Abstract
The objective of the study was the realistic evaluation of the prevalence of eating disorders (ED) among Polish men who sought treatment through the National Health Fund (NFZ) in the years 2010–2017. According to ICD-10, four types of ED were analyzed: anorexia nervosa—AN (F50.0), atypical anorexia nervosa (F50.1), bulimia nervosa—BN (F50.2), and atypical bulimia nervosa (F50.3).
The NFZ database was used. The ED groups were defined according to ICD-10 codes. Demographic data were collected from the web page of Statistics Poland (GUS). The annual prevalence of EDs was estimated, and the age groups were categorized into nine groups. For the incidence of EDs in male patients in the years 2010–2017, relative risk (RR) with 95% confidence interval (95% CI) was calculated.
The frequency trend of AN in males remains relatively stable. AN occurred mainly in young men (between 11 and 30 years). It was noted that AN affected approximately 100 men in each year of observation, while atypical anorexia nervosa affected about 40 men. In 2017, the RR for EDs in young males was 0.041 (95% CI [0.033, 0.051]). Bulimia was relatively rare (about 35 males each year).
The incidence of EDs in males is a relatively constant phenomenon. The real number of male patients with EDs may be higher. The current conceptualizations of ED pathology should be modified and better adapted to men. Clinical guidelines for specialists working with males with EDs should be developed.
Keywords: Anorexia, bulimia, eating disorders, observational studies
Publications on eating disorders (ED) in males are still scarce (Limbers, Cohen, & Gray, 2018). There are substantially more publications on the prevalence of EDs in females, especially young women (below 35 years; Mangweth-Matzek & Hoek, 2017). Publications about EDs in females of middle and older age are also limited (Conceição, Gomes, Vaz, Pinto-Bastos, & Machado, 2017; Lapid et al., 2010). Few studies concentrate on the prevalence of EDs in males (Mangweth-Matzek & Hoek, 2017), which are largely under-represented in the ED peer-reviewed literature and, hence, marginalized. Steps to rectify this are especially important in light of findings from epidemiological studies, suggesting that clinicians will be increasingly likely to treat males with EDs in their practices. It has been, thus, proposed that changes to current conceptualizations of ED pathology that accommodate male ED presentations better are needed (Murray et al., 2017).
Raevuori, Keski-Rahkonen, and Hoek (2014) reported lifetime prevalence rates of anorexia nervosa (AN) = 0.2%–0.3% and of bulimia nervosa (BN) = 0.1%–0.5% in young males, and that the core symptoms for males do not differ from those for females. There are far more publications analyzing the prevalence of EDs in young males than in mature males. The Lipson and Sonneville (2017) study of 9,713 participants showed that about 5.5% of young males (adolescents and young adults from 12 colleges and universities) manifested elevated ED risk in the United States. It needs to be remembered, however, that the study used the Eating Disorder Examination Questionnaire (EDE-Q) to evaluate ED outcomes. The conditions for the EDE-Q were created through a small sample of in-patient males with EDs. Based on the size of the sample and subsample of male patients with EDs, the tool’s sensitivity can be tentative at best (Jennings & Phillips, 2017). In Canadian studies, it has been demonstrated that about 1.1% of adolescent males exhibited a sub-threshold ED, which was associated with significant impairments in psychosocial functioning (Flament et al., 2015). Similar results were obtained in a Dutch sample of young adult males (Smink, van Hoeken, Oldehinkel, & Hoek, 2014). The prevalence of DSM-5 EDs was 1.2% in community samples of adolescent males in Australia (Allen, Byrne, Oddy, & Crosby, 2013). The main limitation of the studies, however, was the inclusion of only a defined age group of males, namely adolescents and young adults. Reas and Stedal (2015) reported lifetime prevalence rates based on supplemental data from the US National Comorbidity survey as 0.0% for AN, and 1.3% for BN in 45–59-year-old males. For males aged 60 years and above, these were less than 1% in all three diagnostic groups (0.3% and 0.3%, respectively). The 12-month prevalence rate for EDs in midlife for older males was estimated between 0.2% and 1.6%. Mangweth-Matzek and Hoek (2017) stress that, so far, no community studies have been reported on middle-aged and older males using two-stage methodological approaches including ICD or DSM criteria.
