Abstract
Background:
The RxEACH randomized trial demonstrated that community pharmacist prescribing and care reduced the risk for cardiovascular (CV) events by 21% compared to usual care.
Objective:
To evaluate the economic impact of pharmacist prescribing and care for CV risk reduction in a Canadian setting.
Methods:
A Markov cost-effectiveness model was developed to extrapolate potential differences in long-term CV outcomes, using different risk assessment equations. The mean change in CV risk for the 2 groups of RxEACH was extrapolated over 30 years, with costs and health outcomes discounted at 1.5% per year. The model incorporated health outcomes, costs and quality of life to estimate overall cost-effectiveness. It was assumed that the intervention would be 50% effective after 10 years. Individual-level results were scaled up to population level based on published statistics (29.2% of Canadian adults are at high risk for CV events). Costs considered included direct medical costs as well as the costs associated with implementing the pharmacist intervention. Uncertainty was explored via probabilistic sensitivity analysis.
Results:
It is estimated that the Canadian health care system would save more than $4.4 billion over 30 years if the pharmacist intervention were delivered to 15% of the eligible population. Pharmacist care would be associated with a gain of 576,689 quality-adjusted life years and avoid more than 8.9 million CV events. The intervention is economically dominant (i.e., it is both more effective and reduces costs when compared to usual care).
Conclusion:
Across a range of 1-way and probabilistic sensitivity analyses of key parameters and assumptions, pharmacist prescribing and care are both more effective and cost-saving compared to usual care. Canadians need and deserve such care.
Knowledge Into Practice.
This is the first study to evaluate the cost-effectiveness of pharmacist case finding, prescribing and care in patients at high risk for cardiovascular disease in comparison to usual care in a community pharmacy setting.
The Canadian health care system could save more than $4.4 billion over 30 years if the pharmacist intervention were delivered to only 15% of the eligible population.
Pharmacist care would be associated with a gain of 576,689 quality-adjusted life years and avoid more than 8.9 million cardiovascular events.
Such benefits, combined with the high level of evidence supporting pharmacist-led interventions in chronic diseases and the support and satisfaction of patients with those interventions, present policy makers and pharmacy associations with an opportunity to add 42,500 helping hands in Canada to tackle the largest health care problem in the world.
Mise En Pratique Des Connaissances.
Il s’agit de la première étude évaluant le rapport évaluant coût-efficacité de la recherche de cas, de la prescription et de la prestation de soins par les pharmaciens, par rapport à la prestation des soins habituels, dans le milieu de la pharmacie communautaire, chez des patients présentant un risque élevé de maladie cardiovasculaire.
Le système de soins de santé canadien pourrait économiser plus de 4,4 milliards de dollars sur 30 ans si les pharmaciens intervenaient auprès de seulement 15 % de la population admissible.
Les soins prodigués par les pharmaciens seraient associés à un gain de 576 689 années de vie ajustées en fonction de la qualité et permettraient d’éviter plus de 8,9 millions d’événements cardiovasculaires.
Ces bienfaits, combinés aux données de grande qualité appuyant les interventions dirigées par les pharmaciens dans les cas de maladie chronique ainsi qu’au soutien et à la satisfaction des patients quant à ces interventions, permettent aux décideurs politiques et aux associations de pharmacies d’ajouter 42 500 ressources supplémentaires pour lutter contre le plus important trouble de santé au monde.
Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide, accounting for nearly one-third of the total deaths in 2016.1 The majority of CVD cases can be prevented by addressing modifiable risk factors, which include tobacco use, hypertension, hyperlipidemia, diabetes, physical inactivity, high-fat diet and obesity.1,2
The major CVD risk factors are still substantially prevalent and undertreated, despite the risk associated with them and the advent of new treatments.3-6 For example, Al Hamarneh3 and colleagues found that almost 50% of community-dwelling Canadians with type 2 diabetes were not at their A1C target. Leiter and colleagues4 reported that almost half of Canadians with type 2 diabetes did not achieve their A1C or cholesterol target, slightly more than one-third achieved their blood pressure targets and only 13% achieved the composite triple target. Such sobering facts combined with the societal and economic burden of CVD (yearly cost in Canada is around $21 billion divided between health care costs and loss of productivity)7 highlight the need for new avenues to tackle CVD and its risk factors.
Pharmacists are frontline primary health care providers who see patients with, or at risk for, chronic diseases frequently.8 As such, they are well positioned to systematically identify patients with or at risk for CVD and help manage their condition. The evidence for the efficacy of pharmacists’ intervention in CVD and its risk factors has been well demonstrated in the literature.9-13 The Alberta Vascular Risk Reduction Community Pharmacy Project (RxEACH) was a large randomized controlled trial designed to evaluate the impact of pharmacist case finding, prescribing and care on cardiovascular (CV) risk in patients at high risk for CV events.12 RxEACH included patients with diabetes, chronic kidney disease (CKD), established vascular disease or primary prevention (Framingham risk >20%) who had at least 1 uncontrolled risk factor (i.e., blood pressure, low-density lipoprotein cholesterol, tobacco use or A1C).12 The pharmacist intervention included patient assessment, laboratory assessment, individualized CV risk assessment and education about this risk, treatment recommendations, medication adaptation and prescribing, regular communication with the patient’s family physician and regular follow-up every month for 3 months.12 The study demonstrated a 21% reduction in risk for CV events compared to usual care.12
Despite the compelling evidence of the benefits of pharmacist management of CVD and its risk factors, there is scant evidence to support the economic value of providing such services as part of their routine care. As such, we conducted this analysis to evaluate the economic impact of pharmacist case finding, prescribing and care for CV risk reduction in a Canadian setting.
