Abstract
A 32‐year‐old woman was referred to our hospital because of severe psychosis and was found to have an ectopic ACTH‐producing thymic neuroendocrine tumor. Laboratory data revealed an elevated serum cortisol and plasma ACTH level, hypokalemia, and metabolic alkalosis. Chest computed tomography (CT) revealed an anterior mediastinal mass and multiple pulmonary nodules. As the patient was unable to communicate because of her consciousness disturbance, she was managed with artificial ventilation and deep sedation. Metyrapone and potassium supplementation were administered, and steroid psychosis gradually improved. Thoracic surgery was performed and the histopathological diagnosis was thymic neuroendocrine tumor with positive anti‐ACTH immunohistochemical staining. Here we present details of the case and review the literature.
Keywords: Mediastinal carcinoid, mental disorder, neuroendocrine carcinoma, pulmonary metastasis, severe psychosis
Introduction
Ectopic adrenocorticotropic hormone (ACTH) secretion syndrome is a rare clinical manifestation, but is responsible for 15% of all cases of Cushing syndrome.1 The most common ectopic ACTH‐producing tumors are thoracic (bronchial and thymic) and gastroenteropancreatic neuroendocrine tumors (NET), followed by medullary thyroid carcinoma, small cell lung cancer, and pheochromocytoma.2, 3, 4
In general, the symptoms of Cushing syndrome include moon face, proximal muscle fatigue, skin pigmentation, uncontrolled hypertension, and diabetes. However, the intensity of symptoms in patients with ectopic ACTH‐producing tumors is dependent on the serum cortisol levels and the growth rate of the tumor. The clinical manifestations are varied in patients with ectopic ACTH‐producing tumors.1, 2, 3, 4
Psychiatric disturbances are frequently seen in patients with Cushing syndrome, the most common of which are depression and impaired cognition.1, 5 Severe psychosis related to increased cortisol secretion, such as emotional lability or mental disturbance, is rare, especially as the initial clinical manifestation of ectopic ACTH‐producing tumors.
We encountered a case of ectopic ACTH‐producing thymic NET initially presenting with severe psychosis that required artificial ventilation and deep sedation. Following improvement of psychosis with an inhibitor of adrenal corticosteroid synthesis, the patient continued treatment for the primary disease. Here, we describe the clinical course along with a brief review of the relevant literature.
Case report
A 32‐year‐old woman was referred to our hospital with severe psychosis. Three months previously, her family recognized emotional changes in the patient, such as euphoria and/or depression. She progressed to cognitive decline, insomnia, and whole‐body edema developed one week before visiting another hospital. On admission to the other hospital, initial endocrine investigations revealed high ACTH (545 pg/mL) and cortisol (136 μg/dL) levels. Computed tomography (CT) showed an anterior mediastinal mass and multiple pulmonary nodules (Fig 1a,b). As ectopic ACTH‐producing mediastinal tumor with pulmonary metastasis was suspected, metyrapone was administered at an initial dose at 250 mg/day, which was gradually increased to 750 mg/day. However, she lost the ability to communicate due to consciousness disturbance within one week of hospitalization. Therefore, she was transferred to the emergency unit of our hospital. Physical examination on admission revealed moon face and proximal muscle weakness. Body height and weight were 164 cm and 55 kg, respectively and her bodyweight