Another important limitation of the research on the prevalence of EDs in males is the vague set of criteria for ED symptoms. For example, in some studies, the evaluation of prevalence of EDs in males was based on questionnaires. Mangweth-Matzek, Kummer, and Pope (2016) analyzed the prevalence of EDs among men aged 40–75 years in Austria using an anonymous questionnaire on ED symptoms (based on either BMI <18.5, binge eating only, binge eating and purging, or purging only), the EDE-Q, body image, and exercise activity including exercise addiction. In other studies, DSM-5 criteria were used. For example, in studies with a sample of older veterans (N = 642 males, N = 55 females, aged on average 62.99, SD ± 12.03), it was demonstrated that 0.1% of male veterans displayed AN and 2.8% BN (Mitchell & Wolf, 2016). Body image disturbance was already identified as one of the central components in various diagnostic criteria, such as those of the DSM-5 or ICD-10. Many men who reported low body image satisfaction undertook radical attempts to modify their weight (Kostecka, Kordyńska, Murawiec, & Kucharska, 2019). The pursuit of a perfect body image is typical for women and men with EDs. Differences relate to the definition of the ideal body and can be attributed to gender roles and norms (Montgomery Sklar, 2017). For women, this ideal relates to slenderness, and for men to musculature. For this reason, it is difficult to find a single criterion.
Taking into account the lack of observational studies evaluating the prevalence of EDs, mainly AN and BN, in males of various age groups, in-house studies were undertaken. In the absence of relevant research, the objective of the article was the realistic evaluation of the prevalence of EDs among Polish men who sought treatment through the National Health Fund (NFZ) in the years 2010–2017. Particular attention was paid to the prevalence of four types of EDs: AN (F50.0), atypical anorexia nervosa (F50.1), BN (F50.2), and atypical bulimia nervosa (F50.3) in males in various age groups.
Methods
Subjects
Criteria for patient inclusion in the study involved the following: (a) eating disorders (F50) diagnosed by a psychiatrist according to ICD-10 (World Health Organization, 2004), (b) patients could belong to any age group, (c) they must have received state medical care in the years 2010–2017, (d) patients given a diagnostic code (ICD-10; World Health Organization, 2004) of EDs (F50) (World Health Organization, 2004) more than once in a given year from January 2010 to December 2017 were included. All patients had made at least one visit to outpatient or inpatient care where they were diagnosed with EDs. Of the entire database of patients with EDs, only those fulfilling the abovementioned criteria were included.
Source of Database
The National Health Information database maintained by the Polish NFZ was used. Retrospective data from January 2010 to December 2017 were collected for patients with EDs. NFZ collects medical data from state and private medical centers that have signed a contract with NFZ under which medical services are financed from public funds. Collecting medical data by the NFZ is regulated by the Regulation of the Minister of Health of June 20th, 2008 (last amendment of July 1st, 2017). In this regard, the database of medical services run by NFZ registers all patients who benefit from medical services financed from public funds (Regulation of the Minister of Health of 20 June 2008 on the scope of necessary information collected by public benefit providers, the detailed manner of registering this information and its transfer to entities authorized to finance health benefits under public funding).
The NFZ database includes specific information on demographic characteristics (gender and age) and consultation statements and diagnoses by the ICD-10 (World Health Organization, 2004). These data are widely accepted to be representative of the entire Polish population, a fact which increases their utility for nationwide population-based studies. Visit sampling and data collection were recorded on patient forms by hospital staff or by field representatives from the NFZ. Data collection methods do not indicate that data recording by hospital staff was done prospectively. Therefore, this study should be considered (conservatively) as a retrospective chart review. Data processing and coding were performed by NFZ. Due to the full anonymity of patients, access to more detailed data than gender and age was blocked.
Ethical Considerations
This study is a retrospective data analysis from the period 2010–2017, using data from a public database. For this reason, approval from an independent ethics committee (IEC) was not necessary. The authors sought advice from the Bioethics Committee of Medical University of Warsaw (MUW) to conduct the presented study. As the “commission does not issue opinions on survey, retrospective and other non-invasive scientific studies,” approval was not required. Data owners have given their permission to use their data.
