Abstract
Background
There is increased emphasis on efficiently administering patient-reported outcome measures (PROMs). The International Hip Outcome Tool-12 (iHOT-12) is a short-form version of the iHOT-33, and relatively little is known about clinically significant outcomes using the iHOT-12.
Questions/Purposes
The purpose of this study was to define minimal clinically important difference (MCID) and patient acceptable symptomatic state (PASS) for the iHOT-12 and to identify predictors for achieving these psychometric end points in patients undergoing arthroscopic treatment of femoroacetabular impingement (FAI).
Methods
Data was prospectively collected and retrospectively analyzed as part of an institutional hip preservation repository. One hundred and twenty patients were included; mean age and body mass index (BMI) were 38.7 years and 25.9, respectively. A majority of patients were female (67.5%) and white (81.7%) and participated in recreational sports (79.2%). The iHOT-12 was administered pre-operatively and at 1-year follow-up to patients undergoing primary hip arthroscopy for FAI. The following anchor question was also asked at 1-year follow-up: “Taking into account all the activities you have during your daily life, your level of pain, and also your functional impairment, do you consider that your current state is satisfactory?” MCID was calculated using a distribution-based method. Receiver-operating characteristic analysis with area under the curve was used to confirm the significance of the PASS threshold.
Results
Mean iHOT-12 scores improved from 35.6 at pre-operative assessment to 70.7 at 1-year follow-up. Patients indicating satisfaction with their outcome improved from 37.5 pre-operatively to 79.0 at 1-year follow-up. MCID value for the iHOT-12 was 13.0. The PASS threshold was 63.0, indicating an excellent predictive value that patients scoring above this threshold were likely to have met an acceptable symptom state. Worker’s compensation patients and those with increased BMI were less likely to achieve PASS; lower pre-operative iHOT-12 score was predictive for achieving MCID, and achieving MCID was predictive for achieving PASS.
Conclusion
This is the first study to define PASS and MCID for the iHOT-12, which measures clinically significant outcome improvement comparably to that of other commonly used hip PROMs. As its use becomes more widespread, the iHOT-12 data-points presented in this study can be used to determine clinically significant improvement of patient-reported outcomes.
Electronic supplementary material
The online version of this article (10.1007/s11420-018-9646-0) contains supplementary material, which is available to authorized users.
Keywords: hip, femoroacetabular impingement, MCID, PASS, patient-reported outcome measures (PROMs)
Introduction
Femoroacetabular impingement (FAI) refers to an atypical anatomic relationship involving the acetabulum and/or the femoral head-neck junction within the hip [1]. It is caused by bony deformities or spatial incongruence that can lead to pathologic contact and shearing forces at the acetabular labrum during normal hip motion [8]. These forces can lead to cartilage wear and progression to hip osteoarthritis. Arthroscopic surgery has become the mainstay of treatment for symptomatic FAI, with a significant increase in the number of elective hip arthroscopic procedures seen in the past decade [3, 10, 11, 14, 19]. Patient-reported outcome measures (PROMs) are the most common method for reporting outcomes after orthopedic procedures. In hip arthroscopic surgery, the Hip Outcome Score (HOS), the modified Harris Hip Score (mHHS), and the International Hip Outcome Tool-33 (iHOT-33) are the most commonly used, and the iHOT-33 has been validated as a reliable measure of functional and quality-of-life outcomes [13].
Although PROMs are increasingly reported in orthopedic surgery, there is still a need to improve the quality of outcome reporting. A prior review noted that few studies use clinically significant outcome parameters to quantify the degree of outcome improvement [20]. Previously reported measures of clinically significant outcome for arthroscopic hip surgery include minimal clinically important difference (MCID) [18], patient acceptable symptomatic state (PASS) [4], and substantial clinical benefit (SCB) [16]. MCID is defined as the “the smallest difference which patients perceive as beneficial and which would mandate, in the absence of troublesome side effects and excessive cost, a change in the patient’s management” [21]. Thus, MCID is the smallest change in a measurement that indicates an important improvement or worsening in a symptom [12]. SCB is defined as the upper threshold of outcome improvement that a patient must achieve in order to feel substantially better [16]. In addition to MCID and SCB, PASS has been adopted as a measure of clinical significance capable of discriminating between feeling acceptably well and unacceptably unwell [20]. PASS is thus considered the minimum score required for a patient to feel well and goes beyond what is minimally detectable (MCID).
