaches to Stop Hypertension) diet,67 or the Nordic diet,73,85,95,102 but these are specific for a region or based on a Western diet (DASH diet). Other indices are based on international guidelines—for example, the Healthy Diet Indicator (HDI),76 based on the 2003 WHO dietary guidelines for elderly; the Diet Quality Score (DQS),61 based on the WHO/FAO Diet, Nutrition and the Prevention of Chronic Diseases Expert Consultation (2003); and the Infant and Young Child Feeding (IYCF) index,58 applied in the context of Mexico but based on WHO best practices for complementary feeding guidelines for infants and young children.45 The HDI and DQS, both applied in the Netherlands, and the IYCF, applied in Mexico, could allow for comparison of food system diet quality associations in different LMIC settings. However, these 3 diet quality indicators have only been tested in 1 country, with the Netherlands being a high-income country; thus additional research regarding their multi-LMIC applicability is needed.
Target group
The reviewed diet quality indices were developed for various age groups, from toddlers to the elderly, although most were developed for the general adult population (without specification of age range, n = 28), young children (infants, toddlers, or preschool children, n = 14), or children (n = 12). Furthermore, specific indices were developed for women (n = 7), children and adolescents (n = 6), adolescents (n = 5), children and adolescents and adults (n = 5), adolescents and adults (n = 1), and the elderly (n = 3). Indices tailored to the needs of a specific population group are, for example, the Mediterranean Diet Index for pregnant women (MDS-P)92 and the Adolescent Micronutrient Quality Index (AMQI),52 although the latter is, according to the authors of the index, easily adjustable for other population groups. There are also scores, such as the HEI-2010,71 that have been developed for a wide population group (children, adolescents, and adults). All diet quality scores list the target group for which it is intended to be used. Different age and sex groups have different requirements (due to, for example, differences in physiological needs or different food preferences during the life course), and therefore 1 index may not fit all target groups equally well.
Components of diet quality indices
Components included in diet quality indices are nutrients, foods, and/or food groups; occasionally they incorporate lifestyle factors. The diet-related components are either recommended to be limited (unhealthy) or enhanced (healthy), and both limiting and enhancing components are sometimes included in 1 index. Fifty-four indices, such as the Diet Quality Scores of Voortman et al113 and Perry et al,98 consist exclusively of foods and/or food groups; 24 indices, such as the Index of Diet Quality,86 consist of foods, food groups, and nutrients; and 344,60,112 include nutrients only. Foods and/or food groups that are mostly included (on different aggregation levels) are fruits, vegetables, staple foods, sugar, dairy products, and other protein sources like meat, eggs, and plant-based protein foods. Nutrients frequently included are sodium, cholesterol, trans fatty acids, unsaturated fatty acids, and n-3 fatty acids. Some indices include other lifestyle factors, like physical activity or time spent watching TV or playing computer games (screen time).64,79,83,89–91 For 7 indices, meal pattern (eg, consumption of breakfast yes or no) was included as 1 of the components.47,70,74,79,85,99,114 Eight43,48,51,59,100,101,108,110 diet quality scores separately calculate a healthy (adequacy) and unhealthy (limiting) part, such as the score from Anderson et al.59 The number and type of components included and the level of aggregation differed broadly for the listed indices, mainly depending on the target group, the intended association between the index and specific health outcome(s), and the detail of food intake data available (depending on the detail of the questionnaire used). Indices including nutrients are generally based on extensive dietary intake data collection and need valid food composition tables, which are often of limited availability in LMICs.
Scoring system
Components are individually scored, and the scoring could be based on medians, tertiles/quartiles/quintiles of the study population, consumption (yes or no), or on recommended amounts consumed, which were either estimated in portions, servings, or weights and sometimes corrected for energy intake. For all indices, the scoring of the individual components is summed into 1 total score and the range of the total score varies highly for the different indices. Not all indices have continuous total scoring; for 3 indices (US Healthy Food Diversity [HFD] index,109 Complementary Feeding Utility Index [CFUI]70 and the WHO’s indicators for infant and young child feeding45) the total score is dichotomized. Scoring components based on amounts, rather than consumption yes or no, seems preferable because it allows for refining the scoring system, increasing the possibility of variation in the score and thus improving association with diseases. However, this requires obtaining information about amounts or portion sizes consumed during data collection, which is challenging in LMICs.120 Also, to the best of the authors’ knowledge, no research has been done on which scoring system is preferable in which situation. There are indices (such as the HEI 200572 and 201071) that score the individual components on a density basis because many recommendations are similar across energy levels; this counteracts a higher intake of foods or food groups caused by a higher energy intake.
Evaluation
The listed diet quality indices have been evaluated in numerous ways. Evaluation strategies include assessing its reproducibility (whether the index yields similar outcomes when assessed on 2 different occasions), reliability (internal consistency), relative validity (whether the index generates similar results when dietary intake data collected by 2 different methods are used), sensitivity/specificity analysis, its ability to discriminate according to sociodemographic factors, and its association with relevant nutrients, foods, and/or food groups intakes (construct validity). An example of an extensively evaluated diet quality score is the New Zealand Diet Quality Index for Adolescents (NZDQI-A)116; it showed an average reliability (Crohnbach’s α = 0.51) and a low overall relative validity (r = 0.39). The construct validity showed that in the highest tertile of the NZDQI-A higher intakes of iron and lower intakes of total fat, saturated fatty acids, and monounsaturated fatty acids (MUFAs) were observed.116
In some papers an association analysis of the index with a health outcome, such as nutrient adequacy, pre-disease state biomarker, obesity or overweight, disease, or overall mortality, was performed. This is less frequently described in papers where the development of the index is discussed because such an analysis is often a next step in the evaluation of a diet quality index. An example from this review of a diet quality index associated with a health outcome is the Aussie Diet Quality Index118; its outcome is related to cancer mortality, overweight, and obesity. Note that diet quality indices comprised of components related to diseases (like sodium intake and coronary heart disease) generally show a higher predictive accuracy, whereas including general and not disease-specific components could lead to dilution of the index–disease association.121 Which health or nutrition outcome to use for validation depends on the aim underlying the development of the index (eg, the DASH index was developed to be associated with hypertension and the Bone Mineral Density [BMD] index with BMD).
