Abstract
Background & Aims:
Irritable bowel syndrome (IBS) is a stress-sensitive disorder associated with dysregulation of the hypothalamic–pituitary–adrenal pathway. We studied the cumulative effect of events during adulthood on this pathway in patients with IBS.
Methods:
We studied 129 patients with IBS, based on Rome III criteria (mean age 28.1 years, 66% women), and 108 healthy individuals (controls; mean age 29.8 years, 60% women) who completed the Life Experiences Survey from August 2013 to September 2017. Data were collected on the presence and effects of events since age 18, IBS severity scores, and IBS-related quality of life. For a subset of subjects, we measured serum cortisol and adrenocorticotropic hormone (ACTH) production in response to administration of corticotrophin-releasing factor and ACTH.
Results:
Compared with controls, patients with IBS perceived more adulthood life events as negative and had a significantly higher negative life event impact score (14.17±12.04 vs 10.83±9.98; P=.022). In patients with IBS, the presence of more-negatively perceived adulthood life events was associated with worse IBS symptom severity (β=1.53, 95% CI, 0.21–2.84; P=.025) and IBS-related quality of life (β=−0.70; 95% CI, −1.02 to −0.38; P<.001). Negatively perceived adulthood life events were associated with reduced production of ACTH in response to corticotrophin-releasing factor in patients with IBS compared with controls (P<.05).
Conclusion:
In a study of more than 200 subjects, we associated more-negatively perceived events during adulthood with an increased risk for IBS, worse symptom severity and quality of life, and a dysregulated stress response. Understanding the effects of events that cause stress in adults and their perceived effects on IBS may help guide disease management.
Keywords: Life events survey (LES), hypothalamic-pituitary-adrenal (HPA), quality of life, irritable bowel syndrome (IBS)
Introduction
Irritable bowel syndrome (IBS) is a stress-sensitive disorder of brain-gut interactions1 that is characterized by the presence of abdominal pain associated with defecation, change in stool frequency and/or change in stool form.2 The pathophysiology of IBS is multifactorial in nature and there is evidence that IBS is a stress sensitive disorder. Multiple studies have demonstrated that early adverse life events (EALs) that occur prior to the age of 18 are associated with the development3 and severity4 of IBS symptoms. In addition, we have previously shown that EALs are associated with enhanced stress responsiveness involving the hypothalamic-pituitary-adrenal (HPA) axis in both IBS patients and healthy individuals.5,6 Dysregulation of the HPA axis has been demonstrated in patients with IBS in response to psychological or physical stress and to hormone challenge.6,7
Prior studies in IBS subjects have examined the role of stressful or negatively perceived adulthood life events occurring in the three to twelve months prior to study enrollment.8–11 In a study by Drossman et al., those with IBS who sought medical care had fewer positively perceived life events in the previous six months.8 Dinan et al. demonstrated that, compared to patients with peptic ulcer disease, those with IBS perceived a more negative overall impact of life events in the previous one year despite documenting the same total number of events.9 Whitehead et al. furthered these findings by demonstrating that IBS patients reported more stressful life events in the previous three months compared to healthy controls. Those who reported more stressful life events were more likely to seek medical care and had a higher number of annual disability days.10 In a study of post-infection IBS, a higher reported number of life events in the past twelve months was associated with IBS, but their perceived impact was not.11 The cumulative effect of all potential life changing events occurring in adulthood, and their perceived impact, on the development and severity of IBS has not been studied. Furthermore, the effect of these potentially stressful or negative life events on the stress response system, specifically the HPA axis, has not been examined.
The purpose of this study is to determine if cumulative life events in adulthood, and their perceived impact, are associated with the risk of having IBS, the severity of IBS symptoms, disease-related quality of life, and HPA axis response to hormone challenge. We aimed to study the following hypotheses: 1) IBS patients will have more negatively perceived life events in adulthood compared to healthy controls; 2) The presence of both negatively perceived life events in adulthood and EALs will increase the probability of having a diagnosis of IBS compared to those with negatively perceived adulthood life events alone; 3) In those with IBS, having more negatively perceived events in adulthood will be associated with worse IBS symptom severity and IBS-related quality of life; and 4) The presence of more negatively perceived events in adulthood will be associated with enhanced stimulated HPA axis response in IBS compared to controls.