Methods
Model structure
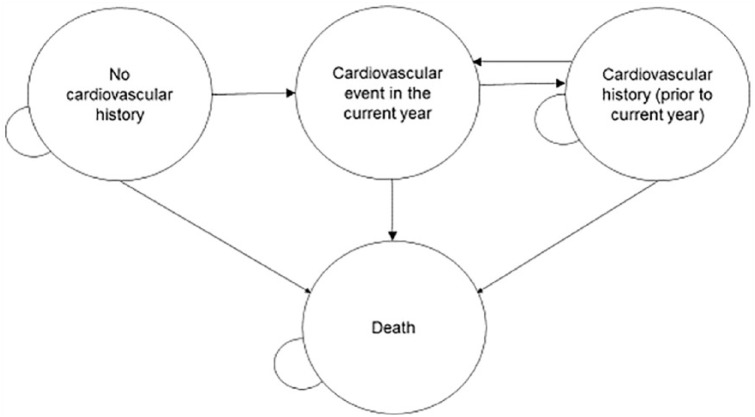
The standard approach for pharmacoeconomic modelling in the absence of particular characteristics that might make an alternative approach is a Markov cohort cost-effectiveness model. As such, we developed a model (Figure 1), with health state characterized by cardiovascular history (none, within the current year, prior to the current year) (Table 1), from a third-party public payer perspective to extrapolate the reduction in long-term CV outcomes, resulting from pharmacist case finding, prescribing and care,12 compared to a status quo scenario of usual care. The model was developed for a population with clinical characteristics as observed in the RxEACH study population (mean age: 61.8 years), and the study’s CV risk results were used to determine transitions between health states. The 10-year probabilities correspond to an annual transition probability for CV event of 3.1% for the usual-care group and 2.2% for the intervention group (that percentage will increase over time due to assumed waning of the intervention). The efficacy of the intervention assumed in the model was based on the 10-year CV risk scores calculated in the RxEACH study for both treatment arms.12 CV risk was calculated based on the patient’s comorbidities (i.e., diabetes, CKD, previous vascular disease or primary prevention). The UK Prospective Diabetes Study (UKPDS) risk assessment equation14 (see Appendix 1, available at www.cpjournal.ca, for risk factors included in the equation) was used to calculate CV risk in patients with diabetes. For primary prevention patients or those with CKD, CV risk was calculated using the Framingham risk assessment equation (Appendix 1).15 In patients with previous vascular disease, the CV risk was calculated using the International Model to Predict Recurrent Cardiovascular Disease risk assessment equation (Appendix 1).16 If the patient had more than 1 comorbidity, the risk was calculated using the relevant risk assessment equations, and the one estimating the highest risk was used. Risk over time was extrapolated from 10-year risk scores to a 30-year time horizon based on the assumption of exponential survival curves. Curves were calculated for both baseline and final risk scores for both treatment arms, and the difference in health and cost outcomes was compared across groups. For individuals who experienced a CV event, the distribution of specific event types (coronary heart disease, stroke, heart failure, myocardial infarction, angina) was based on Framingham calibration factors.15
Figure 1.
Markov model health states
Table 1.
Markov model parameters and stochastic distribution for probabilistic sensitivity analysis
| Parameter | Value | Probabilistic | Source |
|---|---|---|---|
| Base case | |||
| 10-year cardiovascular risk at baseline (pooled across treatment arms) | 26.2% | RxEACH study12 | |
| 10-year cardiovascular risk at 3 months | |||
| Usual care | 26.3% | Normal (26.3, 1.05) | |
| Pharmacist intervention | 20.2% | Normal (20.1, 0.86) | |
| Hazard ratio for mortality after cardiovascular disease | 1.7 | Lognormal (0.538, 0.075) | Pocock et al.19 |
| Cost of pharmacist intervention* | Assumption | ||
| Year 1 | $233.00 | ||
| Year 2 | $175.00 | ||
| Year 3+ | $175.00 | ||
| Cost of stroke† | Mittmann et al.,20 Sorensen et al.21 | ||
| Year 1 | $82,323 | Gamma (197.03, 417.83) | |
| Year 2+ | $12,490 | Gamma (25, 499.59) | |
| Cost per year of heart failure† | $13,637 | Gamma (25, 545.50) | Bentkover et al.22 |
| Cost per year of angina† | $3,877 | Gamma (39.74, 97.56) | McGillion et al.23 |
| Cost of myocardial infarction† | Coyle et al.24 | ||
| Year 1 | $11,857 | Gamma (26.53, 446.93) | |
| Year 2+ | $3468 | Gamma (2.27, 1528.00) | |
| Cost of background medical costs | $6105 | CIHI25 | |
| Utility | Sullivan et al.26 | ||
| General population | 0.867 | ||
| Post stroke | 0.694 | Beta (7090, 3126) | |
| Post heart failure | 0.636 | Beta (480, 275) | |
| Post angina | 0.709 | Beta (4843, 1988) | |
| Post myocardial infarction | 0.725 | Beta (61,446, 23,307) | |
| Disutility per year after age 70 | 0.00029 | ||
The cost of pharmacist intervention for year 1 is composed of $125 (cost of baseline visit) + [3*$25] (cost of 3 follow-up visits) + [$500/15] (cost of half-day training [$500] distributed amongst 15 patients per pharmacist). The cost of pharmacist intervention from year 2 onwards is composed of $125 (cost of baseline visit) + [2*$25] (cost of 2 follow-up visits).
