The authors document the process of implementing a mammography reminder system in a group practice. Women not responding to a mailed reminder were more likely to schedule a mammogram during a simple reminder call than during a call that offered counseling.
Keywords: Mammogram, Reminder system, Breast cancer, Screening, Telephone counseling
Abstract
As population health has become a focus of health care payers and providers, interest has grown in mail, phone, and other forms of outreach for improving population rates of cancer screening. Translational research is needed to compare the effectiveness and cost of low- and high-intensity behavioral outreach interventions for promoting cancer screening. The purpose of the article is to compare the effectiveness in promoting biannual mammograms of three interventions delivered over 4 years to a primary care population with a high baseline mammography adherence of 83.3%. We randomized women aged 40–84 to reminder letter only (LO arm), letter + reminder call (RC arm), and two letters + counseling call (CC arm) involving tailored education and motivational interviewing. Mammography adherence (≥1 mammogram in the previous 24 months) at four time points was determined from insurance claims records. Over 4 years, 30,162 women were randomized. At the end of 4 years, adherence was highest in the RC arm (83.0%) compared with CC (80.8%) and LO (80.8%) arms (p = .03). Only 23.5% of women in the CC arm were reached and accepted full counseling. The incremental cost per additional mammogram for RC arm women was $30.45 over the LO arm cost. A simple reminder call can increase screening mammogram adherence even when baseline adherence is high. Some more complex behavioral interventions delivered by mail and phone as in this study may be less effective, due to limited participation of patients, a focus on ambivalence, lack of follow-up, and other factors.
Implications
Practice: To increase adherence to cancer screening, a personalized reminder letter plus reminder call may be cost-effective. Motivational interviewing–based telephone counseling and tailored education should be avoided until research identifies approaches that are engaging and effective.
Policy: Reminder calls to increase cancer screening should be considered as potentially valuable population health improvement measures and explored in selected populations.
Research: Studies are needed to identify more cost-effective ways of increasing adherence to cancer screening than live reminder calls.
INTRODUCTION
Most authorities now recommend screening mammograms every 1–2 years for women aged 50–74 [1–4]. For women aged 40–49 at average risk for breast cancer, recommendations are to start screening at age 45 [4] or consider screening after a discussion of benefits and harms [3, 4]. For women aged 75 and older, recommendations are to stop screening [2] or continue until life expectancy is <10 years [4] after a discussion of benefits and harms [1, 3].
The Healthy People 2020 target for biannual mammographic screening is 81.1% for women aged 50–74 [5]. In 2015, however, rates were 71.3% and 72.2% for women aged 50–64 and 65–74 respectively. To address suboptimal rates of breast and other cancer screenings, health care payers and providers have been reaching out through mail, phone, and other means to patients due or coming due for screenings [6], but the most cost-effective approaches to outreach have not been definitively identified.
Studies of mammography reminder calls have shown a 5–21 percentage points (pct pts) increase in mammogram completion for a live or automated call compared with a mailed reminder [7–11]. Thirteen studies of tailored telephone counseling, mostly among women overdue for mammograms, have shown gains in mammography completion of 3–25 pct pts over a mailed reminder [12–25]. Research, then, has confirmed that telephone outreach can be more effective than mailed reminders, but two key questions remain to be answered: (i) How effective will these efforts be when delivered routinely for several years in large populations with high baseline screening rates? and (ii) How do mailed reminders, telephone reminders, and tailored telephone counseling calls compare in effectiveness and cost in these populations?
Taplin et al. [8] found no significant difference between a reminder call and a counseling call in women unresponsive to a mailed mammography reminder, but screening rates for both calls exceeded the rate for mail alone. Fortuna et al. [10] compared an autodialed reminder call, a live counseling call, and a mailed reminder. The live call increased mammography by 9.7 pct pts (p < .05) compared with 5 pct pts (p > .05) for the autodialed call.
We are not aware of any multiyear studies directly comparing reminder and counseling calls in large health care systems. To address the two questions about outreach calls, we undertook a 4-year randomized controlled trial (RCT) in a large health care system in which women had high baseline mammography rates We compared three methods for promoting biannual mammograms: a mailed reminder, a reminder call with scheduling, and a theory-based counseling call that included tailored education, motivational interviewing (MI), and an offer to schedule a mammogram. MI engages patients in exploring barriers to and facilitators of behavior change [26] and has outperformed advice giving for several behaviors [27–31]. We hypothesized that counseling would outperform the other two interventions.
METHODS
Study description and design
This RCT was implemented from 2010 to 2014 at the Fallon Clinic [later renamed Reliant Medical Group (RMG)] which serves Worcester County (population 785,000) in Massachusetts. During the study period, 95 primary care providers (PCPs) served adult RMG patients.