had not altered during the previous few months. Blood pressure was 116/61 mmHg. She had emotional lability and impaired memory. Laboratory findings at our hospital demonstrated severe hypokalemia and metabolic alkalosis, in addition to the increase in serum ACTH and cortisol levels (Table 1). She showed self‐injurious behavior, and attempted to bite her tongue. Due to her severe psychosis and consciousness disturbance, intubation was required and she was sedated in the intensive care unit. Metyrapone was increased to the maximal dose of 4000 mg/day via nasogastric tube. In addition, potassium supplementation was performed at 200 mEq/day and spironolactone was used to control low potassium levels. On day 8, we added perospirone hydrochloride hydrate to propofol sedation to suppress restlessness (Fig 2). Thoracic surgery was performed for the lung nodule. Hematoxylin and eosin staining of the resected specimen indicated irregularly‐shaped sheets and nests of tumor cells, and a diagnosis of NET was made (Fig 3). Immunohistochemical staining revealed tumor cells positive for ACTH, chromogranin A, and synaptophysin. The Ki‐67 labeling index was <1%., indicating that cancer staging by the WHO classification was neuroendocrine tumor G1. The time course of changes in serum cortisol levels is shown in Figure 3. As cortisol levels decreased after initiation of metyrapone, her conscious disturbance improved. She became able to communicate and was extubated on day 14 of hospitalization. Somatostatin receptor scintigraphy was performed and showed abnormal accumulation in the anterior mediastinal mass (Fig 4a) but not in the pulmonary nodules (Fig 4b). There were no other metastatic organs, including the brain. Resection of the anterior mediastinal tumor and the largest metastatic lesion of the right lung were subsequently performed through a median sternotomy to decrease serum ACTH level as much as possible. The pathological findings, including immunological staining, in the mediastinal tumor were similar to the initially resected left lung tumor and confirmed that the tumor was thymic in origin. Thus, according to the WHO classification in 2018, a diagnosis of NET of the thymus (typical carcinoid) with multiple pulmonary metastases was made. Postoperatively, a combination of octreotide long‐acting repeatable (LAR; 30 mg) every four weeks and everolimus (10 mg/day) therapy has been continued, and ACTH and cortisol levels have remained stable. There was no personal or family history of multiple endocrine neoplasia type I in the present case.
Figure 1.
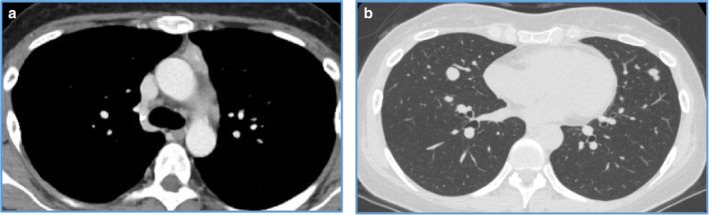
Computed tomography (CT) showed an anterior mediastinal mass (a), mediastinal lymph node and multiple pulmonary nodules (b).
Table 1.
Laboratory data on admission to our hospital
| Hematology | Hormone date | ||||
| WBC | 8710 | /μL | ACTH | 356.0 | pg/mL |
| RRC | 383 | × 104/μL | Cortisol | 65.3 | μg/dL |
| Hb | 14.1 | g/dL | Free T3 | 1.54 | pg/mL |
| PLT | 14.2 | × 104/μL | Free T4 | 1.30 | ng/dL |
| Biochemistry | TSH | 0.60 | μIU/mL | ||
| TP | 6.2 | g/dL | ALD | 53.4 | pg/mL |
| Alb | 3.7 | g/dL | ARC | 2.2 | pg/mL |
| AST | 28 | IU/L | DHEA‐S | 804.0 | μg/dL |
| ALT | 49 | IU/L | Blood gas | ||
| γGTP | 35 | U/L | pH | 7.73 | |
| T‐Bil | 1.13 | mg/dL | pO2 | 143 | mmHg |
| ALP | 141 | U/L | pCO2 | 28.3 | mmHg |
| LDH | 390 | U/L | HCO3 ‐ | 38.6 | mEq/L |
| BUN | 13.0 | mg/dL | BE | 16.7 | mEq/L |
| Cre | 0.49 | mg/dL | Anion gap | 9.5 | mEq/L |
| Na | 141 | mEq/L | |||
| K | 2.8 | mEq/L | |||
| Cl | 90 | mEq/L | |||
| CRP | 0.07 | mg/dL |
Figure 2.
