Abstract
One-to-one instruction is a critical component of evidence-based instruction for students with autism spectrum disorder, but is not used as often as recommended. Student characteristics may affect teachers’ decisions to select a treatment and/or implement it. This study examined the associations between students’ clinical and demographic characteristics and teachers’ reported use of discrete trial training (DTT) and pivotal response training (PRT). Children’s higher sensory symptoms, lower social approach, lower verbal skills and higher self-regulation difficulties were associated with more frequent 1:1 DTT and PRT. Results suggest that teachers give more frequent 1:1 instruction to children with more observable impairments, do not match children to type of 1:1 intervention, and may inadvertently neglect other students for whom individualized intervention may still be beneficial.
Keywords: 1:1 instruction, child characteristics, personalized medicine, teacher decisions
Evidence-based treatments for children with autism spectrum disorder (ASD) include behavioral interventions that teach communication, cognitive, social and adaptive skills. There has been a steady rise in the number of children receiving ASD intervention services through schools (U.S. Department of Education, 2017), but the type and intensity of treatment vary greatly (White, Scahill, Klin, Koenig, & Volkmar, 2007). There is little research on factors that predict the type and intensity of school-based treatment children with ASD receive. Such factors may include different school resources, such as staffing, or teacher characteristics, including teacher preferences, training, pedagogy and skill (Stahmer, Collings, & Palinkas, 2005). Some studies have found associations between these characteristics and use of behavioral interventions for children with ASD (Hogan, Knez, & Kahng, 2015), but others have found no association (Segall & Campbell, 2012; Morrier, Hess, & Heflin, 2011; Mandell et al., 2013; Stahmer et al., 2015).
Variability in treatment delivery also may be driven by child characteristics (Stahmer et al., 2005), such as their language level, severity of ASD symptoms, or regulatory difficulties, all of which may consciously or unconsciously drive teachers’ decisions about who is suited to one-toone (1:1) instruction or a particular type of treatment. Findings of the authors’ have identified that child characteristics account for about half of the variance in the frequency with which children received 1:1 intervention in school (Lushin et al., submitted), but that study did not investigate whether specific child characteristics are associated with teachers’ decisions to provide 1:1 intervention.
Related research has examined whether child characteristics predict outcomes as a result of different types of treatment. Two evidence-based treatment approaches for children with ASD include discrete trial training (DTT; Lovaas, 2003; Lovaas & Buch, 1997) and pivotal response training (PRT; Schreibman et al., 2015). Both DTT and PRT are based on principles of applied behavior analysis (ABA; e.g., operant conditioning, systematic reinforcement; Ringdahl, Kopelman, & Falcomata, 2009; Smith & Iadarola, 2015) and are administered by an adult working 1:1 with a child. A key difference between these two approaches is that DTT is adult-directed and incorporates external reinforcement (e.g., token reward for play initiation), while PRT is child-directed and incorporates naturalistic reinforcement (e.g., smiles/engagement for play initiation; Koegel, Koegel, Harrower, & Carter, 1999; Koegel, Koegel, Shoshan, & McNerney, 1999). Both DTT (Anderson, Avery, DiPietro, Edwards, & Christian, 1987; Lovaas, 1987; McEachin, Smith, & Lovaas, 1993) and PRT (Koegel, Koegel, Shoshan, et al., 1999; Nefdt, Koegel, Singer, & Gerber, 2010) are effective practices for children with ASD. Research has indicated that DTT is most effective when implemented in combination with naturalistic interventions to facilitate generalization of skill development across settings and support the development of spontaneous behaviors, such as play initiation (Duffy & Healy, 2011; National Research Council, 2001; Schreibman et al., 2015; Smith, 2001).
Children who made the greatest gains through DTT demonstrated greater social engagement (social approach, joint attention, and imitation), were younger and had a higher IQ (Smith, Klorman, & Mruzek, 2015). Children who made the greatest gains through PRT were younger (Baker-Ericzén, Stahmer, & Burns, 2007) and had higher social approach, and had higher expressive language ability (not overall IQ). They also had higher positive affect and appropriate toy contact, and lower stereotyped/repetitive vocalizations (Fossum, Williams, Garon, Bryson, & Smith, 2018). Research by Schreibman and colleagues suggests that the profile of children who made greater gains with PRT was specific to PRT, and did not generalize to DTT (Schreibman, Stahmer, Barlett, & Dufek, 2009; Sherer & Schreibman, 2005), indicating utility in identifying unique responder profiles for different treatments. Among children with ASD who received a comprehensive program that incorporates DTT and PRT, fewer self-regulation difficulties over the course of the academic year were associated with higher cognitive skill gains (Nuske et al., 2017). This body of work has therefore identified some overlapping and some unique child characteristics of higher responders to DTT and PRT.