Statistical Analysis
The demographic characteristics of the participants were analyzed through descriptive statistics. The annual prevalence of EDs was estimated for nine groups (above 10, 11–20, 21–30, 31–40, 41–50, 51–60, 61–70, 71–80, and ≥81). For the incidence of EDs in males with reference to all patients with EDs in the years 2010–2017, the relative risk (RR) with 95% confidence interval (95% CI) was calculated (Armitage, Berry, & Matthews, 2008).
Anorexia Nervosa (AN) in Male Patients in 2010–2017 in State Medical Care
What can be inferred from the presented data is that in all observation years, the group of young males with AN dominated. Males aged 11 to 30 years formed the largest group of males with AN recorded. After the age of 40, the number of males with diagnosed AN decreased significantly. Detailed data are presented in Table 1.
Table 1.
Number of Patients With Diagnosed AN or BN.
| Age group | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|
| AN (F50.0) | ||||||||
| Above 10 | 8 | 9 | 8 | 14 | 9 | 6 | 5 | 7 |
| 11–20 | 41 | 51 | 58 | 78 | 71 | 68 | 61 | 59 |
| 21–30 | 15 | 10 | 17 | 22 | 22 | 14 | 10 | 14 |
| 31–40 | 8 | 10 | 15 | 3 | 5 | 3 | 2 | 8 |
| 41–50 | 3 | 2 | 9 | 4 | 5 | 3 | 2 | 3 |
| 51–60 | 1 | 4 | 4 | 1 | 1 | 0 | 1 | 0 |
| 61–70 | 2 | 4 | 4 | 4 | 5 | 4 | 5 | 4 |
| 71–80 | 0 | 1 | 2 | 3 | 1 | 0 | 1 | 2 |
| >81 | 0 | 0 | 1 | 0 | 1 | 1 | 3 | 0 |
| Atypical anorexia nervosa (F50.1) | ||||||||
| Above 10 | 2 | 4 | 5 | 2 | 6 | 2 | 7 | 4 |
| 11–20 | 20 | 21 | 19 | 23 | 23 | 19 | 19 | 14 |
| 21–30 | 3 | 9 | 7 | 7 | 11 | 4 | 4 | 5 |
| 31–40 | 1 | 4 | 4 | 2 | 4 | 3 | 1 | 3 |
| 41–50 | 0 | 3 | 3 | 3 | 3 | 4 | 1 | 1 |
| 51–60 | 1 | 1 | 2 | 1 | 1 | 3 | 0 | 2 |
| 61–70 | 0 | 1 | 2 | 3 | 1 | 3 | 0 | 2 |
| 71–80 | 1 | 0 | 0 | 3 | 0 | 2 | 3 | 0 |
| >81 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 2 |
| BN (F50.2) | ||||||||
| Above 10 | 1 | 2 | 0 | 0 | 0 | 2 | 1 | 0 |
| 11–20 | 10 | 4 | 11 | 10 | 17 | 9 | 8 | 8 |
| 21–30 | 8 | 9 | 15 | 13 | 15 | 6 | 7 | 9 |
| 31–40 | 3 | 6 | 4 | 5 | 5 | 6 | 5 | 6 |
| 41–50 | 1 | 3 | 5 | 4 | 7 | 6 | 7 | 6 |
| 51–60 | 2 | 2 | 1 | 1 | 3 | 5 | 4 | 3 |
| 61–70 | 2 | 4 | 1 | 0 | 0 | 0 | 1 | 1 |
| 71–80 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| >81 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Atypical bulimia nervosa (F50.3) | ||||||||
| Above 10 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 |
| 11–20 | 4 | 3 | 3 | 1 | 4 | 6 | 2 | 1 |
| 21–30 | 3 | 1 | 7 | 7 | 4 | 2 | 2 | 2 |
| 31–40 | 0 | 4 | 0 | 0 | 0 | 3 | 0 | 5 |
| 41–50 | 0 | 0 | 1 | 2 | 2 | 3 | 4 | 7 |
| 51–60 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 2 |
| 61–70 | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 1 |
Atypical anorexia nervosa was most frequently diagnosed in males in the age range of 11–20 years. The discussed relationship was recorded in each year of observation. After the age of 20, the number of males with diagnosed anorexia nervosa decreased significantly. In the case of males over the age of 40, a significant number with atypical anorexia nervosa was recorded. Detailed data are presented in Table 1.
