Abstract
Multiple factors hinder the management of diabetes in hospitals. Amid the demands of practice, health care providers must collect, collate, and analyze multiple data points to optimally interpret glucose control and manage insulin dosing. Such data points are commonly dispersed in different sections of electronic health records (EHR), and the system for data display and physician interaction with the EHR are often poorly conducive to seamless clinical decision making. In this perspective article, we examine challenges in the process of EHR data retrieval, interpretation and decision making, using glucose management as an exemplar. We propose a conceptual, systems-based design for closing the loop between data gathering, analysis and decision making in the management of inpatient diabetes. This concept capitalizes on attributes of the EHR that can enable automated recognition of cases and provision of clinical recommendations.
Keywords: electronic health records, inpatient diabetes, clinical decision making, clinical decision support, health care value, dispersed data
There is an increasing demand to improve quality of care, patient safety, and patient satisfaction while reducing health care costs.1 However, using diabetes as an example, gaps in decision making and clinical management often hinder achieving these goals. In diabetes, glycemic control for hospitalized patients is often suboptimal, there are knowledge gaps, and providers are under significant cognitive load and often focused on the primary clinical problem that is before them.2-5 Even when providers proactively attend to glucose management, the complexity of the task is increased by data that are dispersed, residing in various different locations in electronic health records (EHRs), and requiring significant effort to collate, analyze, and integrate into clinical decisions. Such data include test results, capillary glucose measurements, medication (mostly insulin) administration, clinical status, and nutritional orders. When this information is not appropriately assimilated, it can be assumed that the process can result in suboptimal decision making and poorer outcomes.
In this article, we articulate how bringing together dispersed information in the EHR can support providers’ clinical decision making. We use a clinical scenario to illustrate the “discordance” between data influx and clinical decision making that is fueled by dispersed data elements in the EHR. We propose a conceptual method for designing clinical decision support systems to help address the problem of dispersed data in diabetes management and to optimize glycemic control, and suggest that this method can be applied to a variety of medical issues across disciplines.
The Pursuit of Glucose Control in the Hospital and the Evolving Landscape of Systems of Practice
Inpatient providers across disciplines are in need to care for patients with diabetes at a growing rate and in the midst of increasingly complex and demanding clinical practices. Poor outcomes associated with dysglycemia among hospitalized patients, the growing prevalence of diabetes, and the disproportionate demand versus supply of endocrinologists, including limited availability of diabetes teams in hospitals nationwide, place an increasing demand on primary inpatient teams to effectively provide glucose management in hospitals. As teams address the clinical condition(s) that results in their patients’ hospitalization, inpatient diabetes management is often flawed by multiple barriers including knowledge and attitudinal gaps, complex workflows, and deficient systems.2-4,6,7
Hyperglycemia and hypoglycemia are common scenarios among hospitalized patients with diabetes. While cause-effect association has not been clearly established, both conditions, regardless of an existing diagnosis of diabetes, seem to confer greater risk for poor clinical outcomes such as morbidity, mortality, use of resources, and hospital costs.8,9 Many barriers hinder achieving adequate glucose control in the hospital. The failure to proactively address dysglycemia among hospitalized patients has been coined as “clinical inertia.”10 The practice of using sliding scales as monotherapy in patients with hyperglycemia is ubiquitous and departs from clinical practice recommendations endorsed by professional societies.9,11-13 Stress hyperglycemia is a common scenario that portrays poor outcomes, yet its clinical impact is often overlooked.14,15
Systems of practice are evolving to accelerate the utilization of clinical informatics for health care delivery. The use of EHRs is rapidly advancing motivated by concerns for the “Quality Chasm” in the US health care system.16 The relevance and need for support of better information technology became more apparent following reports by the Institute of Medicine of harm, errors, and deficiencies resulting in poor quality of care.17-19
Evidence of the evolving value of health information technology has been summarized in systematic reviews. This evidence relates to reduction in medical errors, and adherence to clinical guidelines, improvement in surveillance and monitoring, reduction in laboratory redundancy, shortening in hospitals length of stay, and improvement in patient safety.20 EHR adoption and demonstration of benefits are steadily increasing since the inception of the Health Information Technology for Economic and Clinical Health (HITECH) Act in 2010, as part of the American Recovery and Reinvestment Act (ARRA). Ultimate goals related to the use of EHR are to attain better clinical outcomes, increase transparency and efficiency, strengthen population health outcomes, empower individuals, and create robust research data on health systems. These advances related to “meaningful use” of the EHR are tied to financial incentives through the Centers for Medicare & Medicaid Services (CMS).21
Dispersed Data and the Complexity of Managing of Dysglycemia in the Hospital
Consider the following clinical scenario, in which a hospitalist team is committed to optimal glucose management, through daily assessment of glycemic control and adequate insulin dosing and adjustment for the patients it serves. For any given patient receiving subcutaneous insulin, interpretation of glucose control in relation to the type of insulin administered (basal, prandial, and/or correction), as well as assessment of nutritional status, is required at a minimum of four different time points within 24 hours. Caution in reducing or withholding insulin doses will be particularly important in patients with type 1 diabetes, due to the risk for diabetic ketoacidosis. Patients who demonstrate frequent hyperglycemia and occasional hypoglycemia (both common occurrences) will require careful review of insulin doses in relationship to glucose patterns on a daily basis. The team will need to pay attention to special situations such as hyperglycemia associated with steroids, stress hyperglycemia, enteral and parenteral nutrition, transfer between hospital units, and changes in clinical status. Such conditions may occur in multiple patients under the care of the team.
