Abstract
This study evaluated the prognostic implications of post-percutaneous coronary intervention (PCI) neutrophil-to-lymphocyte ratio (NLR) in patients with acute myocardial infarction (AMI). A total of 309 patients with AMI who underwent cardiac magnetic resonance imaging (CMR) and a complete blood cell count within 24 hours before and after PCI were enrolled. Primary outcome was infarct size. Patients were assigned to high (n = 118) or low (n = 191) NLR groups according to the best cut-off value of 3.88. Infarct size (% of total left ventricular mass) was significantly higher in the high NLR group than in the low NLR group (24.1 ± 11.0 vs. 16.7 ± 9.1, p < 0.001). Post-PCI NLR ≥ 3.88 was associated with risk of a large-sized infarction (≥20%) (OR 2.91, 95% CI 1.73–4.88, p < 0.001). The risk of MACE was also significantly higher in the high NLR group than in the low NLR group (15.8% vs. 7.4%, HR 2.60, 95% CI 1.21–5.60, p = 0.015). Among patients with AMI who underwent PCI, high post-PCI NLR value was associated with higher risk of large-sized infarction as measured by CMR, as well as adverse clinical outcomes. Our findings suggest that post-PCI NLR is a useful tool for risk assessment in patients with AMI who undergo PCI.
Subject terms: Risk factors, Interventional cardiology
Introduction
Inflammation plays a role in the initiation and progression of the atherosclerotic process, which is a leading cause of coronary artery disease1,2. Inflammation also occurs as a result of acute myocardial infarction (AMI) and plays a role in the repair and remodeling of infarcted heart tissue3. Based on this concept, several studies have investigated the associations between various inflammatory markers and clinical outcomes in patients with coronary artery disease4–8. Neutrophil-to-lymphocyte ratio (NLR) has emerged as an independent predictor of cardiovascular outcomes in patients with ischemic heart disease, including AMI9–15. Especially, post-percutaneous coronary intervention (PCI) NLR was found to be a better indicator of severity of myocardial damage than pre-PCI NLR12–14.
Cardiac magnetic resonance imaging (CMR) is the current gold-standard technique for evaluating infarct size and transmural extent of infarction and for performing microvascular assessment in the setting of AMI16,17. Furthermore, CMR allows quantification of the extent of area at risk and salvaged myocardium based on delayed hyperenhancement and T2-weighted images16. It is well known that infarct size has the strongest association with late systolic dysfunction and provides incremental prognostic information in addition to left ventricular ejection fraction18,19.
Though several studies have studied the relation between NLR and clinical outcomes, the associations between post-PCI NLR and structural markers of myocardial injury measured by CMR in patients with AMI are unknown. Therefore, we sought to evaluate the relationship between post-PCI NLR and infarct size, and between post-PCI NLR and clinical outcomes in patients with AMI.
Methods
Study population and data collection
The study population was derived from the prospective institutional AMI registry of Samsung Medical Center between December 2007 and July 2014 (Fig. 1). AMI was defined as evidence of myocardial injury (defined as elevation of cardiac troponin values, with at least one value above the 99th percentile upper reference limit) with necrosis in a clinical setting, consistent with myocardial ischemia20. We excluded patients who did not undergo a complete blood cell count (CBC) within 24 hours before and after PCI. A total of 309 AMI patients who underwent CMR and had pre- and post-PCI CBC data was finally included in the current study (Fig. 1). The Institutional Review Board of Samsung Medical Center approved this study, and all patients provided written informed consent. All research was performed in accordance with relevant standard guidelines20–23.
Figure 1.
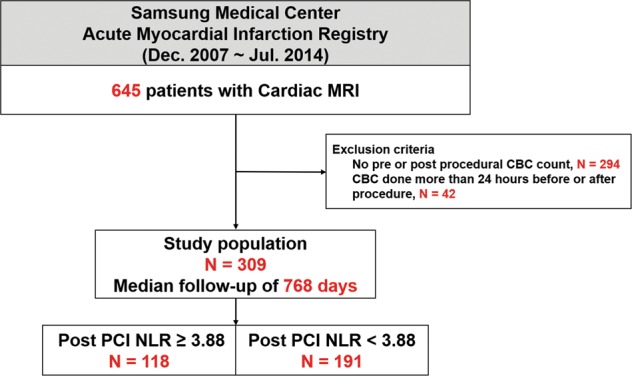
Study flow. Abbreviations: CBC complete blood cell count, MRI magnetic resonance imaging, NLR neutrophil-to-lymphocyte ratio, PCI percutaneous coronary intervention.
Demographic features and cardiovascular risk factors were collected prospectively at the index procedure by patient interview. During hospitalization, coronary angiography, CMR, and echocardiography were conducted. After discharge, patients were followed-up by the attending physician based on individual clinical needs. Follow-up outcomes were obtained from medical records and telephone contact, if necessary. All data were collected by research coordinators of the dedicated registry. Clinical events that occurred within a 2-year follow-up period were analyzed.
Treatment strategy
Patient management was performed according to relevant standard guidelines20–23. The choice of treatment strategy (type, diameter, and length of stents; use of intravascular ultrasound; glycoprotein IIb/IIIa inhibitor use; and thrombus aspiration) was at the discretion of the physicians. PCI was considered successful if the final residual stenosis was <30% with Thrombolysis In Myocardial Infarction grade 3 flow. All patients who were not taking aspirin or a P2Y12 inhibitor received a loading dose of aspirin or P2Y12 inhibitor, respectively. Unless there was an undisputed reason for discontinuing dual-antiplatelet therapy, all patients were recommended to take aspirin indefinitely plus a P2Y12 inhibitor for at least 1 year after the index procedure. Medications were prescribed according to standard guidelines.
