Abstract
Background and Aims:
Youth aged 15–17 years are at high risk of tobacco, alcohol, and drug use. Given the changing landscape with respect to availability, use of emerging products, and regulatory environments, we examined patterns and correlates of poly-substance use among U.S. youth aged 15–17 years.
Design:
Cross-sectional self-reported data.
Setting:
United States.
Participants:
6,127 U.S. youth aged 15–17 years from Wave 1 (2013–2014) of the nationally representative Population Assessment of Tobacco and Health (PATH) Study.
Measurements:
Latent class analysis was used to identify subgroups of poly-substance use including 12 tobacco products, alcohol, marijuana, prescription drugs, and other drugs. Socio-demographic characteristics, residence in urban area, sensation seeking, sexual orientation, and internalizing and externalizing problems were examined as correlates.
Findings:
Approximately 43.5% of 15–17-year olds used at least one substance in the past 12 months. A five-class model was identified: Class 1 ‘abstainers’ (67%), Class 2 ‘alcohol users’ (19%), Class 3 ‘alcohol, marijuana, and tobacco (AMTpredominant AM) users’ (8%), Class 4 ‘alcohol, marijuana, and tobacco (AMTpredominant T) users’ (4%), and Class 5 ‘alcohol, marijuana, tobacco, and other drug (AMTOD) users’ (1%). Abstainers were considered the reference class. Higher sensation seeking scores, higher age, and lower academic grades were each associated with greater likelihood of membership in all user classes. Gender, race/ethnicity, parents/guardians’ education, residence in non-urban areas, and sexual minority groups were associated with membership in some but not all user classes. Compared with no/low/moderate severity, high severity internalizing problems were associated with membership in classes 2, 3, and 5, whereas high severity externalizing problems were associated with membership in classes 3 and 5 only.
Conclusions:
There appear to be three heterogeneous poly-substance use classes among U.S. youth aged 15–17 years. Correlates of substance use among U.S. youth include higher sensation seeking, poor academic performance, urban residence, minority sexual orientation, and mental health problems.
Keywords: poly-substance use, tobacco products, alcohol, marijuana, drugs, youth, correlates
INTRODUCTION
Onset of tobacco, alcohol, and drug use generally occurs during adolescence (1–3). Between 10–20% of U.S. youth report past month tobacco use (4, 5); cigarettes, e-cigarettes, certain cigar types (e.g. cigarillos) and hookah are most commonly used (4, 6). Among youth who use tobacco, multiple product use is common (7, 8), especially among high school students (5). Moreover, youth tobacco users, particularly those who use multiple tobacco products, are also more likely to use alcohol and drugs and to report substance use disorders (SUDs) (8–11). These youth are at risk for several immediate adverse outcomes including dropping out of high school and lower educational attainment (12), cognitive impairment (13), and problem behaviors (e.g. violence, criminal activity, and risky sexual behaviors (14)). Multiple substance use during adolescence is also known to predict substance use and dependence during adulthood (15).
Studies have used latent class analysis, a flexible, person-centric approach, to identify groups of youth defined by similar patterns of tobacco, alcohol, and drug use. A recent systematic review (16) revealed the following classes: no/low users of any substance (i.e. tobacco, alcohol, and drugs) (largest class ranging from 17–77%), alcohol users (second largest class ranging from 15–80%), and poly-substance users i.e. users of two or more substances in a certain time period (occasional and frequent users ranging from 9–29% and 7–18%, respectively). Several studies included in this review were conducted in national samples of U.S. youth; however, they focused on overall tobacco use or cigarette smoking only (16). Although two recent studies have included non-cigarette tobacco products (17, 18), these studies were limited in the range of tobacco products and drugs assessed, and only one utilized a nationally representative sample (17).
In addition to use patterns, studies have identified higher age, poor academic performance, and greater parental and peer substance use as correlates of poly-substance use (16). Findings for gender and race/ethnicity are mixed (16). Although youth substance use co-occurs with mental health problems (15, 19), few national studies have examined internalizing (i.e., anxiety, depression) and externalizing (i.e., behavioral, conduct) problems as correlates of poly-substance use (16). Additionally, high sensation seeking (20, 21), sexual minorities (22), and residence in rural areas (23) have been associated with poly-substance use; yet, no nationally representative study has collectively examined these correlates.
To advance understanding of poly-substance use among high-school-age youth, the current study used latent class analysis to estimate 1) patterns and 2) correlates (including socio-demographic characteristics, sensation seeking, sexual orientation, residence in urban area, and mental health problems) of poly-substance use across 12 tobacco products, alcohol, marijuana, prescription drugs, and other drugs (cocaine and other stimulants, heroin, inhalants, solvents, and hallucinogens) in a nationally representative sample of U.S. youth ages 15–17 years.
METHODS
Study Design and Population
This study examined Wave 1 (September 2013-December 2014) data of the Population Assessment of Tobacco and Health (PATH) Study, an ongoing longitudinal study of U.S. youth and adults. Of the 6,653 15–17-year-olds recruited at Wave 1, the present analyses were restricted to 6,127 youth with data on covariates of interest. The Wave 1 Restricted-Use Files were accessed at the Inter-university Consortium for Political and Social Research through the National Addiction & HIV Data Archive Program.