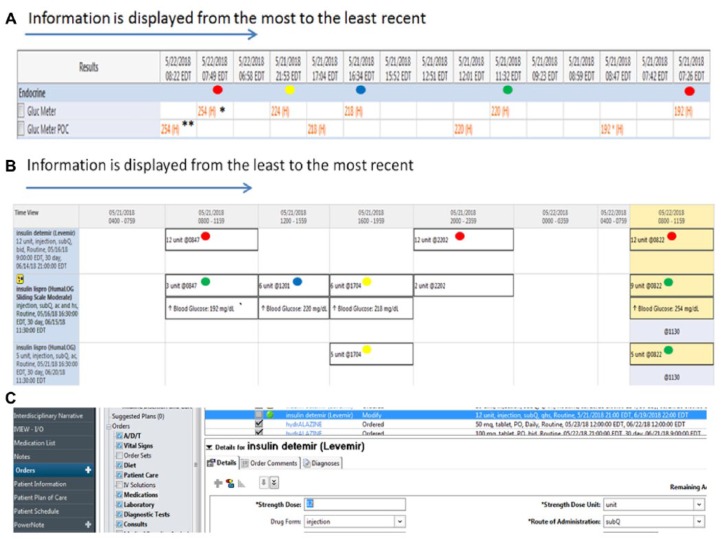
Now, to manage such a panel, the team will need to gather, collate, and analyze data, and will need to make decisions and order appropriate management, all through the EHR. Figures 1a, 1b, and 1c provide examples of how this would be done through a typical EHR. Capillary glucose results in the EHR do not display in a way that facilitates either glucose pattern recognition nor insulin dosage adjustments. For example, glucose control prior to lunch for the patient in this example is in part determined by the dose of insulin administered prior to breakfast. However, decisions regarding increasing the prebreakfast insulin dosage require the clinicians to recognize a pattern of hyperglycemia at lunch time “today” and “yesterday.” Once this is accomplished, information about administered insulin doses needs to be accessed from a completely different screen and section of the EHR. Insulin administration information, glucose results, and the medication list and order menu options appear in separate sections in the EHR making the process of data retrieval and interpretation more cumbersome and nonintuitive.
Figure 1.
Example of an EHR glucose and insulin data display and provider interaction.
(a) Display of glucose data. In this table, blood glucose values stored in the EHR are displayed from the most to the least recent. Repeated (duplicated) numbers shown in the table (example, glucose level 254 marked with asterisks) represent point-of-care (POC) results** that are manually recorded in the EHR and electronically downloaded from the glucose meter* to the computer. The same concept applies to other repeated values in the table. Providers need to be aware that in some instance this may occur because these repeated values could be incorrectly interpreted as different results and this may lead to inadequate decisions on insulin adjustment. The colored dots (not part of EHR display but shown here to facilitate interpretation of glucose control in relation to insulin treatment) indicate the different times within a 24-hour period that glucose values need to be interpreted to assess the effect of previously administered insulin doses. The times include before breakfast-fasting: red dot, lunch: green dot, supper: blue dot, and prior to bedtime: yellow dot. In addition, this interpretation typically needs to be extended beyond 24 hours for recognition of glycemic patterns to have informed decision making for subsequent insulin adjustments . Providers using this EHR would need to decide which data to use (eliminating duplicate values), and mentally organize the data on their own, using the time stamps above each value, without having visual cues such as the colored dots added.