Cardiac magnetic resonance imaging
CMR was performed using a 1.5-T scanner (Achieva, Philips Medical Systems, Best, Netherlands) and analyzed using validated software (ARGUS, Siemens Medical System, Erlangen, Germany). Two experienced radiologists who were blinded to the clinical information measured CMR parameters using the software mentioned above (Supplementary Fig. 1). Infarct size and microvascular obstruction (MVO) were quantified using late gadolinium enhancement images16. Infarct size was calculated as summation of the area with delayed hyperenhancement within each segment of the short-axis images. This value was multiplied by slice thickness to cover the entire left ventricle. Endocardial and epicardial borders were then summed to calculate left ventricle myocardial volume using the same method. Infarct size was expressed as a percentage of the affected left ventricular myocardial volume. MVO, which was the extent of hypoenhancement within bright regions of late gadolinium enhancement, was calculated in the same manner16. Area at risk (AAR) was quantified on T2-weighted images using a similar algorithm as above16. From these parameters, myocardial salvage index (MSI) was derived as follows: MSI = (AAR-infarct size)/AAR16.
Definitions and outcomes
The primary outcome was infarct size as measured by CMR after PCI. The main secondary outcome was 2-year major adverse cardiac events (MACE, a composite of all cause death, any myocardial infarction [MI], and any repeat revascularization). Other secondary outcomes were MVO, AAR, MSI as assessed by CMR, and each component of MACE. All clinical outcomes were defined according to the Academic Research Consortium24. All deaths were considered cardiac unless a definite non-cardiac cause could be established. Recurrent MI was defined as elevated cardiac enzymes greater than the upper limit of the normal value with ischemic symptoms or electrocardiography findings indicative of ischemia that were not related to the index procedure. Repeat revascularization was considered clinically indicated if there were symptoms or functional evidence of ischemia and/or lesion severity >50% of the diameter of stenosis by coronary angiography.
Statistical analysis
Simple linear regression analysis was performed to determine the association between post-PCI NLR and infarct size. Receiver-operating-characteristic (ROC) curve analysis was performed to determine the best cut-off value of post-PCI NLR to predict a large-sized infarction as measured by CMR. A large-sized infarction was defined as an infarction involving ≥20% of the total left ventricular mass, which was a median value in a previous study25. The best cut-off value was used to divide the enrolled patients into the two groups.
Continuous variables were compared using Student’s t-test, and categorical variables were tested using the Chi-square test. Multivariable logistic regression analysis was performed to identify independent predictors of large myocardial infarct (≥20% of total left ventricular mass). We included in the multivariable models those covariates that were significant in univariate analysis or those that were clinically relevant.
Cumulative event rates of clinical outcomes were calculated Kaplan-Meier estimates, and significance levels were assessed with log-rank tests. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated by Cox proportional hazards models to compare clinical outcomes that occurred after the index procedure, between the two groups. The time-to-event was measured as days in Cox proportional hazards models. Multiple sensitivity analyses, namely multivariable adjusted Cox proportional hazard regression and inverse-probability-weighted (IPW) analyses, were performed to adjust baseline differences in both groups. Standardized mean differences after IPW adjustment were within ±10% across all matched covariates, suggesting achievement of balance between the two groups (Supplementary Table 1).
All probability values were two-sided, and p-values < 0.05 were considered statistically significant. Statistical analyses were performed using SPSS (version 24.0, SPSS Inc., Chicago, IL, USA) and R Statistical Software (version 3.4.3, R Foundation for Statistical Computing, Vienna, Austria).
Results
Relation between post-PCI NLR and infarct size
CMR was performed a median of 3.4 days (interquartile range 2.7–4.6 days) after the index procedure. To find which leukocytes and differential counts accurately distinguished large-sized (≥20% of the total left ventricular mass) infarctions, ROC curve analysis was performed. Total white blood cell counts and NLR before and after PCI were compared. Among these parameters, post-PCI NLR had the highest C-index (0.693, 95% CI 0.634–0.751) to discriminate a large-sized infarction, and the best cut-off value of post-PCI NLR was 3.88 (Supplementary Fig. 2). Linear regression analysis showed a significant association between post-PCI NLR and infarct size (R2: 0.089, p < 0.001) (Fig. 2).
Figure 2.
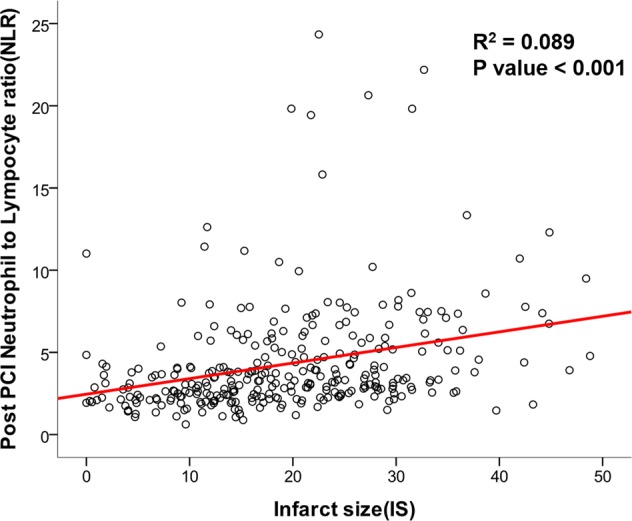
Relation between neutrophil-to-lymphocyte ratio (NLR) and infarct size (IS). Scatter plot is presented to show linear relation between post-PCI NLR and IS. Abbreviations: IS infarct size, NLR neutrophil-to-lymphocyte ratio, PCI percutaneous coronary intervention.