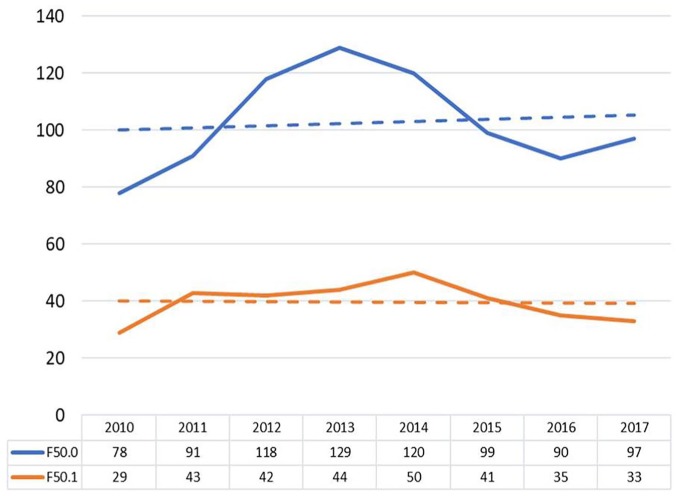
The trend of F50.0 and F50.1 diagnoses among men is presented in Figure 1.
Figure 1.
Coexistence trend of AN (F50.0) and atypical anorexia nervosa (F50.1) in males.
Bulimia Nervosa (BN) in Male Patients in 2010–2017 in State Medical Care
This 8-year observational study demonstrated that BN most often affected young males aged 11–30 years. A considerable decrease in the number of males with diagnosed BN was recorded after the fifth year of observation. It can be argued that in the last 3 years of observations, BN was diagnosed in males aged 11–60 years, which formed however single cases. Detailed data are presented in Table 1.
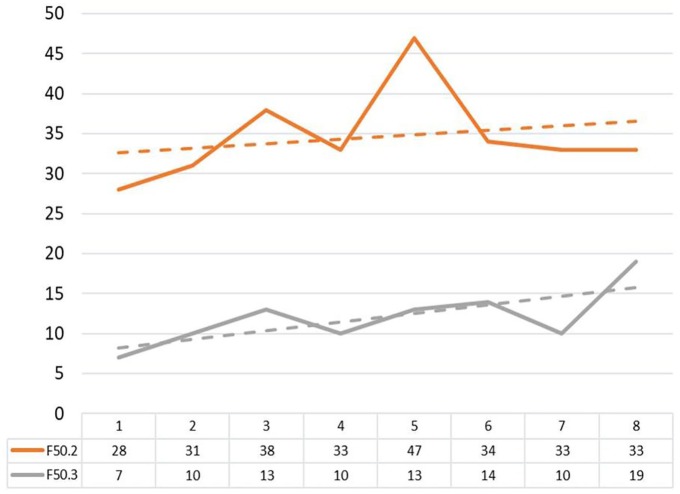
In the case of males aged 71 and above, no diagnosed cases of atypical bulimia nervosa were recorded in the years of observation. The study demonstrated that atypical bulimia nervosa was a relatively rare diagnosis among males in all age ranges. Detailed data are presented in Table 1. The trend of F50.2 and F50.3 diagnoses among men is presented in Figure 2.
Figure 2.
Coexistence trend of BN (F50.2) and atypical bulimia nervosa (F50.3) in males.
Relative Risk of EDs in Males
The calculated RR of incidence of EDs in males is around 95%–96% lower in comparison to females. EDs were analyzed together (AN and BN) when counting the RR. Detailed data of RR in particular years of observation are presented in Table 2.
Table 2.