(b) Display of insulin administration record. This chart illustrates a typical EHR medical administration record, which is found in a separate section of the EHR (requiring the physician to click away from the data screen above), and contains information about the insulin regimen scheduled and the doses received. The colored dots (not part of this EHR) shown next to the insulin doses correspond to the glucose values in Figure 1a. This particular display of information shows insulin treatment scheduled or received before breakfast-fasting: red dot, lunch: green dot, supper: blue dot, and prior to bedtime: yellow dot. Clinicians need to interpret the glycemic response to such doses at various times of the day. Each mealtime glucose status-insulin schedule pairing requires an independent interpretation. This is because the dose of insulin given at the time of a meal will determine the glucose level prior to the next meal. Likewise, basal insulin will influence fasting control (red dot), which in turn, will determine how the basal dose may be adjusted. The regimen shown is applicable for patients who are scheduled to receive meals. The approach and thought process will differ for those who are not being fed, who are receiving enteral or parenteral nutrition, or who require intravenous insulin.
(c) Implementing a glucose management plan. After adequate interpretation of glucose results (Figure 1a) and confirmation of insulin doses administered (Figure 1b), providers then need to exit out of the EHR views above and subsequently access the medication list or orders menu to make changes to the insulin doses as required (Figure 1c).
As evident in this scenario, data influx through the EHR and the challenges of its access and interpretation can result in a disjointed loop of clinical decisions and suboptimal management outcomes for diabetes care. Paradoxically, it may be assumed the onus is on inpatient providers, regardless of their training or clinical background, to discern the intricacies of glycemic management and to provide evidence-based quality care amid sometime dysfunctional systems of practice. However, the system is designed to thwart even those who want to manage adequately. Nonetheless, there are expectations for practice performance, quality of care, patient safety, and overall accountability in care despite the existing seemingly disjointed loops. In the case discussed, some of these expectations include interpretation of glucose patterns in view of nutritional status, insulin dose selection and adjustment for control of hyperglycemia and prevention of hypoglycemia, changes in clinical status, and efforts toward adequate transitions of care among other factors. A cognitive theory was proposed by Bowen and colleagues on the process of clinicians’ interaction with computers to interpret and use inpatient glucose data. A user-centered data display prototype was coined to facilitate clinical decision making for glycemic management in the hospital.22
Countering Data Dispersion with Clinical Decision Support
EHRs contain rich data that needs to be leveraged to become actionable. However, converting data into useful information is challenging.23 As shown in our case scenario, hospital glycemic management requires frequent assessment of multiple glucose results and patterns, and response to type and time of insulin administration. This has been traditionally a responsibility of primary admitting teams, hospitalists, and endocrine consultants when available to hospitals. Some studies demonstrated benefits of using EHR glucose data reports and computed-based assessments of glycemic control.24-27 This approach facilitated decision for consultation by endocrinologists24,25 or for provision of virtual consultations and recommendations through the EHR by members of a diabetes team.25,26 These studies demonstrated significant improvement in glycemic control.24-27 The idea of remote glucose monitoring in hospitals is attractive as it offers an innovative approach to generate efficiency in the recognition and management of patients requiring better glycemic control and insulin prescription. Virtual consultations can also represent an educational tool for the providers receiving recommendations for management.26 The downside to real-time consultation is that it is time and resource intensive, and may require access to specialist consultants that hospitals may or may not have.