With no clear consensus on preferred PROMs, a variety of hip PROMs are employed to grade outcomes of arthroscopic hip surgery. Each offers certain advantages, and some authors have suggested that the iHOT-33 is the most sensitive tool for measuring outcome improvement while also exhibiting minimal ceiling effect [16]. To reduce patient burden and administrative effort, a short version of the iHOT-33, known as the iHOT-12, was developed [6]. The iHOT-12 has shown excellent agreement with the longer i-HOT-33 and comparable sensitivity to change [6]. While the iHOT-12 has been validated as a useful tool, most of the evidence has focused on statistically significant differences between groups rather than clinically significant differences. Specifically, the MCID and PASS have yet to be defined for the iHOT-12. The purpose of this study was to define MCID and PASS for the iHOT-12 and to identify predictors for achieving these psychometric end points. We hypothesized that MCID and PASS for the iHOT-12 would be comparable to those of other commonly used hip PROMs.
Methods
This study was approved by the institutional review board at Rush University. Data was prospectively collected and retrospectively analyzed as part of an institutional hip preservation repository. All patients undergoing primary hip arthroscopy for the treatment of FAI syndrome (FAIS) between January 1, 2012 (the initiation of the repository), and June 25, 2012, for the treatment of FAIS by a single, fellowship-trained surgeon were eligible for inclusion. Inclusion criteria consisted of clinical and radiographic diagnosis of symptomatic FAIS, failure of non-operative management (including physical therapy, activity modification, oral anti-inflammatories, and for some patients fluoroscopically guided intra-articular cortisone injection); and hip arthroscopy performed to address the FAIS, with completion of pre-operative and 1-year follow-up for iHOT-12 (Appendix Table 5). All arthroscopic procedures were performed by the senior author with the patient under general anesthesia in the supine position on a standard traction table using previously described surgical technique [5]. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist was used.
Table 5.
The International Hip Outcome Tool-12 (iHOT-12) Survey
| Question | Scale | |
|---|---|---|
| Overall, how much pain do you have in your hip/groin? | Extreme pain | No pain at all |
| How difficult is it for you to get up and down off the floor/ground? | Extremely difficult | Not difficult at all |
| How difficult is it for you to walk long distances? | Extremely difficult | Not difficult at all |
| How much trouble do you have with grinding, catching, or clicking in your hip? | Severe trouble | No trouble at all |
| How much trouble do you have pushing, pulling, lifting, or carrying heavy objects? | Severe trouble | No trouble at all |
| How concerned are you about cutting/changing directions during your sport or recreational activities? | Extremely concerned | Not concerned at all |
| How much pain do you experience in your hip after activity? | Extreme pain | No pain at all |
| How concerned are you about picking up or carrying children because of your hip? | Extremely concerned | Not concerned at all |
| How much trouble do you have with sexual activity because of your hip? | Severe trouble | No trouble at all |
| How much of the time are you aware of the disability in your hip? | Constantly aware | Not aware at all |
| How concerned are you about your ability to maintain your desired fitness level? | Extremely concerned | Not concerned at all |
| How much of a distraction is your hip problem? | Extreme distraction | No distraction at all |
One hundred and twenty patients met the inclusion criteria. Mean age and body mass index (BMI) were 38.7 (SD ± 11.8) years and 25.9 (SD ± 5.1) kg/m2, respectively. The majority of patients were female (n = 81, 67%) and white (n = 98, 81.7%) and participated in recreational sports (n = 95, 79.2%). Mean radiographic measurements for pre-operative alpha angle and lateral center-edge angle of Wiberg (LCEA) were 62.3° (SD ± 9.6) and 33.4° (SD ± 17.9), respectively (Table 1).