Baseline clinical and angiographic characteristics
According to the post PCI NLR value of 3.88, the study population was stratified into two groups: a high NLR group (post-PCI NLR ≥ 3.88, 118 patients) and a low NLR group (post-PCI NLR < 3.88, 191 patients). Baseline clinical and angiographic characteristics are shown in Tables 1 and 2. Patients in the high NLR group were older and had more frequent previous history of myocardial infarction and PCI than patients in the low NLR group. The high NLR group was more frequently manifested as ST-segment elevation myocardial infarction (STEMI) than those in the low NLR group. Other baseline characteristics were similar between the two groups.
Table 1.
Baseline characteristics of patients with acute myocardial infarction according to an NLR cut-off value of 3.88.
| Variables | Total (N = 309) | NLR ≥ 3.88 (N = 118) | NLR < 3.88 (N = 191) | P value |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) | 60.2 ± 12.3 | 62.1 ± 13.6 | 59.1 ± 11.3 | 0.045 |
| Male | 252 (81.6) | 95 (80.5) | 157 (82.2) | 0.710 |
| Body mass index, kg/m2 | 24.6 ± 3.4 | 24.0 ± 3.7 | 24.9 ± 3.1 | 0.024 |
| Cardiovascular risk factors | ||||
| Hypertension | 130 (42.1) | 53 (44.9) | 77 (40.3) | 0.426 |
| Diabetes mellitus | 68 (22.0) | 32 (27.1) | 36 (18.8) | 0.088 |
| Dyslipidemia | 51 (16.5) | 16 (13.6) | 35 (18.3) | 0.273 |
| History of myocardial infarction | 15 (4.9) | 10 (8.5) | 5 (2.6) | 0.020 |
| History of percutaneous coronary intervention | 22 (7.1) | 14 (11.9) | 8 (4.2) | 0.011 |
| History of cerebrovascular accident | 14 (4.5) | 6 (5.1) | 8 (4.2) | 0.713 |
| Laboratory findings | ||||
| NT-proBNP, pg/mL | 209.6 (55.9–807.5) | 204.1 (69.1–1012.3) | 212.6 (50.6–696.7) | 0.246 |
| White blood cell, ×103/μL | 9.9 ± 3.1 | 11.4 ± 3.4 | 9.0 ± 2.6 | <0.001 |
| Hemoglobin, g/dL | 13.5 ± 1.9 | 13.2 ± 2.0 | 13.7 ± 1.8 | 0.013 |
| Platelet, 103/μL | 206.8 ± 45.4 | 209.5 ± 48.6 | 205.1 ± 43.4 | 0.403 |
| Clinical presentation | ||||
| NSTEMI | 82 (26.5) | 16 (13.6) | 66 (34.6) | <0.001 |
| Door-to-balloon time, min | 681.5 (192.5–1287.5) | 478.5 (155.5–1246.0) | 700.0 (192.5–1308.3) | 0.460 |
| Symptom-to-balloon time, min | 1296.0 (624.0–1892.8) | 1265.5 (546.0–2468.5) | 1338.5 (688.5–1892.8) | 0.923 |
| STEMI | 227 (73.5) | 102 (86.4) | 125 (65.4) | <0.001 |
| Door-to-balloon time, min | 70.0 (53.0–82.0) | 70.0 (51.0–81.5) | 70.0 (53.5–82.0) | 0.793 |
| Symptom-to-balloon time, min | 198.0 (116.0–410.0) | 202.0 (101.5–412.5) | 198.0 (123.0–423.0) | 0.576 |
| Post-percutaneous coronary intervention medication | ||||
| Aspirin | 309 (100.0) | 118 (100.0) | 191 (100.0) | >0.99 |
| P2Y12 inhibitor | 303 (98.1) | 116 (98.3) | 187 (97.9) | >0.99 |
| Beta-blocker | 280 (90.6) | 106 (89.8) | 174 (91.1) | 0.710 |
| ACE inhibitor or ARB | 246 (79.6) | 89 (75.4) | 157 (82.2) | 0.151 |
| Statin | 296 (95.8) | 111 (94.1) | 185 (96.9) | 0.255 |
Data are presented as n (%), mean ± SD, or median (interquartile range).
Abbreviations: ACE angiotensin converting enzyme, ARB angiotensin receptor blocker, NLR neutrophil-to-lymphocyte ratio, NT-proBNP N-terminal pro-brain natriuretic peptide, STEMI ST-segment elevation myocardial infarction, NSTEMI non-ST-segment elevation myocardial infarction.
Table 2.