Such research could be used to inform a personalized medicine approach (i.e. individual tailoring of treatment) for children with ASD, by selecting interventions for a child based on their characteristics or behavioral profile (Masi, DeMayo, Glozier, & Guastella, 2017; Ousley & Cermak, 2014). Personalized medicine approaches have been recently applied to clinical psychology, so to increase the efficacy of behavioral and cognitive treatments (Drake, Cimpean, & Torrey, 2009; Fisher, 2015; Jeon & Fava, 2015; Kasari et al., 2014; Lei, Nahum-Shani, Lynch, Oslin, & Murphy, 2012; Ng & Weisz, 2016). The premise is that by individualizing treatments (e.g. selecting one over others, or some components of an intervention over other components), treatments will be most effective. These approaches bring new methodological considerations and challenges, and necessitate research designs that allow for treatment individualization via systematized trial and error, for example, in the case of adaptive, sequential and crossover designs (for review, Lillie et al., 2011). Importantly, individualization may be most effective when completed a priori to starting treatment. This approach entails selecting treatments based on children’s behavioral profile before treatment or programming begins, so to potentially avoid spending time using treatments or components of treatments that are not suited to a particular child.
However, it is possible that teachers may be using this approach already, either from reading of the research or from their own experience, when deciding which intervention to use with which children. Indeed, teachers note that individualizing instruction based on a child’s strengths and weaknesses is important (Stahmer et al., 2005). In the only published study on this topic, teachers reported choosing DTT for students who had more significant cognitive delays, who struggled with compliance, and who did not imitate or attend in less structured settings (Stahmer et al., 2005). No study to date has empirically tested whether frequency of treatment delivery and teacher selection of treatment approach relate to their students’ characteristics.
The present study is the first to quantitatively examine the associations between child characteristics and teacher selection and frequency of use of PRT and/or DTT. Based on the prior qualitative study in this area (Stahmer et al., 2005), researchers hypothesized that teachers would be more likely to use DTT with children who had more severe ASD symptoms, lower cognitive skills, and higher regulatory difficulties. Based on prior research regarding PRT outcomes (Schreibman et al., 2009; Sherer & Schreibman, 2005), researchers hypothesized that children with higher social and semantic pragmatic skills and higher verbal ability, would be more likely to receive PRT. Researchers also explored associations with sex and race, and described the variability in use of DTT and PRT across children and classrooms.
Method
Setting
Data were collected from teachers and students with ASD in the School District of Philadelphia, the eighth largest district in the United States. Most students are ethnic minorities (69%), with 75% living below the federal poverty line. The district has collaborated with the research team since 2008 (Mandell et al., 2013), to improve access to evidence-based interventions for students with ASD. The research team contracts with the district to train and coach teachers of autism support classrooms in these practices. The term “autism support classroom” is used within the district to describe classrooms that include only children with an educational classification of ASD. These classrooms are designed to provide specialized supports for students with ASD within daily routines throughout the day, including the use of structured routines, visual supports, positive behaviour management, and individualized or small-group instruction. DTT and PRT are provided within individualized and small-group instructional rotations. The present study used data from a randomized trial of a computerized intervention, TeachTown:Basics (Pellecchia et al., 2016). University and school district institutional review board approvals were obtained prior to initiating study procedures.
Participants
Teachers.
Participating teachers were kindergarten-through-second-grade autism support teachers (n = 80) who had enrolled in a randomized, controlled trial conducted in partnership with the School District of Philadelphia (Pellecchia et al. XXXX). All teachers were state certified to teach special education in Pennsylvania; 81% had a graduate degree, 15% had an undergraduate degree, and 4% did not report their education. Teachers were excluded from the analysis if less than 2 students in their classroom consented to participate in the study (n = 11), making the final sample of teachers = 69.
Children with ASD.
A total of 228 children with ASD participated in the study. All children were between the ages of 5 and 9 years and were enrolled in a kindergarten-through-second-grade autism support classroom for at least half the day, and had an educational classification of ASD. Full child characteristics are provided in Table 1.
Table 1.