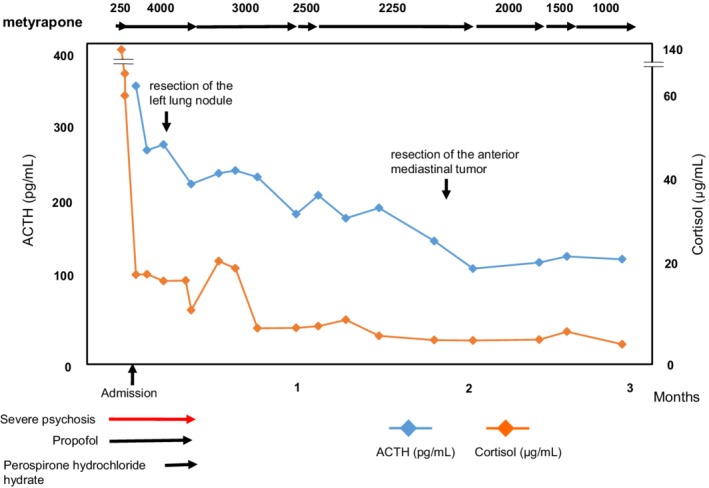
Alterations in serum cortisol and ACTH levels during the clinical course.
Figure 3.
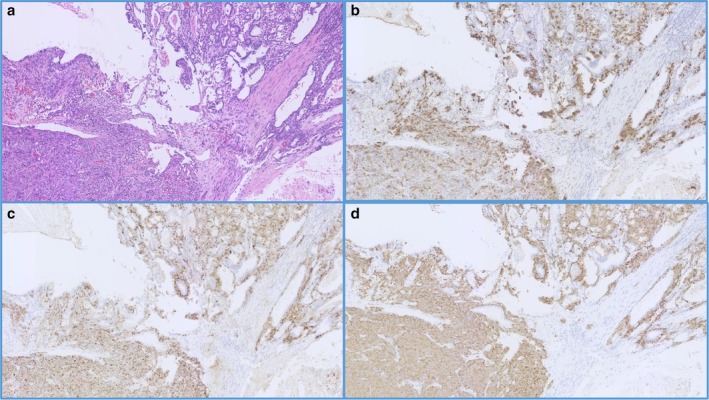
Hematoxylin and eosin staining of the resected specimen showed irregularly‐shaped sheets and nests of tumor cells (a). Immunohistochemical staining revealed tumor cells positive for ACTH (b), chromogranin A (c), and synaptophysin (d).
Figure 4.
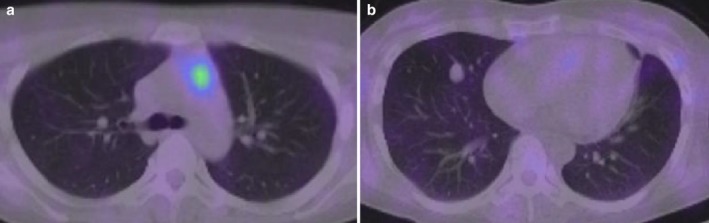
Somatostatin receptor scintigraphy showed abnormal accumulation in the anterior mediastinal mass (a) and pulmonary lesions (b).
Discussion
Here we report on a case of ectopic ACTH‐producing thymic NET. It is noteworthy that the patient developed hypercortisolemia‐induced psychosis that required artificial ventilation and deep sedation before diagnosis. The clinical manifestation of severe psychosis in ectopic ACTH‐producing tumors, especially at initial clinical presentation, is extremely rare in clinical practice.
