Abstract
Objectives
Previous studies have evidenced cement-in-cement techniques as reliable in revision arthroplasty. Commonly, the original cement mantle is reshaped, aiding accurate placement of the new stem. Ultrasonic devices selectively remove cement, preserve host bone, and have lower cortical perforation rates than other techniques. As far as the authors are aware, the impact of ultrasonic devices on final cement-in-cement bonds has not been investigated. This study assessed the impact of cement removal using the Orthosonics System for Cemented Arthroplasty Revision (OSCAR; Orthosonics) on final cement-in-cement bonds.
Methods
A total of 24 specimens were manufactured by pouring cement (Simplex P Bone Cement; Stryker) into stainless steel moulds, with a central rod polished to Stryker Exeter V40 specifications. After cement curing, the rods were removed and eight specimens were allocated to each of three internal surface preparation groups: 1) burr; 2) OSCAR; and 3) no treatment. Internal holes were recemented, and each specimen was cut into 5 mm discs. Shear testing of discs was completed by a technician blinded to the original grouping, recording ultimate shear strengths. Scanning electron microscopy (SEM) was completed, inspecting surfaces of shear-tested specimens.
Results
The mean shear strength for OSCAR-prepared specimens (33.6 MPa) was significantly lower than for the control (46.3 MPa) and burr (45.8 MPa) groups (p < 0.001; one-way analysis of variance (ANOVA) with Tukey’s post hoc analysis). There was no significant difference in shear strengths between control and burr groups (p = 0.57). Scanning electron microscopy of OSCAR specimens revealed evidence of porosity undiscovered in previous studies.
Conclusion
Results show that the cement removal technique impacts on final cement-in-cement bonds. This in vitro study demonstrates significantly weaker bonds when using OSCAR prior to recementation into an old cement mantle compared with cement prepared with a burr or no treatment. This infers that care must be taken in surgical decision-making regarding cement removal techniques used during cement-in-cement revision arthroplasty, suggesting that the risks and benefits of ultrasonic cement removal need consideration.
Cite this article: A. Liddle, M. Webb, N. Clement, S. Green, J. Liddle, M. German, J. Holland. Ultrasonic cement removal in cement-in-cement revision total hip arthroplasty: What is the effect on the final cement-in-cement bond? Bone Joint Res 2019;8:246–252. DOI: 10.1302/2046-3758.86.BJR-2018-0313.R1.
Keywords: Ultrasonic cement removal, Cement-in-cement, Revision hip arthroplasty, Cemented total hip arthroplasty
Article focus
This study investigated the impact of cement removal methods on the final cement-in-cement bond.
The null hypothesis was that there would be no difference in the cement-in-cement bond strength between specimens in the Orthosonics System for Cemented Arthroplasty Revision (OSCAR), burr, or control groups.
The secondary aim of this study was evaluation with scanning electron microscopy, assessing for any visible variation that may account for shear strength differences.
Key messages
The mean shear strength of OSCAR-prepared specimens was significantly lower (27% lower) and more variable than in the control and burr groups.
Scanning electron microscopy of OSCAR specimens demonstrated an additional porous zone not previously discovered.
Strengths and limitations
The results are highly statistically significant and demonstrate a new finding that OSCAR-prepared samples are weaker and show microscopic variation.
In vitro study and hence further work is required to investigate clinical significance.
The results raise important questions over the reliability of this commonly used surgical technique and open up further interesting research topics.
Introduction
As the population continues to age, the number of primary total hip arthroplasties, and thus revision hip arthroplasties, will continue to increase.1,2 The National Joint Registry (NJR) reported 8417 revision hip procedures in the United Kingdom during 2016 alone.3 In the case of cemented femoral stem revision, removal of the original cement mantle can be technically challenging and time-consuming, and can carry increased risks of complications such as bleeding, cortical perforation, and even femoral fracture.4-6 Where appropriate, it is possible to avoid complete cement removal, allowing recementation of a new component into a well-fixed mantle. This is a recognized technique, with numerous studies proving cement-in-cement as a reliable method for primary revision,7-11 as well as those hips requiring multiple revision procedures. Data show good outcomes in hips undergoing up to four repeat cement-in-cement revisions.6
Often, to allow a new stem to fit and/or to reorientate the prosthesis, part of the original cement mantle needs to be removed or refashioned from within; this can be completed with a rasp, burr, or ultrasonic device.12,13 The use of ultrasonic devices for cement removal is appealing due to their efficiency in selectively removing cement while preserving host bone. This technique also holds a lower cortical perforation rate when compared with other options.13 With increasing numbers of cement-in-cement hip revisions, the use of ultrasonic cement removal is likely to increase; however, the effect of this technique on the final cement-in-cement bond strength has not been investigated.