Angiographic and procedural characteristics of patients with acute myocardial infarction according to an NLR cut-off value of 3.88.
| Variables | Total (N = 309) | NLR ≥ 3.88 (N = 118) | NLR < 3.88 (N = 191) | P value |
|---|---|---|---|---|
| Infarct-related artery | 0.286 | |||
| LAD | 145 (46.9) | 63 (53.4) | 82 (42.9) | |
| LCX | 48 (15.5) | 16 (13.6) | 32 (16.8) | |
| RCA | 115 (37.2) | 39 (33.1) | 76 (39.8) | |
| LM | 1 (0.3) | 0 (0.0) | 1 (0.5) | |
| Number of diseased vessels | 0.253 | |||
| 1 | 163 (52.8) | 56 (47.5) | 107 (56.0) | |
| 2 | 101 (32.7) | 45 (38.1) | 56 (29.3) | |
| 3 | 45 (14.6) | 17 (14.4) | 28 (14.7) | |
| Multi-vessel disease | 146 (47.2) | 62 (52.5) | 84 (44.0) | 0.143 |
| Pre-PCI TIMI flow ≤ 1 | 232 (75.1) | 96 (81.4) | 136 (71.2) | 0.062 |
| Post-PCI TIMI flow 3 | 288 (93.2) | 108 (91.5) | 180 (94.2) | 0.357 |
| Thrombus aspiration | 166 (53.7) | 69 (58.5) | 97 (50.8) | 0.188 |
| Number of implanted stents | 1.2 ± 0.7 | 1.1 ± 0.7 | 1.2 ± 0.6 | 0.833 |
| Stent diameter, mm | 3.2 ± 0.5 | 3.1 ± 0.5 | 3.2 ± 0.6 | 0.175 |
| Stent diameter < 3 mm | 122 (39.5) | 55 (46.6) | 67 (35.1) | 0.058 |
| Stent length, mm | 31.6 ± 17.1 | 30.9 ± 16.9 | 32.0 ± 17.2 | 0.619 |
Data are presented as n (%), mean ± SD, or median (interquartile range).
Abbreviations: LAD left anterior descending artery, LCX left circumflex artery, RCA right coronary artery, LM left main coronary artery, NLR neutrophil-to-lymphocyte ratio, PCI percutaneous coronary intervention, TIMI thrombolysis in myocardial infarction.
Outcomes
Laboratory, echocardiography, and CMR findings according to the NLR cut-off value of 3.88 are presented in Table 3. The high NLR group had a significantly larger infarct size than the low NLR group (24.1 ± 11.0 vs. 16.7 ± 9.1, p < 0.001). Size of AAR (40.7 ± 16.3 vs. 29.5 ± 15.1, p < 0.001) and MVO (2.9 [0–9.3] vs. 0 [0–3.7], p < 0.001), which are other important indicators of severe infarction, were also significantly larger in the high NLR group. MSI tended to be lower in the high NLR group than the low NLR group (40.3 ± 16.9 vs. 42.7 ± 17.5, p = 0.237), but this difference was not statistically significant. Post-PCI NLR ≥ 3.88 was the strongest predictor of large-sized infarction (odds ratio: 2.91, 95% CI: 1.73–4.88, p < 0.001) by multivariable logistic regression analysis (Table 4).
Table 3.
Infarct size assessment using laboratory, echocardiography, and cardiac MRI data according to an NLR cut-off value of 3.88.
| Variables | Total (N = 309) | NLR ≥ 3.88 (N = 118) | NLR < 3.88 (N = 191) | P value |
|---|---|---|---|---|
| Cardiac laboratory profiles after percutaneous coronary intervention | ||||
| Peak troponin I, ng/mL | 45.3 (11.9–116.2) | 75.3 (22.3–185.5) | 35.8 (8.0–80.3) | <0.001 |
| Peak CK-MB, ng/mL | 140.3 (47.8–248.9) | 193.2 (80.0–314.0) | 100.8 (39.3–210.9) | <0.001 |
| Echocardiography | ||||
| EF | 52.2 ± 10.9 | 49.1 ± 11.5 | 54.1 ± 10.0 | <0.001 |
| Wall motion score index (WMSI) | 1.4 (1.2–1.7) | 1.5 (1.2–1.8) | 1.3 (1.1–1.6) | <0.001 |
| Cardiac MRI | ||||
| Infarct size (% of LV) | 19.5 ± 10.5 | 24.1 ± 11.0 | 16.7 ± 9.1 | <0.001 |
| Area at risk (% of LV) | 33.8 ± 16.5 | 40.7 ± 16.3 | 29.5 ± 15.1 | <0.001 |
| Myocardial salvage index | 41.8 ± 17.3 | 40.3 ± 16.9 | 42.7 ± 17.5 | 0.237 |
| Microvascular obstruction (per Vol) | 0.9 (0–5.4) | 2.9 (0–9.3) | 0 (0–3.7) | <0.001 |
| LV EDV | 148.3 ± 37.2 | 149.7 ± 41.5 | 147.5 ± 34.3 | 0.612 |
| LV ESV | 73.3 ± 32.9 | 79.8 ± 40.3 | 69.3 ± 26.7 | 0.013 |
| LV mass (g) | 108.7 ± 27.4 | 107.9 ± 29.5 | 109.2 ± 26.1 | 0.700 |
| LV EF | 52.1 ± 10.8 | 48.8 ± 11.7 | 54.2 ± 9.7 | <0.001 |
| LV SV | 74.8 ± 16.9 | 69.9 ± 16.0 | 77.9 ± 16.7 | <0.001 |
| LV CO | 5.1 ± 1.1 | 5.0 ± 1.1 | 5.2 ± 1.1 | 0.172 |
Data are presented as mean ± SD or median (interquartile range).