Thymic NET accounts for approximately 2–4% of all anterior mediastinal tumors.6, 7 The prevalence of ectopic ACTH syndrome in all NETs was estimated to be 3.2%.1 The proportion in gastroenteropancreatic NETs was greater than thoracic (lung/bronchus and thymic) NETs. However, the prevalence of ectopic ACTH syndrome in thoracic NETs was significantly higher than that in gastroenteropancreatic NETs.1, 3 Thus, although ectopic ACTH‐producing thymic NET is extremely rare, the disease associated with ectopic ACTH syndrome should be noted in clinical practice. Based on the results of a PubMed search, Neary et al. 8 reported that the median age in patients with thymic NET associated with ACTH syndrome was 34 years, ranging from two to 75 years, and the male to female ratio was 1.5:1. Wick et al. 9 reported that thymic NET associated with ACTH syndrome had a higher 10‐year mortality rate than those without endocrinopathy (65% vs. 29%).9 Moran et al. 10 examined 80 NET patients and reported that patients with NET of the thymus and Cushing syndrome had a relatively poor prognosis.10 Based on a case series study, the median time to death was 35 months.8 In addition, several studies suggested that thymic NET associated with ACTH syndrome was an aggressive disease and/or had poor prognosis, particularly in young patients.8, 10, 11, 12
With regard to the psychiatric disturbance in patients with Cushing syndrome, insomnia, impaired cognition, memory disturbance, and depression have been reported at a frequency of <20%.1 Although our patient previously visited another hospital with insomnia and physical edema, she developed severe psychosis after hospitalization, resulting in the requirement for artificial ventilation and deep sedation. To our knowledge, only three similar cases have been reported previously.13, 14, 15 Similar to our case, psychotic symptoms were observed on diagnosis of ectopic ACTH syndrome in these previously reported cases. The serum cortisol level at diagnosis in the present case was higher than in the previous case reports. We have summarized case reports and reviewed patients with ACTH‐producing thymic tumors over the past 10 years published in English,8, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24 and the cortisol and ACTH levels are presented in Table 2. Serum cortisol and plasma ACTH levels in our patient were relatively high, and we speculated that the extremely high cortisol level could have been related to the development of severe psychosis.
Table 2.
Case reports and case series in ACTH‐producing thymic tumors over the past 10 years (published in English)
| Case | Authors | Year of publication | Age | Sex | Tumor type | Cortisol (μg/dL) | ACTH (pg/mL) |
|---|---|---|---|---|---|---|---|
| 1 | Sato et al. 16 | 2010 | 56 | F | Atypical thymic carcinoid | 29 | 258 |
| 2 | Saito et al. 17 | 2011 | 38 | M | Large cell NEC of the thymus | 34.1 | 140 |
| 3 | Neary et al. 8 | 2012 | Review (n = 12) | Thymic NET | — | 149 (median) | |
| 4 | Somasundarm et al. 18 | 2013 | 34 | F | Thymic carcinoid | 32.4 | 130 |
| 5 | Barbieri et al. 19 | 2013 | 61 | M | Typical thymic carcinoid | — | 152 |
| 6 | Sekiguchi et al. 20 | 2015 | 32 | F | Thymic NET | 39.2 | 68.7 |
| 7 | Chen et al. 21 | 2016 | Review (n = 16) | Atypical thymic carcinoid/typical thymic carcinoid | 46.4 (median) | 197 (median) | |
| 8 | Oda et al. 22 | 2017 | 44 | M | Large cell NEC of the thymus | 49.1 | 354.1 |
| 9 | Fujiwara et al. 23 | 2018 | 10 | M | Typical thymic carcinoid | 107.7 | 1100 |
| 10 | Jibran et al. 12 | 2018 | 11 | M | Thymic NET | 28.2 | 105.1 |
| 11 | Szczepanek‐Parulska et al. 24 | 2018 | 25 | F | Thymic NET | 63.4 | 268 |
| 12 | Our case | 32 | F | Thymic NET | 136 | 545 | |
In addition, it is reported that the mean interval from the first clinical complaints to the diagnosis of ectopic ACTH syndrome was 11 months in patients with thymic NET,1 and the interval ranged from six months to eight years in other reports.1, 3, 8, 11 The interval in the present case was three months. The relatively short interval to onset and the markedly increased serum cortisol level may have been related to the development of psychotic symptoms in the present case. It is well known that the biological activities in thymic NETs are indolent, but hormonogenesis from the tumor cells may be intermittent or independent secretion with tumor growth.8, 11 Clinicians should be aware of the presence of psychosis disturbance at initial clinical presentation in patients with Cushing syndrome, although the physical signs, such as moon face, central obesity, and pigmentation of hypercortisolism are the predominant features.