Study population and randomization
Eligibility criteria were (i) female gender, (ii) age 50–84 (Year 1) and age 40–84 in Years 2–4, (iii) patient of an RMG PCP, (iv) member of Fallon Community Health Plan [later renamed Fallon Health (FH)] for ≥18 months, and (v) no bilateral mastectomy. Eligible patients who declined the interventions and patients excluded by PCPs did not receive letters or calls, but were included in the intention to treat (ITT) analyses. PCPs received lists of women potentially eligible for the study and could exclude patients for any reason. In supporting screening for women aged 40–49 and 75–84, RMG PCPs were following the American Cancer Society’s guideline for breast cancer screening in place during the study [32]. We determined eligibility and accrued patients daily during the entire study period through automated review of RMG databases. Patients stayed in the study until they no longer met eligibility criteria. Accrued patients were randomized to three interventions: letter only (LO arm), letter + a reminder call (RC arm), or two letters + a counseling call (CC arm).
Interventions and fidelity
All women received the same initial reminder letter at study entry if they had no mammogram in the last 18 months and none scheduled. The letter informed women that there was no record of a mammogram in the last 18 months and that RMG providers recommend mammograms every 1–2 years because mammograms are the “best way to find breast cancers that are very small and curable.” Women were invited to call the study office to schedule a mammogram. Additional reminder letters were sent while a woman remained eligible for interventions whenever no mammogram was completed in the last 18 months and none was scheduled for a future date. Women who had received a reminder letter, had no mammogram within 12 months of the letter, and none scheduled in the future received a booster letter and intervention. A woman in the study for 4 years with a mammogram every 18 months received no reminders, while one with no mammograms received a reminder every 12 months.
Women in the RC arm were called 2 weeks after the reminder letter was sent if no mammogram was scheduled. The caller confirmed that the patient was due for a mammogram and offered to schedule one. Women in the CC arm received a second letter and an educational booklet 2 weeks after the first letter if no mammogram was scheduled and a counseling call 1 week later if still no mammogram was scheduled. In both call arms up to five call attempts were made at different times with two voicemail messages requesting a call back “about a test that is coming due.” Details of the content of the interventions are summarized elsewhere [33].
The CC arm counseling protocol drew on the Precaution Adoption Process Model [34] which classifies individuals by stage of readiness for screening, allowing counseling to be tailored to five stages: Unaware (never heard about mammograms), Decided Against, Undecided, Planning, and Scheduled. Based on the stage, counselors offered scripted, tailored education to encourage on-time mammograms and/or MI to (i) help women identify and enhance motivations to have a mammogram, (ii) highlight the discrepancy between their values and nonadherence to screening, and (iii) help women explore and resolve ambivalence about mammography. Women reporting logistical challenges to getting a mammogram received barrier counseling. Counselors could schedule a mammogram on the call when a woman agreed to one following counseling. If a woman declined to engage in counseling, she was then offered the opportunity to schedule a mammogram. The design of a computer-assisted telephone interviewing system supporting the interventions, the training of callers, and call monitoring for protocol fidelity are described elsewhere [33].
Study measures and outcomes
The primary outcome, measured at the end of each study year, was the proportion of women continuously enrolled in FH for ≥24 months with a current RMG PCP who had an FH claim for ≥1 mammogram during the last 24 months. Secondary outcomes in the CC arm were patient engagement in the full counseling protocol and change of stage of readiness from Not Planning to Planning. We calculated the relative decrease in nonadherence by dividing the percentage point increase in adherence by the baseline nonadherence proportion.
Statistical analyses
Data were analyzed using Stata LP, version 14.1 (College Station, TX). Relative frequencies for subject characteristics were calculated for the ITT analytic samples. Longitudinal mixed models, accounting for within-patient correlation, assessed the unadjusted between group differences in mammography adherence from baseline to the end of the last valid period. For women aged 40–49, the baseline year was study Year 2. For women aged 75–84, the last valid measurement year was Year 3 because many older women left FH when FH discontinued their Medicare Advantage Plan. Adjusted odds ratios (OR) and 95% confidence intervals (CI) for factors associated with mammography completion were calculated using logistic regression models that included selected potential confounders. Chi-square statistics quantified differences in mammography completion across arms.
Cost analyses
The cost per completed reminder call and counseling call was based on the duration of a sample of calls and related tasks and the estimated hourly wages for callers. The incremental cost per additional woman up to date with mammography in the RC arm over the LO arm was calculated by equalizing the letter only and reminder call denominators and adjusting the number of women up to date and of completed calls appropriately. The adjusted total cost for completed calls was calculated in Years 2 and 3 for women aged 50–84 and Years 3 and 4 for women aged 40–49. Total direct cost in the RC arm was then divided by the adjusted number of additional women up to date.
Consent processes
Before enrollment women were sent a letter asking them to call a specified number to opt out of interventions. Women in the CC arm were consented for collecting counseling data. The FH/RMG Institutional Review Board approved consent processes and the study protocol.