When a diet quality index is validated with nutrient intakes or nutrient adequacies obtained by the same dietary assessment method in the same study population as the one used to assess the components of the diet quality index correlated errors could cause higher correlations.121 Biomarkers of exposure (eg, urinary sodium for sodium intake) are a preferred reference method because of their assumed independent error structure with reported intake measurements. Also, including a dietary diversity score or food variety score in the total diet quality index, while similar food groups are included as a separate component in the index, could introduce correlation among the different components of the index, which is the case for the Mexican Diet Quality Index (ICDMx).57 Furthermore, it causes these twice-included food groups to have a higher weight in the index; they thus have a higher importance in the overall score. Correlation among the different components could cause a reduction in the accuracy of the diet quality index.121
Validation of an index is of utmost importance before starting to use it in food system research projects. A food system entails the full process of feeding the population and includes all stages from growing to consumption. In general, validation should be done regardless of the use of a diet quality index in a food system project or not. It is recommended that the index be evaluated by assessing its reproducibility, reliability (internal consistency), relative validity, and construct validity, and by performing a sensitivity/specificity analysis; additionally an assessment of the association of the index with the health outcome(s) of interest, preferably in the intended target population, and when aiming to develop an index for global use, in different countries, should be completed. Furthermore, it is important to avoid correlated errors by using 2 independent datasets for validation purposes.
Dietary assessment method and use of screeners
The methods used to measure the dietary components of the diet quality indices deserve attention. For most of the components, the traditional dietary intake assessment methods—24-hour recall (24hR), food frequency questionnaire (FFQ), (weighed) food record, and diet history—were used. In the last decade, diet quality index–specific tools, developed to measure the components of that diet quality index, also known as screeners, have been increasingly used.122–124 Short screeners collect only the necessary data to estimate the components of a diet quality index. Development of such a screener takes place after the development of the diet quality score. Leppala et al evaluated such a tool against the index outcome obtained with a 7-day food record and concluded that this screener is a useful tool to measure the individual components of their diet quality index.85
Screeners measuring the relevant foods and products to assess the diet quality index could be useful in LMICs because they are relatively short and easy to administer compared with the traditional dietary intake methods, although some information regarding food intake is lost. Such a tool should undergo extensive validation before it can be widely used. When validated tools are not available, repeated 24hRs are a sound alternative. The repeated 24hR allows for adjustment of day-to-day variation of the individual dietary intake, provides a detailed list of the foods eaten, and is easiest, although time consuming, to administer in an LMIC setting.125
The 14 country-specific indices developed for LMICs and the 4 international indices developed for cross-country comparisons in LMICs are described according to their adherence to the 7 recommended points (Box 1) to be taken into account for the development of a diet quality index for LMICs (Table 5). The majority of the indices (n = 8) focus on the risk factors for NCDs and meeting the nutritional needs of the target group, whereas the child and infant indices (n = 6) focus on child survival as the outcome. Five indices include nutrients in addition to foods and/or food groups. All indices capture the variety dimension of diet quality, and 13 also mention the moderation dimension (include components that should be consumed in moderation). Nutrient adequacy was only mentioned for 4 indices, but this is often done as an evaluation of a diet quality index and not always described in the articles included in this review. Three indices include a separate score for unhealthy foods (eg, foods for which a maximum intake is recommended) in addition to a score for healthy foods (eg, foods that require a minimum intake). Nine indices make use of cutoff points to score the components rather than consumption yes or no. For 10 of the indices, the individual components were scored dichotomously, and only 1 index, the Chinese Healthy Eating Index (CHEI),48 used unequal weighing factors for the individual components.
Box 1 Suggested recommendations for developing a diet quality index in low- and middle-income countries
Food systems research is often multidisciplinary and includes a wide range of indicators to be collected (social, agricultural, production, nutrition). It is therefore of utmost importance that a diet quality index used in such a setting be easy to administer without compromising its validity and quality. The following 7 recommendations should be taken into account in developing such an index in the food system context.
Define the purpose of the index. For application of the diet quality score, it is important that the purpose includes the target group, because different age and sex groups have different needs, as well as the health outcome(s) of interest. Furthermore, the focus of the index should be not only on dietary deficiencies but also on obesity and NCDs to address the triple burden of disease, which represents a growing public health problem in LMICs.
Use foods and food groups instead of nutrients as components in the score. Sixty-seven percent of the 81 reviewed indices used foods and food groups only. It is important to use food and food groups instead of nutrients because of the limitations of food composition tables, such as being incomplete, being outdated, and lacking nutrient content of processed, fortified, and cooked foods. Thus creating an index that is based on foods and food groups would be preferred in LMICs.126
The index should capture the three dimensions of diet quality: nutrient adequacy, food variety or food diversity, and moderation of foods/food groups. Individual dietary diversity may reflect nutrient adequacy fairly well.127–131 Controversy exists about dietary diversity and the moderation dimension because a wider consumption of different foods might be related to excess energy intake,132 thus violating the energy balance. In most cases, assessing whether the nutrient adequacy dimension is fulfilled for the target group is done after assessing dietary diversity, acting as a validation step.
The limiting and enhancing foods/food groups should be included in separate scores. The recommendations include a division of the components included in the index into healthy and unhealthy components. Some of the reviewed diet quality indices already include separate scores for the healthy and unhealthy components.43,48,51,59,100,101,108 Three scores could be calculated, one including all components, the second including only healthy foods/food groups, and the third including only the unhealthy foods/food groups. Assessing the limiting and enhancing scores independently is expected to increase the ability43 to determine the specific areas that (food system) research and policymakers need to address to improve diets through food system innovations.
Use minimum/maximum cutoff points or a range for amounts consumed. Because the amount of a food determines whether it will provide a protective or harmful effect on the human body, the scoring of a food or food group should be based on scientifically proven cutoff points and standards (based on grams, servings, or portion sizes). Scoring should be based on the type of component; adequacy, moderation, optimum, or ratio components as described in more detail in Looman et al.133 Cutoff points for the different components could be based on absolute or energy density (energy-adjusted) cutoff points. Absolute amounts of intake (both nutrient and food based) could differ among sex and age groups due to differences in energy intake, but when using an energy density approach, these differences in energy intake are taken into account. However, such energy density approaches have not been applied to indices applicable in LMICs; thus further research on this topic in the LMIC setting is necessary.
Give the same weight to the different components in the total scoring and use a dichotomous scoring system. Unless research indicates a certain food or food group is of higher importance, give all components the same weight in the total scoring. The simplest and recommended scoring system is based on adherence to the guidelines regarding the amounts consumed (yes or no, minimum amount is reached or the maximum amount is not exceeded) using a dichotomous scoring of the individual component. No consensus exists about the best scoring system to use for a diet quality index.
Diet quality indices should be evaluated before widely used. Proper evaluation of the developed diet quality index is paramount. It is advised to evaluate the index in numerous ways, including the assessment of its reproducibility, reliability (internal consistency), relative validity, and its construct validity. Additionally a sensitivity/specificity analysis an evaluation of the index by associating it with the health outcome(s) of interest should be completed.
