Abstract
Objective:
Impaired psychosocial functioning previously emerged as the only risk factor to predict future onset of each of the four DSM-5 eating disorders (Stice et al., 2017). The goal of this follow-up report was to refine understanding of this newly identified risk factor.
Method:
Combining data from women at risk for eating disorders because of body image concerns (N = 1,153, meanage =18.5 years, SD = 4.2), we investigated which subdomain(s) and individual item(s) of psychosocial functioning (friends, family, school, and work) at baseline predicted onset of any eating disorder, using Cox Regression (CRA) and Classification Tree Analysis (CTA).
Results:
Psychosocial impairment with friends, family, and at school, but not at work, significantly increased risk for disorder onset over 3-year follow-up in univariate models. A one-unit increase in each domain raw score was associated with a 107%, 22%, and 43% increased hazard of eating disorder onset, respectively. Multivariate CRA found friends functioning, with a 92% increased hazard of disorder onset, contributed the strongest unique effect. CTA suggested that loneliness was the most potent risk factor with a 3-fold increased onset risk (eating disorder incidence for high versus low scorers was 27% and 8%). Three friends functioning items and one school functioning item produced additional CTA branches.
Discussion:
Results refine understanding of the relation of psychosocial impairment to future onset of eating disorders, suggesting that peer functioning is the most critical. Data imply it would be useful to target young women with impaired psychosocial functioning in prevention programs.
Keywords: psychosocial functioning, friends, family, school, eating disorders, prevention, etiology
Eating disorders in young women are serious, disabling and costly mental illnesses (Agras, 2001; Simon, Schmidt, & Pilling, 2005) which can be chronic, show high rates of comorbidity (Allen, Byrne, Forbes, & Oddy, 2009; Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011), and result in increased suicide attempts ( Mandelli, Arminio, Atti, & De Ronchi, 2018; Pisetsky, Thornton, Lichtenstein, Pedersen, & Bulik, 2013) and mortality rates ( Fichter & Quadflieg, 2016). Given that 13% of women will experience a DSM-5 (American Psychiatric Association, 2013) eating disorder by young adulthood (Stice, Marti, & Rohde, 2013), effective prevention programs are needed (e.g., Melioli et al., 2016; Wilksch et al., 2017).
Psychosocial functioning has been defined as a person’s ability to successfully interact with their environment, which includes building and maintaining gratifying relationships with family members, partners, and peers and appropriately responding to societal demands at school, work and other social settings (Mehta, Mittal, & Swami, 2014). Though impaired psychosocial functioning has been found to be a consequence of eating disorders (Bohn et al., 2008; Lynch et al., 2010) persistent even after recovery (Herzog, Pepose, Norman, & Rigotti, 1985; Wentz, Gillberg, Anckarsater, Gillberg, & Rastam, 2009), to our knowledge only two studies have investigated impaired psychosocial functioning as a putative risk factor that predicts future eating disorder onset (Jacobi et al., 2011; Stice, Gau, Rohde, & Shaw, 2017). Both studies used a prospective design assessing psychosocial functioning by a global self-report measure (Weissman, Orvaschel, & Padian, 1980) precedent to eating disorder onset, according to the same risk factor terminology (Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001), and using diagnostic interviews to verify future onset of eating disorders.
Jacobi et al. (2011) followed a high-risk sample of female adolescents longitudinally and found no predictive effects of impaired psychosocial functioning on future onset of any eating disorder over 3-year follow up, potentially because their sample included only 236 participants. Stice et al. (2017) followed a larger sample of 1,272 women at high risk for eating pathology by virtue of self-reported body image concerns and tested whether baseline risk factors predicted future onset of subthreshold and threshold diagnoses (as operationalized in Stice et al. [2013]) of anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder (BED), and purging disorder (PD) over 3-year follow-up. Although other variables had higher hazard ratios in associations with specific eating disorders, impaired psychosocial functioning was the only risk factor among those examined to significantly predict future onset of all four eating disorder types at both subthreshold and threshold levels (Stice et al., 2017), which we label as a ‘transdiagnostic’ eating disorder risk factor.
Given that impaired psychosocial functioning was the only predictor of onset of each of the four types of eating disorders in this data set, we conducted an exploratory follow-up study to Stice et al. (2017) in a three step procedure. First, we examined the univariate effects of specific psychosocial functioning domains (friends, family, school and work) in predicting future onset of any eating disorder. Second, we tested the unique influence of each subdomain via multivariate analyses. Third, we subdivided the measure into its 17 individual items to explore, using classification tree analysis (CTA), which specific aspect(s) of functioning predicted future onset of any eating disorder. Thus, the primary aim of this exploratory analysis was to disaggregate the global measure of psychosocial functioning to examine which domain(s) and individual item(s) of psychosocial impairment showed the strongest relations to future onset of any eating disorder to advance knowledge of this general eating disorder risk factor.