Methods
Study Subjects
Participants who were at least 18 years of age were obtained from a group of IBS patients and controls who were previously recruited for studies conducted by our center from August 2013 to September 2017 and had completed the questionnaires detailed below. All IBS subjects fulfilled the Rome III diagnostic criteria12 and the diagnosis of IBS was confirmed by a clinician with expertise in this area. Controls did not have a history of IBS or other gastrointestinal (GI) disorders. The subjects were recruited predominantly from community advertisements. Exclusion criteria for both groups included presence of chronic GI disease (i.e.: celiac disease, inflammatory bowel disease, malignancy, cirrhosis) and poorly controlled psychiatric disease. Clinical characteristics included age, sex, and BMI were collected. This study was approved by the University of California Los Angeles Institutional Review Board. All study subjects signed a written informed consent prior to inclusion in these studies. Participants were compensated for completion of a history, physical examination and a variety of questionnaires.
Questionnaires
Life Events Survey (LES)13-
This validated survey contains sixty potential life events. It is designed to document both the presence of and impact (as rated on a scale of −3 to +3) of events that have occurred in the year prior to survey completion. In this study a modified version of the LES was used whereby subjects documented the presence and perceived impact of adulthood life events that occurred since age 18 to the time of completion of the survey. For the purposes of this study, three scores were generated from this survey; the number of negatively perceived life events (0 to 60), the negative impact score determined by the sum of the impact scores of negatively perceived life events alone (0 to 180; higher scores indicate greater negative impact), and the total impact score determined by the sum of the impact scores of both negatively and positively perceived life events (−180 to 180; higher scores indicate an overall more positive impact and lower scores indicate an overall more negative impact of all adulthood life events).
Adverse Childhood Experience (ACE) survey14-
This questionnaire includes 18 validated questions that document the presence of EALs that occurred prior to age 18 in eight domains (emotional abuse, physical abuse, sexual abuse, substance abuse exposure, parental separation, mental illness exposure, the presence of an incarcerated household member and violence toward a parent). Each domain is given one point if the respondent indicates a yes answer to any of the questions in that domain. This generates a score out of eight with higher scores indicating the presence of more EALs. We have previously measured EALs using ACE in IBS and HCs.4
IBS-Severity Scoring System (IBS-SSS)15-
This is a validated scoring system that measures the severity of IBS symptoms. Visual analog scales are used to indicate the number of days out of ten where abdominal pain is present, the severity of abdominal pain and distension, satisfaction with bowel movements, and the degree to which IBS symptoms are interfering with life in general. The maximum score is 500. Those with scores less than 175 are considered to have mild symptoms, 175 to 300 moderate symptoms and greater than 300 severe symptoms.
IBS-Quality of Life (IBS-QOL)16-
This thirty four question validated survey measures the impact of IBS on the respondent’s quality of life. A total score is generated and then transformed into a score out of 100 with higher scores indicating a higher quality of life.
Hormone Challenge Tests
A subset of patients who completed the LES underwent a corticotrophin releasing factor (CRF) stimulation test and an adrenocorticotrophin hormone (ACTH) stimulation test as part of a previously published study.6 For the CRF stimulation test, serum ACTH and cortisol levels were measured at 60 minutes, 30 minutes and just prior to administration of CRF. Subjects were then administered intravenous ovine CRF at a dose of 1 μg kg−1. Serum ACTH and cortisol levels were then measured at the 5, 15, 30, 60, 90 and 120-minute time points. At least one week after the CRF stimulation test, subjects underwent the ACTH stimulation test. Baseline serum ACTH and cortisol levels were measured at 30 minutes and just prior to administration of ACTH. Intravenous 25 μg Cortrosyn (Organon, West Orange, New Jersey) and serum cortisol levels were measured at 30, 60, 90, 120, 150 and 180-minute time points. All samples were collected and processed according to the standard procedures of the UCLA Clinical and Translational Research Center.