Table 1.
Demographics of cohort
| Demographic | N/mean |
|---|---|
| Total | 120 |
| Female (%) | 81 (67.5%) |
| Age at surgerya | 38.7 ± 11.7 |
| Body mass indexa | 25.9 ± 5.1 |
| Race and ethnicity | |
| White | 98 (81.7%) |
| African American | 8 (6.7%) |
| Hispanic | 5 (4.2%) |
| Other | 2 (1.7%) |
| Worker’s compensation | |
| No | 112 (93.3%) |
| Yes | 6 (5%) |
| Sports/physical level of competition | |
| None | 18 (15%) |
| Recreational | 95 (79.2%) |
| High school | 3 (3%) |
| College | 2 (1.7%) |
| Professional | 1 (0.8%) |
| Alpha anglea | 62.3 ± 9.6 |
| Lateral center-edge anglea | 33.4 ± 6.8 |
| Tönnis grade | |
| 0 | 93 (77.5%) |
| 1 | 6 (5.0%) |
aReported in mean ± standard deviation
All patients received a series of pre-operative radiographs consisting of a standing anteroposterior (AP) pelvis radiograph, an AP hip radiograph, a false-profile hip radiograph, and a Dunn lateral hip radiograph. The joint-space width was measured in three positions on the AP hip radiograph, as was the LCEA. Alpha angle was measured on the Dunn lateral view of the hip. The Tönnis grade was determined.
Patients enrolled in the registry complete PROMs, which are delivered pre-operatively and at 1-year follow-up assessment. In addition to PROMs, patients respond to the following anchor question at 1-year follow-up: “Taking into account all the activities you have during your daily life, your level of pain, and also your functional impairment, do you consider that your current state is satisfactory?” Patients can answer “yes” or “no.”
Numerous models exist to calculate MCID and PASS, two of which are distribution and anchor methods [9, 22]. Within distribution-based models, statistical analyses calculate changes in outcome that represent the minimal clinically significant change occurring beyond expected variance or error [17]. Prior investigations have demonstrated that half the standard deviation of outcome scores for a given instrument can reliably determine MCID [7, 15]. Within anchor-based models, patients answer an “anchor” question, based upon their global function, pain, or satisfaction. Anchor questions seek to ascertain patient-perceived improvement. Anchor responses are then compared to outcome scores to determine values for MCID or PASS, respectively.
In this study, MCID was calculated using a distribution-based method. PASS was calculated using a distribution-based method while a non-parametric receiver-operating characteristic (ROC) analysis with area under the curve was used to confirm the significance of the PASS threshold. Post-operative outcome score means between the “satisfactory” and “non-satisfactory” groups were compared with ROC analysis to identify a mean post-operative score that significantly differentiated the two groups; this score was defined as the absolute post-operative PASS value. In order to determine the validity of identified threshold values for predicting a patient’s likelihood to achieve PASS (strength of association), an area under the curve (AUC) of ROC analysis was performed. Based on prior evidence, the strength of association was considered “acceptable” for AUC of more than 0.7 and “excellent” for AUC of more than 0.8 [2].
To determine factors associated with and predictive of MCID/PASS, separate analyses were conducted. Univariate analyses were performed, and multivariable logistic models were fitted to determine which patient factors and clinical characteristics are associated with achieving MCID and PASS. Variables used in univariate and regression analyses included age, sex, BMI, ethnicity, worker’s compensation status, alpha angle, LCEA, Tönnis grade, labral treatment (repair vs. debridement), acetabular/femoral osteoplasty, and level of sports participation. Additionally, pre-operative outcome score was controlled for in regression analyses. Significance was set at a p value of less than 0.05. Analyses were performed using SAS software, version 9.3 (SAS Institute, Cary, NC, USA).