Abbreviations: CK-MB creatine kinase-myocardial band, CO cardiac output, EDV end diastolic volume, EF ejection fraction, ESV end systolic volume, LV left ventricle, NLR neutrophil-to-lymphocyte ratio, SV stroke volume.
Table 4.
Independent predictors of large myocardial infarction (≥20%) in patients with acute myocardial infarction.
| OR (95% CI)* | P value | |
|---|---|---|
| ST-segment elevation myocardial infarction | 1.81 (1.02–3.24) | 0.042 |
| Post PCI NLR ≥ 3.88 | 2.91 (1.73–4.88) | <0.001 |
| Male | 1.98 (1.01–3.87) | 0.043 |
| Body mass index ≥ 25 kg/m2 | 0.55 (0.33–0.92) | 0.021 |
Adjusted variables were age, male, hypertension, diabetes mellitus, history of myocardial infarction, history of PCI, ST-segment elevation myocardial infarction, multi-vessel disease, anterior infarction, body mass index ≥ 25 kg/m2, and post-PCI NLR ≥ 3.88.
*C-index of the logistic regression model for large infarct size was 0.717 (95% CI 0.659–0.775).
Abbreviations: CI confidence interval, OR odds ratio, NLR neutrophil-to-lymphocyte ratio, PCI percutaneous coronary intervention, TIMI Thrombolysis In Myocardial Infarction.
Median follow-up duration was 768 days. Cumulative incidence of MACE was significantly higher in the high NLR group than in the low NLR group (15.8% vs. 7.4%, HR: 2.60, 95% CI: 1.21–5.60, p = 0.015) (Table 5 and Fig. 3). After adjusting baselines by multivariable Cox regression and IPW adjustment, post-PCI NLR ≥ 3.88 was consistently associated with a higher risk of MACE (Table 5). The higher risk of MACE in AMI patients with high post-PCI NLR was mainly driven by the higher rates of hard endpoints, including all-cause death (4.6% vs. 0.6%, HR 8.47, 95% CI 0.99–72.51, p = 0.051) and MI (4.9% vs. 0.8%, HR 8.64, 95% CI 1.01–73.97, p = 0.049) (Table 5 and Supplementary Fig. 3).
Table 5.
Two-year clinical outcomes in patients with acute myocardial infarction according to an NLR cut-off value of 3.88.
| NLR ≥ 3.88 (n = 118) | NLR < 3.88 (n = 191) | Unadjusted | Adjusted | IPW-adjusted | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95% CI) | p value | HR(95% CI) | p value | HR(95% CI) | p value | |||
| MACE | 16 (15.8) | 11 (7.4) | 2.60 (1.21–5.60) | 0.015 | 2.38 (1.01–5.17) | 0.028 | 1.69 (1.00–2.86) | 0.048 |
| All-cause death | 5 (4.6) | 1 (0.6) | 8.47 (0.99–72.51) | 0.051 | 6.09 (0.70–52.78) | 0.101 | 2.65 (0.96–7.26) | 0.059 |
| Myocardial infarction | 5 (4.9) | 1 (0.8) | 8.64 (1.01–73.97) | 0.049 | 6.70 (0.75–59.70) | 0.088 | 4.31 (0.88–21.18) | 0.072 |
| Any revascularization | 8 (8.8) | 8 (5.5) | 1.78 (0.67–4.74) | 0.250 | 1.50 (0.53–4.25) | 0.445 | 1.30 (0.65–2.57) | 0.456 |
Adjusted variables were age, sex, diabetes mellitus, history of myocardial infarction, ST-segment elevation myocardial infarction, anterior infarction, TIMI flow grade 0 before PCI.
Data are presented as n (%).
Abbreviations: CI confidence interval, HR hazard ratio, IPW inverse-probability-weighted, MACE major cardiac adverse event, NLR neutrophil-to-lymphocyte ratio, PCI percutaneous coronary intervention, TIMI Thrombolysis In Myocardial Infarction.
Figure 3.
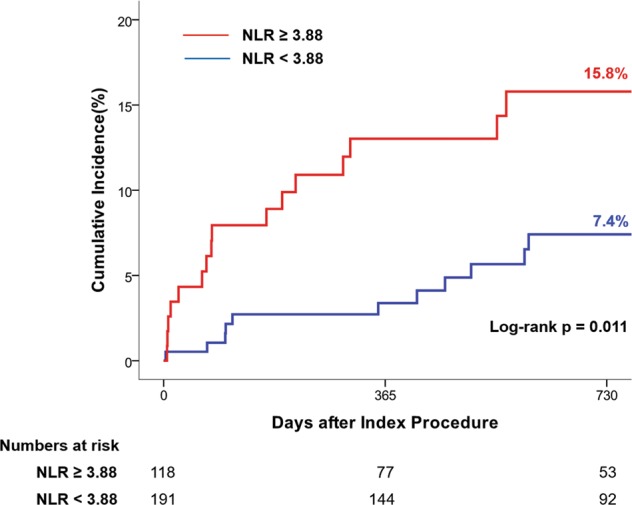
Cumulative incidence of major adverse cardiac events (MACE) at 2 years after the index procedure. Kaplan-Meier curves are presented to compare the cumulative incidence of MACE between the high NLR group and low NLR group. Abbreviations: MACE major adverse cardiac event, NLR neutrophil-to-lymphocyte ratio.