Statistical Analysis
Clinical characteristics were stratified by IBS status and summarized as count (%) and mean standard deviation (SD). Categorical variables were compared with IBS status using a chi-squared test and continuous variables using a t-test. Logistic regression was used to evaluate 1) the association of negatively perceived adulthood life events (number and LES impact scores) with IBS status and 2) whether negatively perceived adulthood life events with at least one EAL (ACE score ≥1) and negatively perceived adulthood life events without EALs (ACE score of 0) were predictive of an increased probability of having IBS while controlling for age, sex and BMI. Linear regression was used to determine the association of negatively perceived adulthood life events (number and LES impact scores) with measures of IBS symptom severity and IBS-related quality of life. Area under the curve with respect to the minimum value (AUCi) was calculated to measure the overall magnitude of ACTH and cortisol response to hormone challenge. Linear regression was also used to determine whether the association between negatively perceived adulthood life events (number and LES impact scores) and HPA axis (AUCi) differed by IBS status by including an interaction term between HPA axis and IBS status in the model. All regression models adjusted for age, sex and BMI. All analyses were done using R version 3.4.4 (http://cran.r-project.org/). Statistical significance was defined as p<0.05.
Results
Subject Characteristics
One hundred and twenty-nine Rome III12 positive IBS patients (66% women, average age 28.09±9.61 years) and 108 controls (60% women, average age 29.75±9.77 years) were included in this study. Compared to controls, the IBS patients had a significantly lower average BMI and higher ACE scores (Table 1). In those with IBS, the average IBS-SSS score was 236.62±85.45 which is considered moderate IBS symptom severity.
Table 1:
Subject Characteristics
| Clinical Characteristic: Mean (SD) | HCs (n=108) |
IBS (n=129) |
p-value |
|---|---|---|---|
| Female: n (%) | 65 (60%) | 85 (66%) | 0.44 |
| Age | 29.75 (9.77) | 28.09 (9.61) | 0.098 |
| BMI | 28.77 (5.8) | 24.53 (4.28) | <0.001 |
| Education | 0.186 | ||
| Some College or Less | 50 (48%) | 68 (55%) | |
| College Graduate | 30 (29%) | 23 (19%) | |
| Any Post Graduate Work | 24 (23%) | 33 (26%) | |
| ACE Score (range: 0–8) | 1.4 (1.79) | 1.85 (1.84) | 0.017 |
| IBS-SSS (range: 0–500) | 236.62 (85.45) | ||
| IBS-QOL (range: 0–100) | 66.75 (21.44) | ||
| IBS Rome III Subtype | |||
| IBS-C: n (%) | 24 (18.6%) | ||
| IBS-D: n (%) | 37 (28.7%) | ||
| IBS-M: n (%) | 66 (51.2%) | ||
| IBS-U: n (%) | 2 (1.5%) |
HCs-healthy controls; IBS-irritable bowel syndrome; SD-standard deviation; BMI-body mass index; ACE-adverse childhood experiences survey; IBS-SSS-IBS-severity scoring system; IBS-QOL-IBS quality of life.