Results
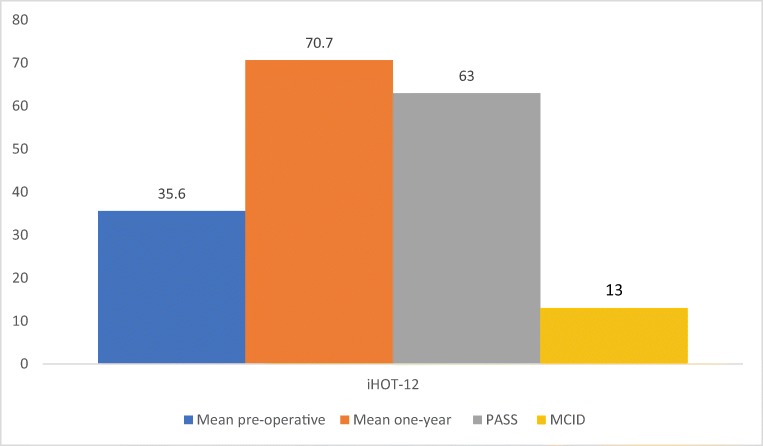
Mean outcome score for the iHOT-12 showed statistically significant improvement from 35.6 (SD ± 17.9) at pre-operative baseline to 70.7 ± 5.1 at 1-year follow-up (p < 0.001) (Fig. 1). Seventy-six of the 120 (63.3%) patients provided responses to the anchor question at 1-year follow-up, and 74% reported that they were satisfied with their current state. Patients indicating that their current state was satisfactory improved from mean baseline iHOT-12 score of 37.5 (SD ± 17.4) to 79.0 (SD ± 16.4) at 1-year follow-up.
Fig. 1.
Comparison of pre-operative, post-operative, patient acceptable symptomatic state (PASS), and minimal clinically important difference (MCID) values for the international Hip Outcome Tool-12 (iHOT-12).
The MCID for the IHOT-12 was 13.0. A 1-year post-operative iHOT-12 absolute score of 63 (AUC 0.93) significantly corresponded to PASS. Based on the AUC score, the identified value has an excellent predictive value that patients scoring above this threshold are likely to have met a minimum acceptable symptom state.
In univariate analysis for MCID, no clinical or demographic factor was significantly predictive of achieving MCID (Table 2). However, in logistic regression analysis, patients with higher pre-operative iHOT-12 scores were significantly less likely to achieve MCID (OR 0.95; 0.93–0.98) (Table 3).
Table 2.
Univariate analysis for minimal clinically important difference (MCID)
| Predictor | Odds ratio | Lower 95% CI | Upper 95% CI | p value |
|---|---|---|---|---|
| Age | 1.00 | 0.96 | 1.04 | 0.894 |
| Sex (female vs. male) | 1.73 | 0.71 | 4.23 | 0.230 |
| Body mass index | 0.97 | 0.89 | 1.06 | 0.546 |
| Race/ethnicity (white vs. non-white) | 0.52 | 0.09 | 3.04 | 0.468 |
| Worker’s compensation (yes vs. no) | 0.26 | 0.05 | 1.37 | 0.111 |
| Alpha angle | 0.99 | 0.94 | 1.04 | 0.619 |
| Lateral center-edge angle | 0.96 | 0.90 | 1.02 | 0.177 |
| Tönnis grade (1 vs. 0) | > 999.99 | < 0.001 | > 999.99 | 0.973 |
| Labral repair (yes vs. no) | 0.26 | 0.04 | 1.97 | 0.194 |
| Acetabular rim trimming (yes vs. no) | 1.12 | 0.12 | 10.51 | 0.919 |
| Cleared to return to sport (yes vs. no) | 1.29 | 0.52 | 3.22 | 0.570 |
| Sport level of competition (Ref: recreational) | ||||
| None | 0.61 | 0.19 | 1.92 | 0.397 |
| High school | 0.12 | 0.01 | 1.36 | 0.087 |
| College | > 999.99 | < 0.001 | > 999.99 | 0.978 |
| Professional | < 0.001 | < 0.001 | > 999.99 | 0.985 |
Table 3.