Results from these analyses may suggest directions regarding how psychosocial impairment could best be integrated into etiological models for eating disorders. To date, models have tended to not conceptualize psychosocial impairment as relevant for the onset of eating disorders. Thus, the present exploratory analyses may advance etiologic theory. It has recently been proposed that adolescent girls who experience impaired psychosocial functioning might turn to pursuit of the culturally sanctioned thin beauty ideal to gain greater social acceptance, which increases risk for body dissatisfaction, dieting, and negative affect, which increase risk for emergence of unhealthy weight control behaviors and binge eating (Stice & Van Ryzin, in press). As theorized, psychosocial functioning typically emerges before pursuit of the thin beauty ideal, which typically emerges before body dissatisfaction, dieting, negative affect, and onset of eating disorders (Stice & Van Ryzin, in press). A better understanding of psychosocial functioning domains or even individual items could also potentially guide the development of new eating disorder prevention programs. As reported elsewhere (Melioli et al., 2016; Wilksch et al., 2017; Wilksch, O’Shea, & Wade, 2018 ), programs that reduce the onset of multiple eating disorders would be advantageous from a public health perspective, and could identify high-risk subgroups to target with selective prevention programs
Method
Participants
As in Stice et al. (2017), we merged data from three randomized controlled trials that collected diagnostic data and conducted an individual patient data (IPD) meta-analysis, which differs from standard meta-analysis. In standard meta-analysis, summary scores on a topic are extracted from each study; conversely, in IPD meta-analysis the original data from individual participants in each of the studies arecombined and re-analyzed. By increasing statistical power, IPD meta-analyses should improve the reliability of results (Thomas, Radji, & Benedetti, 2014). We combined data from one efficacy trial (Stice, Marti, Spoor, Presnell, & Shaw, 2008) and two effectiveness trials: Trial 2; (Stice, Marti, & Durant, 2011); Trial 3; (Stice, Rohde, Butryn, Shaw, & Marti, 2015) for the present study. Trial 1 participants (N = 481 from high schools or college, mean age = 17.0 [SD = 1.4]; 95% retention) were randomized to the Body Project prevention program, Healthy Weight prevention program, an expressive writing intervention, or assessment-only control. Trial 2 (N = 306 from high schools, mean age = 15.7 [SD = 1.1]; 84% retention) and Trial 3 (N = 485 from colleges, mean age = 21.6 [SD = 5.6]; 89% retention) participants were randomized to the Body Project or educational brochure control. The only inclusion criterion in all trials was that participants answer affirmatively to having body image concerns during a phone screen. Participants completed surveys and interviews at baseline and at 1-, 6-, 12-, 24-, and 36-month follow-up (the 6-month assessment was not conducted in Trial 3). The resulting 1,272 participants (mean age at study entry = 18.5, SD = 4.2) were composed of 5% African American, 10% Asian American/Pacific Islander, 67% White, 11% Hispanic, 2% Native American and 4% who specified as other or mixed racial heritage. Parental education was 11% high school graduate or less, 18% some college, 37% college graduate, and 33% advanced graduate/professional degree.
Measures
Eating pathology.
The semi-structured Eating Disorder Diagnostic Interview (EDDI; Stice et al., 2013) assessed eating disorder symptoms over the past 3 months at baseline and since the last interview at follow-ups on a month-by-month basis, allowing us to examine variables that predict future onset of any DSM-5 eating disorder over 3-year follow-up. DSM-5 criteria for eating disorders were used, as operationalized in Stice et al. (2013), which included threshold and subthreshold criteria for AN, BN, BED, and PD. EDDI eating disorder diagnoses have shown 1-week test-retest reliability (κ = .79), inter-rater agreement (κ = .75), convergent validity, and sensitivity to detecting prevention program effects (Stice et al., 2008).
Psychosocial impairment.
Impairment in the friends, family, school and work domains was measured with 17 items from the Social Adjustment Scale-Self Report for Youth (Weissman et al., 1980). The original scale has shown convergent validity with clinician and collateral ratings (mean r = .72) and sensitivity to treatment effects (Weissman & Bothwell, 1976). The 17-item version has shown internal consistency (α = .77) and 1-week test–retest reliability (r = .83; Stice et al., 2008). Participants were asked to “circle the best response to describe your behavior over the last 6 months” using a 5-point response (1 = never, 5 = always); three positively worded items were reverse coded so that higher scores indicated poorer functioning. An average score was created for each domain. The family domain (α = .81) consisted of two items: “Had arguments with your family?” and “Had your feeling hurt by a family member?” The school domain (α = .81) consisted of four items: “Missed school?”; “Felt upset at school?”; “Felt ashamed of how you do your school work?” and “Had arguments with people at school?” The work domain (α = .76) consisted of four items: “Missed work?”; “Felt upset at work?”; “Felt ashamed of how you do your work?” and “Had arguments with people at work?” The 7-item friends domain showed lower internal consistency (α = .51) suggesting that functioning with same-aged peers might be more variable. Items were as follows: “Seen friends or spoken on the telephone?”; “Gone out socially with other people, such as to a movie?”; “How often have you had arguments with friends?”; “How often have you had your feelings hurt by a friend?”; “How often have you felt shy or uncomfortable with people?”; “How often have you felt lonely and wished for more friends?”; and “How often have you dated someone?” .