p-value<0.05 is considered statistically significant.
Association of Adulthood Life Events and IBS
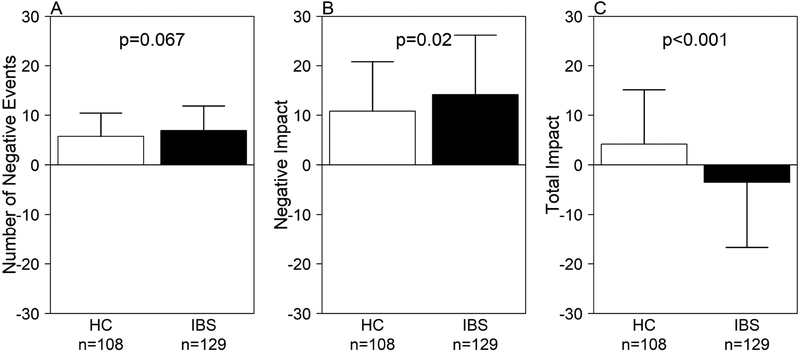
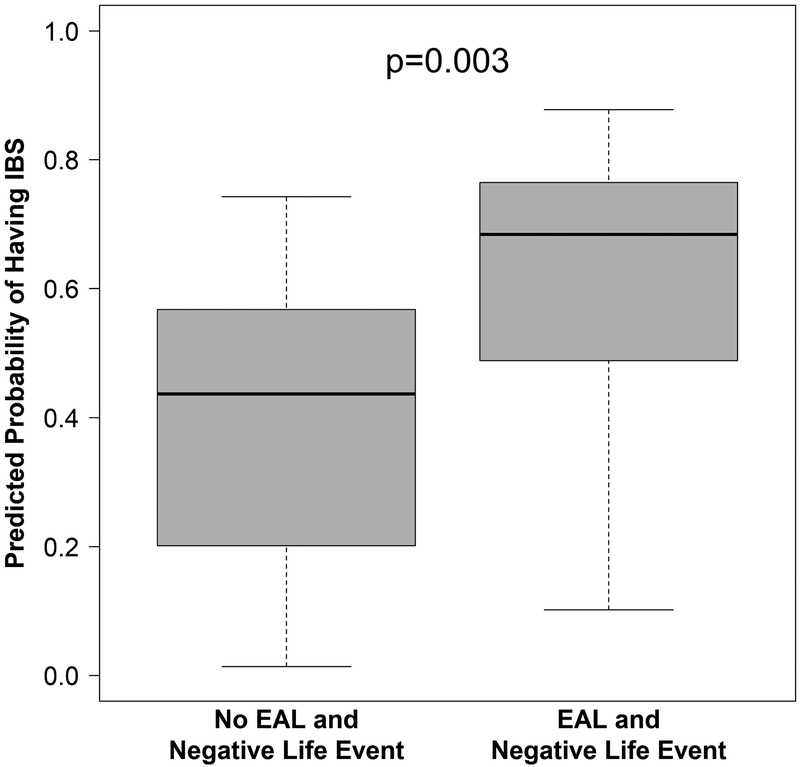
Subjects with IBS did not demonstrate a difference in the number of negatively perceived adulthood life events compared to controls (6.95±4.92 vs. 5.78±4.69 in HCs, p=0.067). However, the negative impact score (i.e., sum of impact scores of negatively perceived life events alone) was significantly greater in IBS patients compared to controls (14.17±12.04 vs. 10.83±9.98, p=0.022). IBS patients also had an overall negative total impact score (i.e., sum of the impact scores of both negatively and positively perceived life events), while controls had an overall positive impact score (−3.40±13.20 vs. 4.21±10.94 in HCs, p<0.001) (Figure 1). Subjects had a higher probability of having IBS if they reported at least one EAL and negatively perceived adulthood life events compared to those with negatively perceived adulthood life events and no history of EALs (Figure 2). These results did not differ by IBS bowel habit subtype.
Figure 1:
The association of adulthood life events in IBS compared to controls (HC). Those with IBS demonstrated A) a similar total number of negatively perceived adulthood life events (p=0.067); B) a greater negative impact score (p=0.02); and C) a more negative total impact score (p<0.001).
Figure 2:
The probability of having IBS in those with negatively perceived adulthood life events with and without EALs. Those with at least one EALs and negatively perceived adulthood life events were more likely to have irritable bowel syndrome (IBS) compared to those with negatively perceived adulthood life events alone and no EALs (p=0.003).
Association of Adulthood Life Events and IBS Symptom Severity and Quality of Life
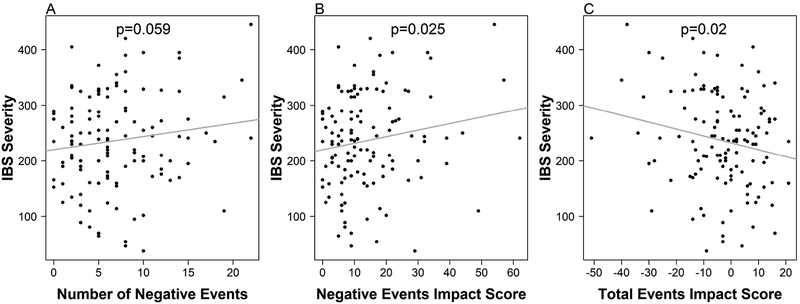
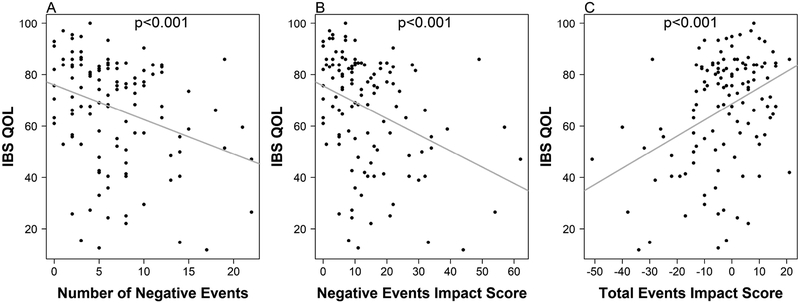
Worse IBS symptom severity was associated with a higher negative impact score (β=1.53, 95% CI (0.21, 2.84); p=0.025; a one point increase in IBS symptom severity is associated with an increase of 1.53 points in the negative impact score) and a more negative total impact score (β=−1.36, 95% CI (−2.49, −0.226); p=0.02; a one point score increase in IBS symptom severity is associated with a decrease of 1.36 in total impact score) (Figure 3). This association was not significant for the number of negatively perceived adulthood life events (β=3.15, 95% CI (−0.09, 6.37); p=0.059; a one point score increase in IBS symptom severity is associated with an increase of 3.15 negatively perceived adulthood life events). However, a poorer IBS-related QOL was associated with a greater number of negatively perceived adulthood life events (β=−1.48, 95% CI (−2.27, −0.68); p<0.001; a