Subgroup analysis of STEMI patients
Because presentation with STEMI is an independent predictor of large-sized infarction, subgroup analysis was performed to determine whether post-PCI NLR plays a role in risk stratification for STEMI patients. STEMI patients with NLR ≥ 3.88 had significantly larger infarct size, AAR, and MVO, consistent with findings in the larger study population (Supplementary Fig. 4). In addition, the high post-PCI NLR group showed significantly higher risk of MACE than the low NLR group among patients who presented with STEMI (Supplementary Fig. 5).
Discussion
In this present study, we evaluated the association between post-PCI NLR and infarct size as well as clinical outcomes in patients with AMI. Our key findings were as follows. First, among various pre- and post-leukocyte parameters and differential counts, post-PCI NLR showed the best ability to discriminate large-sized infarctions. Second, elevated post-PCI NLR was associated with larger infarct size and MVO and higher risk of MACE, and this association was robust after adjusting baselines using multivariable adjusted Cox regression and IPW adjustments. Third, subgroup analysis of STEMI patients revealed that infarct size was significantly larger and risk of MACE significantly higher in the post-PCI NLR ≥ 3.88 group than the post-PCI NLR < 3.88 group.
AMI remains one of the most important causes of morbidity and mortality worldwide despite recent advances in PCI techniques and devices26. Therefore, there have been numerous efforts to predict prognosis and improve outcomes in AMI patients18,27,28. Inflammation is not only an important cause of atherosclerosis, but also involved in the repair and adverse remodeling of infarcted heart tissue3. In this regard, interest in the role of inflammation in patients with AMI is increasing, and numerous studies have evaluated the associations between various inflammatory markers and clinical outcomes in patients with AMI4–15. A previous study showed that leukocyte differentials have greater predictive value of clinical outcome than total leukocyte count29. In that study, NLR was the most powerful predictor of death or myocardial infarction among various leukocyte parameters and differential counts29. In particular, Park et al. showed that post-PCI NLR was more strongly associated with mortality than baseline or pre-PCI NLR12. A possible explanation for this finding is that the time elapsed after infarction is too short for pre-PCI leukocyte profiles to fully reflect the severity of the ongoing myocardial damage. Similarly, considering that CMR was performed few days after PCI, temporal proximity may be a reason to explain that the post-PCI NLR may better reflect infarct size than the pre-PCI NLR. Furthermore, post-PCI leukocyte profiles have the advantage that they may also reflect peri-procedural myocardial damage14. In accordance with previous studies12,14,29, we showed that patients with AMI and a high post-PCI NLR had a higher risk of adverse cardiac events than those with a low post-PCI NLR. The reason for this association is that, in addition to their role in repair of the infarcted heart, leukocytes are also involved in infarct expansion29,30. After infarction, neutrophils release superoxide radicals, enzymes, and other metabolites that facilitate plaque disruption and lead to infarct expansion. Neutrophils aggregate with platelets and damage micro-vessels, which can also promote infarct expansion29. In addition, lymphocytes are trapped and sequestered within the myocardial microvasculature and release inflammatory mediators, contributing to further leukocyte infiltration and myocardial damage31. On this background, the results of the current study suggest that post-PCI NLR might be a predictor of clinical outcomes in AMI patients.
CMR is considered the gold standard for evaluating cardiac volumes and systolic function16. In addition, CMR has become the most accurate tool to visualize and quantify post-infarction parameters in patients with AMI18. Among post-infarction parameters, infarct size is strongly associated with mortality and hospitalization for heart failure32. Furthermore, infarct size can provide incremental prognostic information in addition to left ventricular ejection fraction, which is a well-established predictor of outcome in AMI18. Because left ventricular ejection fraction is influenced both by stunned viable myocardium and nonviable myocardium, CMR parameters can be more specific markers for determining the extent of irreversible myocardial damage33. Although several studies have investigated the association between white blood cell count and extent of infarct measured by CMR4,34–36, limited data are available regarding the association between post-PCI NLR and infarct size. Therefore, we sought to assess whether high post-PCI NLR value is associated with larger infarct size as assessed by CMR in patients with AMI. We found that high post-PCI NLR was consistently associated with larger infarct size and MVO as assessed by various tools, including cardiac enzymes, echocardiography, and CMR in patients with AMI who underwent PCI. Furthermore, there was a linear correlation between post-PCI NLR and infarct size as measured by CMR. Although the myocardial salvage index was numerically lower in the high post-PCI NLR group, this difference was not statistically significant. The results of our study suggest that post-PCI NLR, which is a simply measured marker of inflammation, can help predict infarct size as well as prognosis of patients with AMI after PCI.