Statistical Procedures
We first examined the univariate predictive effects of impairments in the 4 specific domains of psychosocial functioning predicted future onset of any eating disorder. Univariate Cox proportional hazard models tested whether each of the baseline domains of psychosocial functioning, when they were examined separately, predicted time to the onset of any partial/full syndrome eating disorder. Second, we tested the unique influence of each subdomain via multivariate analyses (controlling for other subdomains) associated with disorder onset. Multivariate Cox proportional hazard models were used to examine which of the baseline domains of psychosocial functioning, adjusted for the other subdomains, contributed the most unique influence to onset of any partial/full syndrome eating disorder.
Models specified onset of disorder in months since the baseline assessment and were fit with STATA software. Participants who met diagnostic criteria at baseline were excluded from the Cox models. The Breslow (1974) method was used to handle tied event times in the hazard models. The proportional hazard assumption for each model was examined and tested with Schoenfeld residuals.
Missing onset data were accounted for with right-censoring in the hazard models. Missing data for psychosocial predictors were minimal (1–2%) with the exception of the work domain (22%) because not all participants were employed. Models controlled for the condition to which participants were assigned. We examined whether intervention condition interacted with each of the psychosocial functioning measures in predicting eating disorder onset; not of those interactions were significant, suggesting that condition did not differentially impact the predictive effects of functioning.
In a third step, we subdivided the measure into its 17 individual items to explore, using classification tree analysis (CTA; Breiman, Friedman, Stone, & Olshen, 2918) to examine which specific aspect(s) of functioning best predicted onset of any eating disorder. This seemed important because some of the domain subscales had low internal consistency and also because CTA is uniquely able to detect interactions, including non-linear interactions (Breiman et al., 1984). CTA is a hypothesis-generating approach that investigates potential interactions between risk factors in the prediction of a dichotomous outcome (e.g., eating disorder onset). CTA first identifies the single most potent risk factor that predicts the outcome and selects the optimal cutpoint on that risk factor that creates subgroups with maximally different probabilities for the outcome. This process is repeated in each of the identified subgroups, or branches, in a recursive fashion until there are no remaining predictors for adequately large groups of participants. When different risk factors emerge for two branches from the same fork, it signifies an interaction. The Chi-Square Automatic Interaction Detection (CHAID) growing method was used and the minimum node size was set at 25 for the parent (i.e., initial) node and 10 for child (i.e., subsequent) nodes to minimize Type I error and influential outliers. A Bonferroni correction was used to maintain alpha at p = .05 for splitting nodes. CTA provides a nonparametric alternative to linear and additive logistic models for dichotomous outcomes and is an exploratory method of examining (a) which specific psychosocial functioning items are most predictive of eating disorder onset, and (b) what cutpoints of each item provide the greatest predictive ability.
Results
Preliminary Analyses
At baseline, 8.5% of the 1,272 participants met diagnostic criteria for an eating disorder and were excluded from analyses, resulting in a sample of 1,153; among the participants who were diagnosis-free at baseline, 12.5% showed onset of a threshold or subthreshold eating disorder during the 36-month follow-up. Table 1 provides correlations and descriptive statistics for the study predictors. Correlations ranged from r = .15 to .40 (all p < .001; mean r = .29). Data suggest that school functioning was most strongly correlated with functioning in the family (r = .40) and work domains (r = .40). Mean functional impairment scores were highest for family (mean = 2.77; SD = 1.02), followed by friends (mean = 2.75; SD = 0.62), school (mean = 2.18; SD = 0.70), and work (mean = 1.48; SD = 0.59).
Table 1.
Pearson Correlations and Descriptive Statistics for Study Predictors
| 1 | 2 | 3 | 4 | ||
|---|---|---|---|---|---|
| 1. | Peer group | 1.00 | |||
| 2. | Family | .29 | 1.00 | ||
| 3. | School | .34 | .40 | 1.00 | |
| 4. | Work | .15 | .18 | .40 | 1.00 |
| Mean | 2.75 | 2.77 | 2.18 | 1.48 | |
| SD | 0.62 | 1.02 | 0.70 | 0.59 |
N = 1,153. All correlation statistically significant at p < .001.
Domain Subscale Predictors of Eating Disorders Onset
We first estimated univariate Cox proportional hazard models to determine the relations between baseline functional impairment domains and future onset of an eating disorder (Table 2). Three of the four psychosocial domains significantly predicted onset of any eating disorder: friends, family and school. The domain of work did not have a predictive effect, potentially because 22% of the sample was not working. In these three models, a one unit increase in raw scores on the domain measures of friends, family, and school impairment was associated with a 107%, 22%, and 43% increase in hazard of an eating disorder onset, respectively. Next, we ran a multivariate Cox proportional hazard models with those psychosocial functioning domains (friends, family, and school) that showed significant relations to eating disorder onset. In this model only the friends functioning domain showed a significant unique effect (see Table 2). A one unit increase in raw score on this domain was associated with an increased hazard of 92% of disorder onset.