one point score decrease in IBS related quality QOL is associated with an increase of 1.48 negatively perceived adulthood life events), a higher negative impact score (β=−0.70, 95% CI (−1.02, −0.38); p<0.001; a one point score decrease in IBS related QOL is associated with an increase of 0.70 in the negative impact score) and a more negative total impact score (β=0.63, 95% CI (0.35, 0.90); p<0.001; a one point score increase in IBS related QOL is associated with an increase of 0.63 in the negative impact score) (Figure 4).
Figure 3:
The association of adulthood life events with IBS symptom severity. IBS symptom severity is not associated with A) the absolute number of negatively perceived adulthood life events (p=0.059). Worse IBS symptom severity is associated with B) a greater negative impact score (p=0.025) and C) a more negative total impact score (p=0.02).
Figure 4:
The association of adulthood life events in adulthood with IBS-related quality of life. Lower IBS-related quality of life is associated with A) a higher absolute number of negatively perceived adulthood life events (p<0.001), B) a greater negative impact score (p<0.001) and C) a more negative total impact score (p<0.001).
Association of Adulthood Life Events and HPA Axis Response to Hormone Challenge in IBS vs. HCs
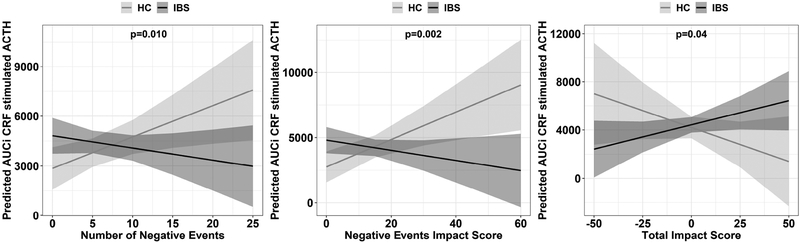
The hormone challenge tests were completed in 66 patients with IBS and 41 HCs. We have previously published the hormone stimulated HPA axis response and its relationship toe EALs in IBS and controls.6 In the current study, there were no significant differences between the participants who did and did not undergo hormone challenge testing. All three LES scores moderated the effect of IBS status on HPA axis (p<0.05 for all three scores). In controls, more negatively perceived adulthood life events, both by total number and negative impact scores, were associated with a greater ACTH response to CRF stimulation. In contrast, in IBS patients, more negatively perceived adulthood life events were associated with a blunted ACTH response to CRF stimulation (Figure 5). There were no significant associations between negatively perceived adulthood life events and CRF or ACTH stimulated cortisol responses.
Figure 5:
Association of adulthood life events with HPA response to CRF stimulation in IBS compared to controls (HC). Controls with more negatively perceived adulthood life events had a greater ACTH response to CRF stimulation that those with positively perceived life events. Those with IBS and more negatively perceived adulthood life events had a blunted ACTH response to CRF stimulation compared to controls. This effect is seen with A) the absolute number of negatively perceived adulthood life events (p=0.010), B) negative impact score (p=0.002) and C) total impact score (p=0.048).