Costs include all direct medical costs associated with the condition, including inpatient, outpatient, surgery and other procedures and medications.
A waning effect of treatment was incorporated, assuming that the intervention would be 50% effective after 10 years17 and 0% effective after 30 years, with sensitivity analysis conducted based on 0% effectiveness after 15 and 20 years. Costs and outcomes were discounted at 1.5% per year.18 Canadian life tables were used to calculate age- and sex-specific mortality over time. For individuals with a history of CVD, a hazard ratio of 1.71 was applied by multiplying with the relevant age- and sex-specific life table hazard (see Table 1).19
Individual-level results were scaled up to population level based on the assumption that 29.2% of Canadian adults27 (approximately 9,000,000 people) would be eligible to receive the intervention (i.e., are at high CV risk). Of the full eligible population, it was assumed that only a subset would actually access the intervention, and results were calculated based on potential uptake rates of 15% of the eligible population, with sensitivity analyses conducted based on 30% and 45% uptake rates. In addition to the prevalent population assumed to access the intervention initially, incident cases of high CV risk were also assumed to initiate the intervention each year. The same 15% uptake rate was assumed for incidence, and the incident rate was calculated based on the assumption that the ratio of incidence to prevalence would be the same for overall increased CV risk as has been reported for hypertension.28,29
Results were characterized by differences in costs, life years, quality-adjusted life years (QALYs) and incremental cost per QALY between treatment arms at both the individual and population levels. The distribution of results was characterized by a 5000-iteration probabilistic sensitivity analysis. Model parameters were consistent with a recent model developed to assess the impact of pharmacist intervention on hypertension.30
Health state utility values
It has been reported that utility values are similar among patients in Canada and the United States.31 As such, we used a published catalogue of EuroQol 5 dimension (EQ-5D) utility values to quantify health state utility values (HSUVs) for health states of interest. Resulting utilities were 0.725 (standard error [SE] 0.0015) for myocardial infarction (MI), 0.709 (SE 0.0055) for angina, 0.694 (SE 0.0046) for stroke and 0.636 (SE 0.0175) for heart failure. Resulting HSUVs were applied based on the occurrence of the first CV event; adjustments were not made for multiple events. A utility decrement of 0.00029 per year was applied to all years accrued older than age 70 years (e.g., for individuals surviving to age 75, a QALY decrement of 0.00029 × 5 = 0.00145).26
Costs
Costs included direct medical costs as well as the costs associated with implementing the pharmacist intervention. Investigators’ familiarity with implementing such programs in a clinical trial setting provided the assumptions to calculate the cost of the pharmacist intervention (a similar approach was implemented in a recent model developed to assess the impact of pharmacist intervention on hypertension).30 It was assumed that individuals would be seen 4 times in the first year and 3 times per year thereafter. The unit cost of the first consultation of each year is $125 CAD and $25 for subsequent consultations, reflecting the fee schedule in Alberta at the time the study was conducted.32 Conservatively, we also assumed that there would be no difference in other background medical costs, despite the fact that the intervention group would likely have physician visits offset by the additional pharmacist consultations. All aspects of the intervention program are within the current core competencies of pharmacists in Alberta, and any additional training would likely be covered by the pharmacy or done as part of usual continuing professional development by pharmacists. However, as a conservative assumption, it was assumed that a government payer would contribute funding for a half-day training per pharmacist to familiarize themselves with the intervention and required documentation. Assuming $1000 per training-day to be distributed among 15 patients per pharmacist, the resulting cost is an additional $33 per patient receiving the intervention.
CVD costs were based on a review of the Canadian studies published in peer-reviewed journals. To inflate values to 2017 $CAD values, we used the Canadian Health and Personal Care component of the Consumer Price Index.33
Based on Canadian Institutes for Health Information (CIHI) reports, $6105 per person per year was assumed to be the overall Canadian average background non-CV medical cost.34 When building the base case, we used the overall average rather than age-specific values to prevent double-counting of costs. Since age-specific values in older individuals are expected to comprise a substantial proportion of CV-related costs, these are being explicitly incorporated into the model.