Detailed methodological information about the study design and protocol is available elsewhere (24) and at https://doi.org/10.3886/Series606. Briefly, participants were recruited via an address-based, area-probability sampling approach that oversampled adult tobacco users, young adults, and African-American adults. An in-person household screener was used to select youth and adults from households. Generally, up to two youth were sampled per household. The weighting procedures adjusted for oversampling and nonresponse, allowing estimates to be representative of the non-institutionalized, civilian U.S. population (household screener response rate: 54%, weighted response rate among youth: 78.4%). Consent for youth interviews was obtained via written informed consent forms from either parents or emancipated youth and assent from non-emancipated youth. Data were collected using Audio-Computer Assisted Self-Interviews administered in English or Spanish. The study was conducted by Westat and approved by Westat’s Institutional Review Board.
Measures
Tobacco, Alcohol, and Drug Use
Aided by brief descriptions and pictures of each product (except cigarettes), participants self-reported ever using the following tobacco products even one or two puffs/times: cigarettes, e-cigarettes, traditional cigars, cigarillos, filtered cigars, pipe, hookah, smokeless tobacco (i.e. loose snus, moist snuff, dip, spit, or chewing tobacco), snus pouches, kreteks, bidis, and dissolvable tobacco. Participants who reported ever using a tobacco product were asked when they last used the product. Those who reported using in the past 12 months were defined as past 12-month users of that specific tobacco product.
Similarly, participants self-reported ever use of alcohol, marijuana (including blunts), non-prescribed Ritalin® or Adderall® and painkillers, sedatives, or tranquilizers, and cocaine or crack, and other stimulants (i.e. methamphetamine or speed), heroin, inhalants, solvents, and hallucinogens. These items were adapted from the National Epidemiologic Survey on Alcohol and Related Conditions (25) and the National Health and Nutrition Examination Survey (26). ‘Other drug use’ was defined as the use of cocaine or crack, other stimulants (i.e. methamphetamine or speed), heroin, inhalants, solvents, or hallucinogens.
Participants who reported ever using alcohol or drugs were asked how long it has been since last use; those who reported using in the past 12 months were defined as past 12-month users of that substance or class of substances.
Covariates
Socio-demographic characteristics included participants’ age, gender, and race/ethnicity (White non-Hispanic, Black non-Hispanic, Other non-Hispanic, and Hispanic). Additionally, information was collected on participants’ sexual orientation (straight/lesbian/gay/bisexual and something else) and parents/guardians’ highest completed grade or year of school (less than high school, high school diploma or equivalent, some college/technical program, college/technical school/Associate’s degree, and graduate/professional degree/some graduate school) and their child’s school performance in the past 12 months.
Sensation seeking, a risk factor for substance use (27), was assessed via three modified items from the Brief Sensation Seeking Scale. The item “I would like to explore strange places.”, was omitted. Response options for each item were summed to create a mean score (10). The scale is internally consistent among youth in the PATH Study (Cronbach’s α=0.76).
The urban primary sampling unit (PSU) indicator variable was used to define residence as “not urban” if at least 70% of its measure of size for sampling is contributed by counties not belonging to a Core Based Statistical Area (CBSA), and “urban” otherwise (28).
Internalizing and externalizing problems were assessed via modified subscales of the Global Appraisal of Individual Needs - Short Screener (GAIN-SS) (29) and categorized into no/low/moderate (0–3 symptoms) or high (4/4+ symptoms) severity (10). The response option “1+ years ago” for both subscales was modified to “Over a year ago”. The suicidality item in the internalizing problems subscale was omitted.
Analyses
Distributions of covariates, tobacco, alcohol, and drug use were examined. For ease of interpretation, all variables (except sensation seeking) were categorized for analyses.
For the latent class analysis, 17 dichotomous (yes, no) variables were created for past 12-month use of tobacco products, alcohol, and drugs. The optimal number of classes was selected by specifying separate models, beginning with the most parsimonious one-class model and estimating successive models with two to six classes (30). Pearson and likelihood ratio chi-square statistics were examined, with nonsignificant p-values indicating good absolute model fit. Model selection criteria included statistical fit indices such as Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), or sample-size-adjusted BIC. Smaller AIC and BIC values suggest a better model fit. The TECH11 Lo-Mendell-Rubin (LMR) test was also used to assess relative model fit (31). A low p-value rejects the k-1 class model in favor of the k class model. Adequate classification quality was determined by relative entropy and average classification probabilities (ACP). Higher entropy values indicate greater classification accuracy and ACP values close to 1 indicate high certainty and reliability.
Subsequently, the 3-step method was used to examine covariates that predict latent class membership via the AUXILIARY (R3STEP) option (32). In this approach, the first step is a regular latent class analysis using only the latent class indicators; the second step creates the most likely class variable, a nominal variable, using the latent class posterior distribution obtained during the estimation; and step three, the most likely class variable is used as the latent class indicator variable with uncertainty rates prefixed at the probabilities obtained in step 2. All covariates were entered in one model; therefore, each covariate is adjusted for all other covariates.
Distributions were examined using SAS Survey Procedures 9.4. Estimates were weighted to represent the U.S. youth population; variances and Wilson confidence intervals (CIs) were estimated using the balanced repeated replication method (33) with Fay’s adjustment set to 0.3 to increase estimate stability (34). Latent class analyses were conducted in Mplus, version 7.4 with weight, strata, and cluster variables to accommodate the complex sampling design. Two-sided p-values of <.05 were considered statistically significant. Estimates based on fewer than 50 observations in the denominator or the relative standard error greater than 0.30 were suppressed (35). Full Information Maximum Likelihood was used to handle missing data on indicators of the latent variable. However, individuals with missing data on any covariate were deleted from the analysis (n=526).