Individual Item Predictors of Eating Disorders Onset
We then conducted an exploratory CTA to test whether any of the 17 items of the psychosocial functioning scale predicted onset of an eating disorder, singly or in combination. All items were coded so that higher scores indicated greater impairment. Results are shown in Figure 1. Each box in the figure shows the number of participants in that branch of the classification tree and the number (and percentage) who developed an eating disorder over follow-up (incidence rates refer to only the number of participants in that specific box and do not reflect cumulative risk). The friends item of “How often have you felt lonely and wished for new friends?” emerged as the most potent predictor of eating disorder onset creating a three level split; the model divided the total sample into 523 participants with low scores, 540 with medium scores, and 90 with high scores. Among participants with high loneliness scores, 26.7% developed a future eating disorder, compared to 14.3% of participants with medium loneliness scores, and 8.2% of participants with low loneliness scores, suggesting a 3-fold increase in risk for disorder onset for the highest versus lowest risk groups.
Figure 1.
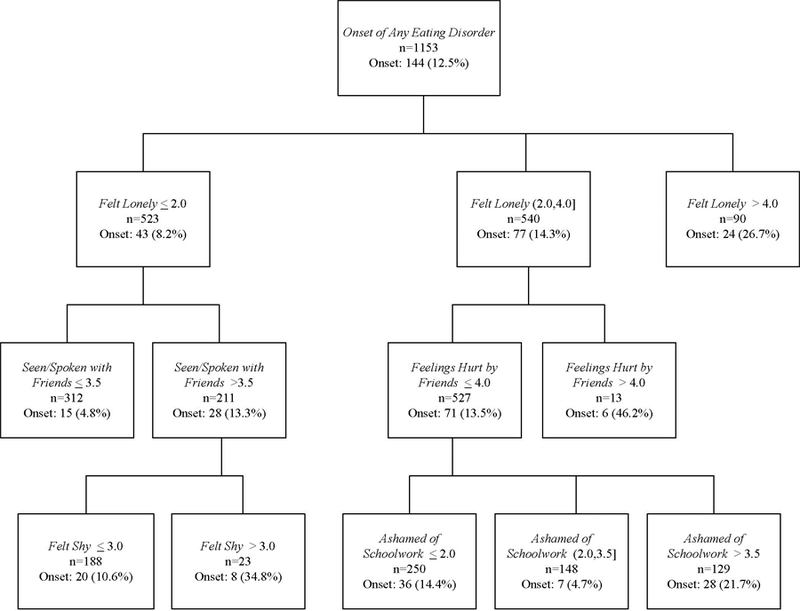
Classification Tree Analysis of Individual Psychosocial Functioning Items Predicting Eating Disorder Onset.
The CTA had four subsequent branches indicating different risk pathways, one for participants with low loneliness scores (it had two branches) and another pathway for participants with medium loneliness scores (it had two different branches). For participants with low loneliness, the friends item “Seen friends or spoken on the telephone?” was the first branch. Participants who reported low rates of seeing or speaking with friends had a 13.3% rate of eating disorder onset compared a rate of 4.8% for those who reported high rates, reflecting a 3-fold increase in onset risk. Another significant branch emerged for participants with low friend engagement for the item “How often have you felt shy or uncomfortable with people?” Among this group of 211 participants, 34.8% of the 23 individuals who reported high rates of shyness experienced eating disorder onset compared to 10.6% of the remaining 188 participants who reported low rates.
Another risk pathway emerged for the 540 participants who had medium loneliness scores, with two branches. First, a branch split was found for the friends item “Feelings get hurt by a friend?” For the small number of participants who scored very high on this measure (n = 13), almost half (46.2%) developed an eating disorder versus 13.5% for the remaining 527 participants who reported lower scores of hurt, which reflected a 3-fold increase in onset risk. The last branch occurred for the 527 participants who had low rates of hurt feelings, on the item “Felt ashamed of how you do your school work?” with three branches. This split was somewhat difficult to interpret because it suggested a quadratic effect in that the 129 participants with the highest rates of schoolwork embarrassment showed an incidence rate of 21.7% for an eating disorder onset versus 14.4% for the 250 participants with low scores, however, the lowest onset rate (4.7%) was for the 148 individuals with medium scores on this item. Overall, the CTA model had an 87.5% correct classification rate, indicating three general risk pathways.
Discussion
Our report is an exploratory analysis that sought to refine our understanding of psychosocial impairment, which was recently found to be the only variable in that study predicting future onset of each of the four eating disorders (Stice et al., 2017). Although a number of earlier papers have hypothesized the importance of factors related to psychosocial impairment in association with disordered eating and weight control behaviors, including public self-consciousness and social anxiety (Striegel-Moore, Silberstein, and Rodin, 1993), shame (Silberstein, Striegel-Moore, and Rodin, 1987), low assertiveness and social skill deficits (Arcelus, Haslam, Farrow, and Meyer, 2013), to our knowledge, only one other study (Jacobi et al., 2011) used a prospective design with non-disordered individuals to test the relation of psychosocial functioning to future eating disorder onset. To deepen the understanding of which specific aspects of this risk factor may increase risk for eating disorders, we examined this same high risk sample of young women to disaggregate the global measure of psychosocial functioning and investigate the univariate, multivariate, and individual item effects of specific functioning domains (friends, family, school and work) in an individual patient data (IPD) meta-analysis. Whereas the univariate models found significant predictive effects for the three domains of friends, family and school, a subsequent multivariate model found that the friends domain was the only aspect of functioning that had a unique predictive association with future eating disorder onset adjusting for other domains. The importance of friends functioning for adolescent well-being more broadly is well-known as social contacts with peers and the identification with a peer group are important for developmental tasks during this time period, including identity formation, positive self-concept, increased sense of autonomy from parents, and independent decision-making (Brown & Lohr, 1987; Sussman, Pokhrel, Ashmore, & Brown, 2007). The domain of work functioning did not have a univariate predictive effect on eating disorder onset, which may be explained by the smaller sample size because many participants did not work, which could have attenuated sensitivity, or because psychosocial functioning in the work domain is less important in explaining onset of eating disorders.
