Abstract
Introduction:
Hip fractures represent an important health-care dilemma, costing the US$ billions annually. Hip fractures can diminish quality of life and significantly increase morbidity and mortality if not properly treated. Recent research has brought forth new information regarding treatment as well as information on emerging complications seen within the fixation constructs themselves.
Significance:
Understanding the pathoanatomy of hip fractures and the biomechanics of surgical fixation constructs is critical for successful treatment. In this article, we review the relevant anatomy and classification of femoral neck and intertrochanteric fractures. Furthermore, the biomechanics of hip fracture fixation strategies as well as implant-related complications are addressed.
Results:
Even though laboratory testing demonstrated that intramedullary nails have greater biomechanical stability, the clinical results between fixation constructs have been similar when the chosen implant (ie, sliding hip screw vs cephalomedullary nail) has been correctly applied to the specific fracture pattern. Recently, data have shown that when using cephalomedullary nails, there is potential for increased failure with cutout when using the helical blade versus the lag screw, with majority being the atypical “medial cutout.”
Conclusion:
The goal of surgical treatment of hip fractures is surgical treatment that allows for early mobilization and weight bearing. A full understanding of the anatomy and fracture characteristics will allow the surgeon to correctly apply the right implant to allow for uneventful healing. Surgeons need to be aware, however, of complications that can arise when using specific implants. Further research is ongoing to further determine the treatments that will allow optimal cost-effective care for the geriatric patient with hip fracture.
Keywords: fragility fractures, hip fracture, geriatric trauma, hip fracture review, biomechanics
Epidemiology
Hip fractures are an important health-care concern in the elderly population. Currently, hip fractures affect 18% of women and 6% of men globally.1 Epidemiological studies have demonstrated that the incidence of hip fractures had increased from 1986 to 1995 but then steadily declined until 2012. The decline is likely related to improvements in the diagnosis and medical treatment of osteoporosis.2-4 From 2012 to 2015, the incidence of hip fractures reached a plateau, possibly related to the declining proportion of patients undergoing osteoporosis screening and medical treatment for osteoporosis.4 Moreover, as the life expectancy improves and the geriatric population continues to expand, the global number of hip fractures is estimated to increase from 1.26 million in 1990 to 4.5 million by 2050.1
It is also important to recognize that hip fractures confer significant societal and personal economic burden. Although hip fractures represent only 14% of all fragility fractures, these injuries represent a significant expense with an estimated cost up to US$15 billion annually.5 Treatment of hip fractures was also ranked 13th most expensive diagnoses by Medicare for 2011.6 Moreover, an economic analysis demonstrated that although a hip fracture was estimated to confer approximately US$10 000 for the initial hospitalization, the estimated 1-year health-care and social costs are approximately US$43 000 and is likely due to increasing need for additional care and supervision following surgical treatment.7 This is further supported by studies demonstrating that a proportion of patients with hip fractures may require long-term care facility placement with associated costs of US$19 000 to US$66 000.8,9 Thus, the management of hip fractures will remain a significant aspect of geriatric health care.
Anatomy
Knowledge of the musculoskeletal anatomy of the hip is critical to understanding how normal joint reactive forces across the hip influence fracture healing and underlines the importance of restoring normal anatomy.
Osteology and Muscular Attachments
The hip joint is a synovial joint that consists of the femoral head and neck. The femoral head is connected inferolaterally to the shaft via the femoral neck, which lies between the greater and lesser trochanter. The angle formed by the femoral neck and the medial aspect of the femoral shaft is approximately 127° with a range of 120° to 140°.10 Femoral version is formed by the angle of axis between the femoral neck and the transcondylar femoral axis. An important structure, known as the calcar femorale, is a dense cancellous strut that extends from the posterior aspects of the femoral neck to the posteromedial proximal femoral shaft.11 This structure plays a critical role in providing structural support and allowing stress distribution from the femoral head to the proximal femur.11 Thus, its presence or absence plays an important role in appropriate implant selection for hip fracture treatment.
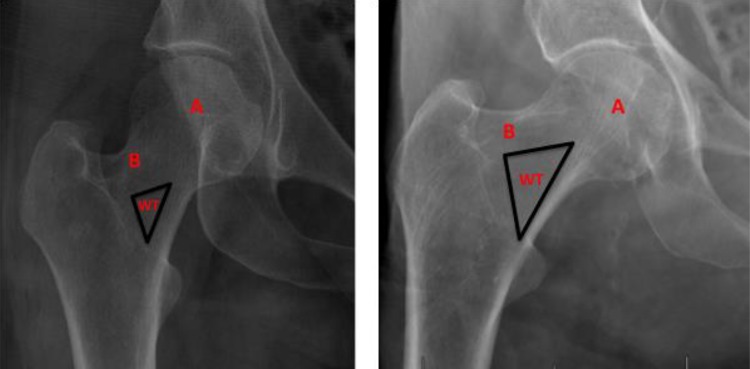
Within the femoral neck lies the compressive and tensile trabeculae, which form Ward triangle that is bound superiorly by tensile trabeculae and inferomedially by the compressive trabeculae and represents a region of low bone density (Figure 1).12 Recent studies have shown that the degeneration of trabeculae was closely related to the occurrence of femoral neck fractures, and enlargement of Ward triangle was related to occurrence of intertrochanteric fractures.13
Figure 1.
(Left) Right hip x-ray of a 30-year-old female. (Right) Right hip x-ray of a 98-year-old male. Note that the size of Ward triangle (WT) is significantly larger in the right image compared to the left image and that there is greater degeneration of principle compressive trabeculae (A) and principle tensile trabeculae (B) in the right image compared to the left image.