Child Characteristics
| M/# | SD/% | Range | ||
|---|---|---|---|---|
| Child Demographics | ||||
| Age (Years) | 6.11 | 0.91 | 5–9 | |
| Sex: | Male | 180 | 78.9 | |
| Female | 37 | 16.2 | ||
| Not provided | 11 | 4.8 | ||
| Race: | Black/African American | 106 | 46.5 | |
| White | 55 | 24.1 | ||
| American Indian or Alaska Native | 1 | 0.4 | ||
| Asian | 16 | 7.0 | ||
| Middle-Eastern | 3 | 1.3 | ||
| Other | 37 | 16.2 | ||
| Not provided | 10 | 4.3 | ||
| Child Clinical Profile | ||||
| PDDBIa Sensory Symptoms | 51.75 | 14.75 | 35–90 | |
| PDDBIa Ritualistic / Resistance to Change | 51.52 | 11.70 | 37–85 | |
| PDDBIa Social Pragmatic Problems | 54.05 | 11.81 | 34–80 | |
| PDDBIa Semantic Pragmatic Problems | 54.00 | 11.04 | 36–78 | |
| PDDBIa Social Approach | 53.79 | 12.08 | 24–75 | |
| DASb Verbal Subscale | 63.48 | 22.32 | 30–115 | |
| DASb Non-Verbal Composite (SNC) | 68.62 | 20.70 | 30–102 | |
| BICSc Self-Regulation Difficulties | 1.96 | 0.73 | 1–3.83 | |
| Teacher Characteristics | ||||
| Sex: | Male | 2 | 2.5 | |
| Female | 77 | 96.2 | ||
| Not provided | 1 | 1.3 | ||
| Race: | Black/African American | 8 | 10.0 | |
| White | 68 | 85.0 | ||
| American Indian or Alaska Native | 1 | 1.25 | ||
| Asian | 1 | 1.25 | ||
| Other | 1 | 1.25 | ||
| Not provided | 1 | 1.25 | ||
| Classroom Characteristics | ||||
| Number children | 7.42 | 1.22 | 2–10 | |
| Number of support staff | 3.77 | 1.18 | 2–7 | |
Pervasive Developmental Disorder Behavior Inventory,
Differential Ability Scales, 2nd Edition,
Behavioral Interference Coding Scheme
Teacher Training
All teachers received training and consultation in DTT, PRT, positive reinforcement for classroom management, and use of visual schedules. Teachers and classroom staff received intensive training and support throughout the school year from master’s level consultants with expertise in ABA. Training included three days of intensive workshops at the start of the school year, hands-on work in the classrooms with teachers to set up classrooms and plan student lessons at the start of the school year, quarterly half-day workshops during the school year, and ongoing in-vivo coaching for two to three hours per month throughout the school year.
Discrete Trial Training.
DTT comprises intensive, 1:1 teaching sessions using mass trials, or the repeated practice of the same response for several successive teaching episodes. Use of reinforcers in DTT are functionally unrelated to the response (e.g. a candy for correctly identifying a car). DTT instruction involves breaking down complex skills into small component parts, and teaching each component part individually.
Pivotal Response Training.
PRT comprises a 1:1 teaching technique that involves loosely structured but targeted sessions. PRT sessions rely on capturing and contriving a child’s motivation to guide instruction. Teaching sessions are initiated and paced by the child, take place in a variety of naturalistic and play-based settings, and use items and activities that are highly preferred by the child. During PRT, the child chooses the instructional object or activity, and the reinforcer is related to the response (e.g. playing with a toy car for correctly identifying a car).
Measures
Autism symptoms.
Student ASD symptoms were measured using the teacher version of the Pervasive Developmental Disorders Behavior Inventory (PDDBI; Cohen & Sudhalter, 2005). This questionnaire is designed to measure both adaptive skills and maladaptive behaviors relevant to ASD. It provides a quantitative assessment of the severity of a child’s ASD symptomology, as compared to other children with ASD. Researchers used standard scores from the five subscales encompassed under ASD symptoms: sensory symptoms, ritualistic/resistance to change, social pragmatic problems, semantic pragmatic problems, and social approach abilities. For each scale except for social approach, higher scores indicate more problems (higher scores on social approach indicate better abilities). Teachers completed a Teacher PDDBI form for each consented student in their classroom a minimum of one month after the beginning of the school year, therefore they had adequate time to become familiar with the child’s ASD symptom presentation prior to filling out this measure.
Cognitive and language ability.
The Early Years Battery of the Differential Abilities Scales – Second Edition (DAS-II) was used as a clinical assessment of a child’s cognitive abilities (Beran, 2007; Elliott, 1990; Marshall, McGoey, & Moschos, 2011), administered by researchers at the beginning of the school year. The present study used the DAS-II Verbal Ability subscale and the Special Non-Verbal Composite score. Other studies have similarly chosen to use the DAS-II as the outcome measure in studies of children with ASD (Anderson et al., 2007; Thurm, Lord, Lee, & Newschaffer, 2007).
Self-regulation difficulties.
Self-regulation difficulties were measured using the Self-Regulation subscale of the Behavioral Interference Coding Scheme (BICS; Freeman et al., submitted). This scale measures behavioral manifestations of self-regulation difficulties that are observable during standardized testing. In the present study, researchers completed this scale based on the children’s behavior during the DAS-II administration. Self-regulation behaviors in the scale are based on those measured by similar parent-report scales (e.g., the Behavior Regulation scale of the Behavior Rating Inventory of Executive Function; Gioia, Isquith, Retzlaff, & Espy, 2002), and includes ten items: 1) easily distractible, 2) impulsive, 3) noncompliant with task directions, 4) needs prompting and reminders for compliance, 5) difficulties with transitions, 6) low frustration tolerance, 7) rigid/inflexible, 8) easily fatigued, 9) gives up easily and 10) aggressive. Items were scored as 1 = never, 2 = sometimes, 3 = often, and 4 = constant. Study analyses used the mean of the ten items, with higher scores indicating more frequent self-regulation difficulties. Internal consistency (Cronbach’s α) was high (α = .87).