As hospitals continue the quest for improvements in efficiency, access to care, safety, quality and cost containment, there is a need to continue identifying innovative methods to address poor inpatient glycemic states. Data related to status of glucose control and insulin dosing recommendations can be intelligently queried in the EHR to generate patients’ specific information that can be tied to management recommendations.28 This is one example, among many, how EHRs can facilitate clinical decision support to enhance health care.29
Clinical decision support (CDS) systems refer to electronic systems designed to assist in clinical decision making by provision of specific recommendations tailored to patients’ characteristics. Benefits of CDS systems have been demonstrated in facilitating preventive care services, requesting necessary clinical studies, and prescribing treatments.30 Providing decision support to clinicians results in improved decision making leading to improved quality and efficiency in patient care.31 Implementing clinical support rule(s) and monitoring compliance with the rules are among the core set of objectives to demonstrate meaningful use of EHR by clinical organizations.32
We propose an automated EHR method to recognize dysglycemia, to coherently align dispersed actionable glucose data, and to provide clinical recommendations through a messaging system at the point of care. We envision that such a clinical decision support approach can enable optimization of glucose management and related outcomes in hospitals and can be accessible to resource-limited institutions. In alignment with virtual diabetes consults, our proposed approach has the potential to expedite assessment and recommendations. Furthermore, it can expand on the number of cases addressed at any given point in time, reduce professional effort resulting from rounding activities, and provide education to providers in the context of practice. In contrast with remote monitoring and virtual consults, this method can further reduce labor of chart reviews and manual inclusion of recommendations. This can provide a service to hospitals without endocrine consultants or diabetes consult teams, thus potentially ameliorating the demand-supply mismatch between numbers of diabetes patients in hospital and diabetes specialists at a large scale. This model operationalizes the expert process of review of glucose data and insulin treatment, while providing prompt recommendations in real time.28
In Table 1 we present an algorithmic design of a clinical decision support system for the management of hyperglycemia in the hospital that can be used in the design of alerts or messaging system to health care providers. The design of such algorithm requires understanding of clinical indicators that are relevant in decision making and the nuances of clinical working environments. It provides an outline for key steps in designing a CDS tool, shows the application of the key steps to a clinical problem, and proposes how the design may help integrate dispersed EHR data and positively impact the care of patients with hyperglycemia in the hospital. As shown, this design does not present the technical elements to program automated messages which would be unique to electronic records programs hospitals may use. The concept of clinical decision support can be extended to other diabetes management scenarios such as hypoglycemia or inadequate use of insulin, or extrapolated to other inpatient or ambulatory scenarios beyond diabetes care.
Table 1.
Algorithmic Design to Develop an Automated Clinical Decision Support (CDS) Tool for Management of Hyperglycemia in the Hospital.
| Key steps to CDS design | Identify a gap in care needed to be addressed | Define the target population | Outline EHR data elements | Codify rules in software | Deliver real time recommendations | Delineate and measure outcomes |
|---|---|---|---|---|---|---|
| Outlining key steps to address a clinical gap | Define the problem that can be addressed by streamlining the interaction between clinician and EHR | Define the population and how it is identified through the EHR | Identify discrete EHR data elements (that can be searched automatically) to address the clinical issue in question | Develop and program decision rules that use discrete data points to query patients experiencing the problem to be addressed, and to whom can be applied insulin adjustment recommendations | Present messages to providers at the point of care with a display of aggregated data and with predetermined recommendations that are congruent with practice recommendations or clinical guidelines from professional societies | Use the data gathering and decision system to track discrete data points to monitor processes and outcomes |
| Addressing our specific case scenario applying the steps above | Inadequate glycemic control or management (eg, usage of sliding scale insulin as the sole management strategy, episodes of hyperglycemia requiring insulin adjustment, etc) in hospitalized patients | Adult patients with elevated blood glucose levels (with or without diabetes) within all hospital locations | Capillary blood glucose measurements, type of insulin order, dietary status | Patients in whom insulin dose adjustment is considered appropriate based on patterns or severity of abnormal glucose, eg, two consecutive glucose readings >180 mg/dl at least 3 hours apart | CDS offers real-time alert messages to providers through the EHR that are patient-centered, and in the context of the care; messages appear when clinicians are working in the charts of patients and contain concise recommendations for glucose management | Rates of hyperglycemia or hypoglycemia, use of hospital resources (ie, length of hospital stay), practice performance (ie, insulin adjustments) can be monitored to assess the overall impact of the CDS tool |
This algorithmic design does not supplant clinical intuition or routine assessment of clinical status. It does not account for nutrition changes and changes in glucose altering medications, or judgement related to insulin safety. This design can eliminate redundant data results, aggregate data for ease of interpretation, assist in identifying patterns that require action, and thus aid providers in focusing on the important cognitive exercise of decision making.
A limitation of this method includes the need to leverage technology. An automated program removes the diabetes expert from the process of individual chart review and is restricted to a virtual analysis of glucose control and insulin use. Data and management recommendations presented to the caring providers require exercising judgement and aligning recommendations in context as messages are received. Another potential limitation includes alert fatigue, which if conflicting with other priorities may result in dismissal of recommendations.
Conclusions
The need to increase value in health care drives hospitals to find innovative and efficient ways to care for patients. To attain these goals, resources in the systems of practice are much needed to support, inform, and engage health professionals to consistently recognize and act upon opportunities for improvement that can drive better outcomes. Clinical decision making collides with many barriers in practice such as information overload, dispersed medical records data, complexity of clinical practice, and gaps in practice performance which can compromise quality and safety of patient care. As systems of practice continue to adopt meaningful use of EHRs, it is necessary to recognize that glucose and insulin data displays and dispersion are common yet underestimated barriers to diabetes care in the hospital. This notion expands on an already existing myriad of barriers to diabetes care in the hospital.