The primary aim of this study was to compare the shear strength of the cement-in-cement interface for a cement mantle prepared with Orthosonics System for Cemented Arthroplasty Revision (OSCAR; Orthosonics, Maidenhead, United Kingdom) ultrasonic cement removal versus those prepared with a burr and those with no preparation (control). The secondary aim was to evaluate the cement-in-cement bond with scanning electron microscopy (SEM), assessing whether there were observable variations to account for any shear strength differences. The null hypothesis was that there would be no difference in the cement-in-cement bond strength between specimens prepared with OSCAR, specimens prepared with burr, or specimens with no preparation (control).
Materials and Methods
Preparation of cement specimens
Test specimens were manufactured as described by Weinrauch et al,14 in stainless steel moulds with internal diameters of 38 mm, with a 19.1 mm diameter rod polished to Exeter V40 specifications (Fig. 1). The rod was constrained within central recesses in both the top and bottom plate of the mould, therefore guaranteeing a centralized hole with the same geometric location in all specimens. The top cap of the mould also served to prevent cement extrusion as the cement cured.
Fig. 1.

Photographs showing a stainless steel mould.
A single mix of Stryker Simplex cement (Simplex B Bone cement; Stryker UK Ltd, Newbury, United Kingdom) was mixed according to the manufacturer’s instructions under negative pressure in theatre-controlled temperature conditions for one minute. The cement was then poured into the mould with the rod in situ. Specimens were held with the top cap in situ for a minimum of ten minutes or until the cement had cured. Following this, the central rod was extracted and the specimens were post-cured in a dry, controlled-temperature environment for a minimum of 24 hours.
A total of 24 initial specimens were made. Any specimens found to have macroscopic porosity were discarded and further specimens were produced in replacement. The specimens were each randomly allocated to one of three different internal preparation groups (with eight cylinders allocated to each group), as follows: a) no treatment (control); b) burr; and c) OSCAR. The specimens were washed and dried, and then the internal aspect was prepared according to group. Burr specimens had the internal surface burred to a depth of approximately 2 mm using a high-speed burr. The OSCAR specimens had cement removal using an OSCAR probe at every point (I to XII) on a ‘clock-face’ drawn on the outer surface at the end of the cylinder. Specimens were washed with detergent to remove any residue from handling, removing any third body particles with potential to contaminate the cement-in-cement interface. After thorough rinsing, specimens were dried, then left to dry fully for a further minimum of 24 hours at 20°C (Fig. 2). An extra specimen was manufactured in each group for analysis with SEM to assess surface structure.
Fig. 2.