Teacher reported frequency of use and selection of 1:1 instruction per child.
Teachers’ reported frequency of use of 1:1 instruction strategies (PRT and DTT) was measured using self-report. Each month, teachers were asked how often they implemented 1:1 DTT and PRT with each student in their classroom during the past week. Teachers reported on the previous week rather than each week in the whole month to avoid recall biases or reporting errors. Frequencies were reported using a 5-point likert scale (0 = less than once per week; 1 = once per week; 2 = two to four times per week; 3 = once per day; 4 = twice per day). Researchers averaged frequency data across months February to May as these were months after all DTT and PRT training was complete.
Teacher and classroom level covariates.
Teachers’ experience with children with ASD and their baseline accuracy in PRT and DTT may affect their reported use of these interventions. Researchers therefore assessed teachers’ ASD experience, through self-report via the teacher’s demographic questionnaire (did/did not have experiencing teaching children with ASD). Baseline accuracy in PRT and DTT was measured through a 1-hour period of live classroom-based behavioral coding by researchers during the first month of school whereby researchers rated teachers on key aspects of DTT and PRT implementation (see Pellecchia et al., submitted for details). Accuracy (fidelity) was measured once a month throughout the course of the academic year, alongside frequency of implementation (as per above). To explore the impact of in-class resources, researchers also measured mean number of students and support staff in the classroom, averaged across months February to May (months after all DTT and PRT training was complete). Finally, researchers assessed whether teachers received TeachTown as part of the randomized trial.
Data Analysis
Descriptive statistics were performed in SPSS Version 25 and inferential statistics were performed using Mplus Version 8. Researchers first computed frequencies of reported students’ receipt of DTT and PRT, to determine (a) which classroom had no implementation of DTT/PRT, (b) which had the same frequency of DTT/PRT implementation across all children (within 0.25 scale points; see Teacher use of 1:1 instruction), and (c) which teachers varied in their reported treatment use among students in their classroom. Second, to examine the overall contribution of child characteristics to reported children’s receipt of treatment, researchers calculated intra-class correlations (ICCs) for use of any 1:1 instruction (sum of DTT and PRT), and DTT, and PRT, which reflect the ratio of within-classroom variance (child characteristics) to overall variance (the sum of child and classroom-level variance) (Castro, 2002).
Third, continuous variables were checked for normality and deemed appropriate for parametric statistics. Missing data were addressed by the full information maximum likelihood (FIML) protocol as implemented in Mplus. Correlations between continuous predictor variables were examined to check for collinearity; correlations were within recommended guidelines (Tabachnick & Fidell, 2007), so all variables were included. Three sets of multiple (ordinary least squares) regression analyses were conducted to examine which child characteristics were associated with reported 1:1 instruction use, for (a) any 1:1 instruction (sum of DTT and PRT), (b) DTT, and (c) PRT. Regression models were used to examine the association between each child characteristic (PDDBI Sensory Problems, PDDBI Rituals/Resistance to Change Problems, PDDBI Social Pragmatic, PDDBI Semantic Pragmatic Problems, PDDBI Social Approach Abilities, DAS-II Verbal Ability, DAS-II Non-Verbal Ability (Special Non-Verbal Composite), BISC Self-Regulation Problems, child age, sex, and race), with each model controlling for covariates that met criteria for inclusion. Following recommendations of Hosmer and Lemeshow (2000), the criteria set were that bivariate associations of the covariates (listed above) with the outcome variables would be significant at p < .2 in each of the regression models. Based on this criterion, teacher baseline accuracy to the corresponding intervention model(s) and teacher’s reported experience in ASD intervention was entered for all models, and additionally, for the regressions on reported receipt of DTT as the dependent variable, mean number of support staff in the classroom was also entered, and for regressions on reported receipt of PRT, RCT random assignment was also entered. Class size was unrelated to reported children’s receipt of treatment (p > .67), and was therefore not included as a covariate in any of the analyses. Analyses were nested in classrooms, to statistically account for the multilevel data structure. Multiple regression analyses were pursued via “Type: Complex” estimator with Cluster function, as implemented in Mplus. Classroom-based groups were specified as clusters.
Results
From February to May, teachers’ average scores on the scale of EBP use intensity were the following: for DTT, an average reported intensity score was 0.76 (between less than 1 and 1 time per week, for each student; SD = 0.80), for PRT, an average reported intensity score was 0.81 (between less than 1 and 1 times per week, for each student; SD = 0.96), and for any 1:1 strategy (sum of DTT and PRT), an average reported intensity score was 1.55 (between 1 and 4 times per week, for each student; SD = 1.70).