Surgery is the most effective treatment for thymic NETs, even in patients with Cushing syndrome.3, 6, 7 However, it has been shown that thymic NETs exhibited more advanced or metastatic disease at the initial diagnosis compared with other NETs,1, 3, 8 which was also similar to our case. Therefore, medical management could play an important role in the treatment of thymic NETs. Based on large placebo‐controlled phase III studies, Frzio et al. 25 performed subgroup analysis and reported that everolimus improved progression‐free survival in cases of advanced lung/thymic NET by 2.4‐fold, compared with the placebo group. Our patient was treated with everolimus plus LAR and achieved stable disease. There is a lack of information or clinical experience available regarding the efficacy of chemotherapy in inoperable and metastatic thymic NET producing ACTH. Further case studies and/or clinical experience are required to determine the efficacy of chemotherapy.
In conclusion, we describe a case of ectopic ACTH‐producing thymic neuroendocrine tumor initially presenting with severe psychosis. ACTH‐producing thymic neuroendocrine tumor is extremely rare in clinical practice. However, we emphasize that steroid psychosis could be an initial presentation in patients with Cushing syndrome, and clinicians should be aware of possible mental disturbance as a clinical manifestation in patients with Cushing syndrome, as well as taking into account the results of general physical examinations.
Disclosure
None of the authors have any potential conflicts of interest associated with this report.
References
- 1. Kamp K, Alwani RA, Korpershoek E, Franssen GJH, de Herder WW, Feelders RA. Prevalence and clinical features of the ectopic ACTH syndrome in patients with gastroenteropancreatic and thoracic neuroendocrine tumors. Eur J Endocrinol 2016; 174: 271–80. [DOI] [PubMed] [Google Scholar]
- 2. Maragliano R, Vanoli A, Albarello L et al. ACTH‐secreting pancreatic neoplasms associated with Cushing syndrome: Clinicopathologic study of 11 cases and review of the literature. Am J Surg Pathol 2015; 39: 374–82. [DOI] [PubMed] [Google Scholar]
- 3. Davi' MV, Cosaro E, Piacentini S et al. Prognostic factors in ectopic Cushing's syndrome due to neuroendocrine tumors: A multicenter study. Eur J Endocrinol 2017; 176: 451–9. [DOI] [PubMed] [Google Scholar]
- 4. Ilias I, Torpy DJ, Pacak K, Mullen N, Wesley RA, Nieman LK. Cushing's syndrome due to ectopic corticotropin secretion: Twenty years' experience at the National Institutes of Health. J Clin Endocrinol Metab 2005; 90: 4955–62. [DOI] [PubMed] [Google Scholar]
- 5. Tang A, O'Sullivan AJ, Diamond T, Gerard A, Campbell P. Psychiatric symptoms as a clinical presentation of Cushing's syndrome. Ann Gen Psychiatry 2013; 12: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ruffini E, Oliaro A, Novero D, Campisi P, Filosso PL. Neuroendocrine tumors of the thymus. Thorac Surg Clin 2013; 21: 13–23. [DOI] [PubMed] [Google Scholar]
- 7. Chaer R, Massad MG, Evans A, Snow NJ, Geha AS. Primary neuroendocrine tumors of the thymus. Ann Thorac Surg 2002; 74: 1733–40. [DOI] [PubMed] [Google Scholar]
- 8. Neary NM, Lopez‐Chavez A, Abel BS et al. Neuroendocrine ACTH‐producing tumor of the thymus‐experience with 12 patients over 25 years. J Clin Endocrinol Metab 2012; 97: 2223–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wick MR, Scott RE, Li CY, Carney JA. Carcinoid tumor of the thymus. A clinicopathologic report of seven cases with a review of the literature. Mayo Clin Proc 1980; 55: 246–54. [PubMed] [Google Scholar]