Logistic regression analysis for minimal clinically important difference (MCID) and patient acceptable symptomatic state (PASS)
| Predictor | Odds ratio | Lower 95% CI | Upper 95% CI | p value | Model AUC |
|---|---|---|---|---|---|
| MCID | |||||
| Age | 0.97 | 0.93 | 1.01 | 0.195 | 0.71 |
| Sex (male vs. female) | 1.54 | 0.58 | 3.98 | 0.376 | |
| Pre-op. iHOT-12 score | 0.95 | 0.93 | 0.98 | 0.001 | |
| PASS | |||||
| Age | 0.99 | 0.95 | 1.03 | 0.502 | 0.76 |
| Sex (male vs. female) | 0.64 | 0.22 | 1.68 | 0.383 | |
| MCID achieved vs. not achieved | 17.09 | 5.94 | 59.02 | < 0.0001 | |
AUC area under the curve, iHOT-12 International Hip Outcome Tool-12
In univariate analysis for PASS, patients with worker’s compensation status (OR 0.1; 0.01–0.84) and increased BMI (OR 0.92; 0.85–1.00) were less likely to achieve PASS (Table 4). In multivariable analysis, however, lower pre-operative iHOT-12 score was predictive of achieving MCID, and achieving MCID was predictive of achieving PASS (p < 0.0001 for both), after adjusting for age and sex (Table 3).
Table 4.
Univariate analysis for patient acceptable symptomatic state (PASS)
| Predictor | Odds ratio | Lower 95% CI | Upper 95% CI | p value |
|---|---|---|---|---|
| Age | 0.99 | 0.96 | 1.02 | 0.511 |
| Sex (female vs. male) | 0.95 | 0.42 | 2.12 | 0.894 |
| Body mass index | 0.92 | 0.85 | 1.00 | 0.047 |
| Race/ethnicity (white vs. non-white) | 0.41 | 0.08 | 2.13 | 0.287 |
| Worker’s compensation (yes vs. no) | 0.10 | 0.01 | 0.84 | 0.034 |
| Alpha angle | 0.98 | 0.94 | 1.02 | 0.365 |
| Lateral center-edge angle | 1.00 | 0.94 | 1.06 | 0.953 |
| Tönnis grade (1 vs. 0) | > 999.99 | < 0.001 | > 999.99 | 0.968 |
| Labral repair (yes vs. no) | 0.17 | 0.02 | 1.64 | 0.124 |
| Acetabular rim trimming (yes vs. no) | 0.78 | 0.13 | 4.87 | 0.790 |
| Cleared to return to sport (yes vs. no) | 1.50 | 0.68 | 3.32 | 0.318 |
| Sport level of competition (Ref: recreational) | ||||
| None | 0.35 | 0.13 | 0.98 | 0.046 |
| High school | 0.88 | 0.08 | 10.08 | 0.917 |
| College | > 999.99 | < 0.001 | > 999.99 | 0.982 |
| Professional | < 0.001 | < 0.001 | > 999.99 | 0.986 |
Discussion
In this study, we defined MCID and PASS for the iHOT-12 after arthroscopic FAI surgery. We found that a 13-point increase on the iHOT-12 is representative of MCID, while attaining an absolute post-operative score of 63 constitutes PASS. Although increased BMI and worker’s compensation status were predictive of not achieving PASS, in multivariable analysis, only pre-operative outcome score was predictive of achieving MCID, and achieving MCID was predictive of achieving PASS. Our study findings provide useful reference values as clinicians and researchers increasingly utilize the iHOT-12.
This study has several limitations. Our anchor question was administered at 1-year follow-up, and we are thus able to comment only on clinically significant outcome improvement by this point in time. It is possible that clinically significant outcome improvement continues to occur beyond the 1-year point, and this may change the magnitude of our MCID and PASS values. Additionally, we are limited in our methodology and reporting by the use of our anchor question, which was administered with a goal to elicit PASS. Different anchor questions are required in order to calculate SCB and an anchor-based MCID (we used a distribution-based MCID). Furthermore, our study is limited by the predominantly female population, the low response rate for the PASS anchor question (63.3%), and the use of a single fellowship-trained hip surgeon at a high-volume institution; therefore, our findings have limited generalizability.