Knowledge of the muscular anatomy of the proximal femur is important to understand the deforming forces on fracture fragments and for surgical approaches. The gluteus minimus and medius insert onto the anterolateral and lateral aspects of the greater trochanter, respectively, and together serve as the main hip abductors.14 The iliopsoas tendon inserts onto the lesser trochanter and serves as the main hip flexor. The hip external rotators consist of the piriformis, superior and inferior gemellus, quadratus femoris, and obturator externus, which insert onto the medial aspect of the greater trochanter, except for the piriformis and obturator internus, which insert onto the superomedial aspects of the greater trochanter and the intertrochanteric crest, respectively.14
Vascular Anatomy
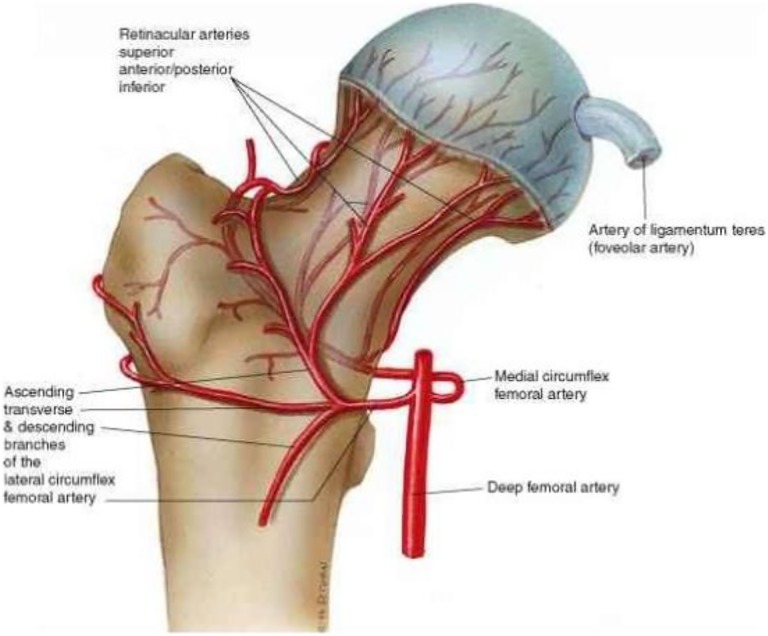
The vascular anatomy of the femoral head and neck is important for assessing the potential risk of avascular necrosis following proximal femur fractures (Figure 2). The main vascular supply to the femoral head and neck is the medial femoral circumflex and, more recently, highlighted the inferior gluteal artery.15,16 The medial femoral circumflex artery originates from the deep femoral artery and common femoral artery and courses between the piriformis and iliopsoas muscles.15 It then divides into the deep and descending branches.15 The deep branch courses toward the femoral head between the quadratus femoris and obturator externus and enters the posterior aspect of the hip capsule.15,16 Once intra-articular, the artery divides into the posterior superior nutrient arteries, which represent the most important blood supply to the femoral head and neck.15 More recent studies examining the inferior gluteal artery has shown that it provides significant blood supply to the femoral head, and in certain anatomic variants, this artery provides the dominant blood supply to the femoral head.15,17 The distal deep branch of the inferior gluteal artery anastomoses with the medial femoral circumflex artery prior to entering the posteroinferior hip capsule.15 Other vessels such as the lateral circumflex artery, superior gluteal artery, obturator artery, and acetabular branch of the obturator artery within the ligamentum teres provide minor contribution to the vascular supply of the femoral head.11
Figure 2.
Proximal femoral vascular anatomy. Main blood supply to the femoral head comes from the medial circumflex artery, which courses posterosuperiorly before penetrating the joint capsule into its terminal retinacular branches. Image reprinted with permission from ALPF Medical Research.
Neural Anatomy
A brief overview of the nervous anatomy that transverses the hip deserves mention. The obturator nerve and femoral nerve transverse along the anteromedial hip capsule. The superior gluteal nerve is adjacent to the posterior aspects of the hip capsule.11 The sciatic nerve courses inferior to the piriformis muscle and lies posterior to the external rotators of the hip.18 It is also important to recognize that there may be anatomic variations where the common fibular branch of the sciatic nerve may pierce the piriformis muscle or may pass over the piriformis.18 Another nerve that may be potentially injured during open approaches to the hip is the lateral femoral cutaneous nerve. This nerve exits approximately 2 cm medial from the anterior superior iliac spine and then divides into 2 branches that cross the anterior margin of the tensor fascia lata.11
Role of Osteoporosis and Aging in Geriatric Fractures
Aging is associated with changes in the femoral neck that increases fracture risk. The porosity of cortical bone also increases with age, with porosity increasing from 4% in young healthy patients to close to 50% in the elderly patients.19,20 In addition, microcracks gradually accumulate in cortical bone and increase significantly with advanced age.19,20 These microcracks generally accumulate more quickly in women compared to men.19,20 Moreover, nonenzymatically cross-linking of collage in bone can also adversely affect bone. These changes in the material properties of bone reduce the elasticity (material stiffness), strength (maximum stress in a load to failure test), and most importantly, the fracture toughness (energy required to fracture) of cortical bone, thereby increasing the risk of low-energy fractures.21-23 In addition, the cortex of the femoral neck expands with increasing age, with greater endosteal expansion compared to periosteal expansion resulting in thinning of cortical bone.24,25 Specifically, the superior aspect of the femoral neck undergoes more cortical thinning because it bears less load compared to the inferior regions of the femoral neck, and thus, it is at a higher risk of fracture.26
Classification of Hip Fractures
Hip fractures can be classified based on their relationship to the hip capsule. Therefore, fractures can be intracapsular, such as femoral neck fractures, or extracapsular, such as intertrochanteric and subtrochanteric fractures. This review focuses on femoral neck and intertrochanteric fracture patterns.