Results
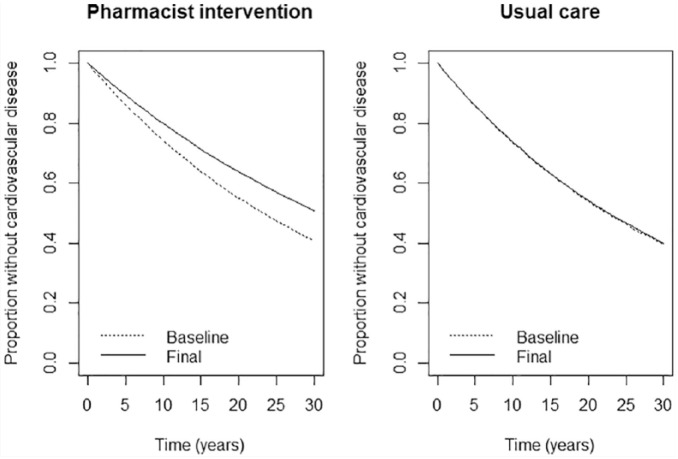
In the RxEACH study, the pooled baseline CV risk score for the entire study population was estimated to be 26.2%. At end of treatment, this risk score was reduced to 20.2% (SE 0.86%) in the intervention group and remained similar to baseline (26.3% [SE 1.05%]) in the usual-care group. Based on the assumption of an exponential function and extrapolating from 10-year risk scores, 30-year risk of CVD for both treatment arms is shown in Figure 2.
Figure 2.
Extrapolated risk of cardiovascular disease based on observed 10-year cardiovascular risk scores from RxEACH study
At the end of the 30-year time horizon, it is estimated that each individual accessing the pharmacist intervention would gain 0.11 life years and 0.19 QALYs, experience 0.10 fewer CV events, and accrue $2149 less in direct medical costs compared to an individual not receiving the intervention. For every 100 individuals accessing the intervention, it is estimated that the avoided CV events would include 3 cases of stroke, 5 MIs, 2 anginas and 1 heart failure. These differences result from reduced incidence of CV events predicted by the reduction in CV risk scores, leading to improved survival and lower medical costs. The intervention is therefore estimated to be economically dominant (i.e., more effective and less costly) relative to the usual care. The dominant result held in 100% of iterations of the probabilistic sensitivity analysis (5000 iterations) (Figure 3). (There is 100% probability of cost-effectiveness at all willingness-to-pay thresholds.) The overall dominant result remained when the maximum time at which the intervention waned to zero efficacy was reduced from the base case assumption of 30 years to 15 and 20 years.
Figure 3.
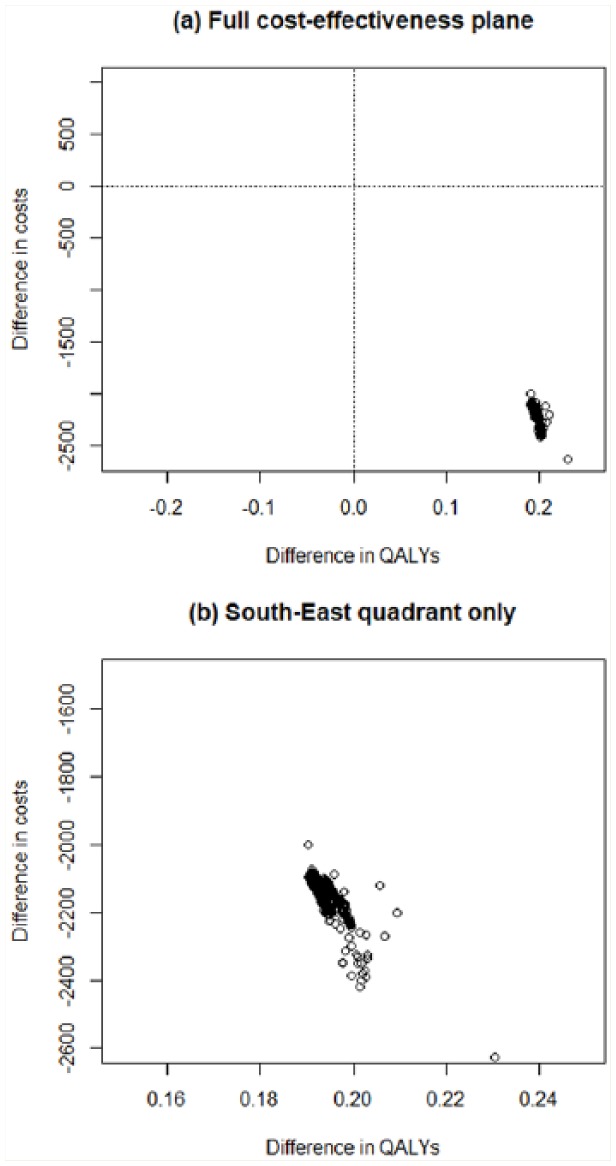
Cost-effectiveness plane across 5000-iteration probabilistic analysis
When the individual-level results are scaled up to the population level, the base case assumption of a 15% uptake rate resulted in an estimated 1.3 million prevalent individuals accessing the intervention in the first year. It was assumed that 100,000 incident individuals would enter the cohort each year. For this population size, across probabilistic sensitivity analysis interventions, the mean incremental cost (discounted 1.5%) associated with the intervention was a savings of more than $4.4 billion over 30 years. Corresponding mean differences in health outcomes were an additional 576,689 QALYs, 380,143 life years, and more than 8.9 million fewer CV events. When uptake rates were increased to 30% or 45% of the eligible population, relative to the base case assumption of 15%, cost savings and health outcomes improvements increased accordingly (Table 2).