Discussion
Previous studies have examined the relationship of adulthood life events in the three to twelve months prior to study enrollment with the presence of IBS, IBS symptom severity, healthcare utilization and productivity.8–11 The current study expands upon this work by demonstrating the following main findings: 1) Compared to controls, IBS patients reported a similar number of negatively perceived events in adulthood, but perceive these events as more stressful or negative; 2) The risk of having IBS associated with the presence of negatively perceived adulthood life events was further increased by a coexistent history of EALs; 3) In those with IBS, the presence of more negatively perceived adulthood life events was associated with worse IBS symptom severity and worse IBS-related QOL; and 4) The presence of negatively perceived adulthood life events was associated with a dysregulated stress response.
For a similar total number of negatively perceived life events in adulthood, those with IBS tend to rate the impact of these events more negatively than HCs. Thus, in adulthood, the subjective assessment of a life event as negative has a greater influence on having IBS and IBS-related outcomes, than the actual occurrence of a given life event. Our findings also suggest that the presence of more positively perceived adulthood life events serve as a protective factor in IBS associated with reduced symptom severity and increased disease-related QOL. This may have important therapeutic implications. IBS patients may benefit from treatment interventions, such as cognitive behavioral therapy (CBT), to reframe their thoughts around particular events or situations and lessen the perceived negative impact of these events in their lives. CBT has been shown to be an effective treatment in IBS and may exert its beneficial effect, at least in part, by reframing, reinterpreting, or altering the impact of these negatively perceived or stressful life events on symptoms.17
The effect of negatively perceived adulthood life events on IBS is even further enhanced in the presence of a positive history for EALs. This builds upon previous work that has demonstrated the important role that early life adversity plays in the development and severity of IBS.3,4 Individuals with a history of EALs are more likely to experience adverse life events in adulthood and may influence the perception of these events later in life.18 We have previously shown that IBS patients have decreased resilience, which is the ability to recover from and adapt positively to stress. Resilience is particularly decreased in individuals with a history of EALs.19 Thus, while it is clinically important to understand the role of adulthood life stressors on symptoms and overall well-being in patients with IBS, the presence of early life adversity cannot be neglected and should be addressed in patients if needed.
In our study, the increased ACTH response to CRF in HCs with negatively perceived adulthood life events but decreased response in IBS patients supports dysregulation of the pituitary response in IBS patients with stressful life events in adulthood. A number of studies have demonstrated HPA axis dysregulation in patients with IBS.7 Multiple factors can affect HPA axis function which is likely in part why studies have shown increased,20,21 decreased,22,23 or normal24 HPA axis response in IBS patients compared to HCs. We have previously shown that a history of EALs is associated with an enhanced cortisol response to a visceral stressor5 and to CRF stimulation.6 However, these prior studies did not address the relationship between hormone-stimulated HPA axis response and stressful life events in adulthood. Our current findings of an increased HPA axis response in HCs with a higher number of negatively perceived stressful life events in adulthood suggests that the effects of stressful life events on the the HPA axis normally continues from childhood to adulthood, although this is not the case in IBS.
The blunted HPA axis response in IBS patients with greater negatively perceived adulthood life events may be due to several reasons. Repeated exposure to the same stressor (called a ‘homotypic stressor’) can result in habituation, or reduced response, of the HPA axis that is mediated in part by the paraventricular nucleus of the hypothalamus (PVN).25 In the setting of non-habituating chronic stressors (e.g., unpredictable stress, severe stress), the HPA axis response can be enhanced or blunted depending on the type of stressor and the individual.25 For example, a recent met-analysis showed that EALs are associated with a blunted cortisol response to a social stressor.26 Although a blunted HPA axis response is thought to be due to reduced levels of CRF mRNA in the PVN in response to enhanced negative feedback or increased inhibitory neural input27 or due to adrenal hyporesponsiveness (“adrenal exhaustion”), these causes are less likely to explain the results in the current study. Blunted ACTH response to CRF administration in the setting of continued adverse stressful life events through adulthood in IBS may be more likely due to downregulation of the CRF-1 receptor at the level of the pituitary gland from chronically elevated levels of CRF. A dysregulated stress response system, as is present in IBS, may lead to GI dysfunction and symptoms downstream by various potential mechanisms.7
This study has several limitations. One limitation is that it is unclear whether the presence of more negatively perceived life events in adulthood is a causative factor in the development of IBS and worse symptom severity or whether patients with IBS, particularly those with more severe symptoms and poorer quality of life, are more likely to perceive life events as negative compared to controls. In addition, there is a risk for recall bias given that participants were asked about the impact of events that may have occurred several years prior to completion of the study. Furthermore, study participants were predominantly from the West Los Angeles area. It is unclear if there are geographic or cultural differences in the interpretation of the impact of a given life event. Finally, only a subset of patients underwent the hormone challenge tests. However, this is likely a representative sample as there were no significant differences between the groups that underwent the tests and those that did not.