Table 5.
Characteristics of the different diet quality indices applicable in low- and middle-income countries according to the recommendations in Box 1
| Index; Reference | Purpose | Components | Diet quality dimensionsa | Healthy and unhealthy score | Cutoff pointsb | Scoring system | Evaluationc |
|---|---|---|---|---|---|---|---|
| MDD-W; FAO and FHI 360 (2016)42 | Women, nutritional needs | Foods and/or food groups | Variety | No | No | Dichotomous, equal weighing | Not described in this publication, but it is based on the findings from the FGI11 research and further elaborated in Martin-Prével et al46 |
| FGI; Arimond et al (2010)11 | Women, nutritional needs | Food groups | Variety and nutrient adequacy | No | Yes | Dichotomous, equal weighing | Construct validity, se/sp analysis, nutrient adequacy |
| Healthy, unhealthy or combined score; Imamura et al (2015)43 | Adults, nCDs | Foods, food groups, and nutrients | Variety and moderation | Yes | No | Quintiles, equal weighing | Construct validity |
| Indicators for infant and young child feeding; WHO (2008)45 | Infants and young child, child survival | Foods, food groups, and behaviors | Variety | No | No | Dichotomous, equal weighing | Not described in this publication, but for evaluation, see, for example, Jones et al22 |
| ICFI; Bork et al (2012)47 | Infants and toddlers, child survival | Foods, food groups, and behaviors | Variety | No | No | Dichotomous, equal weighing | Construct validity, reliability, height-for-age, and weight |
| CHEI; Yuan et al (2017)48 | Children, adolescents, adults, NCDs and nutritional needs | Foods and/or food groups | Variety and moderation | Yes | Yes | Continuous, weighing factor | Construct validity |
| CCDI; Cheng et al (2016)49 | Children and adolescents, NCDs and nutritional needs | Foods, food groups, nutrients, and behaviors | Variety, moderation, and nutrient adequacy | No | Yes | Continuous, equal weighing | Construct validity, nutrient adequacy |
| CFPS; Xu et al (2015)50 | Adults, NCDs and nutritional needs | Foods and/or food groups | Variety and moderation | No | Yes | Dichotomous, equal weighing | Construct validity |
| BDI; Hardiansyah et al (2015)51 | Children, NCDs and nutritional needs | Foods and/or food groups | Variety, moderation, and nutrient adequacy | Yes | Yes | Continuous, equal weighing | Nutrient adequacy |
| AMQI; Chiplonkar and Rama (2010)52 | Adolescents, NCDs and nutritional needs | Foods and/or food groups | Variety, moderation, and nutrient adequacy | No | Yes | Continuous, equal weighing | Construct validity, nutrient adequacy |
| THEI; Taechangam et al (2008)53 | Adults, NCDs and nutritional needs | Foods, food groups, and nutrients | Variety and moderation | No | Yes | Continuous, equal weighing | Construct validity |
| ALES School Child Diet Index; Molina et al (2010) 54 | Children, not mentioned | Foods, food groups, and behaviors | Variety and moderation | No | No | Dichotomous, Equal weighing | Construct validity |
| DQI-a; Jaime et al (2010)55 | Adults, NCDs and nutritional needs | Foods, food groups, and nutrients | Variety and moderation | No | Yes | Continuous, equal weighing | Construct validity, se/sp analysis |
| DDS; Enneman et al (2009)56 | Infants, child survival | Foods and/or food groups | Variety | No | No | Dichotomous, equal weighing | Reproducibility, construct validity |
| DDS; Enneman et al (2009)56 | Infants, child survival | Foods and/or food groups | Variety and moderation | No | No | Dichotomous, equal weighing | Reproducibility, construct validity |
| DDS; Enneman et al (2009)56 | Infants, child survival | Foods and/or food groups | Variety and moderation | No | No | Dichotomous, equal weighing | Reproducibility, construct validity |
| ICDMx; Macedo-Ojeda et al (2016)57 | Adults, NCDs and nutritional needs | Foods, food groups, and nutrients | Variety and moderation | No | Yes | Continuous, equal weighing | Reproducibility, relative validity |
| IYCF; Monterrosa et al (2015)58 | Infants, child survival | Foods, food groups, and behavior | Variety and moderation | No | No | Dichotomous, equal weighing | Prepregnancy BMI |
Abbreviations: ALES, Indice de Alimentacao do Escolar; AMQI, Adolescent Micronutrient Quality Index; BDI, Balanced Diet Index; BMI, body mass index; CCDI, Chinese Children Dietary Index; CFPS, Chinese Food Pagoda Score; CHEI, Chinese Healthy Eating Index; DDS, Dietary Diversity Score; DQI-a, Diet Quality Index–Adjusted; FGI, Food Group Diversity Indicators; ICDMx, Mexican Diet Quality Index; ICFI, Infant and Young Child Feeding Index; IYCF, Infant and Young Child Feeding Index; MDD-W, Minimum Dietary Diversity for Women; NCD, noncommunicable disease; se/sp analysis, sensitivity/specificity analysis; THEI, Healthy Eating Index for Thais; WHO, World Health Organization of the United Nations.
Nutrient adequacy refers to the provision of levels of energy and macro- and micronutrients appropriate to age, sex, disease status, and physical activity for a healthy life. Variety refers to the consumption of a variety of desirable foods or food groups. Moderation refers to the avoidance or limited consumption of foods, food groups, and nutrients that can be unhealthy if consumed in excess.
Minimum/maximum cutoff or range for the individual components.
Some diet quality indices are more extensively evaluated and described in additional publications; however, our review search was not specifically set up for such validation studies, and thus articles describing such validation studies are not included in our review.
Construct validity was by far the most described evaluation strategy (n = 13 indices), where, apart from nutrient adequacy, as described for 4 indices,11,49,51,52 height-for-age and weight47 and pre-pregnancy body mass index58 were evaluated outcomes. Only 2 country-specific indices include a healthy and unhealthy score and use cutoff points to score the food/food group components of the indices; one is the CHEI48 for children, adolescents, and adults in China, and the other is the Balanced Diet Index (BDI)51 for children in Indonesia. It is not mentioned whether the CHEI also captures the nutrition adequacy dimension of diet quality, and the article describing the development of the BDI does not describe an extensive evaluation, although those assessments could be planned for later for both indices.