Table 2.
Intervention impact on cost and outcomes over 30 years
| Proportion of eligible population
accessing the intervention |
|||
|---|---|---|---|
| 15% | 30% | 45% | |
| Incremental costs | –$4,403,946,776 | –$8,807,893,551 | –$13,211,840,327 |
| QALYs | 576,689 | 1,153,378 | 1,730,067 |
| Life years | 380,143 | 760,285 | 1,140,428 |
| CV events avoided | 8,915,842 | 17,831,684 | 26,747,527 |
CV, cardiovascular; QALY, quality-adjusted life year.
Discussion
To our knowledge, this is the first study to evaluate the cost-effectiveness of pharmacist case finding, prescribing and care in patients at high risk for CVD in comparison to usual care in a community pharmacy setting. Our results demonstrated that the pharmacist intervention was an economically dominant strategy compared to usual care, which means that the intervention both improves patient outcomes and saves the health care system money. Indeed, the dominant result held in 100% of 5000 iterations of the probabilistic sensitivity analysis. Pharmacist care would save more than $4.4 billion, add 576,689 QALYs and prevent more than 8.9 million CV events over 30 years compared to usual care if applied to only 15% of the eligible adults in Canada. Those savings can reach more than $13 billion if the intervention is applied to 45% of the eligible Canadians.
Our findings are consistent with the findings of Marra and colleagues,30 who evaluated the economic impact of a comprehensive community pharmacist intervention (including education and prescribing) in patients with uncontrolled hypertension. They reported that the intervention improved patient outcomes and was associated with cost savings compared to usual care. Similar cost reductions were found in our study.
Omboni and Caserini35 and Altowaijri and colleagues36 conducted systematic reviews to evaluate the clinical and economic effectiveness of pharmacist interventions in the management of CVD. They reported that such interventions (including medication management, patient education and direct measurement and management of CVD risk factors) were associated with reduced health care costs. This is consistent with our findings, in which each individual receiving the pharmacist intervention would accrue $2149 less in direct medical costs compared to an individual who is not.
Limitations
This study is not without limitations. The assumption required to extrapolate the observed data into long-term outcomes is an inherent limitation of any cost-effectiveness model. However, we conducted a series of extensive probabilistic and deterministic analyses as well as a series of threshold analyses to mitigate that limitation. The dominant result held in 100% of iterations of the probabilistic sensitivity analysis. For the base model, we have assumed that the intervention would be delivered to only 15% of the eligible population and used the Alberta fee schedule at the time of study conduct.37 Such assumptions indicate that our model is very conservative. The difference in pharmacy fee schedule in other jurisdictions may affect the generalizability of the findings. However, our conservative assumptions and findings strongly suggest that such intervention could still be effective and cost-saving in any jurisdiction regardless of the fee schedule. Our study used the efficacy data from 1 study.12 However, this study is the largest randomized controlled trial in a community pharmacy setting.12
The findings of this economic evaluation, the improved clinical outcomes in the RxEACH study,12 the high degree of support and appreciation for pharmacists’ full scope of practice38 and the fact that CVD is one of the leading causes of death in Canada7 indicate the need to implement such effective and less costly interventions on a wide scale as a public health service.
The clinical,12 qualitative38 and economic findings of the RxEACH study add to the body of evidence to support pharmacist-led interventions in chronic diseases. Pharmacists, pharmacy associations and payers should seize the opportunity and join the fight against the leading cause of death in the world.1
Conclusion
Across a range of 1-way and probabilistic sensitivity analyses of key parameters and assumptions, pharmacist case finding, prescribing and care are more effective and cost-saving compared to usual care. Such savings, combined with the high level of evidence supporting pharmacist-led interventions in chronic diseases9-13 and the support and satisfaction of patients with those interventions,38 present policy makers and pharmacy associations with an opportunity to add 42,500 helping hands39 in Canada to tackle the largest health care problem in the world.