Intracapsular Hip Fractures
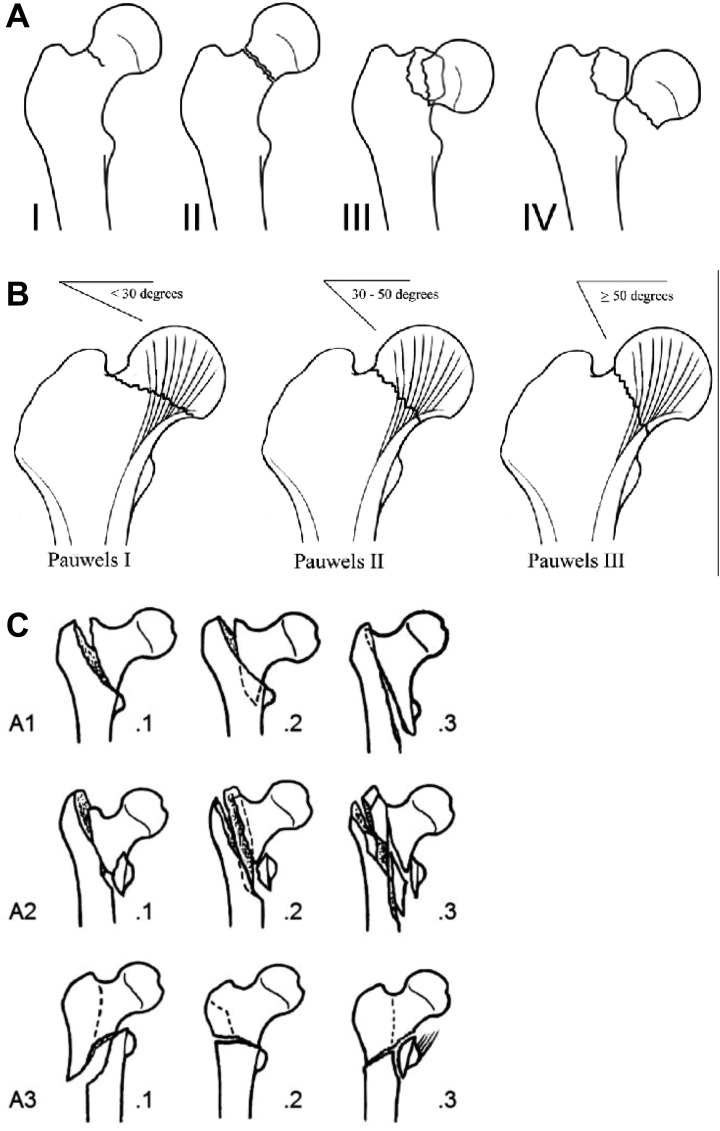
Femoral neck fractures can be described descriptively based the location of the fracture within the femoral neck or classified using the Garden, AO/OTA, or Pauwels classification (Figure 3). Thus, a femoral neck fracture located at the junction of the femoral head and neck is considered to be a subcapital fracture, while a transcervical fracture is located at the middle portion of the femoral neck. A basicervical fracture is located at the base of the femoral neck.
Figure 3.
Hip fracture classification according to Garden (A), Pawels (B), and AO/OTA (C). Figure A reprinted with permission from Hahn S, Young Han L, Seung Hyun L, et al. Easy way out-quick interpretation of musculoskeletal radiographs: the lower extremity. J Korean Soc Radiol. 2017;77(5):263-285. Figure B reprinted with permission from: Ye Y, Stahel P, Mauffrey C and Hak, D. Optimizing stability in femoral neck fractures. Orthopaedics. 2015;38:625-630. Figure C reprinted with permission from: orthopaedic trauma association classification, database and outcomes committee. Fracture and Dislocation Classification Compendium – 2007. J Orthop Trauma. 2007;10 suppl.
The Garden classification is the most widely used classification for elderly hip fractures and is based on the displacement of the fracture as assessed using an anteroposterior (AP) radiograph of the hip. The traditional Garden classification is divided into 4 types. Type 1 fractures are incomplete and valgus impacted, while type 2 fractures are complete.11 Type 3 fractures are partially displaced, and type 4 fractures are completely displaced.11 A modification of the Garden classification simply divides femoral neck fractures into nondisplaced or displaced. A study evaluating the Garden classification found that the κ coefficient (reliability) for the traditional classification was .31 (fair) while the modified system had a κ coefficient of .52 (moderate).27 In turn, the modified Garden classification system demonstrates greater interobserver reliability and is more widely utilized.27 More importantly, this classification system is useful for determining a surgical strategy as displaced fractures are generally treated with arthroplasty options.11
Although mainly used for high-energy femoral neck fractures in the physiologically young patient, the Pauwels classification deserves mention. This classification is based on the Pauwels angle, which is defined using the angle between a line through the fracture and a line that is tangential to the superior aspect of the femoral head.28 In this classification, type I fractures are less than 30°, type II fractures are between 30° and 50°, and type III fractures are greater than 50°.29 It was hypothesized that the Pauwels classification could predict risk of nonunion or loss of reduction as increasing fracture angle leads to increasing shear forces across the fracture site.28 Although there has been some debate regarding the predictive value of this classification scheme, a recent modification to the measurement of Pauwels angle may allow for more reliability.30 Specifically, the modified Pauwels angle is then defined as an angle between an imaginary line drawn perpendicular to the anatomic axis and a line through the fracture.30 A retrospective review demonstrated that a higher modified Pauwels angle was a risk factor associated with nonunion and avascular necrosis.30
The AO/OTA classification system is utilized to classify all fractures.22 Although this classification system is well accepted, it is solely used in research. The femoral neck fracture is 31-B. Further classification of femoral neck fracture includes 31-B1 indicating a fracture of junction between femoral neck and head with minimal displacement, 31-B2 denoting fractures of the middle region of the femoral neck, and 31-B3 representing fractures also at the junction of the femoral neck and head but with displacement.
Extracapsular Fractures
Intertrochanteric hip fractures are defined as fractures between the femoral neck and the lesser trochanter. The Evans classification of intertrochanteric fractures is based on the location and direction of the fracture as well as the stability. However, the most important classification system for an intertrochanteric fracture is whether the fracture pattern is stable or unstable as this affects implant choice. The determination of the stability of an intertrochanteric fracture is based on the integrity of the calcar femorale or the posteromedial cortex of the proximal femur. In addition, reverse obliquity fractures, which are angulated proximal medial to distal lateral, are also generally considered unstable as the femoral shaft has a tendency to medialize. Another fracture variant that is considered unstable is the transverse trochanteric or transtrochanteric fracture where the fracture exits the lateral cortex.