- 10. Moran CA, Suster S. Neuroendocrine carcinomas (cartinoid timor) of the thymus. A clinicopathologic analysis of 80 cases. Am J Clin Pathol 2000; 14: 100–10. [DOI] [PubMed] [Google Scholar]
- 11. de Perrot M, Spiliopoulos A, Fischer S, Totsch M, Keshavjee S. Neuroendocrine carcinoma (carcinoid) of the thymus associated with Cushing's syndrome. Ann Thorac Surg 2002; 73: 675–81. [DOI] [PubMed] [Google Scholar]
- 12. Shrager JB, Wright CD, Wain JC, Torchiana DF, Grillo HC, Mathisen DJ. Bronchopulmonary carcinoid tumors associated with Cushing's syndrome: a more aggressive variant of typical carcinoid. J Thorac Cardiovasc Surg 1997; 114: 367–75. [DOI] [PubMed] [Google Scholar]
- 13. Bilgin YM, van der Wiel HE, Fischer HR, De Herder WW. Treatment of severe psychosis due to ectopic Cushing's syndrome. J Endocrinol Invest 2007; 30: 776–9. [DOI] [PubMed] [Google Scholar]
- 14. Baba M, Ray D. Severe psychosis due to Cushing's syndrome in a patient with a carcinoid tumour in the lung: a case report and review of the current management. World J Surg Oncol 2015; 13: 165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jibran D, Faizan M, Naveed A et al. A case of madness resulting in a fortunate outcome; case report of a psychotic break as a result of cortisol secreting thymic neuroendocrine thymic tumor. J Community Hosp Intern Med Perspect 2018; 8: 38–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sato H, Kajiya H, Kanai G et al. Atypical thymic carcinoid associated with Cushing's syndrome. Tokai J Exp Clin Med 2010; 35: 78–84. [PubMed] [Google Scholar]
- 17. Saito T, Kimoto M, Nakai S e a. Ectopic ACTH syndrome associated with large cell neuroendocrine carcinoma of the thymus. Intern Med 2011; 50: 1471–5. [DOI] [PubMed] [Google Scholar]
- 18. Somasundaram NP, Garusinghe C, Berney D, Grossman AB. A thymic carcinoid tumour causing Zollinger‐Ellison and Cushing's syndromes due to ectopic ACTH and gastrin secretion. Hormones (Athens) 2013; 12: 305–8. [DOI] [PubMed] [Google Scholar]
- 19. Barbieri JS, Seshasai R, Shemesh A, Sedrak M, Hoffman B, Alley EW. Thymic neuroendocrine tumor presenting with the ectopic ACTH syndrome. J Thorac Oncol 2013; 8: e57–8. [DOI] [PubMed] [Google Scholar]
- 20. Sekiguchi Y, Miyamoto Y, Kasahara I et al. Ectopic ACTH syndrome caused by desmopressin‐responsive thymic neuroendocrine tumor. Endocr J 2015; 62: 441–7. [DOI] [PubMed] [Google Scholar]
- 21. Chen YY, Li SQ, Liu HS et al. Ectopic adrenocorticotropic hormone syndrome caused by neuroendocrine tumors of the thymus: 30‐year experience with 16 patients at a single institute in the People's Republic of China. Onco Targets Ther 2016; 9: 2193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Oda N, Miyahara N, Tabata M et al. Pneumocystis pneumonia concomitant with ectopic ACTH syndrome caused by a large cell neuroendocrine carcinoma of the thymus. Intern Med 2017; 56: 551–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fujiwara W, Haruki T, Kidokoro Y et al. Cushing's syndrome caused by ACTH‐producing thymic typical carcinoid with local invasion and regional lymph node metastasis: A case report. Surg Case Rep 2018; 4: 5555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Szczepanek‐Parulska E, Cyranska‐Chyrek E, Nowaczyk M et al. Diagnostic difficulties in a young women with symptoms of Cushing syndrome. Endocr Pract 2018; 24: 766. [DOI] [PubMed] [Google Scholar]
- 25. Fazio N, Granberg D, Grossman A et al. Everolimus plus octreotide long‐acting repeatable in patients with advanced lung neuroendocrine tumors: Analysis of the phase 3, randomized, placebo‐controlled RADIANT‐2 study. Chest 2013; 143: 955–62. [DOI] [PubMed] [Google Scholar]