Supplemental Material
Supplemental material, 851822_App1_online_supp for Pharmacist prescribing and care improves cardiovascular risk, but is it cost-effective? A cost-effectiveness analysis of the RxEACH study by Yazid N. Al Hamarneh, Karissa Johnston, Carlo A. Marra and Ross T. Tsuyuki in Canadian Pharmacists Journal / Revue des Pharmaciens du Canada
Acknowledgments
None of this could have taken place without the dedication and caring of the RxEACH investigators, listed in descending order of recruitment:
Jen Winter and Lonni Johnson (Winter’s Pharmacy, Drayton Valley); Tyler Watson and Andrew Fuller (Pharmacare Specialty Pharmacy, Edmonton); Janelle Fox (Pharmasave #325, Bonnyville); Rick Siemens (London Drugs #38, Lethbridge); Jasbir Bhui and Jasmine Basi (Medicine Shoppe #170, Edmonton); Murtaza Hassanali, Shamas Arshad and Manpreet Mann (Shoppers Drug Mart #371, Edmonton); Theresa Lawrence, Michelle Ewen and Maged Radwan (Rexall Pharmacy #7222 and #7266, Blairmore and Pincher Creek); Anita and Bob Brown (Shoppers Drug Mart #2401, Okotoks); Leanna St. Onge, Otti Gohrbandt and Chelsey Collinge (Co-op Pharmacy, Rocky Mountain House); Jelena Okuka and Michelle Teasdale (Co-op Pharmacy, Lloydminster); Hyder Mohammed (Shoppers Drug Mart #2318, Lethbridge); Gehan Rizkalla (Loblaws Pharmacy #4950, Leduc); Dixie Richardson (Safeway Pharmacy #848, Edmonton); Roberta Taylor (Roots & Berries Pharmacy, Maskwacis); Marnie Kachman and Kristy Russ (Medicine Shoppe #264, Leduc); Anita Wong (Rexall Pharmacy #9801, Edmonton); Sheilah Kostecki (Safeway Pharmacy #2730, Calgary); Terrilynn Eriksen and Sharon Beaudry (Costco Pharmacy #254, Grande Prairie); Nader Hammoud (Shoppers Drug Mart #2326, Calgary); Jim Kitagawa (Pharmasave #345, Brooks); Morenike Olaosebikan (Shoppers Drug Mart #381, Edmonton); Rosalia Yeun (Medicine Shoppe #328, Edmonton); Carlene Oleskyn and Jelena Okuka (Meridian Pharmacy, Stony Plain); Dactin and Monika Tran (Sandstone Sarcee, Calgary); Rita Lyster and Alex Lischuk (Ritas Apothecary, Barrhead); Barb Bryan and Arin Getz (Sobeys Pharmacy #1129, Calgary); Lyn Gilmore and Rick Krieser (Shoppers Drug Mart #2374, Edmonton); Nermen Kassam (Pharmacy Plus Ltd, Calgary); Azita Rezai (Shoppers Drug Mart #385, Calgary); Tony Nickonchuk and Stacy Billows (Walmart Pharmacy #1068, Peace River); Piere Danis, Brittany Dyjur and Meghan Gainer (Safeway Pharmacy #861, Edmonton); Paulise Ly (Walmart Pharmacy #1144, Calgary); Jody Keller and Wade Mannle (Pharmasave #378, Carstairs); Uzma Saeed (Walmart Pharmacy #1071, Vegreville); Rick Mah (Sobeys Pharmacy #1139, Calgary); Ken Pitcher (Save-On Foods Pharmacy #6642, Lethbridge); Mike, Pat and Vanda Kinshella (Value Drug Mart, Peace River); Nadine Abou-Khair and Aileen Coutts (Coop Pharmacy, Calgary); Duy Troung (Shoppers Drug Mart #2300, St. Albert); Janice Chua (Shoppers Drug Mart #324, Wetaskiwin); Brendan Ihijerika (Guardian Pharmacy, Mundare); Marlene Bykowski (Remedy Rx 222, St. Albert); Jaclyn Katelnikoff (Stafford Pharmacy, Lethbridge); Rashid Jomha (Sobeys Pharmacy #3132, Edmonton); Nick Leong (Shoppers Drug Mart #328, Edmonton); Peter Lok (Shoppers Drug Mart #357, Ponoka); Kim Lau (Remedy’s Rx #223, Calgary); Brittany Zelmer (Safeway Pharmacy #864, Edmonton); Anar Dato (Shoppers Drug Mart #2391, Calgary); Kelly Laforge (Shoppers Drug Mart #2448, Edmonton); Todd Pranchau (Shoppers Drug Mart #2450, Sylvan Lake); Folake Adeniji (Shoppers Drug Mart #310, Leduc); Brad Couldwell and Trudy Arbo (Shoppers Drug Mart #321, Calgary); Anita and Reid McDonald (Sunset Ridge Pharmacy, Calgary); Jacki Swindelhurst (Rexall Pharmacy #7245, Drayton Valley).
Footnotes
Author Contributions:Al Hamarneh, Johnston, Marra and Tsuyuki designed the study. Al Hamarneh and Johnston were involved in the data acquisition, analysis, interpretation and drafting the manuscript. Al Hamarneh, Johnston, Marra and Tsuyuki reviewed and approved the manuscript. All authors have made substantial contributions to the manuscript.