RESULTS
Past 12-month Tobacco, Alcohol, and Drug Use
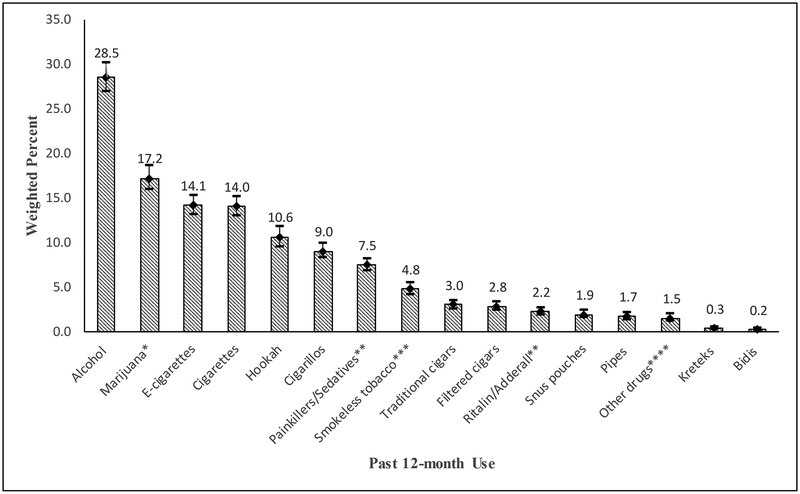
Figure 1 shows the prevalence of past 12-month tobacco, alcohol, and drug use among U.S. youth ages 15–17 years. Approximately 43.5% of youth used at least one substance (i.e. at least one of the 17 tobacco products, alcohol, and drugs) in the past 12 months, and over a quarter (25.6%; 95% CI: 24.1, 27.2; n=1477) used two or more of these 17 substances in the past 12 months (results not shown). Alcohol (28.5%; 95% CI: 26.9, 30.2; n=1695) use was the most prevalent, followed by marijuana (17.2%; 95% CI: 15.9, 18.6; n=1044), e-cigarettes (14.1%; 95% CI: 13.1, 15.3; n=846), and cigarettes (14.0%; 95% CI: 13.0, 15.2; n=851). Hookah and cigarillos were used by 10.6% (95% CI: 9.5, 11.8; n=648) and 9.0% (95% CI: 8.2, 9.9; n=550) of youth, respectively. About 7.5% (95% CI: 6.8, 8.2; n=462) of youth used non-prescribed painkillers/sedatives in the past 12 months.
Figure 1.
Prevalence of Past 12-month Tobacco, Alcohol, and Drug Use among U.S. Youth (15–17 years), Wave 1 (2013–2014) of the Population Assessment of Tobacco and Health (PATH) Study.
* Includes past 12-month use of cigars as blunts.
** Refers to prescription drugs that were not prescribed for the participant or taken only for the experience or feeling they caused.
*** Excludes snus pouches.
**** Includes past 12-month use of cocaine or crack, stimulants (i.e. methamphetamine or speed), heroin, inhalants, solvents, or hallucinogens.
Estimates were weighted to represent the U.S. youth population; variances were estimated using the balanced repeated replication (BRR) method with Fay’s adjustment set to 0.3 to increase estimate stability.
Proportions presented in the column graph are not mutually exclusive.
Estimates with a denominator <50 or a relative standard error >30% were suppressed, therefore proportions for dissolvable tobacco are not shown in the figure.
Latent Classes of Poly-substance Use
Fit statistics are presented in Table 1 for models with 1–6 latent classes. Pearson and likelihood ratio chi-square statistics were not significant for models with 1–6 classes, indicating good absolute model fit. The LMR test was not significant for the 4-class, 5-class, and 6-class models, thus failing to reject the 3-class model in favor of these models. However, the 5-class solution had minimum values on the BIC and sample-size adjusted BIC and acceptable entropy (0.805) and ACP (0.777–0.931). The bootstrap likelihood ratio test (BLRT), the best performing of the likelihood ratio tests (including the LMR), is more consistent at identifying the correct number of classes than the BIC for categorical outcomes (31). However, the BLRT is not available for complex mixture models used in the current study. Therefore, the BIC was relied upon to determine the best model fit. Using the BIC as a guide, the 5-class solution was a better fit than either the 3-class or the 6-class solutions.
Table 1.
Fit Statistics for 1–6 Latent Classes, Wave 1 (2013–2014) of the Population Assessment of Tobacco and Health (PATH) Study.
