Abstract
People with diabetes have been experimenting and self-modifying diabetes devices and technologies for many decades, in order to achieve the best possible quality of life and improving their long-term outcomes. There are now hundreds of individuals using DIY closed loop systems globally. They work similarly to commercial systems at a basic level, automatically adjusting and controlling insulin dosing, but are different in terms of transparency, access, customization, and usability. The potential downsides to DIY closed looping include varying responses from individual HCPs, who may be concerned about their own liability. However, initial outcomes from this self-selected community (including adult and pediatric populations globally) have been positive. There have now been several studies documenting improvements in A1c, time in range, and other outcomes such as quality-of-life benefits. More studies on quality-of-life improvements and more collaboration between companies and the community are recommended.
Keywords: artificial pancreas, APS, OpenAPS, closed loop, automated insulin delivery system, #WeAreNotWaiting
Open source artificial pancreas technology.1 Do-it-yourself remote monitoring software.2 Self-replacing of CGM transmitter batteries.3 These are just a few of the projects that have emerged as part of the #WeAreNotWaiting community, a social media mantra that describes one of the motivations behind do-it-yourself (DIY) diabetes.
However, DIY in diabetes is not new. People with diabetes have been experimenting and self-modifying diabetes devices and technologies for many decades, in order to achieve the best possible quality of life and improving their long-term outcomes. Self-monitoring blood glucose testing is one such example of this phenomenon.4 More than 95% of diabetes care is done by the person living with diabetes.5 As new technology becomes available, people with diabetes have taken full advantage of it, and the resulting DIY methods appear to have snowballed.6
This commentary will address DIY closed looping: how it was developed and how it works; potential benefits and documented outcomes from and by this self-selected population; potential disadvantages of this approach; and perspective on where DIY is going and how it effects other diabetes technology development.
How the DIY Closed Looping Project and Movement Began
In November 2013, I stumbled across an old tweet from John Costik, demonstrating that he was accessing his son’s CGM data remotely. We reached out, interested in learning how he had accomplished this. John was willing to share his code, enabling me to upload my CGM data via a local computer and send it into the cloud. This enabled me to achieve a key goal of creating louder alerts than my CGM receiver was capable of. With additional data I tracked (insulin dosing and food), we iterated and built an algorithm that predicted the impact on BG levels over time, resulting in predictive alarms and recommended actions. Without planning to, we had built what researchers call an “open loop” system.
Months later, we met and began working with Ben West, who had reverse engineered the communication protocols of certain insulin pumps. We realized that if we combined the ability to control the pump with our algorithm, we could close the loop. We did (in December 2014), and then decided to open source our work, launching the OpenAPS (the open source artificial pancreas system) movement.
How DIY Closed Loop Systems Work
The first DIY closed loop system contained basic components of a mini-computer to hold the algorithm; a radio stick to communicate with the pump using its proprietary 915MHz radio protocol; a battery; and an existing insulin pump and CGM. There is an emergence (in Europe and Asia) of modern Bluetooth-enabled pumps on the commercial market that, instead of requiring custom radio hardware, allow a mobile device (phone) to connect directly to the insulin pump. These mobile devices can host the algorithm7 and communicate with the insulin pump directly.
Most DIY systems are built using the safety principles we spelled out in early 2015 prior to sharing any code, which we called the OpenAPS Reference Design.8 Recognizing the limitations of both hardware and software—and prioritizing safety—the reference design articulates the principles behind dealing with missing or faulty CGM data and loss of communication with the pump. For safety, the system is designed to simply fall back to standard insulin pump therapy. Additionally, it is designed around the same diabetes math a patient would be doing manually, and it is open and transparent about how it works (and what and why it is taking any action or not) at all times.
Generally speaking, most closed loop algorithms work similarly: they collect CGM data and previous insulin dosing and food information; forecast into the future what BG values will be over time; and issue insulin dosing commands to the pump in order to modulate insulin delivery to help bring the eventual BG into range. This is true for both commercial and DIY closed loop systems. However, the major differences come down to customization and flexibility of feature sets. With DIY systems, there are a wide range of features that can be enabled or adjusted by the individual. There are also interoperability benefits: the person with diabetes can choose their pump, CGM, algorithm, and feature set of choice. They can also use the mobile device(s) of choice for remote monitoring and interacting with their closed loop system, allowing targets to be set or carbohydrates to be entered from mobile devices and smart watches.