Funding:We would like to acknowledge the funders of RxEACH: Alberta Health (Workforce Planning), Cardiovascular Health and Stroke Strategic Clinical Network of Alberta Health Services and Merck Canada (investigator-initiated funding for the educational program).
We would like to acknowledge the data management and statistical support provided by the Consultation and Research Services Platform at the Alberta SPOR SUPPORT Unit.
None of our funders had any role in the study design, collection, analysis, interpretation of the data, writing the report and the decision to submit for publication.
Financial Disclosure: Drs. Al Hamarneh, Tsuyuki, Johnston and Marra declare they have no relevant financial interests.
References
- 1. World Health Organization. Cardiovascular diseases (CVDs). 2017. Available: www.who.int/mediacentre/factsheets/fs317/en/ (accessed Jul. 27, 2018).
- 2. Government of Canada. Heart disease—heart health. 2017. Available: https://www.canada.ca/en/public-health/services/diseases/heart-disease-heart-health.html (accessed Jul. 27, 2018).
- 3. Al Hamarneh YN, Rosenthal M, Tsuyuki RT. Glycemic control in community-dwelling patients with type 2 diabetes. Can Pharm J (Ott) 2012;145(2):68-69.e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leiter LA, Berard L, Bowering CK, et al. Type 2 diabetes mellitus management in Canada: is it improving? Can J Diabetes 2013;37(2):82-9. [DOI] [PubMed] [Google Scholar]
- 5. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380(9859):2224-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zillich AJ, Sutherland JM, Kumbera PA, Carter BL. Hypertension outcomes through blood pressure monitoring and evaluation by pharmacists (HOME study). J Gen Intern Med 2005;20(12):1091-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Heart Research Institute. Facts about heart disease. 2018. Available: http://www.hricanada.org/about-heart-disease/facts-about-heart-disease (accessed Jul. 27, 2018).
- 8. Shiu J, Simpson S, Johnson J, Tsuyuki R. Quantifying opportunities to affect diabetes management in the community. Can Pharm J (Ott) 2006;139(3):37-8. [Google Scholar]
- 9. McLean DL, McAlister FA, Johnson JA, et al. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: Study of Cardiovascular Risk Intervention by Pharmacists–Hypertension (SCRIP-HTN). Arch Intern Med 2008;168(21):2355-61. [DOI] [PubMed] [Google Scholar]
- 10. Santschi V, Chiolero A, Burnand B, Colosimo AL, Paradis G. Impact of pharmacist care in the management of cardiovascular disease risk factors: a systematic review and meta-analysis of randomized trials. Arch Intern Med 2011;171(16):1441-53. [DOI] [PubMed] [Google Scholar]
- 11. Scott DM, Boyd ST, Stephan M, Augustine SC, Reardon TP. Outcomes of pharmacist-managed diabetes care services in a community health center. Am J Health Syst Pharm 2006;63(21):2116-22. [DOI] [PubMed] [Google Scholar]
- 12. Tsuyuki RT, Al Hamarneh YN, Jones CA, Hemmelgarn BR. The effectiveness of pharmacist interventions on cardiovascular risk: the multicenter randomized controlled RxEACH trial. J Am Coll Cardiol 2016;67(24):2846-54. [DOI] [PubMed] [Google Scholar]
- 13. Tsuyuki RT, Johnson JA, Teo KK, et al. A randomized trial of the effect of community pharmacist intervention on cholesterol risk management: the Study of Cardiovascular Risk Intervention by Pharmacists (SCRIP). Arch Intern Med 2002;162(10):1149-55. [DOI] [PubMed] [Google Scholar]
- 14. Stevens RJ, Kothari V, Adler AI, Stratton IM, Holman RR. The UKPDS risk engine: a model for the risk of coronary heart disease in type 2 diabetes (UKPDS 56). Clin Sci 2001;101(6):671-9. [PubMed] [Google Scholar]
- 15. D’Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008;117(6):743-53. [DOI] [PubMed] [Google Scholar]
- 16. Wilson PWF, D’Agostino R, Bhatt DL, et al. An international model to predict recurrent cardiovascular disease. Am J Med 2012;125(7):695-703. [DOI] [PubMed] [Google Scholar]
- 17. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-Year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008;359(15):1577-89. [DOI] [PubMed] [Google Scholar]
- 18. Canadian Agency for Drugs and Technologies in Health. Guidelines for the economic evaluation of health technologies: Canada 2018. Available: https://www.cadth.ca/about-cadth/how-we-do-it/methods-and-guidelines/guidelines-for-the-economic-evaluation-of-health-technologies-canada (accessed Jul. 27, 2018). [Google Scholar]
- 19. Pocock SJ, McCormack V, Gueyffier F, Boutitie F, Fagard RH, Boissel JP. A score for predicting risk of death from cardiovascular disease in adults with raised blood pressure, based on individual patient data from randomised controlled trials. BMJ 2001;323(7304):75-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mittmann N, Seung SJ, Hill MD, et al. Impact of disability status on ischemic stroke costs in Canada in the first year. Can J Neurol Sci 2012;39(6):793-800. [DOI] [PubMed] [Google Scholar]