| Latent Classes | ||||||
|---|---|---|---|---|---|---|
| Tests of Model Fit | 1 | 2 | 3 | 4 | 5 | 6 |
| # free parameters | 17 | 35 | 53 | 71 | 89 | 107 |
| General model fit | ||||||
| Log-likelihood | −22166.131 | −17718.294 | −17280.716 | −17150.655 | −17062.982 | −17013.859 |
| Pearson χ2 | 13927.719 | 12691.798 | 12147.637 | 11807.67 | 11872.673 | 11715.731 |
| df | 130778 | 130951 | 130946 | 130942 | 130936 | 130916 |
| P-value | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Likelihood ratio G2 | 8325.443 | 9108.579 | 8915.121 | 8904.478 | 8878.676 | 8799.383 |
| df | 130778 | 130951 | 130946 | 130942 | 130936 | 130916 |
| P-value | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Incremental model fit | ||||||
| Information Criteria | ||||||
| AIC | 44366.3 | 35506.6 | 34667.4 | 34443.3 | 34304.0 | 34241.7 |
| BIC | 44480.5 | 35741.8 | 35023.6 | 34920.5 | 34902.1 | 34960.8 |
| Sample-size adjusted BIC | 44426.5 | 35630.6 | 34855.2 | 34694.8 | 34619.3 | 34620.8 |
| Lo-Mendell-Rubin test | N/A | 8839.361 | 869.616 | 258.474 | 174.236 | 97.625 |
| P-value | N/A | 0.00 | 0.00 | 0.11 | 0.15 | 0.68 |
| Quality of classification | ||||||
| Entropy | N/A | 0.91 | 0.85 | 0.87 | 0.81 | 0.81 |
| Average class probabilities | 1 | 0.980–0.954 | 0.879–0.959 | 0.809–0.963 | 0.777–0.931 | 0.686–0.933 |
| Average posterior probabilities | 1 | 0.990–0.915 | 0.792–0.986 | 0.719–0.984 | 0.581–0.988 | 0.369–0.984 |
AIC: Akaike information criterion; BIC: Bayesian information criterion
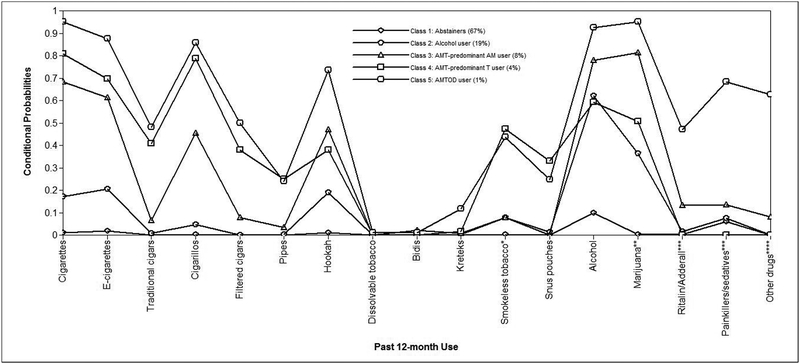
Figure 2 reports the class prevalence and item response probabilities of the 5-class model. Class 1 formed the largest group, ‘abstainers’ (67.3%), with very low probabilities (≤0.1) of using tobacco, alcohol, and drugs. Class 2 comprised the ‘alcohol users’ (19.2%), with a higher probability of using alcohol (0.62) than tobacco products and drugs. Classes 3 and 4 comprised of alcohol, marijuana, and tobacco (AMT) users; however, the two classes differed in the probabilities of endorsement of alcohol and marijuana versus tobacco use. Users in class 3 had higher probabilities of using alcohol (0.78) and marijuana (0.81) than tobacco products (cigarettes (0.68), e-cigarettes (0.61), and other tobacco products (≤0.50)) and were therefore labeled as ‘AMTpredominant AM users’ (8.2%). In contrast, users in class 4 had higher probabilities of using tobacco products (cigarettes (0.81), e-cigarettes (0.70), and cigarillos (0.79)) than alcohol (0.59) and marijuana (0.51). Users in this class also had higher probabilities of using snus pouches (0.33) and smokeless tobacco excluding snus pouches (0.47) compared to any other class. Therefore, class 4 was labeled the ‘AMTpredominant T users’ (3.9%). Class 5 was comprised of ‘alcohol, marijuana, tobacco, and other drug (AMTOD) users’ (1.4%) due to much higher probabilities of using alcohol (0.93), and marijuana (0.95), tobacco products [cigarettes (0.95), e-cigarettes (0.87), cigarillos (0.86), hookah (0.74)], non-prescribed painkillers/sedatives (0.68), and other drugs (0.63) compared to other classes.
Figure 2.
Latent Classes of Past 12-month Poly-substance Use among U.S. Youth (15–17 years), Wave 1 (2013–2014) of the Population Assessment of Tobacco and Health (PATH) Study.
* Excludes snus pouches.
** Includes past 12-month use of cigars as blunts.
*** Refers to prescription drugs that were not prescribed for the participant or taken only for the experience or feeling they caused.
**** Includes past 12-month use of cocaine or crack, stimulants (i.e. methamphetamine or speed), heroin, inhalants, solvents, or hallucinogens.
Latent class analyses were conducted in MPlus, version 7.4 with weight, strata, and cluster variables to accommodate the complex sampling design.
Latent Classes of Poly-substance Use with Covariates
Class 1 was considered the reference class due to low probabilities of tobacco, alcohol, and drug use (Table 2). Adjusting for all other covariates in the model, higher sensation seeking scores, higher age, and lower academic grades were each associated with greater likelihood of membership in all user classes. Compared to females, males had a lower likelihood of membership in class 3 (AOR=0.6; 95% CI: 0.5, 0.8), but a higher likelihood of membership in classes 4 (AOR=4.0; 95% CI: 2.7, 6.1) and 5 (AOR=1.9; 95% CI: 1.0, 3.6) relative to class 1. Compared to non-Hispanic Whites, racial/ethnic minorities had lower likelihood of membership in classes 4 (non-Hispanic Blacks, non-Hispanic other races, and Hispanics) and 5 (non-Hispanic Blacks and Hispanics) versus class 1. The likelihood of membership in class 5 versus class 1 was lower for youth whose parents/guardians had a college degree (AOR=0.4 95% CI: 0.2, 1.0) compared to those with less than high school education. Compared to youth residing in urban PSUs, those in non-urban PSUs had higher odds (AOR=2.2, 95% CI: 1.3, 3.6) of membership in class 4 relative to class 1. Compared to no/low/moderate severity problems, high severity internalizing problems were associated with higher likelihood of membership in classes 2, 3, and 5 versus class 1, whereas high severity externalizing problems were associated with higher likelihood of membership in only classes 3 and 5 versus class 1. Compared to those of straight sexual orientation, those identifying as lesbian, gay, bisexual, or something else had higher likelihood of membership in classes 4 and 5 relative to class 1.