Developing a diet quality index is complex, and issues regarding the construction of such an index are not yet solved (eg, what scoring system to use and which individual components to include in the index at what aggregation level). Reporting errors originating from the dietary intake assessment tools used are expected,126,127 which in turn will affect the outcome of the diet quality index. Furthermore, our recommendation of separating the healthy and unhealthy components into different scores will need further research; it seems promising given that Imamura et al43 showed a diluting effect when combining both healthy and unhealthy components into 1 score. Some of the reviewed diet quality indices already include separate scores for the healthy and unhealthy components.43,48,51,59,100,101,108 Separating the scores will create a small additional analytical burden, but it could be of use to policymakers to understand both positive and negative trends in intake. However, the message to policymakers could become more complicated, but, given the additional information on where to focus, it seems worthwhile to explore including healthy and unhealthy components in separate scores. Indices that underwent a thorough evaluation and have been validated against outcomes such as disease or nutrient adequacy lend more confidence in their results.
CONCLUSION
Of the 81 indices described, only 14 LMIC country-specific and 4 global indices have been identified to be potentially eligible for use in LMIC food system research. However, further analysis revealed that none of the 18 indices adhered to the 7 suggested recommendations: 16 LMIC-applicable indices did not capture all 3 dimensions of diet quality (adequacy, diversity and moderation), included nutrients instead of foods and/or food groups only, did not include a minimum/maximum cutoff for the individual components in the score, or did not calculate the healthy and unhealthy components as 2 separate scores. The 2 other indices developed were promising but unfortunately specific to a country. Furthermore, special attention should be given to solid validation of the index through examining the relationship with nutrient intakes, assessing reproducibility and reliability, analyzing sensitivity/specificity, assessing the comparability of the index between dietary assessment methods, and assessing the association with the intended diet-related health outcome(s).
A diet quality index that adheres to the suggested recommendations and is applicable in food system research in LMICs could take a global or a country-based perspective. One globally applicable diet quality index would allow for comparison of the diet quality of various countries, which is often an important prerequisite of such a metric in food system research. Furthermore country-specific indices based on native food–based dietary guidelines are tailored to a country’s specific disease profile and food habits and are therefore important indicators for within-country comparison.
In conclusion, there is an urgent need for the development of both country-specific food-based dietary guideline–based indices and a global diet quality index, all of which must undergo extensive evaluation.
Acknowledgments
The authors thank Marianne Renkema for her help with setting up the search strategy for references. The authors also thank Dr Marrit van den Berg, Dr Rosaline Remans, Dr Anouk Geelen, Dr Marga Ocké, and Dr Trudy Wijnhoven for critically reviewing the manuscript.
Author contributions. The search strategy was developed and conducted by L.T. and I.D.B. Screening of the articles and data extraction were done by L.T. and I.D.B. All authors had a substantial role in writing and reviewing the article. All authors have read and approved the final manuscript.
Funding. This research is supported by a grant from the International Food Policy Research Institute (IFPRI), Agriculture for Nutrition and Health program. The funder did not have any influence on the study design, data collection and analysis, manuscript preparation and revision, and publication decisions.
Declaration of interest. The authors have no relevant interests to declare.
References
- 1. Food and Agricultural Organization of the United Nations (FAO). Rome Declaration on Nutrition. Paper presented at International Conference on Nutrition, Rome, 2014. http://www.fao.org/resources/infographics/infographics-details/en/c/266118. Accessed August 2016.
- 2. McDermott J, Johnson N, Kadiyala S, et al. Agricultural research for nutrition outcomes— rethinking the agenda. Food Sec. 2015;7:593–607. [Google Scholar]
- 3. International Food Policy Research Institute (IFPRI). Global Nutrition Report 2016. From Promise to Impact: Ending Malnutrition by 2030. Washington DC: IFPRI; 2016.
- 4. GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1345–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Food and Agriculture Organization of the United Nations (FAO), World Health Organization (WHO). Second International Conference on Nutrition—Conference Outcome Document: Rome Declaration on Nutrition. 2014. http://www.fao.org/3/a-ml542e.pdf. Accessed August 2016.
- 6.High Level Panel of Experts (HLPE). Nutrition and Food Systems. A Report of the High Level Panel of Experts on Food Security and Nutrition of the Committee on World Food Security, Rome. 2017. http://www.fao.org/fileadmin/user_upload/hlpe/hlpe_documents/HLPE_Reports/HLPE-Report-12_EN.pdf.
- 7. Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–451. [DOI] [PubMed] [Google Scholar]
- 8. Alkerwi A. Diet quality concept. Nutrition. 2014;30:613–618. [DOI] [PubMed] [Google Scholar]
- 9. Global Panel on Agriculture and Food Systems for Nutrition. Food Systems and Diets: Facing the Challenges of the 21st Century. London, 2016. https://www.glopan.org/sites/default/files/Downloads/Foresight%20Report.pdf. [Google Scholar]
- 10. Herforth A, Frongillo EA, Sassi F, et al. Toward an integrated approach to nutritional quality, environmental sustainability, and economic viability: research and measurement gaps. (A global research agenda for nutrition science.). Ann N Y Acad Sci. 2014;1332:1–21. [DOI] [PubMed] [Google Scholar]