Although there are important reservations when relying on single items, the exploratory CTA of individual items from the functioning measure likewise underscored the potential importance of functioning problems with friends as risk factors for eating disorder onset, in that 4 of the 5 branches consisted of items from the friends domain. Loneliness in the area of same-aged peers was the strongest individual predictor. For young women who reported the highest loneliness, it was the sole predictor of eating disorder onset. For women with medium loneliness, reports of having one’s feelings hurt by friends amplified the predictive effects of loneliness. For women with low loneliness, low social contact with friends emerged as a pathway to eating disorder onset. The CTA model further suggested that high shyness amplified the risk conveyed by low social contact with friends for onset of any eating disorder.
The one non-friends item selected in the CTA model was feeling ashamed of one’s school work. For this item, both very low and very high feelings of shame were associated with greater eating disorder onset. We did not collect data on actual school performance and high shame could either signal actual or perceived poor academic performance that indicate high perfectionism and performance pressure (Forbush, Heatherton, & Keel, 2007) or fear of negative evaluation (Levinson & Rodebaugh, 2012), which have found to be associated with eating disorders. A prospective study found that high scholastic performance increased risk for the development of AN and BN (Sundquist, Ohlsson, Winkleby, Sundquist, & Crump, 2016).Overall, the CTA results are clearly hypothesis-generating rather than hypothesis-confirming, but suggest intriguing possibilities for future research.
Our findings are consistent with results of a prior prospective study that found that withdrawal from social activities, acting immature, getting teased, not being liked by one’s peers predicted onset of any type of subthreshold/threshold eating disorders, with mixed evidence for AN (Allen, Byrne, Oddy, Schmidt, & Crosby, 2014) Similarly, a large cross-sectional study comparing eating disordered patients with healthy controls found that retrospective reports of less socializing with friends preceded the onset of subthreshold and threshold eating disorders (Krug et al., 2013).
Though we did not conduct a sequential analysis to assess whether aspects of impaired psychosocial functioning predicted future increases in other established risk factors included in the Dual Pathway model (Stice, 1994), a recently published exploratory prospective study by Stice & Van Ryzin (in press) using different data, found that psychosocial impairment tended to precede the emergence of pursuit of the thin beauty ideal, which in turn typically emerged before body dissatisfaction, dieting, and negative affect, which typically emerged before the onset of BN, BED, and PD (AN onset was excluded in that study because body dissatisfaction, dieting, and negative affect did not predict onset of AN). In the context of the Dual Pathway model, it is possible that psychosocial impairments may motivate young women to begin pursuing the thin ideal in an effort to gain greater personal and social acceptance (Cruz-Saez, Pascual, Salaberria, Etxebarria, & Echeburua, 2015). Continued examination of psychosocial functioning in sequential pathways to the development of any or of specific types of eating disorder should be a focus of future research.
Our results are novel and may influence both etiological models and preventive programs for eating disorders. Our previous research found that impaired psychosocial functioning was the only risk factor to predict future onset of all four types of eating disorders. The present findings suggest that this risk may be driven most strongly by deficits in peer functioning, including loneliness, hurt feelings (perhaps indicating interpersonal sensitivity), limited social contact/social withdrawal, and shyness. Many of these aspects of functioning could be consequences of temperamental shyness and/or social anxiety, which have been found to be comorbid with AN and BN (Arcelus et al., 2013; Brewerton et al., 1995; Bulik, Sullivan, Weltzin, & Kaye, 1995; Kaye, Bulik, Thornton, Barbarich, & Masters, 2004; Levinson & Rodebaugh, 2012). Impairment in key areas of functioning is a fundamental aspect of all mental disorders (American Psychiatric Association, 2013) and disorders such as social anxiety, which could result in peer/friend functioning problems, have been found to predate eating disorder onset (Bulik, Sullivan, Fear, & Joyce, 1997). Regarding prevention implications, findings suggest that it might be useful if young women with deficits in friends, family, and school functioning were offered preventive intervention that focus on improving these limitations. These domains and possibly specific aspects of the friends domain (loneliness, poor interaction with peers, shyness) could serve both as potential screening variables and could guide the development of new preventive interventions aimed at increasing social engagement (behavioral activation), reducing social anxiety (social skills training), and possibly even academic tutoring, suggesting that psychosocial functioning is a risk factor that can be manipulated rather than being static. Interestingly, qualitative data from college aged women who completed the Body Project eating disorder prevention programs revealed that the most valued aspect of the intervention was the social support provided by other groups members (Shaw, Rohde, & Stice, 2016), potentially suggesting that one of the mechanism by which this intervention reduces eating disorder risk is by improving functioning with same-aged peers.