Table 2.
Correlates of Past 12-month Poly-substance Use among U.S. Youth (15–17 years), Wave 1 (2013–2014) of the Population Assessment of Tobacco and Health (PATH) Study.
| Class 2: Alcohol User | Class 3: AMTpredominant AM User | Class 4: AMTpredominant T User | Class 5: AMTOD User | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | ||||||||
| Class proportions | 19.2% | 8.2% | 3.9% | 1.4% | |||||||||||||||
| Mean sensation seeking score* | 1.7 | 1.5 | 1.9 | 0.00 | 2.6 | 2.0 | 3.4 | 0.00 | 2.4 | 1.8 | 3.1 | 0.00 | 3.2 | 2.2 | 4.8 | 0.00 | |||
| Age (years) | |||||||||||||||||||
| 15 | referent | referent | referent | referent | |||||||||||||||
| 16 | 1.6 | 1.3 | 2.0 | 0.00 | 2.3 | 1.5 | 3.5 | 0.00 | 2.3 | 1.4 | 3.7 | 0.00 | 1.8 | 0.7 | 4.4 | 0.19 | |||
| 17 | 2.3 | 1.7 | 3.1 | 0.00 | 5.4 | 3.7 | 7.7 | 0.00 | 4.4 | 2.7 | 7.0 | 0.00 | 5.9 | 3.0 | 11.9 | 0.00 | |||
| Sex | |||||||||||||||||||
| Female | referent | referent | referent | referent | |||||||||||||||
| Male | 1.0 | 0.8 | 1.2 | 0.72 | 0.6 | 0.5 | 0.8 | 0.00 | 4.0 | 2.7 | 6.1 | 0.00 | 1.9 | 1.0 | 3.6 | 0.04 | |||
| Race/ethnicity | |||||||||||||||||||
| White, non-Hispanic | referent | referent | referent | referent | |||||||||||||||
| Black, non-Hispanic | 0.7 | 0.5 | 1.0 | 0.07 | 0.9 | 0.6 | 1.3 | 0.52 | 0.1 | 0.0 | 0.4 | 0.00 | 0.1 | 0.0 | 0.8 | 0.03 | |||
| Other, non-Hispanic** | 0.8 | 0.5 | 1.3 | 0.37 | 0.5 | 0.2 | 1.3 | 0.16 | 0.5 | 0.2 | 1.0 | 0.04 | 1.0 | 0.5 | 2.3 | 0.95 | |||
| Hispanic | 1.0 | 0.7 | 1.3 | 0.91 | 0.9 | 0.6 | 1.3 | 0.55 | 0.3 | 0.2 | 0.6 | 0.00 | 0.4 | 0.2 | 0.9 | 0.03 | |||
| Urban PSU | |||||||||||||||||||
| Urban | |||||||||||||||||||
| Not urban | 1.1 | 0.6 | 2.0 | 0.86 | 0.5 | 0.1 | 1.6 | 0.24 | 2.2 | 1.3 | 3.6 | 0.00 | 0.3 | 0.1 | 1.3 | 0.11 | |||
| Grade | |||||||||||||||||||
| at least some A’s | |||||||||||||||||||
| B’s and C’s | 1.7 | 1.3 | 2.2 | 0.00 | 3.0 | 2.2 | 4.0 | 0.00 | 2.8 | 1.8 | 4.5 | 0.00 | 2.4 | 1.3 | 4.5 | 0.01 | |||
| C’s and D’s | 2.9 | 2.0 | 4.2 | 0.00 | 5.5 | 3.5 | 8.8 | 0.00 | 7.1 | 4.3 | 11.7 | 0.00 | 8.9 | 3.9 | 20.2 | 0.00 | |||
| D’s and F’s | 4.4 | 2.0 | 9.7 | 0.00 | 10.0 | 4.8 | 21.1 | 0.00 | 9.8 | 3.9 | 24.4 | 0.00 | 13.5 | 4.7 | 39.3 | 0.00 | |||
| Parent education | |||||||||||||||||||
| Less than high school | referent | referent | referent | referent | |||||||||||||||
| High school diploma or equivalent | 1.1 | 0.8 | 1.5 | 0.60 | 0.9 | 0.5 | 1.4 | 0.59 | 1.3 | 0.8 | 2.2 | 0.32 | 0.9 | 0.3 | 2.5 | 0.88 | |||
| Some college/technical program | 1.0 | 0.7 | 1.4 | 0.97 | 1.0 | 0.6 | 1.6 | 0.98 | 1.2 | 0.6 | 2.4 | 0.68 | 0.8 | 0.3 | 1.9 | 0.61 | |||
| College/technical school/Associate’s degree | 0.8 | 0.5 | 1.1 | 0.12 | 1.1 | 0.7 | 1.6 | 0.78 | 0.6 | 0.3 | 1.2 | 0.16 | 0.4 | 0.2 | 1.0 | 0.04 | |||
| Graduate/professional degree/some graduate school | 1.0 | 0.6 | 1.7 | 0.95 | 1.0 | 0.6 | 1.9 | 0.93 | 0.8 | 0.3 | 1.8 | 0.55 | 0.8 | 0.3 | 2.2 | 0.73 | |||
| Past-year internalizing problems*** | |||||||||||||||||||
| No/low/moderate severity | referent | referent | referent | referent | |||||||||||||||
| High severity | 2.1 | 1.5 | 3.0 | 0.00 | 2.0 | 1.4 | 2.8 | 0.00 | 1.0 | 0.6 | 1.5 | 0.85 | 2.1 | 1.0 | 4.0 | 0.04 | |||
| Past-year externalizing problems*** | |||||||||||||||||||
| No/low/moderate severity | referent | referent | referent | referent | |||||||||||||||
| High severity | 1.3 | 1.0 | 1.8 | 0.07 | 1.7 | 1.2 | 2.4 | 0.00 | 1.4 | 0.9 | 2.0 | 0.13 | 2.8 | 1.5 | 5.3 | 0.00 | |||
| Sexual orientation | |||||||||||||||||||
| Straight | referent | referent | referent | ||||||||||||||||
| Lesbian, Gay, Bisexual, Something else | 1.4 | 0.9 | 2.1 | 0.17 | 1.5 | 0.9 | 2.4 | 0.12 | 2.6 | 1.3 | 5.2 | 0.01 | 3.9 | 1.9 | 8.2 | 0.00 | |||
Class 1: Abstainers is the referent class.