- 11. Arimond M, Wiesmann D, Becquey E, et al. Simple food group diversity indicators predict micronutrient adequacy of women's diets in 5 diverse, resource-poor settings. J Nutr. 2010;140 (suppl):2059S–2069S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hawkes C, Popkin BM.. Can the sustainable development goals reduce the burden of nutrition-related non-communicable diseases without truly addressing major food system reforms? BMC Med. 2015;13:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Popkin BM. Nutrition transition and the global diabetes epidemic. Curr Diabetes Rep. 2015;15:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Anand SS, Hawkes C, De Souza RJ, et al. Food consumption and its impact on cardiovascular disease: importance of solutions focused on the globalized food system a report from the workshop convened by the World Heart Federation. J Am Coll Cardiol. 2015;66:1590–1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Roman-Vinas B, Ribas Barba L, Ngo J, et al. Validity of dietary patterns to assess nutrient intake adequacy. BJN. 2009;101(suppl 2):S12–S20. [DOI] [PubMed] [Google Scholar]
- 16. Ruel MT. Operationalizing dietary diversity: a review of measurement issues and research priorities. J Nutr. 2003;133(suppl 2): 3911S–3926S. [DOI] [PubMed] [Google Scholar]
- 17. Wirt A, Collins CE.. Diet quality—what is it and does it matter? Public Health Nutr. 2009;12:2473–2492. [DOI] [PubMed] [Google Scholar]
- 18. Guenther PM, Reedy J, Krebs-Smith SM, et al. Evaluation of the Healthy Eating Index–2005. J Am Diet Assoc. 2008;108:1854–1864. [DOI] [PubMed] [Google Scholar]
- 19. Grimstvedt ME, Woolf K, Milliron BJ, et al. Lower Healthy Eating Index–2005 dietary quality scores in older women with rheumatoid arthritis v. healthy controls. Public Health Nutr. 2010;13:1170–1177. [DOI] [PubMed] [Google Scholar]
- 20. Guenther PM, Kirkpatrick SI, Reedy J, et al. The Healthy Eating Index–2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr. 2014;144:399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Anic GM, Park Y, Subar AF, et al. Index-based dietary patterns and risk of lung cancer in the NIH-AARP diet and health study. Eur J Clin Nutr. 2016;70:123–129. [DOI] [PubMed] [Google Scholar]
- 22. Jones AD, Ickes SB, Smith LE, et al. World Health Organization infant and young child feeding indicators and their associations with child anthropometry: a synthesis of recent findings. Matern Child Nutr. 2014;10:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gorgulho BM, Pot GK, Sarti FM, et al. Indices for the assessment of nutritional quality of meals: a systematic review. Br J Nutr. 2016;115:2017–2024. [DOI] [PubMed] [Google Scholar]
- 24. Gil A, Martinez de Victoria E, Olza J.. Indicators for the evaluation of diet quality. Nutr Hosp. 2015;31(suppl 3):128–144. [DOI] [PubMed] [Google Scholar]
- 25. Fern EB, Watzke H, Barclay DV, et al. The nutrient balance concept: a new quality metric for composite meals and diets. PLoS One. 2015;10:e0130491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fulgoni Iii VL, Keast DR, Drewnowski A.. Development and validation of the nutrient-rich foods index: a tool to measure nutritional quality of foods. J Nutr. 2009;139:1549–1554. [DOI] [PubMed] [Google Scholar]
- 27. Julia C, Touvier M, Mejean C, et al. Development and validation of an individual dietary index based on the British Food Standard Agency nutrient profiling system in a French context. J Nutr. 2014;144:2009–2017. [DOI] [PubMed] [Google Scholar]
- 28. Katz DL, Njike VY, Faridi Z, et al. The stratification of foods on the basis of overall nutritional quality: the overall nutritional quality index. Am J Health Promot. 2009;24:133–143. [DOI] [PubMed] [Google Scholar]
- 29. Hernández Ruiz A, García-Villanova B, Guerra Hernández EJ, et al. Description of indexes based on the adherence to the Mediterranean dietary pattern: a review. Nutricion Hospitalaria. 2015;32:1872–1884. [DOI] [PubMed] [Google Scholar]
- 30. Drewnowski A. Concept of a nutritious food: toward a nutrient density score. Am J Clin Nutr. 2005;82:721–732. [DOI] [PubMed] [Google Scholar]
- 31. Waijers PM, Feskens EJ, Ocke MC.. A critical review of predefined diet quality scores. Br J Nutr. 2007;97:219–231. [DOI] [PubMed] [Google Scholar]
- 32. Marshall S, Burrows T, Collins CE.. Systematic review of diet quality indices and their associations with health-related outcomes in children and adolescents. J Hum Nutr Diet. 2014;27:577–598. [DOI] [PubMed] [Google Scholar]
- 33. Lazarou C, Newby PK.. Use of dietary indexes among children in developed countries. Adv Nutr. 2011;2:295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kourlaba G, Panagiotakos DB.. Dietary quality indices and human health: a review. Maturitas. 2009;62:1–8. [DOI] [PubMed] [Google Scholar]
- 35. Kant AK. Indexes of overall diet quality: a review. J Am Diet Assoc. 1996;96:785–791. [DOI] [PubMed] [Google Scholar]
- 36. Fransen HP, Ocke MC.. Indices of diet quality. Curr Opin Clin Nutr Metab Care. 2008;11:559–565. [DOI] [PubMed] [Google Scholar]
- 37. Drewnowski A, Fulgoni III V.. Nutrient profiling of foods: creating a nutrient-rich food index. Nutr Rev. 2008;66:23–39. [DOI] [PubMed] [Google Scholar]
- 38. de Carvalho KMB, Dutra ES, Pizato N, Gruezo ND, Ito MK.. Diet quality assessment indexes. Rev Nutr. 2014;27:605–617. [Google Scholar]
- 39. Arvaniti F, Panagiotakos DB.. Healthy indexes in public health practice and research: a review. Crit Rev Food Sci Nutr. 2008;48:317–327. [DOI] [PubMed] [Google Scholar]
- 40. Asghari G, Mirmiran P, Yuzbashian E, et al. A systematic review of diet quality indices in relation to obesity. Br J Nutr. 2017;117:1055–1065. [DOI] [PubMed] [Google Scholar]
- 41. Morais DC, Moraes LFS, Silva DCG d, Pinto CA, et al. Methodological aspects of dietary quality assessment in Brazil: systematic review. Ciencia e Saude Coletiva. 2017;22:2671–2680. [DOI] [PubMed] [Google Scholar]
- 42. Food and Agricultural Organization of the United Nations (FAO), FHI 360. Minimum Dietary Diversity for Women: A Guide for Measurement. Rome: FAO; 2016:82. [Google Scholar]
- 43. Imamura F, Micha R, Khatibzadeh S, et al. Dietary quality among men and women in 187 countries in 1990 and 2010: a systematic assessment. Lancet Glob Health. 2015;3:e132–e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Verger EO, Mariotti F, Holmes BA, et al. Evaluation of a diet quality index based on the probability of adequate nutrient intake (PANDiet) using national French and US dietary surveys. PLoS One. 2012;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. World Health Organization (WHO). Indicators for Assessing Infant and Young Child Feeding Practices, Part 1: Definitions. 2008. https://www.who.int/maternal_child_adolescent/documents/9789241596664/en/. Accessed August 2016.