RESULTS
Primary results
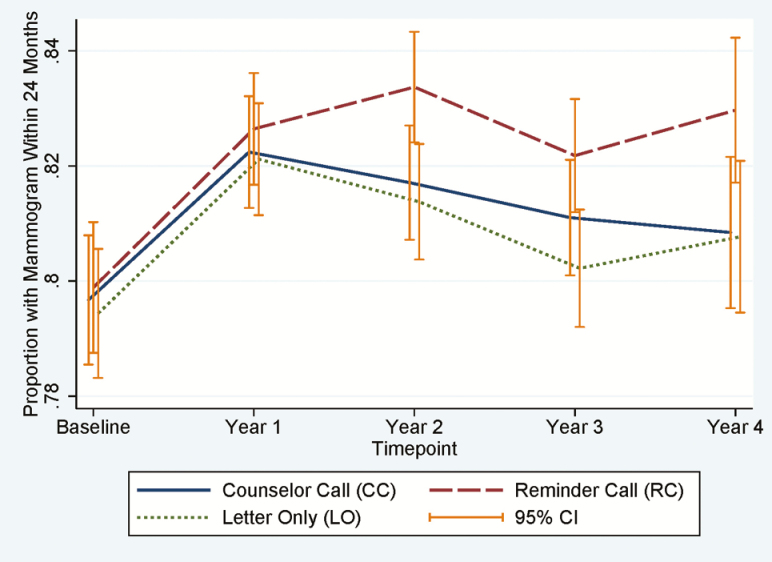
The similar distribution of subject characteristics across the three arms (Table 1) confirms the effectiveness of randomization. The numbers of women initially eligible, excluded from interventions by PCPs, opting out, and receiving reminders are reported elsewhere [33]. The majority of subjects were aged 50–74 and white with commercial or Medicare insurance. The sample sizes in Fig. 1 vary across years because we enrolled women continuously, and those leaving FH or RMG became ineligible. From baseline to the end of Year 1, adherence rose almost 3 pct pts in all arms (Fig. 1). Subsequently, adherence in the RC arm outpaced both the LO and CC arm adherence. RC arm adherence was 2–3 pct pts higher than LO arm adherence from Years 2–4 (p < .05 for all years). At the end of 4 years, adherence was highest in the RC arm (83.0%) compared with CC (80.8%) and LO (80.8%) arms (p = .03) adherence.
Table 1.
Characteristics of the subjects ever active in the study (≥18 months with Fallon Health and with RMG PCP) by arm and selected characteristics
| Characteristics | Study arms | Total (n = 30,160) | ||
|---|---|---|---|---|
| Counseling call (n = 10,054) | Reminder call (n = 10,043) | Letter only (n = 10,063) | ||
| n (%) | n (%) | n (%) | n (%) | |
| Age | ||||
| 40–49 | 2,246 (22.3) | 2,361 (23.5) | 2,244 (22.3) | 6,851 (22.7) |
| 50–59 | 2,511 (25.0) | 2,529 (25.2) | 2,484 (24.7) | 7,524 (24.9) |
| 60–69 | 1,963 (19.5) | 1,967 (19.6) | 1,959 (19.5) | 5,889 (19.5) |
| 70–74 | 1,025 (10.2) | 965 (9.6) | 1,047 (10.4) | 3,037 (10.1) |
| 75–84 | 2,309 (23.0) | 2,221 (22.1) | 2,329 (23.1) | 6,859 (22.7) |
| Race/ethnicity | ||||
| White | 7,355 (73.2) | 7,340 (73.1) | 7,416 (73.7) | 22,111 (73.3) |
| Black or African American | 176 (1.8) | 212 (2.1) | 200 (2) | 588 (1.9) |
| Asian | 175 (1.7) | 152 (1.5) | 164 (1.6) | 491 (1.6) |
| American Indian/Alaskan native | 91 (0.9) | 82 (0.8) | 82 (0.8) | 255 (0.8) |
| Native Hawaiian/other Pacific Islander | 3 (0.0) | 8 (0.1) | 6 (0.1) | 17 (0.1) |
| Other | 31 (0.3) | 36 (0.4) | 30 (0.3) | 97 (0.3) |
| Prefer not to answer or unknown | 2,223 (22.1) | 2,213 (22) | 2,165 (21.5) | 6,601 (21.9) |
| Insurance type | ||||
| FH Commercial | 5,931 (59.0) | 6,035 (60.1) | 6,000 (59.6) | 17,966 (59.6) |
| FH Medicare | 3,613 (35.9) | 3,460 (34.5) | 3,600 (35.8) | 10,673 (35.4) |
| FH Medicaid | 510 (5.1) | 548 (5.5) | 463 (4.6) | 1,521 (5.0) |
| Ever smoked | ||||
| Yes | 3,237 (32.2) | 3,286 (32.7) | 3,168 (31.5) | 9,691 (32.1) |
| No | 3,489 (34.7) | 3,465 (34.5) | 3,564 (35.4) | 10,518 (34.9) |
| Unknown | 3,328 (33.1) | 3,292 (32.8) | 3,331 (33.1) | 9,951 (33.0) |
| Had a mammogram in 24 months prior to study entry | ||||
| No | 3,076 (30.6) | 3,043 (30.3) | 3,047 (30.3) | 9,166 (30.4) |
| Yes | 6,978 (69.4) | 7,000 (69.7) | 7,016 (69.7) | 20,994 (69.6) |
RMG Reliant Medical Group; PCP primary care provier
Fig 1.