Relative Risk (RR) of Eating Disorders in Males in Comparison to Females.
| RR | Year of observation | |||||||
|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
| 0.046 | 0.044 | 0.046 | 0.056 | 0.052 | 0.046 | 0.045 | 0.041 | |
| 95% CI | [0.097, 0.058] | [0035, 0.055] | [0.037, 0.057] | [0.046, 0.067] | [0.043, 0.063] | [0.037, 0.056] | [0.036, 0.055] | [0.033, 0.051] |
Discussion
The present study demonstrates a realistic prevalence of AN and BN among Polish men who sought treatment through the NFZ. The obtained results are, therefore, more reliable and accurate. Over these 8 years, it has been shown that the number of males with AN was relatively stable. It seems reasonable to examine the diagnostic criteria in AN in ICD-10 (World Health Organization, 2004). In the literature, the need to change current conceptualizations of ED pathology and adapt them better to males is stressed. This is connected to the fact that for many years AN has been treated as an illness exclusive to females. In this regard, relevant research pertaining to males constituted a gap in the literature (Murray et al., 2017). This lack of data had contributed to the creation of stigma for men, preventing many from seeking help. Moreover, it can be argued that men who do seek help are less likely to be diagnosed with AN. Ascribing AN predominantly to women may bias clinicians against an AN diagnosis for males (Kostecka et al., 2019).
Publications stress that AN may also occur in males, but not as often as in females. Some researchers indicate different strategies applied by young females and males in relation to their own body dissatisfaction. For example, in females, body dissatisfaction is usually associated with a desire to be thinner, but in groups of adolescent and young adult males, body dissatisfaction is related to being “bigger” and more muscular (Limbers et al., 2018; Tylka & Subich, 2002). This difference can be attributed to the relationship between feminine gender role stresses and ED symptomatology. Fear of being evaluated as unattractive correlated with dietary restraint. Moreover, the stress of conforming to feminine gender stereotypes is associated with a range of unhealthy body attitudes and behaviors (Montgomery Sklar, 2017). Males with AN, who are more concerned about thinness and not muscularity, are an exception (Field et al., 2014). Such a statement may be a generalization, as not every young male who is dissatisfied with their body shape takes actions aimed at becoming more muscular. Men with EDs who have normalized their weight may continue to overestimate their body-fat levels and experience distress with regard to their body image (Kostecka et al., 2019). Omission of this aspect in the ED concept may minimize the significance of the problem of anorexia nervosa among males, as well as raise a social barrier in seeking medical help. For example, a young male with AN who does not fit in the concept of “building body mass,” apart from experiencing multiple negative emotions, may also employ defense mechanisms, for example, deny his own illness, as it does not fit in with the current notion of EDs.
The literature points to the fact that EDs among men concern mainly the need for muscle expansion instead of body mass reduction and, by extent, AN (Field et al., 2014; Montgomery Sklar, 2017). Moreover, the field of men’s health has proven slow in exploring issues related to body weight and body image, at a time when these are rapidly becoming critical in society. This is challenged even further by the lack of academic research centers on men’s health by comparison to those dedicated to women’s health (Montgomery Sklar, 2017). Still, observations made in this study indicate a relatively stable trend of AN occurrence in males. From the presented data, it becomes clear that AN occurs far more often than atypical anorexia nervosa. AN (F50.0) affected on average 100 males in each year of observation, while atypical anorexia nervosa concerned around 40 males.
In all years of observation, the group of young males with typical anorexia nervosa was dominant. Both typical AN and atypical anorexia occurred mainly in young men. An important difference was the age range. Typical AN was recorded mainly in individuals aged 11–30 years, but atypical anorexia nervosa was most frequently diagnosed in the age range of 11–20 years. After the age of 40, the number of males with diagnosed AN decreased significantly, but there were still observed cases. For males over the age of 40, those with atypical anorexia nervosa were individual cases. The data obtained are in line with the literature reports. It is stressed that adolescence and young adulthood are peak periods for the development of EDs (Campbell & Peebles, 2014). In these periods, the greatest level of disappointment from the shape of one’s own body and utilization of unhealthy weight control behaviors are reported. For example, up to 30% of adolescent males in Australia and the United States report body dissatisfaction (McCabe, Ricciardelli, & Banfield, 2001).