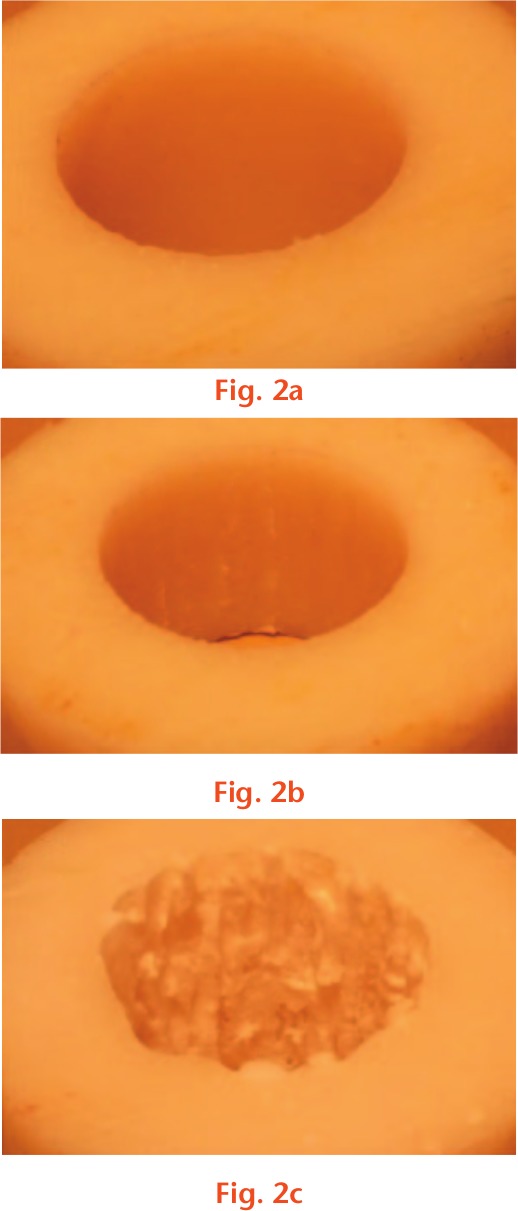
Internal surface preparation: a) control; b) burr; and c) Orthosonics System for Cemented Arthroplasty Revision (OSCAR).
Following cylinder preparation, further single cement mixes (made with the same technique detailed above) were poured into the centre of all cement cylinders, then left to cure for 24 hours. Pressurization techniques were not used during this stage of the process. Unlike introducing cement into a porous structure (e.g. cancellous bone), when cementing into a non-porous cavity (e.g. a pre-existing cement mantle), interdigitation and quality of bonding was not expected to be improved by pressurization. Specimens were labelled according to internal surface preparation.
Discs 5 mm thick were parted from each cylinder (Colchester Bantam lathe (Colchester Machine Tool Solutions, Elland, United Kingdom), using parting bits GTN3 TICN (MSC Industrial Supply, Wednesbury, United Kingdom)) and faced (Myford Super 7 lathe (Myford Ltd, Mytholmroyd, United Kingdom), using facing bits TCMT110204FP (MSC Industrial Supply)) while checking with an infrared probe to ensure that temperatures did not exceed 25°C. Discs were measured with a digital caliper to ensure uniform thickness and were examined visually for homogeneity. Any specimens with porosity were discarded, along with all the other discs cut from the same cement cylinder.
Mechanical tests
The shear strength of the interface of the discs was tested at room temperature, as described by Weinrauch et al,14 by a technician blinded to the original grouping. Discs were placed in a mechanical testing machine (Instron 5567; Instron, High Wycombe, United Kingdom), using a 30 kN load cell at a crosshead speed of 1 mm/min. Samples were fixed into the holder and tightened using a 5 Nm torque driver before testing, ensuring that a fixed force was applied to each specimen in all planes. Force was applied to the central portion of the disc, and the force (F) required to cause failure of the interface was recorded. The interfacial shear strength (MPa) was calculated by dividing the failure force (N) by 2πrh, where r was the radius of the specimen (mm) and h its height (mm): interfacial shear strength (MPa) = F/(2πrh)
Scanning electron microscopy
After shear testing, representative specimens from each group were selected for SEM analysis. Specimens were carefully sectioned using a band saw (model CBS350, Clarke International, Epping, United Kingdom) and then coated with 15 nm gold using a Polaron sputter coating unit. Specimens were then analyzed using a Tescan Vega 3 LMU SEM (Tescan Orsay Holding, Kohoutovice, Czech Republic), with all images taken away from the cut edges to avoid artefacts produced during band saw preparation. Images were acquired from both sides of the failed interface of the shear-tested specimens.
Statistical analysis
Statistical analysis was performed using Statistical Package for Social Sciences version 17.0 (SPSS Inc., Chicago, Illinois). A mean and standard deviation were taken as descriptive statistics of all strength data. Comparison between groups was conducted using one-way analysis of variance (ANOVA) and Tukey’s post hoc analyses. A p-value of < 0.05 was defined as significant. A post hoc power analysis was performed using G*Power 3.1.15
Results
Shear testing
After discarding macroscopically porous samples (three specimens), there were a total of 21 specimens (105 discs) deemed suitable for shear testing.