Proportion of all active subjects with 24 months Fallon Health (FH) enrollment and a mammogram in the last 24 months by time point and study arm (baseline: n = 14,707; Year 1: n = 17,824; Year 2: n = 17,402; Year 3: n = 17,543; Year 4: n = 10,301). Error bars represent 95% confidence intervals.
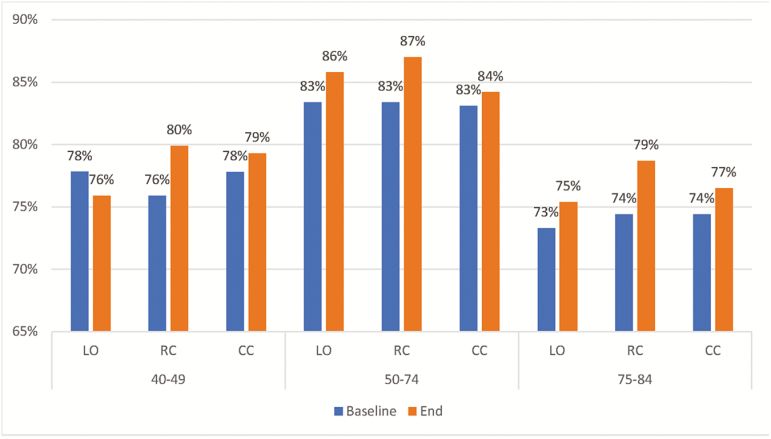
Women in the RC arm had the highest adherence at the end of the last valid period for all ages (Fig. 2). In Table 2, the difference in adherence during the last valid study period between the RC and LO arms, stratified by age, ranges from 1.2 to 4.0 pct pts, and in all age groups is larger than the difference in adherence between CC and LO arms. However, the difference in adherence across arms was statistically significant only in the 50- to 74-year-old group (p = .04). To adjust for differences in baseline adherence across age and arms (Fig. 2), we calculated the absolute change in adherence from baseline to the end of the last valid period (Table 2). The change is greatest in the RC arm, but statistically significant only for women age 40–49 years. The logistic regression analysis in Table 3 compares all arms at the end of Year 4 and shows a 16% relative greater adherence in the RC arm over the LO arm. Adjusted ORs and 95% CIs for Years 1, 2, and 3 comparing RC and LO arms are 1.05 (0.95–1.16), 1.17 (1.05–1.29), and 1.15 (1.05–1.21) respectively and comparing CC and LO arms are 1.01 (0.92–1.11), 1.04 (0.94–1.14), and 1.06 (0.97–1.16). The number of months in the study has a positive association with the outcome.
Fig 2.
Comparison of the percent of women with a mammogram in the last 24 months at baseline and at the end of the last valid study period by age and arm. For age 40–49, baseline is end of Year 1, last valid period is Year 4. For age 50–74, baseline is Year 0, last valid period is Year 4. For age 75–84, baseline is Year 0, last valid period is Year 3. LO letter only arm; RC reminder call arm; CC counseling call arm.
Table 2.
Comparison of mammography adherence across arms at end of last valid period and change in mammography adherence from baseline to end of last valid period by arm and age
| Age | Absolute difference in mammography adherence percentage between call arms and LO arm at end of last valid period | Absolute change in adherence percentage from baseline to end of last valid period | ||||||
|---|---|---|---|---|---|---|---|---|
| LO | RC | CC | p Value | LO | RC | CC | p Value | |
| 40–49a | Ref. | +4.0 | +3.4 | 0.05 | –1.3 | +4.0 | +1.5 | 0.03 |
| 50–74b | Ref. | +1.2 | –1.6 | 0.04 | +1.6 | +3.3 | +1.1 | 0.69 |
| 75–84c | Ref. | +3.3 | +1.1 | 0.10 | +2.1 | +4.3 | +2.1 | 0.43 |
CC counseling call arm; LO letter only arm; RC reminder call arm.
aBaseline is end of Year 1, last valid period is Year 4.
bBaseline is Year 0, last valid period is Year 4.
cBaseline is Year 0, last valid period is Year 3.
Table 3.
Unadjusted and logistic regression adjusted associations of subject characteristics and intervention arms with mammography adherence at the end of Year 4
| Characteristics | Odds ratio | ||
|---|---|---|---|
| Unadjusted | Adjusted | 95% CIa | |
| Study arm | |||
| CC vs. LO | 1.01 | 1.00 | 0.88–1.13 |
| RC vs. LO | 1.16 | 1.16 | 1.02–1.31 |
| Age | |||
| 40–49 vs. 50–74 | 0.61 | 0.75 | 0.66–0.85 |
| 75–84 vs. 50–74 | 0.34 | 0.34 | 0.28–0.42 |
| Insurance | |||
| FH Medicaid vs. FH Commercial | 0.58 | 0.67 | 0.44–1.01 |
| FH Medicare vs. FH Commercial | 0.63 | 0.90 | 0.75–1.08 |
| Months in study | |||
| 12–23 vs. 0–11 | 2.57 | 2.48 | 1.95–3.15, |
| 24–35 vs. 0–11 | 2.75 | 2.71 | 2.14–3.43 |
| 36–48 vs. 0–11 | 3.54 | 3.67 | 3.00–4.50 |
CC counseling call arm; CI confidence interval; FH Fallon Health; LO letter only arm; RC reminder call arm.
aFor adjusted odds ratio.