In the current study, we thoroughly compared various pre and post PCI leukocytes profiles and identified that post-PCI NLR showed the best ability to discriminate large-sized infarctions assessed by CMR. To verify prognostic implication of post-PCI NLR, comprehensive assessment was conducted to find relation with post-PCI NLR and various markers of infarct size such as laboratory and echocardiographic findings as well as adverse clinical outcomes. Furthermore, the robustness of these results were supported by many sensitivity analyses such as multivariable regression and IPW adjustment. Thereby our results suggest that post-PCI NLR can be used for predicting prognosis as well as an infarct size predictor in future trials that aim to reduce infarct size. However, this study had several limitations. First, it was a retrospective study. Therefore, there may have been selection bias, and confounding variables may not have been accounted for. To overcome retrospective design of study, multivariable regression and IPW adjustment were performed to minimize the effect of confounders. Second, many patients were excluded from the study because they did not undergo pre- and post-PCI CBC with differential counts. This exclusion could have resulted in selection bias. Third, the number of patients who presented with STEMI was significantly different between the low and high post-PCI NLR groups. However, results from subgroup analysis of STEMI patients only were consistent with the results obtained for the entire study population. Fourth, the post-PCI NLR cut-off value was lower than that reported in previous studies12,13. Unlike previous studies that reported NLR cut-off values that best predicted clinical outcomes, we determined the cut-off value that best predicted large-sized infarction. Therefore, it is not surprising that the cut-off value was lower than reported in previous studies because not all patients who have a large-sized infarction have clinical events. Our cut-off value showed a significant association with poorer clinical outcomes and large-sized infarction.
Conclusions
High post-PCI NLR value was associated with higher risk of large-sized infarction as measured by CMR, as well as adverse clinical events in AMI patients who underwent PCI. Our findings suggest that post-PCI NLR, which is an easily measurable and universally available marker, could be a useful tool for risk assessment and prognosis prediction in AMI patients undergoing PCI.
Supplementary information
Acknowledgements
None.
Author Contributions
Hong D., Choi K.H. and Song Y.B.: conception and design of the study, acquisition of data, analysis and interpretation of data, and drafting and revising the article; Lee J.M., Park T.K., Yang J.H., Hahn J.Y., Choi J.H., Choi S.H. and Gwon H.C.: acquisition of data; Kim S.M., Choe Y.H., Kim E.K., Chang S.A., Lee S.C. and Oh J.K.: analysis of images. All authors read and approved the final manuscript.
Data Availability
The data that support the findings of this study are available, on reasonable request, from the corresponding author.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
David Hong and Ki Hong Choi contributed equally.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-46117-8.
References
- 1.Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N. Engl. J. Med. 1997;336:973–979. doi: 10.1056/NEJM199704033361401. [DOI] [PubMed] [Google Scholar]
- 2.Ross R. Atherosclerosis–an inflammatory disease. N. Engl. J. Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 3.Seropian IM, Toldo S, Van Tassell BW, Abbate A. Anti-inflammatory strategies for ventricular remodeling following ST-segment elevation acute myocardial infarction. J. Am. Coll. Cardiol. 2014;63:1593–1603. doi: 10.1016/j.jacc.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 4.Chung S, et al. Impact of white blood cell count on myocardial salvage, infarct size, and clinical outcomes in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a magnetic resonance imaging study. Int. J. Cardiovasc. Imaging. 2014;30:129–136. doi: 10.1007/s10554-013-0303-x. [DOI] [PubMed] [Google Scholar]
- 5.Shah, B. et al. White Blood Cell Count and Major Adverse Cardiovascular Events After Percutaneous Coronary Intervention in the Contemporary Era: Insights From the PARIS Study (Patterns of Non-Adherence to Anti-Platelet Regimens in Stented Patients Registry). Circ. Cardiovasc. Interv. 10 (2017). [DOI] [PMC free article] [PubMed]
- 6.Dhillon OS, et al. Pre-discharge risk stratification in unselected STEMI: is there a role for ST2 or its natural ligand IL-33 when compared with contemporary risk markers? Int. J. Cardiol. 2013;167:2182–2188. doi: 10.1016/j.ijcard.2012.05.073. [DOI] [PubMed] [Google Scholar]
- 7.Lindmark E, Diderholm E, Wallentin L, Siegbahn A. Relationship between interleukin 6 and mortality in patients with unstable coronary artery disease: effects of an early invasive or noninvasive strategy. JAMA. 2001;286:2107–2113. doi: 10.1001/jama.286.17.2107. [DOI] [PubMed] [Google Scholar]
- 8.Orn S, et al. C-reactive protein, infarct size, microvascular obstruction, and left-ventricular remodelling following acute myocardial infarction. Eur. Heart J. 2009;30:1180–1186. doi: 10.1093/eurheartj/ehp070. [DOI] [PubMed] [Google Scholar]
- 9.Duffy BK, et al. Usefulness of an elevated neutrophil to lymphocyte ratio in predicting long-term mortality after percutaneous coronary intervention. Am. J. Cardiol. 2006;97:993–996. doi: 10.1016/j.amjcard.2005.10.034. [DOI] [PubMed] [Google Scholar]
- 10.Tamhane UU, et al. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am. J. Cardiol. 2008;102:653–657. doi: 10.1016/j.amjcard.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Azab B, et al. Usefulness of neutrophil to lymphocyte ratio in predicting short- and long-term mortality after non-ST-elevation myocardial infarction. Am. J. Cardiol. 2010;106:470–476. doi: 10.1016/j.amjcard.2010.03.062. [DOI] [PubMed] [Google Scholar]