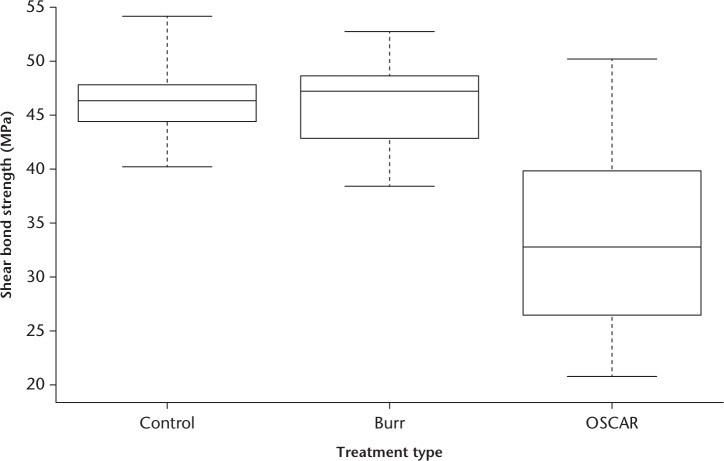
The interfacial shear strengths for specimens from the three groups are summarized in Table I and Figure 3. The control and burr groups demonstrated a consistent distribution of shear strength throughout the samples, illustrated by the similar standard deviations of 2.9 and 3.8, respectively. In contrast, the OSCAR group had a wider shear strength distribution (Fig. 3), which is signified by the greater standard deviation of 7.9. The control group had a slightly higher mean strength (46.3 MPa) than the burr group (45.8 MPa), but this difference was not found to be significant. In contrast, the OSCAR group exhibited a significantly lower mean interfacial shear strength (33.6 MPa) than the control and burr groups (p < 0.001). This reduction in the interfacial shear strength for specimens made using OSCAR represents a loss of 27% compared with the control samples.
Table I.
Comparison of interfacial shear strengths
| Strength | Groups | Difference | 95% CI | p-value* | |
|---|---|---|---|---|---|
| Control (n = 40) | Burr (n = 35) | ||||
| Shear strength, MPa (sd) | 46.3 (2.9) | 45.8 (3.8) | -0.5 | -2.0 to 1.1 | 0.57 |
| Control (n = 40) | OSCAR (n = 30) | ||||
| Shear strength, MPa (sd) | 46.3 (2.9) | 33.6 (7.9) | -12.7 | -10.0 to 15.4 | < 0.001 |
| Burr (n = 35) | OSCAR (n = 30) | ||||
| Shear strength, MPa (sd) | 45.8 (3.8) | 33.6 (7.9) | -12.3 | -15.3 to -9.3 | < 0.001 |
One-way analysis of variance (ANOVA) adjusted for multiple testing
CI, confidence interval; OSCAR, Orthosonics System for Cemented Arthroplasty Revision
Fig. 3.
Boxplot showing interfacial shear strength distributions. The horizontal line shows the median, the boxes show the interquartile ranges, and the error bars show the maximum and minimum values. OSCAR, Orthosonics System for Cemented Arthroplasty Revision.
A post hoc power calculation was performed using the data from Table I and an alpha value of 0.005 (to adjust for multiple testing) using a two-way analysis. The power for OSCAR versus control, and for OSCAR versus burr, was 100%; however, this fell to a 15% power for burr versus OSCAR.
Scanning electron microscopy
All inspected specimens showed typical fracture behaviour for glassy polymers (Figs 4 and 5). However, OSCAR specimens also demonstrated an additional porous zone (Fig. 6). One region showed the typical surface expected after fracture through a polymer observed in all specimens (Fig. 7). The other region showed atypical surface appearances with small porous areas of indeterminate depth, as highlighted in zone A (Fig. 6), and again in the magnified image (Fig. 8).
Fig. 4.