Interest has increased in understanding clinically significant outcome improvement after arthroscopic treatment of FAI [4, 16–18]. Chahal et al. [4] derived PASS on the mHHS and the HOS after arthroscopic FAI treatment. Based on analysis of 130 patients, the authors found that at 1 year after surgery, PASS values were 74 (mHHS), 87 (HOS-activities of daily living subscale), and 75 (HOS-sports subscale). To our knowledge, PASS has yet to be described for the iHOT. The present study builds on the work by Chahal et al. by also describing PASS values for the iHOT-12. Notably, we found that the PASS value for the iHOT-12 (63) was lower than previously reported values for the mHHS and the HOS. This finding is consistent with prior psychometric analyses that have demonstrated lower threshold values and limited ceiling effects for the iHOT-33 [16, 17]. MCID has also been previously derived for arthroscopic FAI surgery. Nwachukwu et al. [18] derived MCID values for the mHHS, iHOT-33, and HOS based on 364 patients who underwent arthroscopic FAI surgery. In their study, the MCID for the mHHS, HOS-Activities of Daily Living (HOS-ADL), HOS-Sports, and iHOT-33 was 8.2, 8.3, 14.5, and 12.1, respectively. In the present study, the derived MCID on the iHOT-12 was 13.0 and is comparable to the values previously reported by Nwachukwu et al. [18]. Given the similarities to previously reported values for MCID and PASS, our study supports the use of the iHOT-12 for assessing clinically significant outcome change.
As part of our secondary analyses, we found that achieving MCID was predictive of achieving PASS, suggesting that patients able to achieve a detectable change are also likely to achieve a well state. We also found that pre-operative outcome score was predictive of achieving MCID. This relationship between baseline patient-reported outcome and the degree of outcome improvement has been previously demonstrated [16–18] and is likely explained by the increased capability of patients with low baseline outcome scores to achieve a clinically significant delta in outcome score. Interestingly, Chahal et al. [4] noted a contrasting relationship, wherein patients with higher baseline scores were more likely to achieve PASS. We propose that for patients with higher baseline scores with limited capacity for MCID delta, PASS may represent a more appropriate measure of clinically significant outcome. As part of our univariate analysis, we also found that patients with worker’s compensation status and increased BMI were less likely to achieve PASS. These variables lost significance in our logistic regression analyses when we tested for clinical/demographic variables, as well as pre-operative baseline outcome scores. It is possible that we were underpowered to detect a difference once multiple variables were controlled or that the demonstrated association for worker’s compensation status and BMI was confounded by baseline outcome score.
In conclusion, the iHOT-12 measures clinically significant outcome improvement that is comparable to that of other commonly used hip PROMs. Achieving MCID is predictive for achieving PASS, and patients with lower pre-operative outcome scores are most likely to achieve MCID. As use of the iHOT-12 spreads, the data presented in this study can be used to determine clinically significant patient reported improvement.
Electronic supplementary material
(PDF 2046 kb)
Appendix
Compliance with Ethical Standards
Conflict of Interest:
Benedict U. Nwachukwu, MD, Brenda Chang, MPH, Edward C. Beck, MPH, William H. Neal, BS, and Kamran Movassaghi, MD, declare that they have no conflicts of interest. Shane J. Nho, MD, MS, reports research support from Allosource, Arthrex, Inc., Athletico, DJ Orthopedics, Linvatec, Miomed, Smith & Nephew, and Stryker; editorial board membership from American Journal of Orthopedics; board or committee membership from American Orthopaedic Society for Sports Medicine and Arthroscopy Association of North America; personal fees from Ossur; and publishing royalties from Springer, outside the submitted work. Anil S. Ranawat, MD, reports personal fees from Arthrex, Smith & Nephew, and Stryker, outside the submitted work.
Human/Animal Rights:
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent:
Informed consent was waived from all patients included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level IV: Case Series.