The AO/OTA classification of intertrochanteric fractures is designated as 31-A. It is further divided based on stability and fracture pattern. 31-A1 is a stable intertrochanteric fracture, and 31-A2 is an unstable intertrochanteric fracture, while 31-A3 is a reverse obliquity fracture or fractures that involve the lateral cortex. As with the AO/OTA classification for femoral neck fractures, this classification is reliable but is generally used for research purposes.
Treatment of Hip Fractures
The main goal of hip fracture treatment is early mobilization as it decreases the risk of postoperative complications and improves long-term mortality rate.31 In turn, surgical treatment is generally indicated unless the patient has significant comorbidities that present an unacceptable risk.
Surgical Treatment of Femoral Neck Fractures
The fixation strategy for femoral neck fractures is based on fracture displacement. In general, while displaced femoral neck fractures are usually treated with arthroplasty, fractures that are nondisplaced or minimally displaced (Garden type I or II fractures) can be managed with multiple cancellous lag screws or a sliding hip screw. Cancellous lag screw technique involves screw placement typically in an inverted triangle configuration with screws placed anterosuperiorly, posterosuperiorly, and along the inferior femoral neck. In order to maximize fracture stabilization, the cancellous screws should abut the cortical walls.32 Biomechanical studies suggest that the inverted triangle configuration with screws abutting the cortical surfaces confers the greatest mechanical stability compared to other screw fixation patterns.32,33 Biomechanical analysis also suggest that the use of washers should be considered especially in the setting of osteoporosis as it can distribute forces over the lateral cortex, thereby increasing insertional torque, improving fracture compression and fixation, and decreasing the risk of screw backout.34 The use of a fourth cancellous screw is controversial but can be considered in fracture patterns with significant posterior comminution.35
The sliding hip screw is an alternative fixation strategy for femoral neck fractures. This fixed angle device consists of placement of a lag screw parallel to the axis of the femoral neck, which is then inserted into a barrel that is attached to a lateral plate. This lag screw is allowed to slide within the barrel, thereby allowing for micromotion and compression across the fracture site. In order to minimize lag screw fixation failure, it is recommended that the screw tip to apex distance (measured as the sum of the distance from the tip of the lag screw to the femoral head on the AP and lateral views) should be equal or less than 25 mm.36 Furthermore, to maximize stability, the lag screw should be placed close to the calcar region (adjacent to the cortex) rather than the central region of the femoral neck.37 This is supported by a biomechanical study that demonstrated calcar cortical adjacent screw fixation demonstrated greater fracture stability and stiffness compared to centrally placed screw fixation.37
Several biomechanical studies have compared the use of cancellous screws versus the sliding hip screw. Another study evaluating basicervical femoral neck fractures using elderly cadaveric femurs found that cancellous screw fixation had a lower axial load to failure compared to sliding hip screw construct.38 Interesting, there was no significant differences in torsional stiffness between the two constructs.38 Another biomechanical analysis evaluating subcapital femoral neck fractures demonstrated that there were no significant differences between cancellous screw fixation and the sliding hip screw.39 In turn, from a biomechanical perspective, the sliding hip screw appears to provide superior fracture stabilization compared to cancellous screw fixation, especially in fracture patterns that are more prone to shear stress such as basicervical fractures.
A recent multicenter randomized controlled trial evaluated reoperation rates following the sliding hip screw fixation versus cancellous screw fixation for femoral neck fractures. The Fixation using Alternative Implants for Treatment of Hip fractures trial randomized 1108 patients (50 years or older) who sustained low-energy femoral neck fractures into sliding hip screw fixation versus cancellous screw fixation and evaluated the reoperations rate within 24 months after surgery. The study found similar rates of reoperations, treatment failures, and fracture healing between cancellous screws fixation and sliding hip screws. There were significantly higher rates of avascular necrosis and reoperation rates for avascular necrosis in patients who underwent the sliding hip screw fixation. Importantly, subgroup analysis found that in patients who were current smokers or had basicervical or displaced fracture patterns, the reoperation rates were significantly lower in patients who received the sliding hip screw fixation. In turn, an interpretation of these findings is that although these two surgical strategies provide similar outcomes, the biomechanical advantages of the sliding hip screw fixation translates into superior clinical outcomes in situations where there is poor bone quality due to smoking, fracture displacement, or fractures located near the intertrochanteric region. Moreover, the use of cancellous screw fixation may allow for preservation of the femoral head and neck blood supply. Overall, aside from special circumstances, the choice of surgical fixation is largely dependent on surgeon preference.40
Displaced femoral neck fractures are associated with a higher risk of avascular necrosis of the femoral head.41,42 Therefore, these fractures are generally treated with arthroplasty in the elderly patients.41,42 These options include total hip arthroplasty (THA) where both the femoral head and acetabulum are replaced or hemiarthroplasty (HA) where only the femoral head is replaced. Hemiarthroplasty is a technically easier procedure and is associated with lower costs, less operative time, less blood loss, and lower risk of dislocation compared to THA.41,43 However, THA is associated with better functional outcomes, especially in physiologically younger patients who are more active.43 In addition, HA may require conversion to a THA due to acetabular erosion, especially in active patients. A meta-analysis comparing HA versus THA found that THA was associated with significantly lower risk of reoperation, and better functional outcomes as determined by the Harris Hip Score and SF-36 Score (Physical Domain), while HA was associated with significantly lower dislocation risk.43 A subanalysis found that THA was associated with superior Harris Hip Score in studies where the mean patient age was less than 80 years, while studies with patients older than 80 years failed to detect any differences in functional outcome scores between HA and THA.43 A recent large retrospective study also found that HA was associated with greater risk of revision.44 Although THA is a more expensive procedure, at 1-year follow-up, the study found that THA was associated with lower overall costs compared to HA.44 It is possible that the improved functional outcomes and lower revision rate of THA may offset the initial costs of the procedure.44 Overall, the decision to choose THA versus HA should be based on patient factors, such as the presence of other comorbidities, the presence of arthritis, activity level prior to injury, and age.