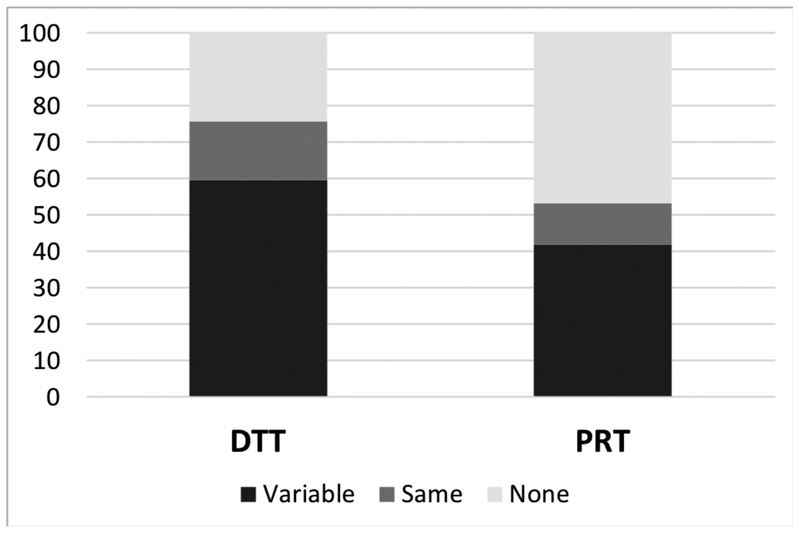
The proportion of teachers who gave no DTT/PRT implementation, the same DTT/PRT implementation across students within their classrooms and variable DTT/PRT implementation across students (e.g. some children with one day reported per week and some children reportedly receiving more frequent treatment) are shown in Figure 1.
Figure 1.
Percentage of classrooms with variable, same or no implementation of DTT and PRT within classrooms.
About half the variance in reported children’s receipt of treatment was accounted for at the child level rather than at the teacher and classroom level: DTT = 0.53, PRT = 0.51 and sum of DTT and PRT = 0.51. Table 2 presents results of regression analyses estimating associations between child characteristics and DTT, PRT or any 1:1 instruction. For both DTT and PRT (separately and combined), children’s higher sensory symptoms, lower social approach, lower verbal skills and higher self-regulation difficulties were associated with more frequent reported 1:1 instruction, with one standard deviation increase in any of the significant child characteristics associated with around ~0.2 standard deviation change in reported frequency of DTT or PRT receipt. Children’s age, sex and race did not emerge as significant predictors of reported childrens’ DTT or PRT receipt. In the separate adjusted models, significant child factors each explained 8–15% of the variance in reported receipt of treatment.
Table 2.
Associations between Child Characteristics and Receipt of 1:1 Instruction
| DTTd | PRTe | Any 1:1 Instruction (sum of DTT and PRT) | ||||
|---|---|---|---|---|---|---|
| R2 | β | R2 | β | R2 | β | |
| Child Clinical Profile | ||||||
| PDDBIa Sensory Symptoms | 0.13* | 0.20* | 0.13* | 0.25*** | 0.15** | 0.28** |
| PDDBIa Ritualistic / Resistance to Change | 0.10* | 0.12 | 0.08# | 0.10 | 0.10* | 0.15# |
| PDDBIa Social Pragmatic Problems | 0.10* | 0.11 | 0.08# | 0.06 | 0.09# | 0.09 |
| PDDBIa Semantic Pragmatic Problems | 0.09* | 0.05 | 0.07 | 0.01 | 0.08# | 0.02 |
| PDDBIa Social Approach | 0.12* | −0.17* | 0.11* | −0.18* | 0.11* | −0.17* |
| DASb Verbal Subscale | 0.14** | −0.23** | 0.13* | −0.24** | 0.14** | −0.24** |
| DASb Non-Verbal Composite (SNC) | 0.09* | 0.04 | 0.08 | 0.03 | 0.08# | 0.03 |
| BICSc Self-Regulation Difficulties | 0.11* | 0.17# | 0.10* | 0.18* | 0.11# | 0.19* |
| Child Demographics | ||||||
| Age (Grade) | 0.09* | 0.05 | 0.08 | 0.03 | 0.08# | 0.01 |
| Sex | 0.09* | −0.02 | 0.08 | −0.05 | 0.08 | −0.03 |
| Race | 0.09* | 0.08 | 0.08 | 0.03 | 0.08# | 0.06 |
Note: All models controlling for significant covariates, see Data Analysis.
Pervasive Developmental Disorders Behavior Inventory,
Differential Ability Scales, 2nd Edition,
Behavioral Interference Coding Scheme,
Discrete Trial Training,
Pivotal Response Training,
p < .001,
p < .01,
p < 0.05,
p <.1
Discussion
Researchers examined the associations of teachers’ reported frequency of use of DTT and/or PRT with children with ASD in their classrooms and these children’s characteristics. The results show that teachers reportedly provided more 1:1 instruction in general to children who have more sensory and self-regulation difficulties, lower verbal skills and less social approach. Findings suggest that teachers give more treatment to children with more obvious impairments. This is encouraging as it suggests that teachers are tapping into some key observable difficulties of particular children and reportedly allocating 1:1 instruction resources from their classrooms accordingly (Linstead et al., 2017). Previous research has shown that children with more significant impairments make the fewest gains in any treatment (Fossum et al., 2018; Smith et al., 2015; Thurm et al., 2007). Therefore, teachers with more severely impaired students face significant challenges in fostering positive outcomes for their students. The results show that teachers are attempting to address these students’ needs by providing them with more individualized intervention.