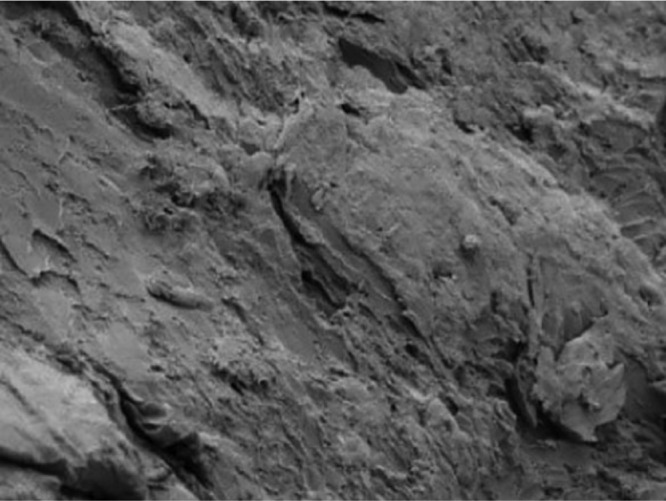
Control specimen shear-tested surface. Magnified 500×.
Fig. 5.
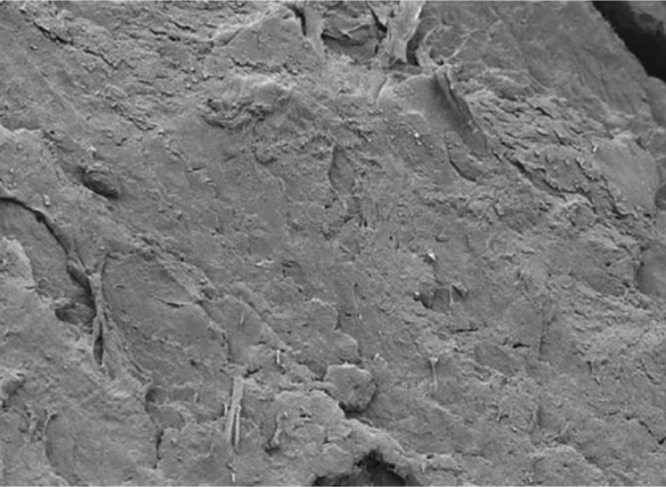
Burr specimen shear-tested surface. Magnified 500×.
Fig. 6.
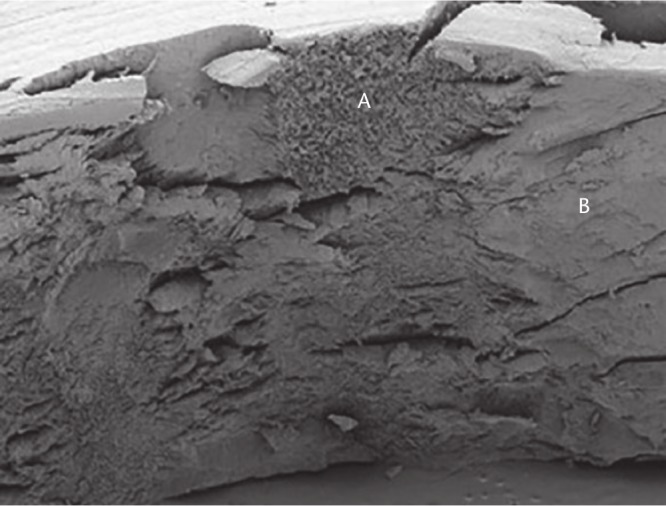
Two areas seen on Orthosonics System for Cemented Arthroplasty Revision (OSCAR) specimens: only seen on OSCAR specimens (A); and typical of all specimens (B). Magnified 51×.
Fig. 7.
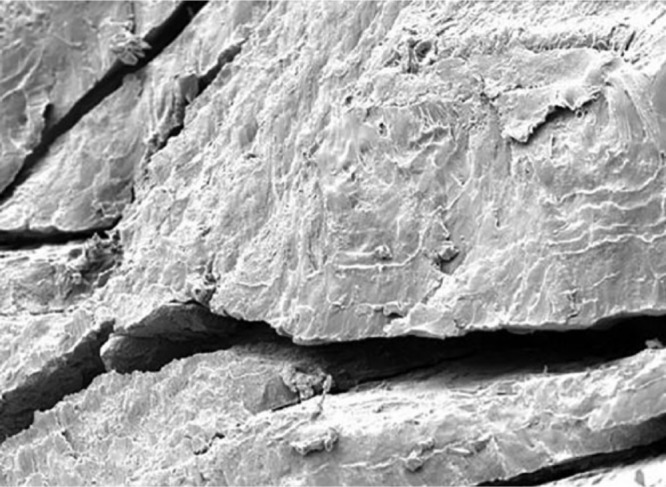
Magnified image of zone B from Figure 6. Magnified 500×.