In summary, our study is the first, to our knowledge, to show that the presence of more negatively perceived life events in adulthood is associated with an increased risk of having IBS, worse symptom severity, poorer disease-related QOL, and a dysregulated stress response in IBS. Understanding the role of adulthood life events and the perceived impact of those events in IBS patients may help guide the approach to treatment, which should include positive reframing of past and future life events with the goal of ultimately altering IBS symptom severity and improving QOL.
Supplementary Material
What You Need to Know.
Background:
We studied the cumulative effect of events during adulthood in patients with IBS.
Findings:
Compared with controls, patients with IBS perceived more adulthood life events as negative and had a significantly higher negative life event impact score. In patients with IBS, the presence of more-negatively perceived adulthood life events was associated with worse IBS symptom severity and IBS-related quality of life. The presence of more negatively perceived adulthood life events is associated with a blunted HPA axis response in IBS patients compared to healthy controls.
Implications for patient care
Understanding the impact of adulthood life events in IBS patients may help guide treatment which could include positive reframing of past and future life events.
Acknowledgements:
The staff of the G. Oppenheimer Center for Neurobiology of Stress and Resilience, University of California Los Angeles
Financial Support
The National Institute of Health (NIH) grants: P50 DK064539, P30 DK041301, T32 DK007180, K32 DK106528EJV supported by the NIH loan repayment program: L30 DK106759
Abbreviations
- IBS
Irritable bowel syndrome
- HPA
hypothalamic-pituitary-adrenal axis
- ACTH
adrenocorticotropic hormone
- CRF
corticotrophin releasing factor
- HCs
healthy controls
- EALs
early adverse life events
- LES
Life Events Survey
- ACE
Adverse Childhood Experience survey
- IBS-SSS
IBS-Severity Scoring System
- IBS-QOL
IBS- Quality of Life
- AUCi
area under the curve with respect to minimum value
- CBT
cognitive behavioral therapy
- PVN
paraventricular thalamic nucleus
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Potential Competing Interests
CHP- Allergan (Educational Support)
BDN- Nothing to disclose.
WS- Nothing to disclose.
APP- Nothing to disclose.
EJV- Nothing to disclose.
EAM- Nothing to disclose.
LC- Nothing to disclose.
References
- 1.Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology. 2016;150(6):1262–1279. [DOI] [PubMed] [Google Scholar]
- 2.Lacy BE, Mearin F, Chang L, et al. Bowel Disorders. Gastroenterology. 2016;150(6):1393–1407. [DOI] [PubMed] [Google Scholar]
- 3.Bradford K, Shih W, Videlock EJ, et al. Association between early adverse life events and irritable bowel syndrome. Clin Gastroenterol Hepatol. 2012;10(4):385–390 e381–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park SH, Videlock EJ, Shih W, et al. Adverse childhood experiences are associated with irritable bowel syndrome and gastrointestinal symptom severity. Neurogastroenterol Motil. 2016;28(8):1252–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Videlock EJ, Adeyemo M, Licudine A, et al. Childhood trauma is associated with hypothalamic-pituitary-adrenal axis responsiveness in irritable bowel syndrome. Gastroenterology. 2009;137(6):1954–1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Videlock EJ, Shih W, Adeyemo M, et al. The effect of sex and irritable bowel syndrome on HPA axis response and peripheral glucocorticoid receptor expression. Psychoneuroendocrinology. 2016;69:67–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang L The role of stress on physiologic responses and clinical symptoms in irritable bowel syndrome. Gastroenterology. 2011;140(3):761–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drossman DA, McKee DC, Sandler RS, et al. Psychosocial Factors in the Irritable Bowel Syndrome. Gastroenterology. 1988;95(3):701–708. [DOI] [PubMed] [Google Scholar]