In the context of limited classroom resources (e.g., time, space, availability of teacher aids), teachers are using 1:1 interventions to treat children who demonstrate the most obvious need. While promising in one sense, it also means that other children may be inadvertently neglected, though they may still benefit from 1:1 treatment. All children in autism support classrooms have an educational classification of ASD, meaning that their school teams have identified significant support needs consistent with ASD. However, those who are easier to manage or who have, relatively speaking, more skills are not receiving potentially beneficial treatment as other children with ASD, though they may have significant developmental delays relative to their typically developing peers. Given that for many children the bulk of their services are received through school, this may mean that many children with ASD are not receiving the 1:1 instruction that they need.
The findings also suggest teachers are not considering students’ age when implementing either PRT or DTT. In the context of findings of higher positive outcomes in PRT or DTT for younger children with ASD (Baker-Ericzén et al., 2007; Smith et al., 2015), this suggests again that teachers are making decisions preferentially based on perceived students’ support needs.
Reportedly, teachers did not differentially use DTT or PRT based on child characteristics, despite the theoretical notion that different profiles of children may be better suited to one over the other (Vivanti, 2017). Evidence suggests that matching children with ASD to certain treatment styles based on their pre-treatment behavioral profile may support positive outcomes (Schreibman et al., 2009; Sherer & Schreibman, 2005). However, researchers found the same student characteristics predicted teachers’ use of DTT and PRT. Given that the ASD field, as well as the mental health field in general, is moving towards a personalized medicine approach to treatment (i.e. to individualise treatments decision based on individual behavioral profiles; Drake et al., 2009; Jeon & Fava, 2015; Ng & Weisz, 2016; Stahmer, Schreibman, & Cunningham, 2011), these results provide important insights into the current state of affairs regarding teachers’ decisions about their students’ educational programming. The results show that teachers are not reportedly using one treatment type more frequently over the other with children with different characteristics. The research on pre-treatment behavioral profiles and optimal treatment fit is promising, but has only recently begun, therefore further work is needed before teacher consultation models around child-treatment fit can be developed.
Limitations and Future Directions
Several limitations of the current study should be noted. First, teacher’s own report of 1:1 instruction use is subject to the social desirability bias, in that teachers may have reported higher frequencies than were actually implemented. However, this may not differentially apply to children of certain characteristics. Nevertheless, observation methods would have strengthened the measurement of intervention implementation and is recommended for future research. Second, while ASD symptoms were measured via teacher report, cognitive and language abilities and self-regulation difficulties were measured by study staff. Therefore the latter may not have necessarily mapped onto teacher’s own perspectives of children’s cognitive and language abilities and self-regulation difficulties and decisions regarding the frequency with which teachers should use 1:1 across different children in their classroom. Third, the extent to which teachers’ decisions to use treatments for more severely impacted children were well-informed or considerate of individual student needs was not specifically examined in this study. Future work could identify factors such as the extent to which cognitive biases, intentions and adherence to coaches’ recommendations affect teachers’ use of 1:1 intervention.
Conclusions
Our findings suggest that teachers make judgements about which students with ASD should receive more frequent 1:1 instruction based on perceived need or specific child characteristics. More obviously impaired students reportedly received more DTT and PRT. The findings beg the questions of whether teachers are accurate in their decisions regarding who benefits from 1:1 instruction, and whether children should be matched to specific types of 1:1 instruction based on their clinical characteristics. In the meantime, to the extent that experts think that less obviously impaired students would benefit from 1:1 instruction, those working with teachers should address practical, attitudinal and structural barriers to providing 1:1 instruction to a larger proportion of students.
Acknowledgements
The research team would like to thank all of the children, parents and teachers who graciously gave their time to the study and the team of dedicated Clinical Research Coordinators who contributed to the success of the school intervention trial, Christine Spaulding, Rachel Ouellette and Max Seidman, as well as all the wonderful student interns who worked tirelessly on the project. We thank also the funder of the school intervention trial, the National Institute of Mental Health (NIMH), without which the research would not have been possible.
Funding: This study was funded by two Grants from the NIMH, Institution No. 10048329: RCT of TeachTown in Autism Support Classrooms: Innovation and Exnovation, 5R01MH106175 (PI: Mandell) and an Institutional Research Training Grant, T32MH109433 (PI: Mandell).