Displaced femoral neck fracture can also be treated using cemented versus cementless HA. A possible risk associated with using a cemented stem is fat embolism, which can lead to cardiopulmonary complications.45 However, there is a higher risk of periprosthetic fracture in cementless stems.46,47 A randomized controlled study comparing the use of cemented HA versus cementless HA found that the use of cementless HA was associated with a significantly greater rate of intraoperative fracture and significantly inferior functional outcome scores at 1-year follow-up.46 A meta-analysis also found that cementless stems were associated with a significantly greater rate of overall complications as well as implant-related complications.47 Overall, the greater prevalence of periprosthetic fractures and inferior functional outcome scores for cementless HA support the use of cemented stems for displaced femoral neck fractures.
Surgical Treatment of Intertrochanteric Femur Fractures
Implant choice is largely based on the stability of the fracture pattern and the integrity of the lateral cortex. A stable intertrochanteric fracture has an intact or well-reduced posteromedial cortical calcar. This intact medial buttress allows the proximal femur to redistribute stress and resist medial compressive loads (Figure 4). In contrast, unstable intertrochanteric fracture patterns are unable to maintain appropriate reduction of the proximal femur when using extramedullary fixation options. These patterns often include fractures with a compromised medial calcar via comminution or a large posteromedial fragment, fractures that extend into the subtrochanteric region, reverse obliquity fractures, or transtrochanteric fractures that involve the lateral cortical wall (Figures 5 –8).48
Figure 4.

X-ray depicting stable intertrochanteric femur fracture (AO/OTA 31-A1). Notice the absence of comminution over the medial calcar.
Figure 5.

X-ray of left hip demonstrating unstable intertrochanteric fracture with separate posteromedial fragment (AO/OTA 31-A2).
Figure 6.

Reverse obliquity intertrochanteric fracture (AO/OTA 31-A3 fracture).
Figure 7.

Unstable intertrochanteric fracture with posteromedial fragment in addition to subtrochanteric extension (AO/OTA 31-A2 fracture).
Figure 8.

Unstable transtrochanteric fracture (AO/OTA 31-A3 fracture).
Compared to sliding hip screws, intramedullary devices offer greater biomechanical stabilization that is especially important in the setting of unstable intertrochanteric fractures.49 In these situations, the lack of contact between the posteromedial osseous fragments would result in transfer of greater medial compressive loads to the implant.50 The intramedullary device is closer to the force vector line of action through the center of the femoral head and has a shorter lever arm. Thus for the same force, the nail experiences less moment and can resist greater loads to failure (Figure 9).50 A biomechanical study found that use of the cephalomedullary device resulted significantly less fracture displacement and similar load to failure compared to sliding hip in the setting of stable and unstable intertrochanteric fracture models.49 Results from prospective randomized controlled trials also suggest that intramedullary fixation was associated with superior radiographic outcomes (limb shortening or femoral neck shortening) postoperatively and lower rates of incomplete union compared to sliding hip screw fixation in unstable intertrochanteric fractures.51,52
Figure 9.
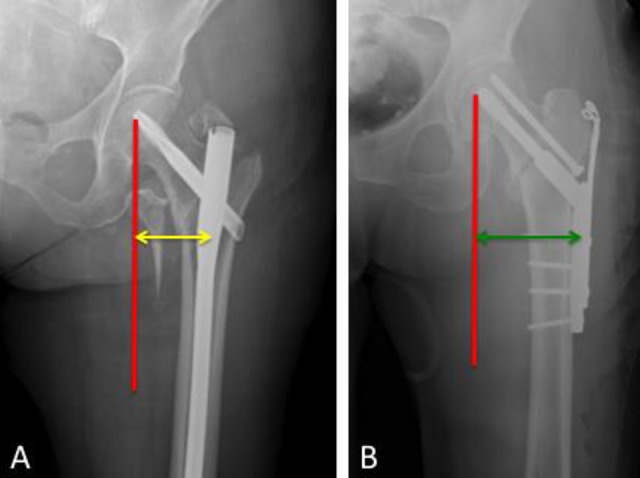
Representation showing that the intramedullary device (A) is closer to the force vector line of action through the center of the femoral head and has a shorter lever arm than the sliding hip screw (B). Thus, for the same force, the nail experiences less moment and can resist greater loads to failure.
The presence of lateral wall fracture in reverse obliquity and transtrochanteric patterns may also compromise the stability of an intertrochanteric fracture and thus may require intramedullary fixation.53 Studies evaluating sliding hip screws and intramedullary constructs found that the presence of lateral cortical wall fracture was a significant independent predictor of implant and treatment failure when using sliding hip screws.54,55 From a biomechanical perspective, the lateral cortical wall acts as a lateral buttress, and thus in the presence of lateral wall fracture, placement of a sliding hip screw can result in loss of reduction via medialization of the femoral shaft and lateralization of the proximal femoral component.53,56 Moreover, for reverse obliquity fractures, the fracture plane is nearly parallel to the direction of the sliding lag screw, and thus use of this implant will result in loss of reduction with significant collapse of the femoral neck.48,50,56 Retrospective studies demonstrated that in reverse obliquity or transtrochanteric fractures, sliding hip screws were associated with higher failure rates compared to the 95° blade plate. However, intramedullary fixation was associated with lower rate of failure rates compared to the 95° blade plate.56,57 In turn, intramedullary nails are superior to sliding hip screws for the treatment of reverse obliquity and transtrochanteric fracture or any intertrochanteric fracture with associated lateral wall fracture. This is because the intramedullary device acts as a substitute lateral wall that can prevent medialization of the femoral shaft and lateralization of the proximal femoral component.48,50,56
The most common mechanism of failure of the sliding hip screw fixation is varus collapse of the femoral neck, leading to lag screw cutout. In turn, the helical blade with the use of a side plate was introduced as an alternative design to reduce the risk of implant failure by increasing the anchorage into the osteoporotic femoral neck and head.58 A biomechanical study found that using a helical blade demonstrated significantly greater resistance to pullout and greater rotational stability compared to a standard lag screw.58 A clinical study comparing the sliding hip screw using a helical blade versus a lag screw in the setting of stable and unstable intertrochanteric fractures found that the helical blade was associated with significantly lower rate of fixation failure.59 Specifically, there were significantly lower rates of implant migration into the femoral head in the helical blade group.59 However, the reoperation rate and rate of cutout were similar between the 2 groups.59 In turn, the side plate with helical blade is an alternative surgical technique that has some biomechanical and clinical benefits over the standard lag screw technique.