Fig. 8.
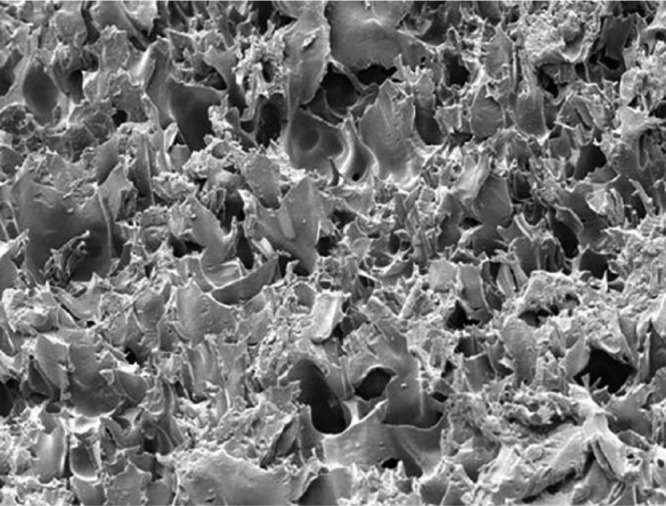
Magnified image of zone A from Figure 6. Magnified 500×.
Discussion
This novel study has demonstrated that cement mantles prepared with an OSCAR ultrasonic probe have a significantly lower cement-in-cement shear strength when compared with those that have been prepared with a burr, and when compared with control samples. This difference may be related to a porous zone that was observed at the cement-in-cement interface for the OSCAR group only.
There has been much research into factors affecting the strength and quality of the final cement-in-cement bond. Previous research has shown that the following factors can affect strength significantly: fluid between the two cement layers;16 contamination with blood or marrow fat;4 roughness of the primary cement mantle;16,17 post-cure duration;14 and porosity of cement.18 Surgical techniques have thus been improved to reduce these risks. It has also been demonstrated that roughening the surface of an old cement mantle with a rasp prior to recementation can improve the bond strength by up to 6%. This is perhaps due to increasing the surface contact area available for mechanical interlocking between the old and new cement surfaces, and potentially due to presenting more residual activator/monomer to the newly applied cement.17 This study has been completed by testing just one formulation of cement (Simplex B Bone cement), but the authors believe it is likely that results would be similar when using a different cement preparation, given their similar chemical composition and physical properties. The current study highlights the use of OSCAR as a new factor that should be recognized to significantly weaken the cement-in-cement bond.
Since a significant weakness was found in the OSCAR specimens, the shear-tested samples were examined using SEM to inspect the failed interface. This revealed an unusual ‘spiked’ surface on those prepared with OSCAR. It is likely that the heat generated from the ultrasonic probe causes the surface to form a foam, which is a weaker structure than the normal cement surface. When a fresh layer of cement is applied, there is interdigitation between the foam and new cement, which breaks easily under stress, meaning that the overall strength is reduced. In fact, close inspection of the surfaces of the OSCAR specimens prior to second cement application (Fig. 2) shows that some surface damage had occurred after the use of the ultrasonic probe. Concerns have been raised in the past regarding the degree of heat generation in the process of ultrasonic cement removal, with the hypothesis being that there will be associated tissue or bone damage.13,19 The effect of this on the final cement-in-cement bond has not, however, been previously considered. The unusual surface pattern on SEM, paired with the significant weakness on shear testing, adds evidence to the argument that ultrasonic cement removal damages the existing cement surface. Therefore, when fresh cement is applied, the new cement-in-cement bonds are significantly affected. It might be possible to remove the surface damaged by the OSCAR (thus improving the cement-in-cement bond strength); however, the damage appears to be of variable depth, which would make its removal, for example with a burr, quite challenging.