- 9.Dinan TG, O’Keane V, O’Boyle C, et al. A comparison of the mental status, personality profiles and life events of patients with irritable bowel syndrome and peptic ulcer disease. Acta Psychiatr Scand. 1991;84:26–28. [DOI] [PubMed] [Google Scholar]
- 10.Whitehead WE, Crowell MD, Robinson JC, et al. Effects of stressful life events on bowel symptoms: subjects with irritable bowel syndrome compared with subject without bowel dysfunction. Gut. 1992;33:825–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parry SD, Barton JR, Welfare MR. Factors associated with the development of post-infectious functional gastrointestinal disease: does smoking play a role? European Journal of Gastroenterology & Hepatology. 2005;17(10):1071–1075. [DOI] [PubMed] [Google Scholar]
- 12.Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. Gastroenterology. 2006;130(5):1480–1491. [DOI] [PubMed] [Google Scholar]
- 13.Sarason IG, Johnson JH, Siegel JM. Assessing the Impact of Life Changes: Development of the Life Experiences Survey. Journal of Consulting and Clinical Psychology. 1978;46(5):932–946. [DOI] [PubMed] [Google Scholar]
- 14.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. American Journal of Preventive Medicine.14(4):245–258. [DOI] [PubMed] [Google Scholar]
- 15.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Alimentary Pharmacology and Therapeutics. 1997;11(2):395–402. [DOI] [PubMed] [Google Scholar]
- 16.Patrick D, Drossman D, Frederick I, et al. Quality of life in persons with irritable bowel syndorme: development and validation of a new measure. Dig Dis Sci. 1998;11:400–411. [DOI] [PubMed] [Google Scholar]
- 17.Ford AC, Quigley EMM, Lacy BE, et al. Effect of Antidepressants and Psychological Therapies, Including Hypnotherapy, in Irritable Bowel Syndrome: Systematic Review and Meta-Analysis. The American Journal of Gastroenterology. 2014;109(9):1350–1365. [DOI] [PubMed] [Google Scholar]
- 18.Jones TM, Nurius P, Song C, Fleming CM. Modeling life course pathways from adverse childhood experiences to adult mental health. Child Abuse & Neglect. 2018;80:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park SH, Naliboff BD, Shih W, et al. Resilience is decreased in irritable bowel syndrome and associated with symptoms and cortisol response. Neurogastroenterol Motil. 2018;30(1):e13155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fukudo S, Nomura T, Hongo M. Impact of corticotropin-releasing hormone on gastrointestinal motility and adrenocorticotropic hormone in normal controls and patients with irritable bowel syndrome. Gut. 1998;42(6):845–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dinan TG, Quigley EM, Ahmed SM, et al. Hypothalamic-pituitary-gut axis dysregulation in irritable bowel syndrome: plasma cytokines as a potential biomarker? Gastroenterology. 2006;130(2):304–311. [DOI] [PubMed] [Google Scholar]
- 22.Bohmelt AH, Nater UM, Franke S, Hellhammer DH, Ehlert U. Basal and stimulated hypothalamic-pituitary-adrenal axis activity in patients with functional gastrointestinal disorders and healthy controls. Psychosom Med. 2005;67(2):288–294. [DOI] [PubMed] [Google Scholar]
- 23.FitzGerald LZ, Kehoe P, Sinha K. Hypothalamic--pituitary--adrenal axis dysregulation in women with irritable bowel syndrome in response to acute physical stress. West J Nurs Res. 2009;31(7):818–836. [DOI] [PubMed] [Google Scholar]
- 24.Elsenbruch S, Lucas A, Holtmann G, et al. Public speaking stress-induced neuroendocrine responses and circulating immune cell redistribution in irritable bowel syndrome. Am J Gastroenterol. 2006;101(10):2300–2307. [DOI] [PubMed] [Google Scholar]
- 25.Herman JP, McKlveen JM, Ghosal S, et al. Regulation of the Hypothalamic-Pituitary-Adrenocortical Stress Response. Compr Physiol. 2016;6(2):603–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bunea IM, Szentagotai-Tatar A, Miu AC. Early-life adversity and cortisol response to social stress: a meta-analysis. Transl Psychiatry. 2017;7(12):1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Albeck DS, McKittrick CR, Blanchard DC, et al. Chronic social stress alters levels of corticotropin-releasing factor and arginine vasopressin mRNA in rat brain. The Journal of Neuroscience. 1997;17(12):4895–4903. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.