The study demonstrated that BN occurs relatively rarely and is stable in males, especially young males aged 11 to 30. Atypical bulimia nervosa was relatively rarely diagnosed among males in all age groups. The data obtained are in line with the reports of other researchers, who stress that BN is known to be less common in adolescent males (Kinasz, Accurso, Kass, & Le Grange, 2016; Norris et al., 2012). It is stressed that males were more likely than females to be presented with a diagnosis other than AN or BN (Kinasz et al., 2016). Possibly, such a minute occurrence of BN in males is connected with gender differences in ED pathology (Montgomery Sklar, 2017). For example, adolescent and young adult males who exhibit bulimic symptoms are less likely to engage in dieting, laxative use, and self-induced vomiting than females (Limbers et al., 2018; Strother, Lemberg, Stanford, & Turberville, 2012). This may impinge on the frequency of diagnosing BN in males, which is connected with diagnostic criteria such as laxative use and self-induced vomiting. Compared to females, adolescent and young adult males are less likely to report eating in response to negative emotions, experiencing a sense of loss of control when binge eating, and restricting their food intake in response to body dissatisfaction (Limbers et al., 2018).
The present results suggest higher prevalence of AN than BN. It should be noted that other EDs were not analyzed in this study. According to the literature, AN and BN occur relatively rarely in men. Much more often, other forms of EDs are observed, such as obesity or males mainly concerned with muscle expansion instead of body mass reduction.
Low rates of AN and BN in men may seem to indicate a rare occurrence of this phenomenon. They can also show, however, that a problem can still occur in spite of gender roles and norms (Montgomery Sklar, 2017). This creates a stigma for men and may prevent many from seeking help (Kostecka et al., 2019). The present results also stress the need for looking for factors behind EDs, regardless of sex. Therefore, the problem of body image in men and its role in the etiology of EDs seems to be crucial. If the sex factor is not explored further, stigma for men will persist. Poor body image could be seen as a contemporary social and psychological barrier. It may be found more commonly among men who are socialized to be less emotive about their vulnerabilities. It may even prevent them from discussing any issues with their health-care providers (Montgomery Sklar, 2017). For this reason, studies on the dynamics of gender determinants of body weight and body image become focal in our understanding of the motives and resolve to manage one’s weight.
Strengths and Limitations
The study belongs to a minority of multi-year observational, and not longitudinal, studies. Longitudinal studies allow for the evaluation of the prevalence of a given phenomenon over a longer time period. This 8-year observational study allowed for a fair evaluation of the prevalence of the two most frequent EDs in males (AN and BN). It should be noted that the studies were conducted in the general population of patients benefiting from state medical care. The data are, therefore, representative of all patients in all medical centers that provide state subsidized treatments. This minimizes the risk of error during data collection in one medical center. Another strong point of the presented study is the diagnostic criteria of EDs. ICD-10 classification and psychiatric consultation were used in the study (World Health Organization, 2004) as the diagnostic criteria. Psychiatric consultation coupled with the use of ICD-10 classification (World Health Organization, 2004) increases the fairness of obtained data. It should be noted that few studies on the prevalence of EDs in males exist. The majority of these uses questionnaires or tools for the evaluation of the intensity of selected behaviors typical for the disorders. As a result, the findings are underestimated.
The present study is not devoid of limitations. Among the most important is concentrating only on the prevalence of EDs in patients who benefit from state medical care, to the exclusion of private medical care patients. The literature stresses that the majority of male patients with EDs are not aware of their illness and do not find their way to a psychiatrist. Compared to females, young adult males are less likely to seek treatment for EDs and do so later relative to the onset of their eating pathology (Limbers et al., 2018; Shingleton, Thompson-Brenner, Thompson, Pratt, & Franko, 2015). This is especially the case for young adult males from ethnic minority groups and lower socioeconomic backgrounds (Shingleton et al., 2015). Attempts have been made at explaining such a trend. It is, however, believed that adolescent and young adult males may not be as readily aware that their eating and weight control behaviors are pathological, due to a perception that EDs mostly affect females (Raisanen & Hunt, 2014). Another important limitation of the study is that it only considered patients who deliberately sought medical help, and were thus engaged in medical treatment. The number of patients who refuse to undergo medical treatment or are unaware of their illness remains unknown. The treatment of EDs in private centers is very expensive and many people cannot afford it. Therefore, private centers often sign a contract with the NFZ. Such subsidized private centers were included in this study. Overall, private medical care facilities for patients with EDs remain limited. Based on clinical observations, it appears that there are between 0 and 2 men in private centers for patients with EDs.