Secondary results
The relative decrease in nonadherence in the RC arm from baseline to the end of the last valid period was 16.6%, 21.1%, and 16.8% for the 40–49, 50–74, and 75- to 84-year-old age groups respectively. Overall only 443 (23.5%) of 1,887 women in the CC arm receiving a first reminder completed the counseling protocol because of wrong numbers, nonresponse, and limited interest in discussing mammograms. Only 20.5% of 156 women not planning a mammogram at the beginning of counseling were moved to planning one after counseling. A report of the response to letters, reminder calls, and counseling calls is available elsewhere [33].
The cost for a reminder call that reached a patient was $7.80 and for a counseling call $11.15, based on an hourly wage of $17.62 for RC arm callers and $24.51 for counselors. The incremental cost per additional woman up to date at the end of the last valid measurement year in the RC arm was $28.05 for women aged 40–49, $33.16 for those aged 50–74, and $34.39 for those aged 75–84.
DISCUSSION AND CONCLUSION
Discussion
A key objective of this study was to compare the effectiveness of theory-based, scripted, and computer-supported telephone counseling to a reminder call for promoting mammography when the interventions are delivered repeatedly in a population with a high mammography rate. We found that reminder calls were more effective than counseling calls and letters alone in all age groups from Years 2–4, although not all differences were statistically significant. At the end of the study, the 40–49-year-old group had the largest difference between the RC and LO arms (4.0 pct pts, p = .05) and those aged 50–74 the least (1.2 pct pts, p = .04). The relative decrease in nonadherence during the study ranged from 16.6% to 21.1% across age groups in the RC arm. The lower adherence in the 40–49 and 75–84-year-old groups was expected, given that some authorities presented screening mammography for these age groups as an option to be considered and not as a service recommended for all [1–4].
Most studies of interventions to promote mammography have enrolled only women overdue for a mammogram and have measured outcomes ≤12 months from interventions. Three studies compared a reminder call following a mailed reminder to a mailed reminder with follow-up of 3.5–12 months [7–9]. Mammography rates ranged from 51.8% to 64.3% in the call groups and were higher than in the mail groups by 9–21 pct pts. An autodialed reminder call following a mailed reminder yielded a 22.8% mammography rate, 5 pct pts greater than for a mailed reminder [10]. An autodialed call alone compared with a mailed reminder in women with a prior mammogram achieved a mammography rate of 4.5 pct pts over a mailed reminder (76.3% vs. 71.8%) [11]. In seven studies, a reminder letter followed by a counseling call was compared with a mailed reminder with follow-up of 3–12 months. In the call groups, mammography rates ranged from 7.8% to 49.2% (2–24 pct pts higher than for mail only) [10, 13–17]. The variation in outcomes across these studies may be due to variation in duration of follow-up, age, education, socioeconomic status, prior mammogram experience, and mammography rate in the source population. But given that mammography rates for all types of calls were 2–24 pct pts higher than for mail only in 12 studies (median +13 pct pts), it is reasonable to conclude that calling women overdue for a mammogram usually will increase mammography use The Community Preventive Services Task Force has reported that multicomponent interventions increased mammography by a median of 6.2 pct pts compared with controls. Multicomponent interventions included two or more interventions aimed at increasing (i) patient demand, (ii) provider delivery, and/or (iii) access to screening [35].
Comparison of our effect sizes with those of other studies of telephone counseling or reminding is complicated by our use of a population-based outcome with a 2-year window rather than an outcome based on follow-up of only women overdue for a mammogram at baseline. We can estimate an outcome measure comparing the RC and LO arms that is comparable with that used in these other studies if we take as the denominator the proportion of women nonadherent in the LO arm at the end of Year 4 (.192) and as the numerator the difference between RC and LO arm adherence (.025). The estimated outcome of 13 pct pts is the same as the median outcome in the 12 studies reported above. The outcome represents the difference in adherence between a virtual cohort of women in the LO arm with 0% adherent after 2 years and a cohort in the RC arm with adherence of 13%.
Only two studies have reported population outcomes for mail + telephone counseling compared with mailed reminders in large health plans [18, 24]. Costanza et al. reported a gain of 2 pct pts in repeat mammography adherence (≥2 mammograms in a 4-year period) for a counseling call following a reminder mailing compared with a mailed reminder. Luckmann et al. reported percentage point gains in mammography in a 12-month period of 3.1 and 4.9 points in two health plan populations when a counseling call was added to a mailed reminder. These gains for counseling calls are similar to the RC arm effect sizes we found, providing further support for the occlusion that reminder calls may be at least as effective as counseling calls.