It is important to consider study limitations. The first category of limitations concerned our independent variable: psychosocial functioning is a broad construct that has been operationalized differently across studies (Ro & Clark, 2009). Also, psychosocial functioning was determined in the present report by a relatively brief self-report measure and some of the domains were assessed by a small number of items, some of which could also reflect symptoms of disorder (e.g., arguments as a symptom of Oppositional Defiant Disorder; shyness and social withdrawal as symptoms of Social Anxiety Disorder); thus differentiating psychosocial functioning from comorbid psychiatric disorders will be important in future research. The internal consistency of some of these domains (especially friends) was low, suggesting that the items do not represent a cohesive single domain. Also, we had no data on the reliability and validity of individual functioning items, which makes the CTA analyses particularly speculative. Ideally, we would have assessed multiple aspects of functioning with more extensive measures, include reports by friends, other peers, family members, teachers, and others in the network directly or check external validity with other measures (e.g., adverse childhood experiences) for conceptual overlap, as interactions between social factors, biological influences, earlier adverse events, and culture are complex (Spence & Rapee, 2016). A second type of limitation is that participants in this study completed eating disorder prevention programs, though the effects of condition were statistically adjusted for and the predictive effects of the risk factors were not found to be affected by condition. Third, due to the exploratory nature of this report, we examined a single dependent variable assessing the future onset of any eating disorder. Future research should evaluate if different subdomains of psychosocial functioning are associated or predict different eating disorders. Fourth, due to a fairly low incidence rate, the CTA model was built using the entire sample rather than developing an initial model with part of the sample and cross-validating it. Fifth, psychosocial functioning impairments had emerged as the sole transdiagnostic eating disorder risk factor in our prior research but that work did not include other variables which could lead to future psychosocial functioning problems, such as the receipt of critical eating and body-related comments, which predicted the onset of various eating disorders (Jacobi et al., 2011), or early childhood adversities, which were found to be associated with some forms of eating disorder (i.e., BN and eating disorders-not otherwise specified but not AN) in retrospective assessments (Larsen et al., 2017). Sixth, the study focused on women only and results may not apply to men.
To our knowledge, the present study is the first longitudinal prospective study to unpack the unique predictive effects of multiple psychosocial functioning domains on the future onset of eating disorders. By merging data across three trials using an individual patient data (IPD) meta-analysis and removing individuals with pre-existing eating disorders at baseline, the study was able to have greater statistical power to detect prospective onset effects with a rigorous methodology. It extends the findings of Stice et al. (2017) and begins to disaggregate the predictive effects of impaired psychosocial functioning domains and items, offering several tentative directions for both etiology models and better tailored prevention programs. Future research should attempt to replicate findings and further assess and unpack the predictive effects of impaired psychosocial functioning, and evaluate prevention programs that improve psychosocial functioning to experimentally test whether reducing psychosocial impairment prevents future onset of all eating disorders.
Acknowledgments
This study was partially supported by National Institutes of Health research grants MH/DK061957, MH070699, and MH086582.
References
- Agras WS (2001). The consequences and costs of the eating disorders. Psychiatric Clinics of North America, 24(2), 371–379. [DOI] [PubMed] [Google Scholar]
- Allen KL, Byrne SM, Forbes D, & Oddy WH (2009). Risk Factors for Full- and Partial-Syndrome Early Adolescent Eating Disorders: A Population-Based Pregnancy Cohort Study. Journal of the American Academy of Child & Adolescent Psychiatry, 48(8), 800–809. doi: 10.1097/CHI.0b013e3181a8136d [DOI] [PubMed] [Google Scholar]
- Allen KL, Byrne SM, Oddy WH, Schmidt U, & Crosby RD (2014). Risk factors for binge eating and purging eating disorders: differences based on age of onset. International Journal of Eating Disorders, 47(7), 802–812. doi: 10.1002/eat.22299 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington. VA: American Psychiatric Publishing. [Google Scholar]
- Arcelus J, Haslam M, Farrow C, & Meyer C (2013). The role of interpersonal functioning in the maintenance of eating psychopathology: A systematic review and testable model. Clinical Psychology Review, 33(1), 156–167. [DOI] [PubMed] [Google Scholar]