- 46. Martin-Prével Y, Allemand P, Wiesmann D, et al. Moving forward on choosing a standard operational indicator of women’s dietary diversity. Rome: Food and Agricultural Organization of the United Nations (FAO); 2015. [Google Scholar]
- 47. Bork K, Cames C, Barigou S, et al. A summary index of feeding practices is positively associated with height-for-age, but only marginally with linear growth, in rural senegalese infants and toddlers. J Nutr. 2012;142:1116–1122. [DOI] [PubMed] [Google Scholar]
- 48. Yuan YQ, Li F, Dong RH, et al. The development of a Chinese healthy eating index and its application in the general population. Nutrients. 2017;9:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Cheng G, Duan R, Kranz S, et al. Development of a dietary index to assess overall diet quality for Chinese school-aged children: the Chinese Children Dietary Index. J Acad Nutr Diet. 2016;116:608–617. [DOI] [PubMed] [Google Scholar]
- 50. Xu X, Hall J, Byles J, et al. Do older Chinese people’s diets meet the Chinese Food Pagoda guidelines? Results from the China Health and Nutrition Survey 2009. Public Health Nutr. 2015;18:3020–3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hardiansyah A, Sukandar D.. Alternative indices for the assessment of nutritional quality of balanced diet of Indonesian children 4–6 years old. Pakistan J Nutr. 2015;14:716–720. [Google Scholar]
- 52. Chiplonkar SA, Rama T.. Development of a diet quality index with special reference to micronutrient adequacy for adolescent girls consuming a lacto-vegetarian diet. J Am Diet Assoc. 2010;110:926–931. [DOI] [PubMed] [Google Scholar]
- 53. Taechangam S, Pinitchun U, Pachotikarn C.. Development of nutrition education tool: healthy eating index in Thailand. Asia Pac J Clin Nutr. 2008;17(suppl 1):365–367. [PubMed] [Google Scholar]
- 54. Molina Mdel C, Lopez PM, Faria CP, et al. Socioeconomic predictors of child diet quality. Rev Saude Publica. 2010;44:785–732. [DOI] [PubMed] [Google Scholar]
- 55. Jaime PC, Bandoni DH, Duran AC, et al. Diet quality index adjusted for energy requirements in adults. Cad Saude Publica. 2010;26:2121–2128. [DOI] [PubMed] [Google Scholar]
- 56. Enneman A, Hernández L, Campos R, et al. Dietary characteristics of complementary foods offered to Guatemalan infants vary between urban and rural settings. Nutr Res. 2009;29:470–479. [DOI] [PubMed] [Google Scholar]
- 57. Macedo-Ojeda G, Márquez-Sandoval F, Fernández-Ballart J, et al. The reproducibility and relative validity of a Mexican diet quality index (ICDMx) for the assessment of the habitual diet of adults. Nutrients. 2016;8:516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Monterrosa EC, Frongillo EA, Neufeld LM, et al. Maternal pre-pregnancy body mass index is not associated with infant and young child feeding in low-income Mexican children 1–24 months old. Matern Child Nutr. 2015;11:215–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Anderson SE, Kaye G, Andridge R, et al. Interrelationships of more healthful and less healthful aspects of diet quality in a low-income community sample of preschool-aged children. Matern Child Healt J. 2015;19:2663–2672. [DOI] [PubMed] [Google Scholar]
- 60. Biltoft-Jensen A, Fagt S, Groth MV, et al. The intake of saturated fat and dietary fibre: a possible indicator of diet quality. Br J Nutr. 2008;100:624–632. [DOI] [PubMed] [Google Scholar]
- 61. Cleghorn CL, Harrison RA, Ransley JK, et al. Can a dietary quality score derived from a short-form FFQ assess dietary quality in UK adult population surveys? Public Health Nutr. 2016;19:2915–2923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Crombie IK, Kiezebrink K, Irvine L, et al. What maternal factors influence the diet of 2-year-old children living in deprived areas? A cross-sectional survey. Public Health Nutr. 2009;12:1254–1260. [DOI] [PubMed] [Google Scholar]
- 63. Drake I, Gullberg B, Ericson U, et al. Development of a diet quality index assessing adherence to the Swedish nutrition recommendations and dietary guidelines in the Malmö Diet and Cancer cohort. Public Health Nutr. 2011;14:835–845. [DOI] [PubMed] [Google Scholar]
- 64. Estaquio C, Castetbon K, Kesse-Guyot E, et al. The French National Nutrition and Health Program score is associated with nutritional status and risk of major chronic diseases. J Nutr. 2008;138:946–953. [DOI] [PubMed] [Google Scholar]
- 65. Falciglia GA, Horner SL, Liang J, et al. Assessing dietary variety in children: development and validation of a predictive equation. J Am Diet Assoc. 2009;109:641–647. [DOI] [PubMed] [Google Scholar]
- 66. Freisling H, Elmadfa I, Schuh W, et al. Development and validation of a food frequency index using nutritional biomarkers in a sample of middle-aged and older adults. J Hum Nutr Diet. 2009;22:29–39. [DOI] [PubMed] [Google Scholar]
- 67. Fung TT, Chiuve SE, McCullough ML, et al. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–720. [DOI] [PubMed] [Google Scholar]
- 68. Gasser CE, Kerr JA, Mensah FK, et al. Stability and change in dietary scores and patterns across six waves of the Longitudinal Study of Australian Children. Br J Nutr. 2017;117:1137–1150. [DOI] [PubMed] [Google Scholar]
- 69. Golley RK, Hendrie GA, McNaughton SA.. Scores on the dietary guideline index for children and adolescents are associated with nutrient intake and socio-economic position but not adiposity. J Nutr. 2011;141:1340–1347. [DOI] [PubMed] [Google Scholar]
- 70. Golley RK, Smithers LG, Mittinty MN, et al. An index measuring adherence to complementary feeding guidelines has convergent validity as a measure of infant diet quality. J Nutr. 2012;142:901–908. [DOI] [PubMed] [Google Scholar]
- 71. Guenther PM, Casavale KO, Reedy J, et al. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet. 2013;113:569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Guenther PM, Reedy J, Krebs-Smith SM.. Development of the Healthy Eating Index–2005. J Am Diet Assoc. 2008;108:1896–1901. [DOI] [PubMed] [Google Scholar]
- 73. Hillesund ER, Bere E, Haugen M, et al. Development of a New Nordic Diet score and its association with gestational weight gain and fetal growth–a study performed in the Norwegian Mother and Child Cohort Study (MoBa.). Public Health Nutr. 2014;17:1909–1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Huybrechts I, Vereecken C, Bacquer D, et al. Reproducibility and validity of a diet quality index for children assessed using a FFQ. Br J Nutr. 2010;104:135–144. [DOI] [PubMed] [Google Scholar]