Footnotes
Disclosure of Potential Conflicts of Interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- Anderson DK, Lord C, Risi S, Dilavore PS, Shulman C, Thurm A, … Pickles A (2007). Patterns of Growth in Verbal Abilities Among Children With Autism Spectrum Disorder. Journal of Consulting and Clinical Psychology, 75(4), 594–604. 10.1037/0022-006X.75.4.594 [DOI] [PubMed] [Google Scholar]
- Anderson SR, Avery DL, DiPietro EK, Edwards GL, & Christian WP (1987). INTENSIVE HOME-BASED EARLY INTERVENTION WITH AUTISTIC CHILDREN. Education and Treatment of Children, 10(4), 352–366. [Google Scholar]
- Baker-Ericzén MJ, Stahmer AC, & Burns A (2007). Child demographics associated with outcomes in a community-based pivotal response training program. Journal of Positive Behavior Interventions, 9(1), 52–60. [Google Scholar]
- Beran TN (2007). Elliott, C. D. (2007). “Differential Ability Scales” (2nd Ed.). San Antonio, TX: Harcourt Assessment. Canadian Journal of School Psychology, 22(1), 128–132. 10.1177/0829573507302967 [DOI] [Google Scholar]
- Castro SL (2002). Data analytic methods for the analysis of multilevel questions: A comparison of intraclass correlation coefficients, rwg (j), hierarchical linear modeling, within-and between-analysis, and random group resampling. The Leadership Quarterly, 13(1), 69–93. [Google Scholar]
- Cohen IL, & Sudhalter V (2005). PDD behavior inventory (PDDBI). Lutz, FL: Psychological Assessment Resources. [Google Scholar]
- Drake RE, Cimpean D, & Torrey WC (2009). Shared decision making in mental health: prospects for personalized medicine. Dialogues in Clinical Neuroscience, 11(4), 455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy C, & Healy O (2011). Spontaneous communication in autism spectrum disorder: A review of topographies and interventions. Research in Autism Spectrum Disorders, 5(3), 977–983. [Google Scholar]
- Elliott CD (1990). Differential Abilities Scales - Second Edition. [Google Scholar]
- Fisher AJ (2015). Toward a dynamic model of psychological assessment: Implications for personalized care. Journal of Consulting and Clinical Psychology, 83(4), 825. [DOI] [PubMed] [Google Scholar]
- Fossum K-L, Williams L, Garon N, Bryson SE, & Smith IM (2018). Pivotal response treatment for preschoolers with autism spectrum disorder: Defining a predictor profile. Autism Research, 11(1), 153–165. 10.1002/aur.1859 [DOI] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Retzlaff PD, & Espy KA (2002). Confirmatory factor analysis of the Behavior Rating Inventory of Executive Function (BRIEF) in a clinical sample. Child Neuropsychology, 8(4), 249–257. [DOI] [PubMed] [Google Scholar]
- Hogan A, Knez N, & Kahng S (2015). Evaluating the Use of Behavioral Skills Training to Improve School Staffs’ Implementation of Behavior Intervention Plans. Journal of Behavioral Education, 24(2), 242–254. 10.1007/s10864-014-9213-9 [DOI] [Google Scholar]
- Hosmer Dw., & Lemeshow S (2000). Applied logistic regression 2nd ed. Chap. 4, Model-Building Strategies. New York, John Wiley & Sons Inc. [Google Scholar]
- Jeon HJ, & Fava M (2015). Chapter Eight - Novel Study Designs for Clinical Trials in Mood Disorders In Tohen M, Bowden CL, Nierenberg AA, & Geddes JR (Eds.), Clinical Trial Design Challenges in Mood Disorders (pp. 87–104). San Diego: Academic Press; Retrieved from http://www.sciencedirect.com/science/article/pii/B9780124051706000087 [Google Scholar]
- Kasari C, Kaiser A, Goods K, Nietfeld J, Mathy P, Landa R, … Almirall D (2014). Communication Interventions for Minimally Verbal Children With Autism: Sequential Multiple Assignment Randomized Trial. Journal of the American Academy of Child and Adolescent Psychiatry, 53(6), 635–646. 10.1016/j.jaac.2014.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koegel LK, Koegel RL, Harrower JK, & Carter CM (1999). Pivotal Response Intervention I: Overview of Approach. Journal of the Association for Persons with Severe Handicaps, 24(3), 174–185. 10.2511/rpsd.24.3.174 [DOI] [Google Scholar]
- Koegel LK, Koegel RL, Shoshan Y, & McNerney E (1999). Pivotal response intervention II: Preliminary long-term outcome data. Journal of the Association for Persons with Severe Handicaps, 24(3), 186–198. [Google Scholar]
- Lei H, Nahum-Shani I, Lynch K, Oslin D, & Murphy SA (2012). A “SMART” Design for Building Individualized Treatment Sequences. Annual Review of Clinical Psychology, 8(1), 21–48. 10.1146/annurev-clinpsy-032511-143152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillie EO, Patay B, Diamant J, Issell B, Topol EJ, & Schork NJ (2011). The n-of-1 clinical trial: the ultimate strategy for individualizing medicine? Personalized Medicine, 8(2), 161–173. 10.2217/pme.11.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linstead E, Dixon DR, French R, Granpeesheh D, Adams H, German R, … Kornack J (2017). Intensity and learning outcomes in the treatment of children with autism spectrum disorder. Behavior Modification, 41(2), 229–252. [DOI] [PubMed] [Google Scholar]