Conclusion
The occurrence of AN in males is a relatively frequent phenomenon. BN occurs in males far less often. The actual number of male patients with ED, however, may be higher. Reluctance to report the problem may stem from sex differences in ED pathology. In this regard, actions need to be taken in order to modify current conceptualizations of ED pathology and their better adaptation to males. Additionally, actions aiming at the development of therapeutic guidelines targeting males with ED would increase the effectiveness of therapy.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Mariusz Jaworski  https://orcid.org/0000-0002-5207-8323
https://orcid.org/0000-0002-5207-8323
References
- Allen K. L., Byrne S. M., Oddy W. H., Crosby R. D. (2013). DSM-IV-TR and DSM-5 eating disorders in adolescents: Prevalence, stability, and psychosocial correlates in a population-based sample of male and female adolescents. Journal of Abnormal Psychology, 122(3), 720–732. doi: 10.1037/a0034004 [DOI] [PubMed] [Google Scholar]
- Armitage P., Berry G., Matthews J. N. S. (2008). Statistical methods in medical research. New York: John Wiley & Sons, Inc. [Google Scholar]
- Campbell K., Peebles R. (2014). Eating disorders in children and adolescents: State of the art review. Pediatrics, 134(3), 582–592. doi: 10.1542/peds.2014-0194 [DOI] [PubMed] [Google Scholar]
- Conceição E. M., Gomes F. V. S., Vaz A. R., Pinto-Bastos A., Machado P. P. P. (2017). Prevalence of eating disorders and picking/nibbling in elderly women. International Journal of Eating Disorders, 50(7), 793–800. doi: 10.1002/eat.22700 [DOI] [PubMed] [Google Scholar]
- Field A. E., Sonneville K. R., Crosby R. D., Swanson S. A., Eddy K. T., Camargo C. A., , . . . Micali N. (2014). Prospective associations of concerns about physique and the development of obesity, binge drinking, and drug use among adolescent boys and young adult men. JAMA Pediatrics, 168(1), 34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flament M. F., Henderson K., Buchholz A., Obeid N., Nguyen H. N. T., Birmingham M., Goldfield G. (2015). Weight status and DSM-5 diagnoses of eating disorders in adolescents from the community. Journal of the American Academy of Child & Adolescent Psychiatry, 54(5), 403–413. doi: 10.1016/j.jaac.2015.01.020 [DOI] [PubMed] [Google Scholar]
- Jennings K. M., Phillips K. E. (2017). Eating Disorder Examination–Questionnaire (EDE–Q): Norms for a clinical sample of males. Archives of Psychiatric Nursing, 31(1), 73–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinasz K., Accurso E. C., Kass A. E., Le Grange D. (2016). Does sex matter in the clinical presentation of eating disorders in youth? Journal of Adolescent Health, 58(4), 410–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostecka B., Kordyńska K. K., Murawiec S., Kucharska K. (2019). Distorted body image in women and men suffering from Anorexia Nervosa – a literature review. Archives of Psychiatry and Psychotherapy, 1, 13–21. [Google Scholar]
- Lapid M. I., Prom M. C., Burton M. C., McAlpine D. E., Sutor B., Rummans T. A. (2010). Eating disorders in the elderly. International Psychogeriatrics, 22(4), 523–536. doi: 10.1017/S1041610210000104 [DOI] [PubMed] [Google Scholar]
- Limbers C. A., Cohen L. A., Gray B. A. (2018). Eating disorders in adolescent and young adult males: Prevalence, diagnosis, and treatment strategies. Adolescent Health, Medicine and Therapeutics, 9, 111–116. doi: 10.2147/AHMT.S147480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipson S. K., Sonneville K. R. (2017). Eating disorder symptoms among undergraduate and graduate students at 12 U.S. colleges and universities. Eating Behaviors, 24, 81–88. doi: 10.1016/j.eatbeh.2016.12.003 [DOI] [PubMed] [Google Scholar]