- 75. Jessri M, Ng AP, L’Abbé MR.. Adapting the Healthy Eating Index 2010 for the Canadian population: evidence from the Canadian National Nutrition Survey. Nutrients. 2017;9:910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Jonge E, Kiefte-de Jong JC, Groot L, et al. Development of a food group–based diet score and its association with bone mineral density in the elderly: the Rotterdam study. Nutrients. 2015;7:6974–6990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Kanerva N, Kaartinen NE, Schwab U, et al. The Baltic Sea Diet Score: a tool for assessing healthy eating in Nordic countries. Public Health Nutr. 2014;17:1697–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Kleiser C, Mensink GB, Scheidt-Nave C, et al. HuSKY: a healthy nutrition score based on food intake of children and adolescents in Germany. Br J Nutr. 2009;102:610–618. [DOI] [PubMed] [Google Scholar]
- 79. Kosti RI, Panagiotakos DB, Mariolis A, et al. The Diet-Lifestyle Index evaluating the quality of eating and lifestyle behaviours in relation to the prevalence of overweight/obesity in adolescents. Int J Food Sci Nutr. 2009;60(suppl 3):34–47. [DOI] [PubMed] [Google Scholar]
- 80. Kourlaba G, Polychronopoulos E, Zampelas A, et al. Development of a diet index for older adults and its relation to cardiovascular disease risk factors: the Elderly Dietary Index. J Am Diet Assoc. 2009;109:1022–1030. [DOI] [PubMed] [Google Scholar]
- 81. Kuriyama N, Murakami K, Livingstone MBE, et al. Development of a food-based diet quality score for Japanese: associations of the score with nutrient intakes in young, middle-aged and older Japanese women. J Nutr Sci. 2016;5:e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Lazarou C, Panagiotakos DB, Matalas AL.. Foods E-KINDEX: a dietary index associated with reduced blood pressure levels among young children: the CYKIDS study. J Am Diet Assoc. 2009;109:1070–1075. [DOI] [PubMed] [Google Scholar]
- 83. Lee L, Geelen A, Huysduynen E, et al. The Dutch Healthy Diet index (DHD-index): an instrument to measure adherence to the Dutch Guidelines for a Healthy Diet. Nutr J. 2012;11:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Lee M, Lai C, Yang F, et al. A global overall dietary index: oDI-R revised to emphasize quality over quantity. Asia Pac J Clin Nutr. 2008;17(suppl 1):82–86. [PubMed] [Google Scholar]
- 85. Leppala J, Lagstrom H, Kaljonen A, et al. Construction and evaluation of a self-contained index for assessment of diet quality. Scand J Public Health. 2010;38:794–802. [DOI] [PubMed] [Google Scholar]
- 86. Li J, O'Sullivan T, Johnson S, et al. Maternal work hours in early to middle childhood link to later adolescent diet quality. Public Health Nutr. 2012;15:1861–1870. [DOI] [PubMed] [Google Scholar]
- 87. Lipsky LM, Cheon K, Nansel TR, et al. Candidate measures of whole plant food intake are related to biomarkers of nutrition and health in the US population (National Health and Nutrition Examination Survey 1999–2002. ). Nutr Res 2012;32:251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Looman M, Feskens EJM, De Rijk M, et al. Development and evaluation of the Dutch Healthy Diet Index 2015. Public Health Nutr. 2017;20:2289–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Manios Y, Kourlaba G, Grammatikaki E, et al. Development of a diet-lifestyle quality index for young children and its relation to obesity: the Preschoolers Diet-Lifestyle Index. Public Health Nutr. 2010;13:2000–2009. [DOI] [PubMed] [Google Scholar]
- 90. Manios Y, Kourlaba G, Grammatikaki E, et al. Development of a lifestyle-diet quality index for primary school children and its relation to insulin resistance: the Healthy Lifestyle-Diet Index. Eur J Clin Nutr. 2010;64:1399–1406. [DOI] [PubMed] [Google Scholar]
- 91. Manios Y, Moschonis G, Papandreou C, et al. Revised Healthy Lifestyle-Diet Index and associations with obesity and iron deficiency in schoolchildren: the Healthy Growth Study. J Hum Nutr Diet. 2015;28:50–58. [DOI] [PubMed] [Google Scholar]
- 92. Mariscal-Arcas M, Rivas A, Monteagudo C, et al. Proposal of a Mediterranean diet index for pregnant women. Br J Nutr. 2009;102:744–749. [DOI] [PubMed] [Google Scholar]
- 93. Marshall S, Watson J, Burrows T, et al. The development and evaluation of the Australian child and adolescent recommended food score: a cross-sectional study. Nutr J. 2012;11:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. McNaughton SA, Ball K, Crawford D, et al. An index of diet and eating patterns is a valid measure of diet quality in an Australian population. J Nutr. 2008;138:86–93. [DOI] [PubMed] [Google Scholar]
- 95. Meinilä J, Valkama A, Koivusalo SB, et al. Healthy Food Intake Index (HFII)—validity and reproducibility in a gestational-diabetes-risk population. BMC Public Health. 2016;16:680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Nishimura T, Murakami K, Livingstone MBE, et al. Adherence to the food-based Japanese dietary guidelines in relation to metabolic risk factors in young Japanese women. Br J Nutr. 2015;114:645–653. [DOI] [PubMed] [Google Scholar]
- 97. Oliveira A, Jones L, de Lauzon-Guillain B, et al. Early problematic eating behaviours are associated with lower fruit and vegetable intake and less dietary variety at 4–5 years of age. A prospective analysis of three European birth cohorts. Br J Nutr. 2015;114:763–771. [DOI] [PubMed] [Google Scholar]
- 98. Perry CP, Keane E, Layte R, et al. The use of a dietary quality score as a predictor of childhood overweight and obesity. BMC Public Health. 2015;15:581.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Pot GK, Richards M, Prynne CJ, et al. Development of the Eating Choices Index (ECI): a four-item index to measure healthiness of diet. Public Health Nutr. 2014;17:2660–2666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Rodríguez-Martin C, Alonso-Domínguez R, Patino-Alonso MC, et al. The EVIDENT diet quality index is associated with cardiovascular risk and arterial stiffness in adults. BMC Public Health. 2017;17:305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Roy R, Hebden L, Rangan A, et al. The development, application, and validation of a Healthy Eating Index for Australian Adults (HEIFA-2013). Nutrition. 2016;32:432–440. [DOI] [PubMed] [Google Scholar]
- 102. Roytio H, Jaakkola J, Hoppu U, et al. Development and evaluation of a stand-alone index for the assessment of small children's diet quality. Public Health Nutr. 2015;18:1941–1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Rumawas ME, Dwyer JT, McKeown NM, et al. The development of the Mediterranean-Style Dietary Pattern Score and its application to the American diet in the Framingham Offspring Cohort. J Nutr. 2009;139:1150–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Scott JA, Chih T, Oddy WH.. Food variety at 2 years of age is related to duration of breastfeeding. Nutrients. 2012;4:1464–1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Sharafi M, Peracchio H, Scarmo S, et al. Preschool-Adapted Liking Survey (PALS): a brief and valid method to assess dietary quality of preschoolers. Child Obes. 2015;11:530–540. [DOI] [PubMed] [Google Scholar]