- Bohn K, Doll HA, Cooper Z, O’Connor M, Palmer RL, & Fairburn CG (2008). The measurement of impairment due to eating disorder psychopathology. Behaviour Research and Therapy, 46(10), 1105–1110. doi: 10.1016/j.brat.2008.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breiman L, Friedman J, Stone CJ, & Olshen RA (1984). Classification and Regression Trees: Taylor & Francis. [Google Scholar]
- Brewerton TD, Lydiard RB, Herzog DB, Brotman AW, O’Neil PM, & Ballenger JC (1995). Comorbidity of axis I psychiatric disorders in bulimia nervosa. Journal of Clinical Psychiatry, 56(2), 77–80. [PubMed] [Google Scholar]
- Brown BB, & Lohr MJ (1987). Peer-group affiliation and adolescent self-esteem: an integration of ego-identity and symbolic-interaction theories. Journal of Personality and Social Psychology, 52(1), 47–55. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Fear JL, & Joyce PR (1997). Eating disorders and antecedent anxiety disorders: a controlled study. Acta Psychiatrica Scandinavica, 96(2), 101–107. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Weltzin TE, & Kaye WH (1995). Temperament in eating disorders. International Journal of Eating Disorders, 17(3), 251–261. doi: [DOI] [PubMed] [Google Scholar]
- Cruz-Saez S, Pascual A, Salaberria K, Etxebarria I, & Echeburua E (2015). Risky eating behaviors and beliefs among adolescent girls. Journal of Health Psychology, 20(2), 154–163. doi: 10.1177/1359105313500683 [DOI] [PubMed] [Google Scholar]
- Fichter MM, & Quadflieg N (2016). Mortality in eating disorders - results of a large prospective clinical longitudinal study. International Journal of Eating Disorders, 49(4), 391–401. doi:doi: 10.1002/eat.22501 [DOI] [PubMed] [Google Scholar]
- Forbush K, Heatherton TF, & Keel PK (2007). Relationships between perfectionism and specific disordered eating behaviors. International Journal of Eating Disorders, 40(1), 37–41. doi: 10.1002/eat.20310 [DOI] [PubMed] [Google Scholar]
- Herzog DB, Pepose M, Norman DK, & Rigotti NA (1985). Eating disorders and social maladjustment in female medical students. Journal of Nervous and Mental Disease, 173(12), 734–737. [DOI] [PubMed] [Google Scholar]
- Jacobi C, Fittig E, Bryson SW, Wilfley D, Kraemer HC, & Taylor CB (2011). Who is really at risk? Identifying risk factors for subthreshold and full syndrome eating disorders in a high-risk sample. Psychological Medicine, 41(9), 1939–1949. doi: 10.1017/s0033291710002631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye WH, Bulik CM, Thornton L, Barbarich N, & Masters K (2004). Comorbidity of anxiety disorders with anorexia and bulimia nervosa. American Journal of Psychiatry, 161(12), 2215–2221. doi: 10.1176/appi.ajp.161.12.2215 [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Offord D, & Kupfer D (2001). How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry, 158(6), 848–856. doi: 10.1176/appi.ajp.158.6.848 [DOI] [PubMed] [Google Scholar]
- Krug Isabel, Penelo Eva, Fernandez-Aranda Fernando, Anderluh Marija, Bellodi Laura, Cellini Elena, . . . Treasure Janet. (2013). Low social interactions in eating disorder patients in childhood and adulthood: A multi-centre European case control study. Journal of Health Psychology, 18(1), 26–37. doi: 10.1177/1359105311435946 [DOI] [PubMed] [Google Scholar]
- Larsen JT, Munk‐Olsen T, Bulik CM, Thornton LM, Koch SV, Mortensen PB, & Petersen L (2017). Early childhood adversities and risk of eating disorders in women: A Danish register‐based cohort study. International Journal of Eating Disorders, 50(12), 1404–1412. doi: 10.1002/eat.22798 [DOI] [PubMed] [Google Scholar]
- Levinson CA, & Rodebaugh TL (2012). Social anxiety and eating disorder comorbidity: the role of negative social evaluation fears. Eating Behaviors, 13(1), 27–35. doi: 10.1016/j.eatbeh.2011.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch FL, Striegel-Moore RH, Dickerson JF, Perrin N, Debar L, Wilson GT, & Kraemer HC (2010). Cost-effectiveness of guided self-help treatment for recurrent binge eating. Journal of Consulting and Clinical Psychology, 78(3), 322–333. doi: 10.1037/a0018982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandelli L, Arminio A, Atti AR, & De Ronchi D (2018). Suicide attempts in eating disorder subtypes: a meta-analysis of the literature employing DSM-IV, DSM-5, or ICD-10 diagnostic criteria. Psychological Medicine, 1–13. doi: 10.1017/s0033291718003549 [DOI] [PubMed] [Google Scholar]
- Mehta S, Mittal PK, & Swami MK (2014). Psychosocial Functioning in Depressive Patients: A Comparative Study between Major Depressive Disorder and Bipolar Affective Disorder. Depression Research and Treatment, 6. doi: 10.1155/2014/302741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melioli T, Bauer S, Franko DL, Moessner M, Ozer F, Chabrol H, & Rodgers RF (2016). Reducing eating disorder symptoms and risk factors using the internet: A meta-analytic review. International Journal of Eating Disorders, 49(1), 19–31. doi: 10.1002/eat.22477 [DOI] [PubMed] [Google Scholar]
- Pisetsky EM, Thornton LM, Lichtenstein P, Pedersen NL, & Bulik CM (2013). Suicide attempts in women with eating disorders. Journal of Abnormal Psychology, 122(4), 1042–1056. doi: 10.1037/a0034902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ro E, & Clark LA (2009). Psychosocial functioning in the context of diagnosis: assessment and theoretical issues. Psychological Assessment, 21(3), 313–324. doi: 10.1037/a0016611 [DOI] [PubMed] [Google Scholar]