Contrary to our main hypothesis, women of all ages in the CC arm had lower adherence in the last valid study period than women in the RC arm. The only other study directly comparing a live counseling call to a reminder call for women unresponsive to a mailing also showed no significant differences in mammography 12 months after the interventions in women overdue for screening (49.8% for counseling, 51.8% for reminder, hazard ratio = 0.97; 95% CI = 0.8–1.2) compared with 35.4% in the mail only group [8]. The counseling protocol included MI, as did our protocol. The study reported by Fortuna et al. allows an indirect comparison of an autodialed reminder call and a live counseling call and shows a 4.7 pct pts gain for the live over the autodialed call, possibly explained by access to immediate mammogram scheduling on the live call [10].
There are several possible explanations for the ineffectiveness of the CC arm intervention in our study. First, only 23.5% of women in the CC arm received the full counseling intervention in the first round of calls because many women were not reached or declined an invitation to discuss mammograms. Others have reported that women asked to address mammography during a clinic visit have declined to engage with providers [36]. The reminder callers in our study, on the other hand, had a simple, brief message, uncluttered by a possibly distracting invitation to discuss mammograms. Opening a call with an invitation to schedule a mammogram may be as or more effective than asking for permission to discuss breast cancer screening, being turned down, and then offering to schedule a mammogram. In other studies of telephone counseling, it is likely that counselors did not ask permission to begin counseling, and it is possible they may have drawn more women into a discussion of mammograms than our counselors did Another reason for failure of the CC intervention among women who did receive full counseling is that a single MI session may have been insufficient to influence them. Studies of MI show a dose–response relationship between the number of MI sessions and outcomes [37, 38]. For recommended preventive measures, exploring ambivalence, a mainstay of many MI protocols, may reduce motivation [38]. Presenting information in didactic formats as in the CC arm print materials may have contributed to counter-arguing [39], and information about the risk of breast cancer could have elicited uncomfortable emotions that reduced motivation to pursue a mammogram.
The duration of time in the study was strongly associated with mammography adherence in all arms. This suggests that for women in the study for 2 years or longer, mammography rates increased over time. We are exploring this in an analysis limited to women remaining in the study for 4 years. Other studies have demonstrated that telephone reminders or counseling can increase repeated mammogram use over a period of years [11, 24]. The increase in adherence during Year 1 in all arms (Fig. 1) could reflect the change in mailed reminders for the 50- to 74-year-old women to our letter, signed by a woman’s PCP and sent 18 months after their last mammogram, from an FH letter not keyed to an upcoming mammogram due date nor signed by the PCP. For 40–49 and 75–84-year-old women, their first experience with any mammography reminder letter came in this study. Other studies have shown that tailored letters, often from a PCP, are more effective than generic letters [40].
Cost of the RC intervention
In two studies comparing mailed reminders + counseling calls to usual care, the call groups had mammography rates of 17 and 41 pct pts over usual care at incremental costs of $125 per mammogram [41] and $0.78 per 1 pct pt increase in mammography [25]. Both studies included some costs which we did not (e.g., computer programming). Differences in study design and methods preclude a direct comparison with our finding of an additional $28–$34 per woman up to date in the RC arm compared with the LO arm.
Limitations
The main limitations of this study are the socioeconomic and racial/ethnic homogeneity of the population, the high baseline adherence rates, and our inability, due to budget constraints, to interview women who refused counseling or calls. Future studies should include more diverse populations with adherence rates more representative of the general population and should plan to gather data on women refusing counseling or calls.
Conclusions
In populations with high mammography utilization, some women may need and respond to a reminder call to adhere to screening recommendations. The result may be a small but possibly cost-effective increase in adherence over a reminder letter. Providing a second letter and educational materials before a call that includes tailored education and counseling may not substantially increase mammography adherence, possibly because most women do not engage in counseling, and counseling including MI may have limited effectiveness. Women aged 40–49 and 75–84 should be engaged in a shared decision-making discussion about breast cancer screening before being encouraged to schedule a mammogram.
Acknowledgments
We thank Devi Sundaresan for her data management support and Kathleen Allain, Ariel Berk, Meaghan Fair, Belinda James, Brenda Kniskem, and Kathleen Matthews for their assistance in implementing the interventions. We thank George Reed for his work as senior statistical consultant in the early phases of the study and Robin Clark for his assistance in collecting and analyzing data on cost. We thank Scott Pilate and his Reliant Medical Group (RMG) Information Services staff for their dedication to meeting our challenging IT needs and Beth Foley for facilitating access to Fallon Health (FH) claims data. We thank the RMG and FH administration for providing access to their systems and patients. This work was supported by Grant R01CA132935 from the National Cancer Institute. The findings reported have not been previously published and this manuscript is not being simultaneously submitted elsewhere. No data previously published are presented, but appropriate reference is made to findings from a process study published in Translational Behavioral Medicine when the process findings help explain our reported outcomes (Transl Behav Med. 2017. Apr 27. doi:10.1007/s13142-017-0497-x. [Epub ahead of print] PMID: 28452044).