Measured via the modified Brief Sensation Seeking Scale.
Includes non-Hispanic American Indian/Alaska Natives, Asian/Native Hawaiian/Other Pacific Islanders, or multiple races.
Assessed via the Global Appraisal of Individual Needs-Short Screener (GAIN-SS) subscales,1 categorized into no/low/moderate severity (0–3 symptoms) and high severity (4/≥4 symptoms).
Odds ratios (ORs) and 95% confidence intervals (CIs) from multinomial regression models using the 3-step method to examine covariates that predict latent class membership.
Statistically significant associations at p<.05 indicated in bold text.
Latent class analyses were conducted in MPlus, version 7.4 with weight, strata, and cluster variables to accommodate the complex sampling design.
DISCUSSION
In this nationally representative study, approximately half of U.S. youth ages 15–17 years used at least one tobacco product, alcohol, or drug in the past 12 months. Alcohol use was the most prevalent, followed by marijuana, e-cigarettes, and cigarettes; these findings largely align with other national studies (6). The current study also reports that one out of four youths in this age group used two or more substances, corroborating findings of multiple substance use, especially tobacco products among youth (7). Whether this finding represents substitution for other substances or more extended-range poly-substance use patterns among youth warrants further research.
The multi-class solution reveals several emerging patterns of poly-substance use among U.S. youth ages 15–17 years. Consistent with prior research (16), abstainers (class 1) made up the largest group of youth. Alcohol users (class 2) continued to make up the largest group of youth substance users, reinforcing the need for sustained alcohol prevention strategies for youth below the legal age of drinking in the U.S. This study also revealed three heterogenous poly-substance use classes. Similar to prior studies (16), alcohol, marijuana, and tobacco use was the most common poly-substance use class. However, the two distinct AMT classes observed in this study highlight important nuances in use patterns not observed in prior studies. Whereas class 3 had higher probabilities of alcohol and marijuana use compared to tobacco product use, class 4 had higher probabilities of multiple tobacco product (i.e. cigarettes, e-cigarettes, and cigarillos) use compared to alcohol and marijuana, reflecting the heterogeneity of tobacco products used by youth in the changing tobacco landscape. The AMTOD users (class 5) made up a small proportion of youth, a finding consistent with the literature (15). However, the extended range of substance use in this class, particularly non-prescribed painkillers/sedatives and other drugs (i.e. cocaine or crack, other stimulants, heroin, inhalants, solvents, or hallucinogens) was striking in comparison to other classes, suggesting the need for ongoing monitoring and interventions for substance use behaviors in this group over time.
Our findings confirm age and academic performance as important correlates of youth poly-substance use (16). Findings are also consistent with prior studies on sensation seeking and poly-substance use (20, 21) supporting the desire for intense and novel experiences as an important factor associated with poly-substance use. That older age, lower academic grades, and higher sensation seeking showed a strong and consistent association with all user classes points to these factors as important markers or risk profiles for poly-substance use. Future studies can build on these findings to determine whether traits such as sensation seeking and poor academic performance predict the progression of youth substance use behaviors or whether youth substance use influences personality development and academic engagement.
Sexual orientation also emerged as a significant correlate of poly-substance use, particularly for classes 4 and 5. Consistent with findings from a prior community-based cohort study of U.S. adolescents (22), these findings highlight the need for tailored interventions and policies for sexual orientation minority youth, a group at high risk for poly-substance use. Interestingly, males, non-Hispanic Whites, and those residing in non-urban PSUs were more likely to belong to class 4 (AMTpredominant T). These findings suggest a potential difference in this class as a normative group of users driven by social and environmental factors (15) who may benefit from tailored substance use prevention programs that consider these factors.
Internalizing and externalizing problems were associated with membership in classes 2 (internalizing problems only), 3, and 5, supporting the growing body of literature regarding the concerning comorbidities between substance use and mental health problems among youth (15, 19). While longitudinal analyses can help determine the temporality of these associations across classes, research supporting the effectiveness of integrated or simultaneous treatment for substance use and psychiatric disorders (15) reinforces the need for comprehensive prevention, screening, and treatment efforts to address these comorbidities. Somewhat surprisingly, mental health problems were not associated with membership in class 4, revealing a previously unreported complexity that the association between mental health and poly-substance use does not hold across all types of polysubstance users. This class was characterized by higher use of smokeless tobacco compared to other classes. Poly-tobacco use is common among smokeless tobacco users and factors associated with membership in this class (i.e. male gender, non-Hispanic White race/ethnicity, and residence in nonurban areas) are consistent with those associated with smokeless tobacco use (36, 37). Furthermore, our findings are consistent with a recent PATH Study finding that neither internalizing nor externalizing problems were associated with onset of smokeless tobacco use. Although low statistical power cannot be ruled out as a possible explanation, future studies should explore why individuals with mental health problems do not appear to be drawn to smokeless tobacco products.