- Shaw H, Rohde P, & Stice E (2016). Participant feedback from peer-led, clinician-led, and internet-delivered eating disorder prevention interventions. International Journal of Eating Disorders, 49(12), 1087–1092. doi: 10.1002/eat.22605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silberstein LR, Striegel-Moore RH, & Rodin J (1987). Feeling fat: A woman’s shame. In Lewis HB (Ed.), The role of shame in symptom formation (pp. 89–108). Hillsdale, NJ: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Simon J, Schmidt U, & Pilling S (2005). The health service use and cost of eating disorders. Psychological Medicine, 35(11), 1543–1551. doi: 10.1017/s0033291705004708 [DOI] [PubMed] [Google Scholar]
- Spence SH, & Rapee RM (2016). The etiology of social anxiety disorder: An evidence-based model. Behaviour Research and Therapy, 86, 50–67. [DOI] [PubMed] [Google Scholar]
- Stice E (1994). Review of the evidence for a sociocultural model of bulimia nervosa and an exploration of the mechanisms of action. Clinical Psychology Review, 14(7), 633–661. doi: 10.1016/0272-7358(94)90002-7 [DOI] [Google Scholar]
- Stice E, Gau JM, Rohde P, & Shaw H (2017). Risk factors that predict future onset of each DSM-5 eating disorder: Predictive specificity in high-risk adolescent females. Journal of Abnormal Psychology, 126(1), 38–51. doi: 10.1037/abn0000219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti CN, & Durant S (2011). Risk factors for onset of eating disorders: evidence of multiple risk pathways from an 8-year prospective study. Behaviour Research and Therapy, 49(10), 622–627. doi: 10.1016/j.brat.2011.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti CN, & Rohde P (2013). Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. Journal of Abnormal Psychology, 122(2), 445–457. doi: 10.1037/a0030679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti CN, Spoor S, Presnell K, & Shaw H (2008). Dissonance and healthy weight eating disorder prevention programs: long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology, 76(2), 329–340. doi: 10.1037/0022-006x.76.2.329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Butryn ML, Shaw H, & Marti CN (2015). Effectiveness trial of a selective dissonance-based eating disorder prevention program with female college students: Effects at 2- and 3-year follow-up. Behaviour Research and Therapy, 71, 20–26. doi: 10.1016/j.brat.2015.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, & Van Ryzin MJ (in press). A Prospective Test of the Temporal Sequencing of Risk Factor Emergence in the Dual Pathway Model of Eating Disorders. Journal of Abnormal Psychology doi: 10.1037/abn0000400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Striegel-Moore RH, Silberstein LR, & Rodin J (1993). The social self in bulimia nervosa: public self-consciousness, social anxiety, and perceived fraudulence. Journal of Abnormal Psychology, 102, 297–303. [DOI] [PubMed] [Google Scholar]
- Sundquist J, Ohlsson H, Winkleby MA, Sundquist K, & Crump C (2016). School Achievement and Risk of Eating Disorders in a Swedish National Cohort. Journal of the American Academy of Child and Adolescent Psychiatry, 55(1), 41–46.e41. doi: 10.1016/j.jaac.2015.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S, Pokhrel P, Ashmore RD, & Brown BB (2007). Adolescent peer group identification and characteristics: a review of the literature. Addictive Behaviors, 32(8), 1602–1627. doi: 10.1016/j.addbeh.2006.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, & Merikangas KR (2011). Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry, 68(7), 714–723. doi: 10.1001/archgenpsychiatry.2011.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas D, Radji S, & Benedetti A (2014). Systematic review of methods for individual patient data meta- analysis with binary outcomes. BMC Medical Research Methodology, 14, 79. doi: 10.1186/1471-2288-14-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman M, & Bothwell S (1976). Assessment of Social Adjustment by Patient Self-Report. Archives of General Psychiatry, 33, 1111–1115. doi: 10.1001/archpsyc.1976.01770090101010 [DOI] [PubMed] [Google Scholar]
- Weissman M, Orvaschel H, & Padian N (1980). Children’s symptom and social functioning self-report scales. Comparison of mothers’ and children’s reports. Journal of Nervous and Mental Disease, 168(12), 736–740. [DOI] [PubMed] [Google Scholar]
- Wentz E, Gillberg IC, Anckarsater H, Gillberg C, & Rastam M (2009). Adolescent-onset anorexia nervosa: 18-year outcome. British Journal of Psychiatry, 194(2), 168–174. doi: 10.1192/bjp.bp.107.048686 [DOI] [PubMed] [Google Scholar]
- Wilksch SM, O’Shea A, Taylor CB, Wilfley D, Jacobi C, & Wade TD (2017). Online prevention of disordered eating in at-risk young-adult women: a two-country pragmatic randomized controlled trial. Psychological Medicine, 48(12), 2034–2044. doi: 10.1017/S0033291717003567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilksch SM, O’Shea A, & Wade TD (2018). Media Smart-Targeted: Diagnostic outcomes from a two-country pragmatic online eating disorder risk reduction trial for young adults. International Journal of Eating Disorders, 51(3), 270–274. doi:doi: 10.1002/eat.22825 [DOI] [PubMed] [Google Scholar]