Conflict of Interest: There are no actual or potential conflicts of interest with the organization that sponsored the research.
Compliance With Ethical Standards
Primary Data: The authors have full control of all primary data and agree to allow the journal to review their data if requested.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. No animal experimental subjects were used in this research. The study was approved by the Reliant Medical Group/Fallon Health Institutional Review Board.
Informed Consent: Informed consent was obtained from all individual participants included in the study. The informed consent process was involved passive consent as stated in the manuscript.
References
- 1. The American College of Obstetricians and Gynecologists. Practice bulletin no. 122: Breast cancer screening. Obstet Gynecol. 2011;118(2 pt 1):372–382. [DOI] [PubMed] [Google Scholar]
- 2. Wilt TJ, Harris RP, Qaseem A; High Value Care Task Force of the American College of Physicians Screening for cancer: Advice for high-value care from the American College of Physicians. Ann Intern Med. 2015;162(10):718–725. [DOI] [PubMed] [Google Scholar]
- 3. US Preventive Services Task Force. Final recommendation statement on breast cancer screening 2016. Available at http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening1#preface. Accessibility verified June 12, 2016.
- 4. Oeffinger KC, Fontham ET, Etzioni R, et al. ; American Cancer Society. Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-term Trends in Health. U.S. Department of Health and Human Services DHHS Publication No. 2017-1232. Hyattsville, MD; 2017 [PubMed] [Google Scholar]
- 6. Perez B, Szekendi MK, Taylor-Clark K, Vaughn J, Susman K. Advancing a culture of health: Population health programs in place at essential hospitals and academic medical centers (2012–2014). J Healthc Qual. 2016;38(2):66–75. [DOI] [PubMed] [Google Scholar]
- 7. Chaudhry R, Scheitel SM, McMurtry EK, et al. . Web-based proactive system to improve breast cancer screening: A randomized controlled trial. Arch Intern Med. 2007;167(6):606–611. [DOI] [PubMed] [Google Scholar]
- 8. Taplin SH, Barlow WE, Ludman E, et al. . Testing reminder and motivational telephone calls to increase screening mammography: A randomized study. J Natl Cancer Inst. 2000;92(3):233–242. [DOI] [PubMed] [Google Scholar]
- 9. Bodiya A, Vorias D, Dickson HA. Does telephone contact with a physician’s office staff improve mammogram screening rates?Fam Med. 1999;31(5):324–326. [PubMed] [Google Scholar]
- 10. Fortuna RJ, Idris A, Winters P, et al. . Get screened: A randomized trial of the incremental benefits of reminders, recall, and outreach on cancer screening. J Gen Intern Med. 2014;29(1):90–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. DeFrank JT, Rimer BK, Gierisch JM, Bowling JM, Farrell D, Skinner CS. Impact of mailed and automated telephone reminders on receipt of repeat mammograms: A randomized controlled trial. Am J Prev Med. 2009;36(6):459–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Carney PA, Harwood BG, Greene MA, Goodrich ME. Impact of a telephone counseling intervention on transitions in stage of change and adherence to interval mammography screening (United States). Cancer Causes Control. 2005;16(7):799–807. [DOI] [PubMed] [Google Scholar]
- 13. Champion V, Maraj M, Hui S, et al. . Comparison of tailored interventions to increase mammography screening in nonadherent older women. Prev Med. 2003;36(2):150–158. [DOI] [PubMed] [Google Scholar]
- 14. Dalessandri KM, Cooper M, Rucker T. Effect of mammography outreach in women veterans. West J Med. 1998;169(3):150–152. [PMC free article] [PubMed] [Google Scholar]
- 15. Davis NA, Nash E, Bailey C, Lewis MJ, Rimer BK, Koplan JP. Evaluation of three methods for improving mammography rates in a managed care plan. Am J Prev Med. 1997;13(4):298–302. [PubMed] [Google Scholar]
- 16. Hegenscheid K, Hoffmann W, Fochler S, et al. . Telephone counseling and attendance in a national mammography-screening program a randomized controlled trial. Am J Prev Med. 2011;41(4):421–427. [DOI] [PubMed] [Google Scholar]
- 17. Rimer BK, Halabi S, Sugg Skinner C, et al. . Effects of a mammography decision-making intervention at 12 and 24 months. Am J Prev Med. 2002;22(4):247–257. [DOI] [PubMed] [Google Scholar]
- 18. Luckmann R, Savageau JA, Clemow L, Stoddard AM, Costanza ME. A randomized trial of telephone counseling to promote screening mammography in two HMOs. Cancer Detect Prev. 2003;27(6):442–450. [DOI] [PubMed] [Google Scholar]
- 19. Champion V, Maraj M, Hui S, et al. . Comparison of tailored interventions to increase mammography screening in nonadherent older women. Prev Med. 2003;36(2):150–158. [DOI] [PubMed] [Google Scholar]