Ultrasonic cement removal has become common practice for many surgeons performing total hip arthroplasty revisions, with the advantages of decreased cortical perforation rates, preservation of host bone stock, and elimination of the need for osteotomy and associated comorbidities.13 Although there have been concerns raised about the degree of heat generation in this process, as well as the potential for tissue damage,13,19 its effect on the final cement-in-cement bond has not been previously considered.
Shear-testing data from this study showed that specimens prepared with OSCAR had a strength that was 27% lower than the control specimens or those prepared with a burr. During cement-in-cement revision, a taper slip stem is typically used, loading the cement mantle in compression.8,20 This study tests the samples in shear to replicate previous cement-in-cement studies,14 which may limit its clinical relevance. As a result, however, this does provide evidence to compare directly with previous laboratory data, and raises an important consideration. Although this is an in vitro study, it may have implications in vivo and, certainly, if a composite beam fixation were used in a cement-in-cement revision, this study would provide evidence against the use of OSCAR in the mantle preparation.
Rates of revision hip surgery are increasing and are expected to continue to rise.1 Since Greenwald et al17 opened discussions regarding the acceptability of cement-in-cement as a technique, surgical techniques have been adapted. There have now been many publications adding to the evidence that cement-in-cement is an acceptable technique, with follow-up reported of up to 15 years.8,9 Ultrasonic cement removal is an attractive option in revision surgery due to the reduced complication rates and associated comorbidities of other cement removal techniques.13 As rates of revision surgery increase, the use of ultrasound cement removal as part of a cement-in-cement femoral revision needs to be considered, since the proven weakened bond may have an impact on long-term results and risk of re-revision. Further work is required to observe what would happen to an OSCAR-prepared cement-in-cement sample, over time, if cyclically loaded from within by a stem. This would also give an opportunity to observe the effect of cement creep on the interface conditions.
In conclusion, this in vitro study demonstrated a significantly weaker cement-in-cement interface when using an OSCAR-prepared cement mantle versus one prepared with a burr or with no preparation. This difference may be related to a porous zone that was only observed at the cement-in-cement interface for the OSCAR group. Whether this difference influences survival of the revised femoral stem remains unknown, but it should be considered carefully during revision surgery.
Acknowledgments
The authors would like to thank Anthony Townshend for preparing and shear testing all specimens.
Footnotes
Author contributions: A. Liddle: Designed the study, Manufactured the cement specimens, Interpreted the data, Wrote the manuscript.
M. Webb: Designed the study, Manufactured the cement specimens, Wrote the manuscript.
N. Clement: Interpreted the data, Wrote the manuscript.
S. Green: Designed the study, Interpreted the data, Wrote the manuscript.
J. Liddle: Interpreted the data, Wrote the manuscript.
M. German: Designed the study, Interpreted the data, Wrote the manuscript.
J. Holland: Designed the study, Interpreted the data, Wrote the manuscript.
Conflict of interest statement: Stryker provided all cement and mixing apparatus for this study. J. Holland reports lecture payments from Stryker not related to this study, as well as a grant from Zimmer Biomet not related to this study.
Follow us @BoneJointRes
Funding statement
Although none of the authors has received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article, benefits have been or will be received but will be directed solely to a research fund, foundation, educational institution, or other non- profit organization with which one or more of the authors are associated.
References
- 1. Pivec R, Johnson AJ, Mears SC, Mont MA. Hip arthroplasty. Lancet 2012;380:1768-1777. [DOI] [PubMed] [Google Scholar]
- 2. Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg [Am] 2014;96-A:624-630. [DOI] [PubMed] [Google Scholar]
- 3. No authors listed. Patient characteristics for revision hip replacement procedures. National Joint Registry (NJR). http://www.njrreports.org.uk/hips-revision-procedures-patient-characteristics/H19v1NJR?reportid=AB5D4468-323C-4E54-8737-11C7DAA7B75E&defaults=DC__Reporting_Period__Date_Range=%22MAX%22,J__Filter__Calendar_Year=%22MAX%22,H__Filter__Joint=%22Hip%22 (date last accessed 3 May 2019).