While most DIY closed looping is thought of as similar to traditional hybrid closed looping, where patients still bolus and announce meals, advancements have continued to have been made in DIY algorithms. Many people choose to enable features that allow them to skip meal announcements and/or the requisite meal bolus while still achieving improvements in outcomes compared to manual diabetes care. Such “fully automated” diabetes care is still years away for commercial systems.
Potential Benefits of DIY Closed Loop Systems
It is probably not surprising that closed loop systems improve clinical outcomes of diabetes. Like users of traditionally developed closed loop systems (by academia and industry), DIY closed loop users observe improved time in range, decreases in A1c, and less time spent high and low. In 2016, a self-reported outcomes study was presented,9 quantifying these improvements. Feedback from the medical community was positive, although there was much interest in additional data and studies from this community. Therefore, in 2018, the community presented another data set (this time not self-reported) analyzing outcomes before and after OpenAPS implementation.10 Additionally, two additional international groups from Italy11 and Korea12 also presented study results analyzing real-world outcomes from DIY closed loop users there. The studies’ results are aggregated and illustrated in Figures 1-3.
Figure 1.
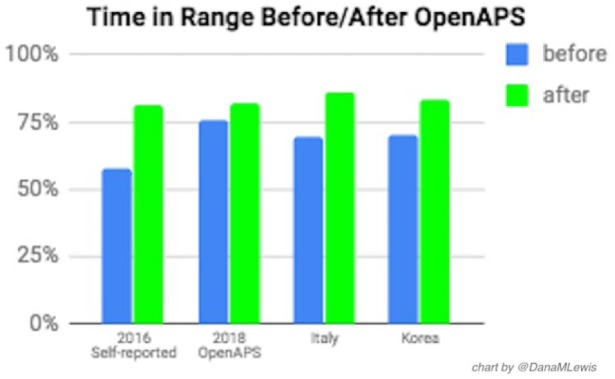
Time in range before/after DIY closed loop initiation.
Figure 2.
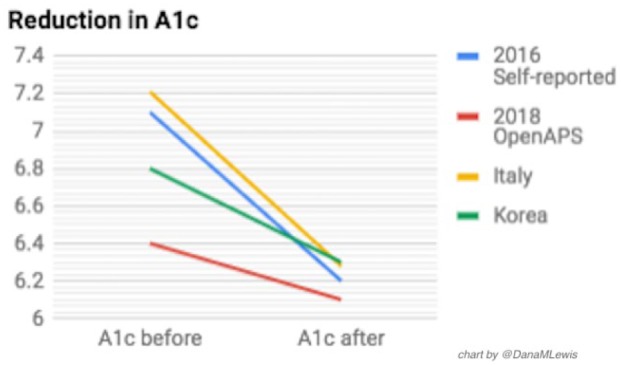
A1C before/after DIY closed loop initiation.
Figure 3.
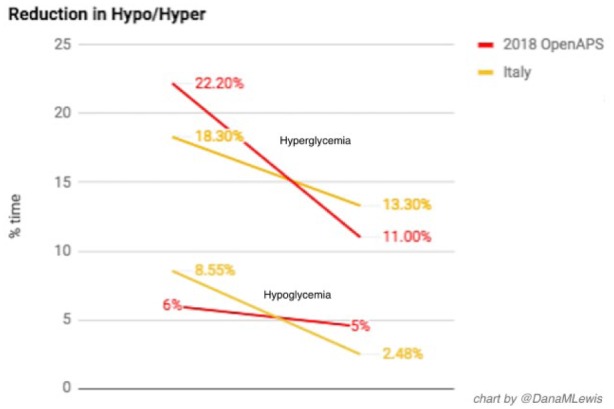
Hypoglycemia and hyperglycemia before/after DIY closed loop initiation.
In addition to clinical outcomes, there are also significant quality-of-life improvements when using a DIY closed loop.
In the 2016 self-reported outcomes study, we surveyed users about sleep, and 56% reported a large improvement in sleep quality. Individuals in the community have also worked to quantify their quality-of-life improvements in other ways.13 Sulka Haro quantified treatment reductions after implementing OpenAPS. With OpenAPS, his family went from 4.5 treatments to less than one (0.7 average/day) treatment per day. Dr Jason Wittmer tallied school nurse visits: before OpenAPS (4th grade) his son averaged 2.3 visits per day (420 total); after OpenAPS (6th grade), his son visited the school nurse 5 times in the entire school year.