This study’s strengths include its nationally representative sample of U.S. youth, assessment of a wide range of tobacco products, alcohol, and drugs, as well as inclusion of personality (sensation seeking), residence in urban area, sexual orientation, and mental health correlates of poly-substance use. However, factors such as differences in sampling frames and timing of tobacco and substance use assessments limit the comparison of findings with prior studies. Although we did not use recent (i.e. past 30-day) use to identify the latent classes, past 12-month use measures ensured sufficient cell sizes and statistical power for our analyses. Because the PATH Study does not include a measure of SUD, we were unable to examine SUDs directly. However, future studies can examine transitions in latent classes and risk for substance use problems via the GAIN-SS, which has been shown to be an indicator of SUD (29). Finally, temporality cannot be determined due to the cross-sectional analyses in this study. While a prior PATH Study paper demonstrated bidirectional longitudinal associations between tobacco use and other substance use between Waves 1 and 2 among youth (11), the current study’s identification of patterns of contemporaneous use across tobacco and other substances among youth suggests that future studies incorporate polysubstance use in definitions of substance use. Furthermore, findings from this Wave 1 analysis establish baseline poly-substance use and longitudinal data from future waves will allow the examination of transitions in poly-substance use patterns and risk factors of poly-substance use among U.S. youth.
In summary, this nationally representative study revealed distinct poly-substance use patterns among U.S. youth ages 15–17 years. Findings point to youth poly-substance users as a sub-group with greater use of emerging tobacco products, marijuana and other drugs. Correlates of substance use included higher sensation seeking, poor academic performance, residence in urban area, minority sexual orientation, and mental health problems. Given the changing tobacco and substance-use landscape with respect to availability, use of emerging products, and regulatory environments, youth poly-substance use patterns are likely to shift over time. The heterogeneous patterns identified in this study support the need for ongoing research to inform targeted prevention strategies. Additionally, effective and resource-efficient interventions are needed for youth engaging in multiple substance use, particularly those with identified mental health concerns and poor school performance.
Supplementary Material
Acknowledgements
The Population Assessment of Tobacco and Health (PATH) Study is supported with Federal funds from the National Institute on Drug Abuse (NIDA), NIH, and the Food and Drug Administration (FDA), HHS, under a contract to Westat (Contract No. HHSN271201100027C). Staff from the NIDA and the FDA contributed to the design, conduct, and management of the PATH Study. The NIDA and the FDA were not directly involved in the collection of study data. No funding was provided specifically for conducting the analysis, drafting the manuscript, or submitting this paper for publication. This article was prepared while Dr. Kevin Conway was employed at the NIDA, NIH, Bethesda, MD. The views and opinions expressed in this manuscript are those of the authors only and do not necessarily represent the views, official policy or position of HHS or any of its affiliated institutions or agencies. Ms. Victoria Green is currently employed as an Analyst in Health Policy by the Congressional Research Service (CRS). This paper was prepared prior to her employment with CRS. The views expressed herein are those of the author and are not presented as those of the Congressional Research Service or the Library of Congress.
Footnotes
Declaration of Interests: None.
References
- 1.National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General, Atlanta (GA): Centers for Disease Control and Prevention (US); 2012. [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services (HHS), Office of the Surgeon General. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health, Washington, DC: HHS; 2016. [PubMed] [Google Scholar]
- 3.Degenhardt L, Stockings E, Patton G, Hall WD, Lynskey M The increasing global health priority of substance use in young people, The lancet Psychiatry 2016: 3: 251–264. [DOI] [PubMed] [Google Scholar]
- 4.Kasza KA, Ambrose BK, Conway KP, Borek N, Taylor K, Goniewicz ML et al. Tobacco-Product Use by Adults and Youths in the United States in 2013 and 2014, N Engl J Med 2017: 376: 342–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jamal A, Gentzke A, Hu SS, Cullen KA, Apelberg BJ, Homa DM et al. Tobacco Use Among Middle and High School Students - United States, 2011–2016, MMWR Morb Mortal Wkly Rep 2017: 66: 597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE Monitoring the Future national survey results on drug use, 1975–2016: Overview, key findings on adolescent drug use, Ann Arbor: Institute for Social Research, The University of Michigan; 2017. [Google Scholar]
- 7.Harrell PT, Naqvi SM, Plunk AD, Ji M, Martins SS Patterns of youth tobacco and polytobacco usage: The shift to alternative tobacco products, The American journal of drug and alcohol abuse 2016: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richter L, Pugh BS, Smith PH, Ball SA The co-occurrence of nicotine and other substance use and addiction among youth and adults in the United States: implications for research, practice, and policy, The American journal of drug and alcohol abuse 2017: 43: 132–145. [DOI] [PubMed] [Google Scholar]