Our conceptual work proposes that clinical decision support systems integrated in EHRs, informed by intelligence algorithms and offered in real time at the point of care can close an important loop to optimize diabetes care in the hospital. This approach can be an effective strategy to overcome inadequacies in hospital glycemic management resulting from dispersed glucose and insulin data. This method aims to reduce the burden of “assembling” dispersed data, avoid overlooking abnormal glucose patterns, and link support messages to clinical recommendations. Aligned with the stated need to conduct rigorously designed studies to evaluate system-level interventions including use of clinical decision aids for diabetes,33 we present a concept that can facilitate operationalizing the implementation and the study of an EHR support tool for diabetes care in the hospital. Testing of our program is undergoing, and we advocate that well-designed, prospective analyses be undertaken to evaluate the impact of initiatives using EHRs support tools. Important domains to adequately assess include practice behaviors, clinical workflows, alert fatigue, glycemic control, and clinical and economical outcomes. We call to diabetes societies to support the development of criteria applicable to prototype algorithms that can be operationalized across EHR systems to promote better care across organizations. We use diabetes as an example for this conceptual work. However, the notion of intelligence algorithms can be extrapolated to other clinical scenarios in hospital practice and to various medical disciplines, not only in inpatient but also in ambulatory settings. For instance, a similar approach can facilitate care of complex health conditions such as heart failure, sepsis, and HIV/AIDS, among other conditions that may require decision making tactics that consider multiple, often dispersed, data points.
Footnotes
Abbreviations: ARRA, American Recovery and Reinvestment Act; CDS, clinical decision support; CMS, Centers for Medicare & Medicaid Services; EHR, electronic health record; HITECH, Health Information Technology for Economic and Clinical Health.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: APL and this work are supported by a career development award (K23DK107914-01) from the National Institute of Diabetes Digestive and Kidney Disease and by the Eberly Medical Research Innovation Fund.
ORCID iD: Ariana R. Pichardo-Lowden  https://orcid.org/0000-0003-4504-4376
https://orcid.org/0000-0003-4504-4376
References
- 1. Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307:1513-1516. [DOI] [PubMed] [Google Scholar]
- 2. Cook CB, Jameson KA, Hartsell ZC, et al. Beliefs about hospital diabetes and perceived barriers to glucose management among inpatient midlevel practitioners. Diabetes Educ. 2008;34:75-83. [DOI] [PubMed] [Google Scholar]
- 3. Cook CB, McNaughton DA, Braddy CM, et al. Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians. Endocr Pract. 2007;13:117-124. [DOI] [PubMed] [Google Scholar]
- 4. Pichardo-Lowden A, Kong L, Haidet P. Knowledge, attitudes, and decision making in hospital glycemic management: are faculty up to speed? Endocr Pract. 2015;21:307-322. [DOI] [PubMed] [Google Scholar]
- 5. Mohan D, Farris C, Fischhoff B, et al. Efficacy of educational video game versus traditional educational apps at improving physician decision making in trauma triage: randomized controlled trial. BMJ. 2017;359:j5416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Costantini TW, Acosta JA, Hoyt DB, Ramamoorthy S. Surgical resident and attending physician attitudes toward glucose control in the surgical patient. Am Surg. 2008;74:993-996. [PubMed] [Google Scholar]
- 7. Trepp R, Wille T, Wieland T, Reinhart WH. Diabetes-related knowledge among medical and nursing house staff. Swiss Med Wkly. 2010;140:370-375. [DOI] [PubMed] [Google Scholar]
- 8. Moghissi ES, Korytkowski MT, DiNardo M, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care. 2009;32:1119-1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Umpierrez GE, Hellman R, Korytkowski MT, et al. Management of hyperglycemia in hospitalized patients in non-critical care setting: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2012;97:16-38. [DOI] [PubMed] [Google Scholar]
- 10. Cook CB, Castro JC, Schmidt RE, et al. Diabetes care in hospitalized noncritically ill patients: more evidence for clinical inertia and negative therapeutic momentum. J Hosp Med. 2007;2:203-211. [DOI] [PubMed] [Google Scholar]