- 20. Page A, Morrell S, Chiu C, Taylor R, Tewson R. State co-ordination unit recruitment to mammography screening: A randomized trial and meta-analysis of invitation letters and telephone calls. Aust N Z J Public Health. 2006;30(2):111–118. [DOI] [PubMed] [Google Scholar]
- 21. Davis NA, Lewis MJ, Rimer BK, Harvey CM, Koplan JP. Evaluation of a phone intervention to promote mammography in a managed care plan. Am j Health Promot. 1997;11(4):247–249. [DOI] [PubMed] [Google Scholar]
- 22. King ES, Rimer BK, Seay J, Balshem A, Engstrom PF. Promoting mammography use through progressive interventions: Is it effective?Am J Public Health. 1994;84(1):104–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Costanza ME, Stoddard AM, Luckmann R, White MJ, Spitz Avrunin J, Clemow L. Promoting mammography: Results of a randomized trial of telephone counseling and a medical practice intervention. Am J Prev Med. 2000;19(1):39–46. [DOI] [PubMed] [Google Scholar]
- 24. Saywell RM Jr, Champion VL, Skinner CS, Menon U, Daggy J. A cost-effectiveness comparison of three tailored interventions to increase mammography screening. J Womens Health (Larchmt). 2004;13(8):909–918. [DOI] [PubMed] [Google Scholar]
- 25. Romano M, Peters L. Evaluating the mechanisms of change in motivational interviewing in the treatment of mental health problems: A review and meta-analysis. Clin Psychol Rev. 2015;38(6):1–12. [DOI] [PubMed] [Google Scholar]
- 26. Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: A systematic review and meta-analysis. Br j Gen Pract. 2005;55(513):305–312. [PMC free article] [PubMed] [Google Scholar]
- 27. Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1(1):91–111. [DOI] [PubMed] [Google Scholar]
- 28. Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71(5):843–861. [DOI] [PubMed] [Google Scholar]
- 29. Everett B, Davidson PM, Sheerin N, Salamonson Y, DiGiacomo M. Pragmatic insights into a nurse-delivered motivational interviewing intervention in the outpatient cardiac rehabilitation setting. J Cardiopulm Rehabil Prev. 2008;28(1):61–64. [DOI] [PubMed] [Google Scholar]
- 30. VanBuskirk KA, Wetherell JL. Motivational interviewing with primary care populations: A systematic review and meta-analysis. j Behav Med. 2014;37(4):768–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Smith RA, Cokkinides V, Brooks D, Saslow D, Brawley OW. Cancer screening in the United States, 2010: A review of current American Cancer Society guidelines and issues in cancer screening. ca Cancer J Clin. 2010;60(2):99–119. [DOI] [PubMed] [Google Scholar]
- 32. Luckmann R, White MJ, Costanza ME, et al. . Implementation and process evaluation of three interventions to promote screening mammograms delivered for 4 years in a large primary care population. Transl Behav Med. 2017;7(3):547–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Weinstein ND, Sandman PM. A model of the precaution adoption process: Evidence from home radon testing. Health Psychol. 1992;11(3):170–180. [DOI] [PubMed] [Google Scholar]
- 34. US Community Preventive Services Task Force. The Community Guide Available at https://www.thecommunityguide.org/sites/default/files/assets/OnePager-CancerScreening-Multicomponent-BreastCancer.pdf. Accessibility verified January 7, 2018.
- 35. Valanis BG, Glasgow RE, Mullooly J, et al. . Screening HMO women overdue for both mammograms and pap tests. Prev Med. 2002;34(1):40–50. [DOI] [PubMed] [Google Scholar]
- 36. Hardcastle SJ, Taylor AH, Bailey MP, Harley RA, Hagger MS. Effectiveness of a motivational interviewing intervention on weight loss, physical activity and cardiovascular disease risk factors: A randomised controlled trial with a 12-month post-intervention follow-up. Int J Behav Nutr Phys Act. 2013;10(3):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Butler CC, Simpson SA, Hood K, et al. . Training practitioners to deliver opportunistic multiple behaviour change counselling in primary care: A cluster randomised trial. BMJ. 2013;346(3):1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kreuter MW, Holmes K, Alcaraz K, et al. . Comparing narrative and informational videos to increase mammography in low-income African American women. Patient Educ Couns. 2010;81(suppl):S6–S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wagner TH. The effectiveness of mailed patient reminders on mammography screening: A meta-analysis. Am j Prev Med. 1998;14(1):64–70. [DOI] [PubMed] [Google Scholar]
- 40. Vogt TM, Glass A, Glasgow RE, La Chance PA, Lichtenstein E. The safety net: A cost-effective approach to improving breast and cervical cancer screening. J Womens Health (Larchmt). 2003;12(8):789–798. [DOI] [PubMed] [Google Scholar]
- 41. Menon U, Belue R, Wahab S, et al. . A randomized trial comparing the effect of two phone-based interventions on colorectal cancer screening adherence. Ann Behav Med. 2011;42(3):294–303. [DOI] [PMC free article] [PubMed] [Google Scholar]