- 12.Park JJ, et al. Prognostic value of neutrophil to lymphocyte ratio in patients presenting with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am. J. Cardiol. 2013;111:636–642. doi: 10.1016/j.amjcard.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 13.Sen N, et al. The neutrophil to lymphocyte ratio was associated with impaired myocardial perfusion and long term adverse outcome in patients with ST-elevated myocardial infarction undergoing primary coronary intervention. Atherosclerosis. 2013;228:203–210. doi: 10.1016/j.atherosclerosis.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 14.Bressi E, et al. Relation of Neutrophil to Lymphocyte Ratio With Periprocedural Myocardial Damage in Patients Undergoing Elective Percutaneous Coronary Intervention. Am. J. Cardiol. 2016;118:980–984. doi: 10.1016/j.amjcard.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 15.Monteiro Junior JGM, et al. Prognostic value of hematological parameters in patients with acute myocardial infarction: Intrahospital outcomes. PLoS One. 2018;13:e0194897. doi: 10.1371/journal.pone.0194897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perazzolo Marra M, Lima JA, Iliceto S. MRI in acute myocardial infarction. Eur. Heart J. 2011;32:284–293. doi: 10.1093/eurheartj/ehq409. [DOI] [PubMed] [Google Scholar]
- 17.Wong DT, et al. The role of cardiac magnetic resonance imaging following acute myocardial infarction. Eur. Radiol. 2012;22:1757–1768. doi: 10.1007/s00330-012-2420-7. [DOI] [PubMed] [Google Scholar]
- 18.Eitel I, et al. Comprehensive prognosis assessment by CMR imaging after ST-segment elevation myocardial infarction. J. Am. Coll. Cardiol. 2014;64:1217–1226. doi: 10.1016/j.jacc.2014.06.1194. [DOI] [PubMed] [Google Scholar]
- 19.Larose E, et al. Predicting late myocardial recovery and outcomes in the early hours of ST-segment elevation myocardial infarction traditional measures compared with microvascular obstruction, salvaged myocardium, and necrosis characteristics by cardiovascular magnetic resonance. J. Am. Coll. Cardiol. 2010;55:2459–2469. doi: 10.1016/j.jacc.2010.02.033. [DOI] [PubMed] [Google Scholar]
- 20.Ibanez B, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur. Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 21.O’Gara PT, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2013;61:e78–140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 22.Amsterdam EA, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014;64:e139–e228. doi: 10.1016/j.jacc.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 23.Roffi M, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC) Eur. Heart J. 2016;37:267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 24.Thygesen K, et al. Universal definition of myocardial infarction. Circulation. 2007;116:2634–2653. doi: 10.1161/CIRCULATIONAHA.107.187397. [DOI] [PubMed] [Google Scholar]
- 25.Jang, W. J. et al. Clinical Significance of Postinfarct Fever in ST-Segment Elevation Myocardial Infarction: A Cardiac Magnetic Resonance Imaging Study. J Am Heart Assoc6 (2017). [DOI] [PMC free article] [PubMed]
- 26.Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet. 2017;389:197–210. doi: 10.1016/S0140-6736(16)30677-8. [DOI] [PubMed] [Google Scholar]
- 27.Morice MC, et al. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N. Engl. J. Med. 2002;346:1773–1780. doi: 10.1056/NEJMoa012843. [DOI] [PubMed] [Google Scholar]
- 28.Giugliano GR, Giugliano RP, Gibson CM, Kuntz RE. Meta-analysis of corticosteroid treatment in acute myocardial infarction. Am. J. Cardiol. 2003;91:1055–1059. doi: 10.1016/S0002-9149(03)00148-6. [DOI] [PubMed] [Google Scholar]
- 29.Horne BD, et al. Which white blood cell subtypes predict increased cardiovascular risk? J. Am. Coll. Cardiol. 2005;45:1638–1643. doi: 10.1016/j.jacc.2005.02.054. [DOI] [PubMed] [Google Scholar]
- 30.Frangogiannis NG. The immune system and the remodeling infarcted heart: cell biological insights and therapeutic opportunities. J. Cardiovasc. Pharmacol. 2014;63:185–195. doi: 10.1097/FJC.0000000000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boag SE, et al. T lymphocytes and fractalkine contribute to myocardial ischemia/reperfusion injury in patients. J. Clin. Invest. 2015;125:3063–3076. doi: 10.1172/JCI80055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stone GW, et al. Relationship Between Infarct Size and Outcomes Following Primary PCI: Patient-Level Analysis From 10 Randomized Trials. J. Am. Coll. Cardiol. 2016;67:1674–1683. doi: 10.1016/j.jacc.2016.01.069. [DOI] [PubMed] [Google Scholar]
- 33.Wu E, et al. Infarct size by contrast enhanced cardiac magnetic resonance is a stronger predictor of outcomes than left ventricular ejection fraction or end-systolic volume index: prospective cohort study. Heart. 2008;94:730–736. doi: 10.1136/hrt.2007.122622. [DOI] [PubMed] [Google Scholar]
- 34.Palmerini T, et al. Relation between white blood cell count and final infarct size in patients with ST-segment elevation acute myocardial infarction undergoing primary percutaneous coronary intervention (from the INFUSE AMI trial) Am. J. Cardiol. 2013;112:1860–1866. doi: 10.1016/j.amjcard.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 35.Husser O, et al. White blood cell subtypes after STEMI: temporal evolution, association with cardiovascular magnetic resonance–derived infarct size and impact on outcome. Inflammation. 2011;34:73–84. doi: 10.1007/s10753-010-9209-0. [DOI] [PubMed] [Google Scholar]
- 36.Reindl M, et al. Relation of inflammatory markers with myocardial and microvascular injury in patients with reperfused ST-elevation myocardial infarction. Eur Heart J Acute Cardiovasc Care. 2017;6:640–649. doi: 10.1177/2048872616661691. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available, on reasonable request, from the corresponding author.