- 21. Sorensen SV, Kansal AR, Connolly S, et al. Cost-effectiveness of dabigatran etexilate for the prevention of stroke and systemic embolism in atrial fibrillation: a Canadian payer perspective. Thromb Haemost 2011;105(5):908-19. [DOI] [PubMed] [Google Scholar]
- 22. Bentkover JD, Stewart EJ, Ignaszewski A, Lepage S, Liu P, Cooper J. New technologies and potential cost savings related to morbidity and mortality reduction in class III/IV heart failure patients in Canada. Int J Cardiol 2003;88(1):33-41. [DOI] [PubMed] [Google Scholar]
- 23. McGillion MH, Croxford R, Watt-Watson J, et al. Cost of illness for chronic stable angina patients enrolled in a self-management education trial. Can J Cardiol 2008;24(10): 759-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Coyle D, Coyle K, Cameron C, et al. Cost-effectiveness of new oral anticoagulants compared with warfarin in preventing stroke and other cardiovascular events in patients with atrial fibrillation. Value Health 2013;16(4):498-506. [DOI] [PubMed] [Google Scholar]
- 25. Canadian Institute of Health Information. National health expenditure trends. Table E. 1.16.2. Available: https://secure.cihi.ca/free_products/nhex_trends_narrative_report_2015_en.pdf (accessed May 17, 2019). [Google Scholar]
- 26. Sullivan PW, Lawrence WF, Ghushchyan V. A national catalog of preference-based scores for chronic conditions in the United States. Med Care 2005;43(7):736-49. [DOI] [PubMed] [Google Scholar]
- 27. Statistics Canada. Health reports: population health impact of statin treatment in Canada (Appendix A) 2017. https://www150.statcan.gc.ca/n1/pub/82-003-x/2016001/article/14305/tbl/tbla1-eng.htm (accessed Jul. 27, 2018).
- 28. Statistics Canada. High blood pressure, by sex, and by province and territory 2014. Available: www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/health70a-eng.htm (accessed Jul. 27, 2018).
- 29. Statistics Canada. Blood pressure of adults, 2012 to 2015. Available: www.statcan.gc.ca/pub/82-625-x/2016001/article/14657-eng.htm (accessed Jul. 27, 2018).
- 30. Marra C, Johnston K, Santschi V, Tsuyuki RT. Cost-effectiveness of pharmacist care for managing hypertension in Canada. Can Pharm J (Ott) 2017;150(3):184-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kaul P, Reed SD, Hernandez AF, et al. Differences in treatment, outcomes, and quality of life among patients with heart failure in Canada and the United States. JACC Heart Fail 2013;1(6):523-30. [DOI] [PubMed] [Google Scholar]
- 32. Canadian Pharmacists Association. 2016 Fees and claims data for government-sponsored pharmacist services, by province. Available: www.pharmacists.ca/cpha-ca/assets/File/pharmacy-in-canada/CFP_prov_chart_june_2014.pdf (accessed May 17, 2019) 2016. [Google Scholar]
- 33. Statistics Canada. Consumer Price Index, monthly, not seasonally adjusted, Canada, provinces, Whitehorse and Yellowknife—health and personal care. 2018. Available: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1810000408. (accessed Dec. 3, 2018).
- 34. Canadian Institute of Health Information. National health expenditure trends. 2015. Available: https://secure.cihi.ca/free_products/nhex_trends_narrative_report_2015_en.pdf (accessed July 27, 2018).
- 35. Omboni S, Caserini M. Effectiveness of pharmacist’s intervention in the management of cardiovascular diseases. Open Heart 2018;5:e000687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Altowaijri A, Phillips CJ, Fitzsimmons D. A systematic review of the clinical and economic effectiveness of clinical pharmacist intervention in secondary prevention of cardiovascular disease. J Manag Care Pharm 2013;19(5): 408-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Alberta Health. Pharmacy funding framework 2018. Available: http://www.health.alberta.ca/services/pharmacy-funding-framework.html (accessed July 27, 2018).
- 38. Al Hamarneh YN, Lamb S, Donald M, et al. Pharmacist prescribing and care improves cardiovascular risk, but what do patients think? A substudy of the RxEACH study. Can Pharm J (Ott) 2018;151(4):223-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Canadian Pharmacists Association. Pharmacists in Canada 2018. Available: https://www.pharmacists.ca/pharmacy-in-canada/pharmacists-in-canada (accessed July 27, 2018).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, 851822_App1_online_supp for Pharmacist prescribing and care improves cardiovascular risk, but is it cost-effective? A cost-effectiveness analysis of the RxEACH study by Yazid N. Al Hamarneh, Karissa Johnston, Carlo A. Marra and Ross T. Tsuyuki in Canadian Pharmacists Journal / Revue des Pharmaciens du Canada