- 4. Li PLS, Ingle PJ, Dowell JK. Cement-within-cement revision hip arthroplasty: should it be done? J Bone Joint Surg [Br] 1996;78-B:809-811. [PubMed] [Google Scholar]
- 5. Masri BA, Mitchell PA, Duncan CP. Removal of solidly fixed implants during revision hip and knee arthroplasty. J Am Acad Orthop Surg 2005;13:18-27. [DOI] [PubMed] [Google Scholar]
- 6. Jameson SS, Wilson MJ, Hubble MJW, Devon R. Cement-in-cement femoral component revision in the multiply revised total hip arthroplasty: results with a minimum follow-up of five years. Bone Joint J 2017;99-B:199-203. [DOI] [PubMed] [Google Scholar]
- 7. Keeling P, Prendergast PJ, Lennon AB, Kenny PJ. Cement-in-cement revision hip arthroplasty: an analysis of clinical and biomechanical literature. Arch Orthop Trauma Surg 2008;128:1193-1199. [DOI] [PubMed] [Google Scholar]
- 8. Duncan WW, Hubble MJW, Howell JR, et al. Revision of the cemented femoral stem using a cement-in-cement technique: a five- to 15-year review. J Bone Joint Surg [Br] 2009;91-B:577-582. [DOI] [PubMed] [Google Scholar]
- 9. Cnudde PHJ, Kärrholm J, Rolfson O, Timperley AJ, Mohaddes M. Cement-in-cement revision of the femoral stem: analysis of 1179 first-time revisions in the Swedish Hip Arthroplasty Register. Bone Joint J 2017;99-B(Suppl B):27-32. [DOI] [PubMed] [Google Scholar]
- 10. Wilson LJ, Bell CGR, Weinrauch P, Crawford R. In vitro cyclic testing of the Exeter stem after cement within cement revision. J Arthroplasty 2009;24:789-794. [DOI] [PubMed] [Google Scholar]
- 11. Dang K, Pelletier MH, Walsh WR. Factors affecting flexural strength in cement within cement revisions. J Arthroplasty 2011;26:1540-1548. [DOI] [PubMed] [Google Scholar]
- 12. Holt G, Hook S, Hubble M. Revision total hip arthroplasty: the femoral side using cemented implants. Int Orthop 2011;35:267-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Goldberg SH, Studders EM, Cohen MS. Ultrasonic cement removal in revision arthroplasty. Orthopedics 2007;30:632-635. [DOI] [PubMed] [Google Scholar]
- 14. Weinrauch PC, Bell C, Wilson L, et al. Shear properties of bilaminar polymethylmethacrylate cement mantles in revision hip joint arthroplasty. J Arthroplasty 2007;22:394-403. [DOI] [PubMed] [Google Scholar]
- 15. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175-191. [DOI] [PubMed] [Google Scholar]
- 16. Rudol G, Wilcox R, Jin Z, Tsiridis E. The effect of surface finish and interstitial fluid on the cement-in-cement interface in revision surgery of the hip. J Bone Joint Surg [Br] 2011;93-B:188-193. [DOI] [PubMed] [Google Scholar]
- 17. Greenwald AS, Narten NC, Wilde AH. Points in the technique of recementing in the revision of an implant arthroplasty. J Bone Joint Surg [Br] 1978;60-B:107-110. [DOI] [PubMed] [Google Scholar]
- 18. Lewis G. Properties of acrylic bone cement: state of the art review. J Biomed Mater Res 1997;38:155-182. [DOI] [PubMed] [Google Scholar]
- 19. Goldberg SH, Cohen MS, Young M, Bradnock B. Thermal tissue damage caused by ultrasonic cement removal from the humerus. J Bone Joint Surg [Am] 2005;87-A:583-591. [DOI] [PubMed] [Google Scholar]
- 20. Young J, Vallamshetla VRP, Lawrence T. The polished tri-tapered stem for cement-in-cement revision hip arthroplasty, a reliable and reproducible technique? Hip Int 2008;18:272-277. [DOI] [PubMed] [Google Scholar]