References
- 1.Beck M, et al. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 2.Berliner JL, et al. John Charnley Award: preoperative patient-reported outcome measures predict clinically meaningful improvement in function after THA. Clin Orthop Relat Res. 2016;474(2):321–329. doi: 10.1007/s11999-015-4350-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement in athletes. Am J Sports Med. 2011;39(Suppl):7S–13S. doi: 10.1177/0363546511404144. [DOI] [PubMed] [Google Scholar]
- 4.Chahal J, et al. The patient acceptable symptomatic state for the modified Harris Hip Score and Hip Outcome Score among patients undergoing surgical treatment for femoroacetabular impingement. Am J Sports Med. 2015;43(8):1844–1849. doi: 10.1177/0363546515587739. [DOI] [PubMed] [Google Scholar]
- 5.Frank RM, et al. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42(11):2634–2642. doi: 10.1177/0363546514548017. [DOI] [PubMed] [Google Scholar]
- 6.Griffin DR, et al. A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy. 2012;28(5):611–6. doi: 10.1016/j.arthro.2012.02.027. [DOI] [PubMed] [Google Scholar]
- 7.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(4):407–15. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- 8.Jamali AA, et al. Management of incarcerating pincer-type femoroacetabular impingement with hip arthroscopy. Arthrosc Tech. 2014;3(1):e155–60. doi: 10.1016/j.eats.2013.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Katz NP, Paillard FC, Ekman E. Determining the clinical importance of treatment benefits for interventions for painful orthopedic conditions. J Orthop Surg Res. 2015;10:24. doi: 10.1186/s13018-014-0144-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khan M, et al. Femoroacetabular impingement: have we hit a global tipping point in diagnosis and treatment? Results From the InterNational Femoroacetabular Impingement Optimal Care Update Survey (IN FOCUS) Arthroscopy. 2016;32(5):779–787 e4. doi: 10.1016/j.arthro.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 11.Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24(5):540–6. doi: 10.1016/j.arthro.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 12.Larson CM, Stone RM. Current concepts and trends for operative treatment of FAI: hip arthroscopy. Curr Rev Musculoskelet Med. 2013;6(3):242–9. doi: 10.1007/s12178-013-9170-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohtadi NG, et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT-33) Arthroscopy. 2012;28(5):595–605. doi: 10.1016/j.arthro.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 14.Nho SJ, et al. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39(Suppl):14S–9S. doi: 10.1177/0363546511401900. [DOI] [PubMed] [Google Scholar]
- 15.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 16.Nwachukwu BU, et al. Defining the “substantial clinical benefit” after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017;45(6):1297–1303. doi: 10.1177/0363546516687541. [DOI] [PubMed] [Google Scholar]
- 17.Nwachukwu BU, et al. Arthroscopic treatment of femoroacetabular impingement in adolescents provides clinically significant outcome improvement. Arthroscopy. 2017;33(10):1812–1818. doi: 10.1016/j.arthro.2017.04.008. [DOI] [PubMed] [Google Scholar]
- 18.Nwachukwu BU, et al. Preoperative outcome scores are predictive of achieving the minimal clinically important difference after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017;45(3):612–619. doi: 10.1177/0363546516669325. [DOI] [PubMed] [Google Scholar]
- 19.Nwachukwu BU, et al. Arthroscopic versus open treatment of femoroacetabular impingement: a systematic review of medium- to long-term outcomes. Am J Sports Med. 2016;44(4):1062–1068. doi: 10.1177/0363546515587719. [DOI] [PubMed] [Google Scholar]
- 20.Nwachukwu BU, et al. How are we measuring clinically important outcome for operative treatments in sports medicine? Phys Sportsmed. 2017;45(2):159–164. doi: 10.1080/00913847.2017.1292108. [DOI] [PubMed] [Google Scholar]
- 21.Philippo MJ, et al. Outcomes 2 to 5 years following hip arthroscopy for femoroacetabular impingement in the patient aged 11 to 16 years. Arthroscopy. 2012;28(9):1255–1261. doi: 10.1016/j.arthro.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 22.Rai SK, et al. Approaches for estimating minimal clinically important differences in systemic lupus erythematosus. Arthritis Res Ther. 2015;17:143. doi: 10.1186/s13075-015-0658-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 2046 kb)