- 106. Spence AC, McNaughton SA, Lioret S, et al. A health promotion intervention can affect diet quality in early childhood. J Nutr. 2013;143:1672–1678. [DOI] [PubMed] [Google Scholar]
- 107. Taylor A, Wilson F, Hendrie GA, et al. Feasibility of a Healthy Trolley Index to assess dietary quality of the household food supply. Br J Nutr. 2015;114:2129–2137. [DOI] [PubMed] [Google Scholar]
- 108. Thorpe MG, Milte CM, Crawford D, et al. A revised Australian Dietary Guideline Index and its association with key sociodemographic factors, health behaviors and body mass index in peri-retirement aged adults. Nutrients. 2016;8:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Vadiveloo M, Dixon LB, Mijanovich T, et al. Development and evaluation of the US Healthy Food Diversity index. Br J Nutr. 2014;112:1562–1574. [DOI] [PubMed] [Google Scholar]
- 110. Vandevijvere S, Vriese S, Huybrechts I, et al. Overall and within-food group diversity are associated with dietary quality in Belgium. Public Health Nutr. 2010;13:1965–1973. [DOI] [PubMed] [Google Scholar]
- 111. Vereecken CA, Rossi S, Giacchi MV, et al. Comparison of a short food-frequency questionnaire and derived indices with a seven-day diet record in Belgian and Italian children. Int J Public Health. 2008;53:297–305. [DOI] [PubMed] [Google Scholar]
- 112. Verger EO, Eussen S, Holmes BA.. Evaluation of a nutrient-based diet quality index in UK young children and investigation into the diet quality of consumers of formula and infant foods. Public Health Nutr. 2015;19:1785–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Voortman T, Kiefte-de Jong JC, Geelen A, et al. The development of a diet quality score for preschool children and its validation and determinants in the Generation R Study. J Nutr. 2015;145:306–314. [DOI] [PubMed] [Google Scholar]
- 114. Wong J, Skidmore PML, Williams SM, et al. Healthy dietary habits score as an indicator of diet quality in New Zealand adolescents. J Nutr. 2014;144:937–942. [DOI] [PubMed] [Google Scholar]
- 115. Wong JE, Haszard JJ, Howe AS, et al. Development of a healthy dietary habits index for New Zealand adults. Nutrients. 2017;9:454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Wong JE, Parnell WR, Howe AS, et al. Development and validation of a food-based diet quality index for New Zealand adolescents. BMC Public Health. 2013;13:562.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Woodruff SJ, Hanning RM.. Development and implications of a revised Canadian Healthy Eating Index (HEIC-2009). Public Health Nutr. 2010;13:820–825. [DOI] [PubMed] [Google Scholar]
- 118. Zarrin R, Ibiebele TI, Marks GC.. Development and validity assessment of a diet quality index for Australians. Asia Pac J Clin Nutr. 2013;22:177–187. [DOI] [PubMed] [Google Scholar]
- 119. Jankovic N, Geelen A, Streppel MT, et al. Adherence to a healthy diet according to the World Health Organization guidelines and all-cause mortality in elderly adults from Europe and the United States. Am J Epidemiol. 2014;180:978–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Kirkpatrick SI, Potischman N, Dodd KW, et al. The use of digital images in 24-hour recalls may lead to less misestimation of portion size compared with traditional interviewer-administered recalls. J Nutr. 2016;146:2567–2573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Kourlaba G, Panagiotakos D.. The number of index components affects the diagnostic accuracy of a diet quality index: the role of intracorrelation and intercorrelation structure of the components. Ann Epidemiol. 2009;19:692–700. [DOI] [PubMed] [Google Scholar]
- 122. Schroder H, Benitez Arciniega A, Soler C, et al. Validity of two short screeners for diet quality in time-limited settings. Public Health Nutr. 2012;15:618–626. [DOI] [PubMed] [Google Scholar]
- 123. Van Lee L, Feskens EJM, Meijboom S, et al. Evaluation of a screener to assess diet quality in the Netherlands. Br J Nutr. 2015;115:517–526. [DOI] [PubMed] [Google Scholar]
- 124. Adjoian TK, Firestone MJ, Eisenhower D, et al. Validation of self-rated overall diet quality by Healthy Eating Index-2010 score among New York City adults, 2013. Prevent Med Rep. 2016;3:127–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Food and Agriculture Organization of the United Nations (FAO). Summary of Proceedings. Measurement and Assessment of Food Deprivation and Undernutrition. 2002. http://www.fao.org/3/1-y4250e.pdf. Accessed August 2016.
- 126. Kipnis V, Subar AF, Midthune D, et al. Structure of dietary measurement error: results of the OPEN biomarker study. Am J Epidemiol. 2003;158:14–21. [DOI] [PubMed] [Google Scholar]
- 127. Prentice RL, Mossavar-Rahmani Y, Huang Y, et al. Evaluation and comparison of food records, recalls, and frequencies for energy and protein assessment by using recovery biomarkers. Am J Epidemiol. 2011;174:591–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Food and Agriculture Organization of the United Nations (FAO). About INFOODS. 2016. http://www.fao.org/infoods/infoods/en/. Accessed August 2016.
- 129. Roche ML, Creed-Kanashiro HM, Tuesta I, et al. Traditional food diversity predicts dietary quality for the Awajun in the Peruvian Amazon. Public Health Nutr. 2008;11:457–465. [DOI] [PubMed] [Google Scholar]
- 130. Moursi MM, Arimond M, Dewey KG, et al. Dietary diversity is a good predictor of the micronutrient density of the diet of 6- to 23-month-old children in Madagascar. J Nutr. 2008;138:2448–2453. [DOI] [PubMed] [Google Scholar]
- 131. Rathnayake KM, Madushani P, Silva K.. Use of dietary diversity score as a proxy indicator of nutrient adequacy of rural elderly people in Sri Lanka. BMC Res Notes. 2012;5:469.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Fujita M, Lo YJ, Baranski JR.. Dietary diversity score is a useful indicator of vitamin A status of adult women in northern Kenya. Am J Hum Biol. 2012;24:829–834. [DOI] [PubMed] [Google Scholar]
- 133. Varsha R, Arends DE, Brouwer ID.. Dietary diversity as an indicator of micronutrient adequacy of the diet of five to eight year old Indian rural children. Nutr Food Sci. 2010;40:466–476. [Google Scholar]
- 134. Vadiveloo M, Dixon LB, Parekh N.. Associations between dietary variety and measures of body adiposity: a systematic review of epidemiological studies. Br J Nutr. 2013;109:1557–1572. [DOI] [PubMed] [Google Scholar]