Other families and individuals with diabetes also share feedback regularly online about quality-of-life improvements that include improved family dynamics (less time spent discussing diabetes and less friction in interactions caused by diabetes), improved family communication around diabetes, improved sleep for multiple family members, and reduced amount of time spent thinking about diabetes and doing diabetes-related tasks (reduction in cognitive burden).
There are a variety of quality-of-life impacts of this technology, and the community also hopes to see traditional and commercial closed loop studies also begin to document and demonstrate these benefits as well.
Potential Disadvantages of DIY Closed Loop Systems
There is a range of potential disadvantages of DIY closed loop systems.
The most obvious and most pointed-to disadvantages are a result of the technical and hardware limitations of the limited number of insulin pumps on the market that have the remote control ability to receive temporary basal rate commands. (These limitations are in part due to a lack of standardized and open protocols at the time of pump development; JDRF’s Open Protocol Initiative, and the FDA’s efforts around approving iPumps, iCGMs, and iAlgorithms, may help future devices.)14 In most countries, these older generation pumps are also no longer in warranty, and not available through insurance or the commercial market. Because additional hardware is required to communicate to these pumps, there is an extra communication step and point of possible failure. In these and other ways, the DIY systems are limited to the capabilities of these existing pumps.
Because additional hardware (a controller device, compatible pump, and/or new mobile phone) is usually required to build a DIY closed loop, the decision to do so comes with a financial cost. These costs are not covered by insurance. (However, these costs are generally modest, and usually cheaper than access to commercial closed loop technology.)
Additionally, there are perceived and real technical barriers to DIY closed looping. Although many hundreds of individuals,15 often with no tech experience, have built DIY closed loop systems, not everyone is comfortable or willing to DIY. While there are many individuals interested in DIY closed loop systems, some are unwilling or unable to try to DIY. DIY is unfortunately not 100% accessible to all; and although there is a supportive community willing to help those who have the time and resources and ability to learn about it, not every person with diabetes is able to do so.
One other major disadvantage to DIY is that some health care providers (HCPs) are uncomfortable. Some pushback is due to discomfort with an unknown solution: many prefer to trust the regulatory stamp of approval (and DIY is not regulatory approved). Some concern is around patient safety, and concern for individual patients’ capabilities and skills for using such technology.
However, the biggest body of concern is around liability16 (or perceived liability) to the HCP for the choices a patient makes. Laws, regulations, and cultural practice differ from country to country. In some places, patients choosing to use their medical devices off-label in conjunction with DIY devices is not a concern to their HCPs. In other places, a HCP is perceived to be liable for the choices a patient makes, even if the HCP is not prescribing or recommending the approach or device. Even within the same country, opinions differ among HCPs, increasing confusion.
This confusion and range of responses by HCPs results in a problematic situation, where patients may not feel comfortable telling their HCPs about the technologies they’re choosing to use, for fear of retribution (such as being reported and/or threatened legally; the HCP refusing to write prescription insulin pump supplies; or being fired as a patient).
However, position statements such as the recently released position statement by Diabetes Australia on people with type 1 diabetes and DIY technology solutions17 makes it clear that people with diabetes should have choice in their technology; and regardless of personal choice, should continue to receive support and care from HCPs.
Where DIY Is Going and How It Will Impact Industry
The commercial medical device industry has a huge opportunity to leverage a wide-ranging body of knowledge from the patient community that is using DIY technology. This should include learning from the DIY community’s real-world experience on which types of features, approaches, and algorithms are safest and most effective, as well as learning from the DIY community’s experience helping others with the learning curve involved in moving from manual to partially and fully automated diabetes care.18 There have been a few successful examples of collaboration and knowledge sharing between DIY and commercial companies, but there are still many more such opportunities to more rapidly advance technology for people with diabetes. Results from these types of collaborations can include improvements in research design and prioritization, codesign of more flexible products and services, and helping HCPs better understand how to help patients best leverage technology.
Although most activities of the DIY community are noncommercial, most of what has been produced is also freely available to be used today by commercial companies. Any company or organization that wishes to do so can leverage and scale it out using their own regulatory and quality systems, and solve some of the accessibility barriers that DIY technologies currently face by turning them into business opportunities.
Conclusion
Clinicians, companies, and patients ultimately have the same shared goal of improving the lives of people with diabetes. Collaborating together, we can achieve this even more quickly for many more people.