- 9.Creamer MR, Portillo GV, Clendennen SL, Perry CL Is Adolescent Poly-tobacco Use Associated with Alcohol and Other Drug Use?, Am J Health Behav 2016: 40: 117–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Conway KP, Green VR, Kasza KA, Silveira ML, Borek N, Kimmel HL et al. Co-occurrence of tobacco product use, substance use, and mental health problems among youth: Findings from wave 1 (2013–2014) of the population assessment of tobacco and health (PATH) study, Addict Behav 2017: 76: 208–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Silveira ML, Conway KP, Green VR, Kasza KA, Sargent JD, Borek N et al. Longitudinal associations between youth tobacco and substance use in waves 1 and 2 of the Population Assessment of Tobacco and Health (PATH) Study, Drug and alcohol dependence 2018: 191: 25–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Register CA, Williams DR, Grimes PW Adolescent drug use and educational attainment, Educ Econ 2001: 9: 1–18. [Google Scholar]
- 13.Fernandez-Serrano MJ, Perez-Garcia M, Verdejo-Garcia A What are the specific vs. generalized effects of drugs of abuse on neuropsychological performance?, Neurosci Biobehav Rev 2011: 35: 377–406. [DOI] [PubMed] [Google Scholar]
- 14.Guilamo-Ramos V, Litardo HA, Jaccard J Prevention programs for reducing adolescent problem behaviors: Implications of the co-occurrence of problem behaviors in adolescence, J Adolesc Health 2005: 36: 82–86. [DOI] [PubMed] [Google Scholar]
- 15.Connor JP, Gullo MJ, White A, Kelly AB Polysubstance use: diagnostic challenges, patterns of use and health, Curr Opin Psychiatry 2014: 27: 269–275. [DOI] [PubMed] [Google Scholar]
- 16.Tomczyk S, Isensee B, Hanewinkel R Latent classes of polysubstance use among adolescents-a systematic review, Drug and alcohol dependence 2016: 160: 12–29. [DOI] [PubMed] [Google Scholar]
- 17.Miech RA, O’Malley PM, Johnston LD, Patrick ME E-Cigarettes and the Drug Use Patterns of Adolescents, Nicotine Tob Res 2016: 18: 654–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morean ME, Kong G, Camenga DR, Cavallo DA, Simon P, Krishnan-Sarin S Latent class analysis of current e-cigarette and other substance use in high school students, Drug Alcohol Depend 2016: 161: 292–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robinson ZD, Riggs PD Cooccurring Psychiatric and Substance Use Disorders, Child Adolesc Psychiatr Clin N Am 2016: 25: 713–722. [DOI] [PubMed] [Google Scholar]
- 20.Malmberg M, Overbeek G, Monshouwer K, Lammers J, Vollebergh WA, Engels RC Substance use risk profiles and associations with early substance use in adolescence, J Behav Med 2010: 33: 474–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Derefinko KJ, Charnigo RJ, Peters JR, Adams ZW, Milich R, Lynam DR Substance Use Trajectories From Early Adolescence Through the Transition to College, J Stud Alcohol Drugs 2016: 77: 924–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kecojevic A, Jun HJ, Reisner SL, Corliss HL Concurrent polysubstance use in a longitudinal study of US youth: associations with sexual orientation, Addiction 2017: 112: 614–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lambert D, Gale JA, Hartley D Substance abuse by youth and young adults in rural America, J Rural Health 2008: 24: 221–228. [DOI] [PubMed] [Google Scholar]
- 24.Hyland A, Ambrose BK, Conway KP, Borek N, Lambert E, Carusi C et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study, Tob Control 2017: 26: 371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Instiutes of Health (NIH). National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). In: National Institute on Alcohol Abuse and Alcoholism (NIAAA), editor, Rockville, MD; 2004–2005. [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC). National Health and Nutrition Examination Survey Questionnaire (NHANES). In: National Center for Health Statistics, editor, Hyattsville, MD,; 2011–2012. [Google Scholar]
- 27.Hoyle RH, Stephenson MT, Palmgreen P, Lorch EP, Donohew RL Reliability and validity of a brief measure of sensation seeking, Pers Individ Dif 2002: 32: 401–414. [Google Scholar]
- 28.Roberts ME, Doogan NJ, Stanton CA, Quisenberry AJ, Villanti AC, Gaalema DE et al. Rural Versus Urban Use of Traditional and Emerging Tobacco Products in the United States, 2013–2014, Am J Public Health 2017: 107: 1554–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dennis ML, Chan YF, Funk RR Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults, Am J Addict 2006: 15 Suppl 1: 80–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Collins LM, Lanza ST Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences: John Wiley & Sons; 2013. [Google Scholar]
- 31.Nylund K, Asparouhov T, Muthén B Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study, Structural Equation Modeling 2007: 14: 535–569. [Google Scholar]
- 32.Asparouhov T, Muthén B Auxiliary Variables in Mixture Modeling: Three-Step Approaches Using Mplus, Struct Equ Modeling 2014: 21: 329–341. [Google Scholar]
- 33.McCarthy PJ Pseudoreplication: further evaluation and applications of the balanced half-sample technique, Vital Health Stat 2 1969: 1–24. [PubMed] [Google Scholar]
- 34.Judkins DR Fay’s method for variance estimation, J Off Stat 1990: 6: 223–239. [Google Scholar]
- 35.Klein RJ, Proctor SE, Boudreault MA, Turczyn KM Healthy People 2010 criteria for data suppression, Healthy People 2010 statistical notes : from the Centers for Disease Control and Prevention/National Center for Health Statistics 2002: 1–12. [PubMed] [Google Scholar]
- 36.Cheng YC, Rostron BL, Day HR, Stanton CA, Hull LC, Persoskie A et al. Patterns of Use of Smokeless Tobacco in US Adults, 2013–2014, Am J Public Health 2017: 107: 1508–1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vander Weg MW, Cunningham CL, Howren MB, Cai X Tobacco use and exposure in rural areas: Findings from the Behavioral Risk Factor Surveillance System, Addictive behaviors 2011: 36: 231–236. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.