- Mangweth-Matzek B., Hoek H. W. (2017). Epidemiology and treatment of eating disorders in men and women of middle and older age. Current Opinion in Psychiatry, 30(6), 446–451. doi: 10.1097/YCO.0000000000000356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangweth-Matzek B., Kummer K. K., Pope H. G. (2016). Eating disorder symptoms in middle-aged and older men. The International Journal of Eating Disorders, 49(10), 953–957. doi: 10.1002/eat.22550 [DOI] [PubMed] [Google Scholar]
- McCabe M. P., Ricciardelli L. A., Banfield S. (2001). Body image, strategies to change muscles and weight, and puberty: Do they impact on positive and negative affect among adolescent boys and girls? Eating Behaviors, 2(2), 129–149. [DOI] [PubMed] [Google Scholar]
- Mitchell K. S., Wolf E. J. (2016). PTSD, food addiction, and disordered eating in a sample of primarily older veterans: The mediating role of emotion regulation. Psychiatry Research, 243, 23–29. doi: 10.1016/j.psychres.2016.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery Sklar E. (2017). Body image, weight, and self-concept in men. American Journal of Lifestyle Medicine, 11(3), 252–258. doi: 10.1177/1559827615594351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray S. B., Nagata J. M., Griffiths S., Calzo J. P., Brown T. A., Mitchison D., , . . . Mond J. M. (2017). The enigma of male eating disorders: A critical review and synthesis. Clinical Psychology Review, 57, 1–11. doi: 10.1016/j.cpr.2017.08.001 [DOI] [PubMed] [Google Scholar]
- Norris M. L., Apsimon M., Harrison M., Obeid N., Buchholz A., Henderson K. A., Spettigue W. (2012). An examination of medical and psychological morbidity in adolescent males with eating disorders. Journal of Eating Disorders, 20(5), 405–415. doi: 10.1080/10640266.2012.715520 [DOI] [PubMed] [Google Scholar]
- Raevuori A., Keski-Rahkonen A., Hoek H. W. (2014). A review of eating disorders in males. Current Opinion in Psychiatry, 27(6), 426–430. doi: 10.1097/YCO.0000000000000113 [DOI] [PubMed] [Google Scholar]
- Raisanen U., Hunt K. (2014). The role of gendered constructions of eating disorders in delayed help-seeking in men: A qualitative interview study. BMJ Open, 4(4), e004342. doi: 10.1136/bmjopen-2013-004342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reas D. L., Stedal K. (2015). Eating disorders in men aged midlife and beyond. Maturitas, 81(2), 248–255. doi: 10.1016/j.maturitas.2015.03.004 [DOI] [PubMed] [Google Scholar]
- Regulation of the Minister of Health of 20 June 2008 on the scope of necessary information collected by public benefit providers, the detailed manner of registering this information and its transfer to entities authorized to finance health benefits under public funding. Journal of Laws, 123, 6636–6695. Item 801. [Google Scholar]
- Shingleton R. M., Thompson-Brenner H., Thompson D. R., Pratt E. M., Franko D. L. (2015). Gender differences in clinical trials of binge eating disorder: An analysis of aggregated data. Journal of Consulting and Clinical Psychology, 83(2), 382–386. doi: 10.1037/a0038849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smink F. R., van Hoeken D., Oldehinkel A. J., Hoek H. W. (2014). Prevalence and severity of DSM-5 eating disorders in a community cohort of adolescents. The International Journal of Eating Disorders, 47(6), 610–619. doi: 10.1002/eat.22316 [DOI] [PubMed] [Google Scholar]
- Strother E., Lemberg R., Stanford S. C., Turberville D. (2012). Eating disorders in men: Underdiagnosed, undertreated, and misunderstood. Journal of Eating Disorders, 20(5), 346–355. doi: 10.1080/10640266.2012.715512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tylka T. L., Subich L. M. (2002). A preliminary investigation of the eating disorder continuum with men. Journal of Counseling Psychology, 49(2), 273–279. [Google Scholar]
- World Health Organization. (2004). International statistical classification of diseases and related health problems (Vol. 1). Geneva: World Health Organization. [Google Scholar]