Acknowledgments
OpenAPS and other DIY closed loop technology would not be possible without years of work by dozens of contributors to the open source, DIY “#WeAreNotWaiting” diabetes community. Thanks to each and every person who has contributed to the body of knowledge of hybrid closed looping, in particular the hundreds of #OpenAPS community “loopers” who have donated their data and experiences of living with DIY closed loops.
Footnotes
Abbreviations: AP/APs or APS, artificial pancreas/artificial pancreas system; BG, blood glucose; CGM, continuous glucose monitor; DIY, do it yourself; HCP; health care provider.
Declaration of Conflicting Interests: The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author received no financial support for the research, authorship, and/or publication of this article.
References
- 1. OpenAPS. Open APS. 2015. Available at: https://OpenAPS.org. Accessed August 24, 2018.
- 2. Lee JM, Newman MW, Gebremariam A, et al. Real-world use and self-reported health outcomes of a patient-designed do-it-yourself mobile technology system for diabetes: lessons for mobile health. Diabetes Technol Ther. 2017;19(4):209-219. [DOI] [PubMed] [Google Scholar]
- 3. Niezen G, Eslambolchilar P, Thimbleby H. Open-source hardware for medical devices. BMJ. 2016;2:78-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bernstein R. Blood glucose self-monitoring by diabetic patients: refinements of procedural technique. Diabetes Care. 1979;2:233-236. [DOI] [PubMed] [Google Scholar]
- 5. Funnell MM, Anderson RM. The problem with compliance in diabetes. JAMA. 2000;284:1709. doi: 10.1001/jama.284.13.1709-JMS1004-6-1. [DOI] [PubMed] [Google Scholar]
- 6. Litchman ML, Lewis D, Kelly LA, Gee PM. Twitter analysis of #OpenAPS DIY artificial pancreas technology use suggests improved A1C and quality of life. J Diabetes Sci Technol. 2019;13:164-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. AndroidAPS. AndroidAPS Documentation. 2018. Available at: http://wiki.AndroidAPS.org. Accessed August 24, 2018.
- 8. OpenAPS. Reference Design. 2015. Available at: https://openaps.org/reference-design/. Accessed on August 24, 2018.
- 9. Lewis D, Leibrand S. Real-world use of open source artificial pancreas systems. J Diabetes Sci Technol. 2016;10:1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lewis DM, Swain RS, Donner TW. Improvements in A1C and time-in-range in DIY closed-loop (OpenAPS) users. Diabetes. 2018;67(suppl 1). Available at: 10.2337/db18-352-OR. [DOI] [Google Scholar]
- 11. Provenzano V, Guastamacchia E, Brancato D, et al. Closing the loop with OpenAPS in people with type 1 diabetes—experience from Italy. Diabetes. 2018;67(suppl 1). Available at: 10.2337/db18-993-P. [DOI] [Google Scholar]
- 12. Choi SB, Hong ES, Noh YH. Open artificial pancreas system reduced hypoglycemia and improved glycemic control in patients with type 1 diabetes. Diabetes. 2018;67(suppl 1). Available at: 10.2337/db18-964-P. [DOI] [Google Scholar]
- 13. DIYPS. Presentations and poster content from @DanaMLewis at #2018ADA. Available at: https://diyps.org/2018/06/23/presentations-and-poster-content-from-danamlewis-at-2018ada/. Accessed August 24, 2018.
- 14. DIYPS. More open innovation coming soon? Available at: https://diyps.org/2017/10/18/more-open-innovation-coming-soon/. Accessed September 26, 2018.
- 15. OpenAPS. OpenAPS Outcomes. 2018. Available at: https://openaps.org/outcomes/. Accessed August 24, 2018.
- 16. Barnard K, Ziegler R, Klonoff D. Open source closed-loop insulin delivery systems: a clash of cultures or merging of diverse approaches?. J Diabetes Sci Technol. 2018;12: 1223-1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Diabetes Australia. Position statement: people with type 1 diabetes and do it yourself (DIY) technology solutions. 2018. Available at: https://static.diabetesaustralia.com.au/s/fileassets/diabetes-australia/ee67e929-5ffc-411f-b286-1ca69e181d1a.pdf. Accessed August 24, 2018.
- 18. Lewis D. Setting expectations for successful artificial pancreas/hybrid closed loop/automated insulin delivery adoption. J Diabetes Sci Technol. 2018;12:533-534. [DOI] [PMC free article] [PubMed] [Google Scholar]