More recent data on intramedullary fixation for intertrochanteric fractures have shown variability in the rates of cutout and failure using the helical blade versus the lag screw. A retrospective review looking at over 350 patients with peritrochanteric proximal femur fractures treated with a cephalomedullary nail demonstrated an almost 2-fold higher cutout rate using the helical blade than with the lag screw. Interestingly, the mode of failure of cutout was mainly medially through the head of the femur as the femoral head lateralized along the blade as opposed to superiorly, as has been published previously. In this study, there was no threshold value of tip-to-apex distance that increased the risk of cutout.60 In a more recent retrospective study, Chapman et al61 looked at the failure rate between the use of the helical blade and lag screw with only 1 type of cephalomedullary implant in 126 patients with low-energy hip fractures. The rate of cutout in this series was 5%, but more importantly, it was only found when the helical blade was used. The mode of cutout was predominantly medial and similar to the previous study, their finding was independent of tip-to-apex distance.61 Although earlier studies have suggested similar clinical results when using either the helical blade or the lag screw,62 more recent studies are showing perhaps a more clinical advantage of using the lag screw instead. Further research, with higher level studies, will need to be done to make a definitive recommendation.
Conclusions
Hip fractures represent a major global health-care problem that may become more prevalent as the elderly population increases. The goal of surgical treatment of hip fractures in the elderly patients is to allow for early mobilization and weight bearing. While displaced femoral neck fractures are usually treated with arthroplasty options, nondisplaced or minimally displaced fractures can be treated with cancellous screw fixation or a sliding hip screw with recent evidence favoring use of sliding hip screws for selected patients. The choice of a sliding hip screw or intramedullary nail fixation for intertrochanteric fractures depends on the overall fracture stability as well as involvement of the lateral cortical wall. Overall, further research is needed to further clarify and determine the treatment strategies that will allow optimal cost-effective care for the geriatric patient with hip fracture.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Publishing funding came from Unite Orthopaedics Foundation.
References
- 1. Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49(8):1458–1460. [DOI] [PubMed] [Google Scholar]
- 2. Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kannus P, Parkkari J, Sievanen H, Heinonen A, Vuori I, Jarvinen M. Epidemiology of hip fractures. Bone. 1996;18(1 suppl):57S–63S. [DOI] [PubMed] [Google Scholar]
- 4. Michael Lewiecki E, Wright NC, Curtis JR, et al. Hip fracture trends in the United States, 2002 to 2015. Osteoporos Int. 2018;29(3):717–722. [DOI] [PubMed] [Google Scholar]
- 5. Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–475. [DOI] [PubMed] [Google Scholar]
- 6. Roberts KC, Brox WT, Jevsevar DS, Sevarino K. Management of hip fractures in the elderly. J Am Acad Orthop Surg. 2015;23(2):131–137. [DOI] [PubMed] [Google Scholar]
- 7. Williamson S, Landeiro F, McConnell T, et al. Costs of fragility hip fractures globally: a systematic review and meta-regression analysis. Osteoporos Int. 2017;28(10):2791–2800. [DOI] [PubMed] [Google Scholar]
- 8. De Rui M, Veronese N, Manzato E, Sergi G. Role of comprehensive geriatric assessment in the management of osteoporotic hip fracture in the elderly: an overview. Disabil Rehabil. 2013;35(9):758–765. [DOI] [PubMed] [Google Scholar]
- 9. Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51(3):364–370. [DOI] [PubMed] [Google Scholar]
- 10. Gilligan I, Chandraphak S, Mahakkanukrauh P. Femoral neck-shaft angle in humans: variation relating to climate, clothing, lifestyle, sex, age and side. J Anat. 2013;223(2):133–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Collin PG, D’Antoni AV, Loukas M, Oskouian RJ, Tubbs RS. Hip fractures in the elderly: a clinical anatomy review. Clin Anat. 2017;30(1):89–97. [DOI] [PubMed] [Google Scholar]
- 12. Shivji FS, Green VL, Forward DP. Anatomy, classification and treatment of intracapsular hip fractures. Br J Hosp Med (Lond). 2015;76(5):290–295. [DOI] [PubMed] [Google Scholar]
- 13. Lu Y, Wang L, Hao Y, Wang Z, Wang M, Ge S. Analysis of trabecular distribution of the proximal femur in patients with fragility fractures. BMC Musculoskelet Disord. 2013;14:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Solomon LB, Lee YC, Callary SA, Beck M, Howie DW. Anatomy of piriformis, obturator internus and obturator externus: implications for the posterior surgical approach to the hip. J Bone Joint Surg Br. 2010;92(9):1317–1324. [DOI] [PubMed] [Google Scholar]
- 15. Kalhor M, Horowitz K, Gharehdaghi J, Beck M, Ganz R. Anatomic variations in femoral head circulation. Hip Int. 2012;22(3):307–312. [DOI] [PubMed] [Google Scholar]