- 11. Baldwin D, Villanueva G, McNutt R, Bhatnagar S. Eliminating inpatient sliding-scale insulin: a reeducation project with medical house staff. Diabetes Care. 2005;28:1008-1011. [DOI] [PubMed] [Google Scholar]
- 12. Umpierrez GE, Smiley D, Jacobs S, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery). Diabetes Care. 2011;34:256-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Umpierrez GE, Smiley D, Zisman A, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial). Diabetes Care. 2007;30:2181-2186. [DOI] [PubMed] [Google Scholar]
- 14. Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87:978-982. [DOI] [PubMed] [Google Scholar]
- 15. Norhammar A, Tenerz A, Nilsson G, et al. Glucose metabolism in patients with acute myocardial infarction and no previous diagnosis of diabetes mellitus: a prospective study. Lancet. 2002;359:2140-2144. [DOI] [PubMed] [Google Scholar]
- 16. Hersh W, Ehrenfeld JM. Clinical informatics. In: Skochelak SE, Hawkins RE, Lawson LE, Starr SR, Borkan JM, Gonzalo JD, eds. Health Systems Science. New York, NY: Elsevier; 2017:105-116. [Google Scholar]
- 17. Anonymous. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 18. Dick RS, Steen EB, Detmer DE. The Computer-Based Patient Record: An Essential Technology for Health Care. Revised ed. Washington, DC: National Academies Press; 1997. [PubMed] [Google Scholar]
- 19. Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 20. Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144:742-752. [DOI] [PubMed] [Google Scholar]
- 21. HealthIT.Gov. Merit-based incentive payment system. Available at: https://www.healthit.gov/topic/federal-incentive-programs/MACRA/merit-based-incentive-payment-system. Accessed July 1, 2018.
- 22. Bowen ME, Rumana U, Killgore EA, Gong Y. A user-centered glucose-insulin data display for the inpatient setting. Stud Health Technol Inform. 2017;245:684-688. [PMC free article] [PubMed] [Google Scholar]
- 23. Eom S, Kim E. A survey of decision support system applications (1995-2001). Eur J Oper Res. 2006;57:1264-1278. [Google Scholar]
- 24. Amor AJ, Rios PA, Graupera I, et al. Management of inpatient glucose in non-critical care setting: impact of a proactive intervention based on a point-of-care of system with remote viewing of capillary blood glucose. Med Clin. 2014;142:387-392. [DOI] [PubMed] [Google Scholar]
- 25. Mendez CE, Ata A, Rourke JM, Stain SC, Umpierrez G. Daily inpatient glycemic survey (dings): a process to remotely identify and assist in the management of hospitalized patients with diabetes and hyperglycemia. Endocr Prac. 2015;21:927-935. [DOI] [PubMed] [Google Scholar]
- 26. Rushakoff RJ, Sullivan MM, MacMaster HW, et al. Association between a virtual glucose management service and glycemic control in hospitalized adult patients: an observational study. Ann Intern Med. 2017;166:621-627. [DOI] [PubMed] [Google Scholar]
- 27. Rushakoff RJ, Rushakoff JA, Kornberg Z, MacMaster HW, Shah AD. Remote monitoring and consultation of inpatient populations with diabetes. Curr Diab Rep. 2017;17:70. [DOI] [PubMed] [Google Scholar]
- 28. Pichardo-Lowden AR, Mouery V, Ward M, Bolton M, Haidet PM. Optimizing inpatient diabetes care using a comprehensive-real time electronic medical records clinical decision support tool [abstract]. In: Proceedings of the 15th Annual Workshop of the Network of Minority Research Investigators Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases; 2017. [Google Scholar]
- 29. Osheroff JA, Teich JM, Middleton B, Steen EB, Wright A, Detmer DE. A roadmap for national action on clinical decision support. J Am Med Inform Assoc. 2007;14:141-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bright TJ, Wong A, Dhurjati R, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;157:29-43. [DOI] [PubMed] [Google Scholar]
- 31. Bennett CC, Doub TW, Selove R. EHRs connect research and practice: where predictive modeling, artificial intelligence, and clinical decision support intersect. Health Policy Technol. 2012;1:104-114. [Google Scholar]
- 32. Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363:501-504. [DOI] [PubMed] [Google Scholar]
- 33. Draznin B, Gilden J, Golden SH, et al. Pathways to quality inpatient management of hyperglycemia and diabetes: a call to action. Diabetes Care. 2013;36:1807-1814. [DOI] [PMC free article] [PubMed] [Google Scholar]