- 16. Zlotorowicz M, Szczodry M, Czubak J, Ciszek B. Anatomy of the medial femoral circumflex artery with respect to the vascularity of the femoral head. J Bone Joint Surg Br. 2011;93(11):1471–1474. [DOI] [PubMed] [Google Scholar]
- 17. Kalhor M, Beck M, Huff TW, Ganz R. Capsular and pericapsular contributions to acetabular and femoral head perfusion. J Bone Joint Surg Am. 2009;91(2):409–418. [DOI] [PubMed] [Google Scholar]
- 18. Pokorny D, Jahoda D, Veigl D, Pinskerova V, Sosna A. Topographic variations of the relationship of the sciatic nerve and the piriformis muscle and its relevance to palsy after total hip arthroplasty. Surg Radiol Anat. 2006;28(1):88–91. [DOI] [PubMed] [Google Scholar]
- 19. Zebaze RM, Ghasem-Zadeh A, Bohte A, et al. Intracortical remodelling and porosity in the distal radius and post-mortem femurs of women: a cross-sectional study. Lancet. 2010;375(9727):1729–1736. [DOI] [PubMed] [Google Scholar]
- 20. Keaveny TM, Hayes WC. A 20-year perspective on the mechanical properties of trabecular bone. J Biomech Eng. 1993;115(4B):534–542. [DOI] [PubMed] [Google Scholar]
- 21. Silva MJ. Biomechanics of osteoporotic fractures. Injury. 2007;38(suppl 3):S69–S76. [DOI] [PubMed] [Google Scholar]
- 22. Burstein AH, Reilly DT, Martens M. Aging of bone tissue: mechanical properties. J Bone Joint Surg Am. 1976;58(1):82–86. [PubMed] [Google Scholar]
- 23. McCalden RW, McGeough JA, Barker MB, Court-Brown CM. Age-related changes in the tensile properties of cortical bone. the relative importance of changes in porosity, mineralization, and microstructure. J Bone Joint Surg Am. 1993;75(8):1193–1205. [DOI] [PubMed] [Google Scholar]
- 24. Duan Y, Beck TJ, Wang XF, Seeman E. Structural and biomechanical basis of sexual dimorphism in femoral neck fragility has its origins in growth and aging. J Bone Miner Res. 2003;18(10):1766–1774. [DOI] [PubMed] [Google Scholar]
- 25. Riggs BL, Melton Iii LJ, III, Robb RA, et al. Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J Bone Miner Res. 2004;19(12):1945–1954. [DOI] [PubMed] [Google Scholar]
- 26. Osterhoff G, Morgan EF, Shefelbine SJ, Karim L, McNamara LM, Augat P. Bone mechanical properties and changes with osteoporosis. Injury. 2016;47(suppl 2):S11–S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Van Embden D, Rhemrev SJ, Genelin F, Meylaerts SA, Roukema GR. The reliability of a simplified Garden classification for intracapsular hip fractures. Orthop Traumatol Surg Res. 2012;98(4):405–408. [DOI] [PubMed] [Google Scholar]
- 28. Parker MJ, Dynan Y. Is Pauwels classification still valid? Injury. 1998;29(7):521–523. [DOI] [PubMed] [Google Scholar]
- 29. Shen M, Wang C, Chen H, Rui YF, Zhao S. An update on the Pauwels classification. J Orthop Surg Res. 2016;11(1):161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wang SH, Yang JJ, Shen HC, Lin LC, Lee MS, Pan RY. Using a modified Pauwels method to predict the outcome of femoral neck fracture in relatively young patients. Injury. 2015;46(10):1969–1974. [DOI] [PubMed] [Google Scholar]
- 31. Maheshwari K, Planchard J, You J, et al. Early surgery confers 1-year mortality benefit in hip-fracture patients. J Orthop Trauma. 2018;32(3):105–110. [DOI] [PubMed] [Google Scholar]
- 32. Zdero R, Keast-Butler O, Schemitsch EH. A biomechanical comparison of two triple-screw methods for femoral neck fracture fixation in a synthetic bone model. J Trauma. 2010;69(6):1537–1544. [DOI] [PubMed] [Google Scholar]
- 33. Selvan VT, Oakley MJ, Rangan A, Al-Lami MK. Optimum configuration of cannulated hip screws for the fixation of intracapsular hip fractures: a biomechanical study. Injury. 2004;35(2):136–141. [DOI] [PubMed] [Google Scholar]
- 34. Zlowodzki MP, Wijdicks CA, Armitage BM, Cole PA. Value of washers in internal fixation of femoral neck fractures with cancellous screws: a biomechanical evaluation. J Orthop Trauma. 2015;29(2):e69–e72. [DOI] [PubMed] [Google Scholar]
- 35. Kauffman JI, Simon JA, Kummer FJ, Pearlman CJ, Zuckerman JD, Koval KJ. Internal fixation of femoral neck fractures with posterior comminution: a biomechanical study. J Orthop Trauma. 1999;13(3):155–159. [DOI] [PubMed] [Google Scholar]
- 36. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip–apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77(7):1058–1064. [DOI] [PubMed] [Google Scholar]
- 37. Booth KC, Donaldson TK, Dai QG. Femoral neck fracture fixation: a biomechanical study of two cannulated screw placement techniques. Orthopedics. 1998;21(11):1173–1176. [DOI] [PubMed] [Google Scholar]
- 38. Deneka DA, Simonian PT, Stankewich CJ, Eckert D, Chapman JR, Tencer AF. Biomechanical comparison of internal fixation techniques for the treatment of unstable basicervical femoral neck fractures. J Orthop Trauma. 1997;11(5):337–343. [DOI] [PubMed] [Google Scholar]
- 39. Clark DI, Crofts CE, Saleh M. Femoral neck fracture fixation. Comparison of a sliding screw with lag screws. J Bone Joint Surg Br. 1990;72(5):797–800. [DOI] [PubMed] [Google Scholar]
- 40. Fixation using alternative implants for the treatment of hip fractures I. Fracture Fixation in the Operative Management of Hip Fractures (FAITH): an international, multicentre, randomised controlled trial. Lancet. 2017;389(10078):1519–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Guyen O. Hemiarthroplasty or total hip arthroplasty in recent femoral neck fractures? Orthop Traumatol Surg Res. 2019;105(1 suppl):S95–S101. [DOI] [PubMed] [Google Scholar]
- 42. Parker MJ, Khan RJ, Crawford J, Pryor GA. Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures in the elderly. a randomised trial of 455 patients. J Bone Joint Surg Br. 2002;84(8):1150–1155. [DOI] [PubMed] [Google Scholar]
- 43. Lewis DP, Waever D, Thorninger R, Donnelly WJ. Hemiarthroplasty vs total hip arthroplasty for the management of displaced neck of femur fractures: a systematic review and meta-analysis. J Arthroplasty. 2019;pii: S0883-5403(19)30326-2. doi:10.1016/j.arth.2019.03.070. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 44. Ravi B, Pincus D, Khan H, Wasserstein D, Jenkinson R, Kreder HJ. Comparing complications and costs of total hip arthroplasty and hemiarthroplasty for femoral neck fractures: a propensity score-matched, population-based study. J Bone Joint Surg Am. 2019;101(7):572–579. [DOI] [PubMed] [Google Scholar]
- 45. Issack PS, Lauerman MH, Helfet DL, Sculco TP, Lane JM. Fat embolism and respiratory distress associated with cemented femoral arthroplasty. Am J Orthop (Belle Mead NJ). 2009;38(2):72–76. [PubMed] [Google Scholar]
- 46. Inngul C, Blomfeldt R, Ponzer S, Enocson A. Cemented versus uncemented arthroplasty in patients with a displaced fracture of the femoral neck: a randomised controlled trial. Bone Joint J. 2015;97-B(11):1475–1480. [DOI] [PubMed] [Google Scholar]
- 47. Veldman HD, Heyligers IC, Grimm B, Boymans TA. Cemented versus cementless hemiarthroplasty for a displaced fracture of the femoral neck: a systematic review and meta-analysis of current generation hip stems. Bone Joint J. 2017;99-B(4):421–431. [DOI] [PubMed] [Google Scholar]
- 48. Tawari AA, Kempegowda H, Suk M, Horwitz DS. What makes an intertrochanteric fracture unstable in 2015? Does the lateral wall play a role in the decision matrix? J Orthop Trauma. 2015;29(suppl 4):S4–S9. [DOI] [PubMed] [Google Scholar]
- 49. Curtis MJ, Jinnah RH, Wilson V, Cunningham BW. Proximal femoral fractures: a biomechanical study to compare intramedullary and extramedullary fixation. Injury. 1994;25(2):99–104. [DOI] [PubMed] [Google Scholar]
- 50. Haidukewych GJ. Intertrochanteric fractures: ten tips to improve results. J Bone Joint Surg Am. 2009;91(3):712–719. [PubMed] [Google Scholar]
- 51. Reindl R, Harvey EJ, Berry GK, Rahme E, Canadian orthopaedic trauma s. intramedullary versus extramedullary fixation for unstable intertrochanteric fractures: a prospective randomized controlled trial. J Bone Joint Surg Am. 2015;97(23):1905–1912. [DOI] [PubMed] [Google Scholar]
- 52. Sanders D, Bryant D, Tieszer C, et al. A multicenter randomized control trial comparing a novel intramedullary device (InterTAN) versus conventional treatment (Sliding Hip Screw) of geriatric hip fractures. J Orthop Trauma. 2017;31(1):1–8. [DOI] [PubMed] [Google Scholar]
- 53. Gupta RK, Sangwan K, Kamboj P, Punia SS, Walecha P. Unstable trochanteric fractures: the role of lateral wall reconstruction. Int Orthop. 2010;34(1):125–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Gao Z, Lv Y, Zhou F, et al. Risk factors for implant failure after fixation of proximal femoral fractures with fracture of the lateral femoral wall. Injury. 2018;49(2):315–322. [DOI] [PubMed] [Google Scholar]
- 55. Ciufo DJ, Zaruta DA, Lipof JS, Judd KT, Gorczyca JT, Ketz JP. Risk factors associated with cephalomedullary nail cutout in the treatment of trochanteric hip fractures. J Orthop Trauma. 2017;31(11):583–588. [DOI] [PubMed] [Google Scholar]
- 56. Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg Am. 2001;83-A(5):643–650. [DOI] [PubMed] [Google Scholar]
- 57. Sadowski C, Lubbeke A, Saudan M, Riand N, Stern R, Hoffmeyer P. Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degrees screw-plate: a prospective, randomized study. J Bone Joint Surg Am. 2002;84-A(3):372–381. [PubMed] [Google Scholar]
- 58. O’Neill F, Condon F, McGloughlin T, Lenehan B, Coffey JC, Walsh M. Dynamic hip screw versus DHS blade: a biomechanical comparison of the fixation achieved by each implant in bone. J Bone Joint Surg Br. 2011;93(5):616–621. [DOI] [PubMed] [Google Scholar]
- 59. Fang C, Lau TW, Wong TM, Lee HL, Leung F. Sliding hip screw versus sliding helical blade for intertrochanteric fractures: a propensity score-matched case–control study. Bone Joint J. 2015;97-B(3):398–404. [DOI] [PubMed] [Google Scholar]
- 60. Stern LC, Gorczyca JT, Kates S, et al. Radiographic review of helical blade versus lag screw fixation for cephomedullary nailing of low energy peritrochanteric femur fractures: There is a difference in cutout. J Orthop Trauma. 2017;31(6):305–310. [DOI] [PubMed] [Google Scholar]
- 61. Chapman T, Zmistowski B, Krieg J, et al. Helical blade versus screw fixation in the treatment of hip fractures with cephomedullary devices: incidence of failure and atypical “medical cutout”. J Orthop Trauma. 2018;32(8):397–402. [DOI] [PubMed] [Google Scholar]
- 62. Stern R, Lubbeke A, Suva D, et al. Prospecitve randomised study comparing screw verses helical blade in the treatment of low-energy trochanteric fractures. Int Orthop. 2011;35:1855–1861. [DOI] [PMC free article] [PubMed] [Google Scholar]