- Lovaas OI (1987). Behavioral treatment and normal educational and intellectual functioning in young autistic children. J Consult Clin Psychol, 55(1), 3–9. [DOI] [PubMed] [Google Scholar]
- Lovaas OI (2003). Teaching Individuals with Developmental Delays: Basic Intervention Techniques. PRO-ED, Inc. [Google Scholar]
- Lovaas OI, & Buch G (1997). Intensive behavioral intervention with young children with autism. Prevention and Treatment of Severe Behavior Problems: Models and Methods in Developmental Disabilities. [Google Scholar]
- Mandell DS, Stahmer AC, Shin S, Xie M, Reisinger E, & Marcus SC (2013). The Role of Treatment Fidelity on Outcomes during a Randomized Field Trial of an Autism Intervention. Autism: The International Journal of Research and Practice, 17(3), 281–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall S, McGoey KE, & Moschos S (2011). Test Review: C. D. Elliott “Differential Ability Scales-Second Edition.” San Antonio, TX--Harcourt Assessment, 2007. Journal of Psychoeducational Assessment, 29(1), 89–93. 10.1177/0734282910368783 [DOI] [Google Scholar]
- Masi A, DeMayo MM, Glozier N, & Guastella AJ (2017). An Overview of Autism Spectrum Disorder, Heterogeneity and Treatment Options. Neuroscience Bulletin, 33(2), 183–193. 10.1007/s12264-017-0100-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEachin JJ, Smith T, & Lovaas OI (1993). Long-term outcome for children with autism who received early intensive behavioral treatment. American Journal of Mental Retardation: AJMR, 97(4), 359–372; discussion 373–391. [PubMed] [Google Scholar]
- Morrier MJ, Hess KL, & Heflin LJ (2011). Teacher Training for Implementation of Teaching Strategies for Students With Autism Spectrum Disorders. Teacher Education and Special Education, 34(2), 119–132. 10.1177/0888406410376660 [DOI] [Google Scholar]
- National Research Council. (2001). Educating Children with Autism. Washington, D.C.: National Academies Press; Retrieved from http://www.nap.edu/catalog/10017 [Google Scholar]
- Nefdt N, Koegel R, Singer G, & Gerber M (2010). The use of a self-directed learning program to provide introductory training in pivotal response treatment to parents of children with autism. Journal of Positive Behavior Interventions, 12(1), 23–32. [Google Scholar]
- Ng MY, & Weisz JR (2016). Annual Research Review: Building a science of personalized intervention for youth mental health. Journal of Child Psychology and Psychiatry, 57(3), 216–236. 10.1111/jcpp.12470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuske HJ, Kane C, Rump K, Pellecchia M, Maddox B, Reisinger Blanch E, & Mandell D (2017). The impact of self-regulation skills on academic outcomes in minimally-verbal school-age children with autism. International Meeting for Autism Research. [Google Scholar]
- Ousley O, & Cermak T (2014). Autism Spectrum Disorder: Defining Dimensions and Subgroups. Current Developmental Disorders Reports, 1(1), 20–28. 10.1007/s40474-013-0003-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellecchia M, Beidas RS, Marcus SC, Fishman J, Kimberly JR, Cannuscio CC, … Mandell DS (2016). Study protocol: implementation of a computer-assisted intervention for autism in schools: a hybrid type II cluster randomized effectiveness-implementation trial. Implementation Science, 11(1), 154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ringdahl JE, Kopelman T, & Falcomata TS (2009). Applied behavior analysis and its application to autism and autism related disorders. 10.1007/978-1-4419-0088-3_2 [DOI]
- Schreibman L, Dawson G, Stahmer AC, Landa R, Rogers SJ, McGee GG, … et al. (2015). Naturalistic developmental behavioral interventions: Empirically validated treatments for autism spectrum disorder. Journal of Autism and Developmental Disorders, 45, 2411–2428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreibman L, Stahmer AC, Barlett VC, & Dufek S (2009). Brief Report: Toward Refinement of a Predictive Behavioral Profile for Treatment Outcome in Children with Autism. Research in Autism Spectrum Disorders, 3(1), 163–172. 10.1016/j.rasd.2008.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segall MJ, & Campbell JM (2012). Factors relating to education professionals’ classroom practices for the inclusion of students with autism spectrum disorders. Research in Autism Spectrum Disorders, 6(3), 1156–1167. 10.1016/j.rasd.2012.02.007 [DOI] [Google Scholar]
- Sherer MR, & Schreibman L (2005). Individual behavioral profiles and predictors of treatment effectiveness for children with autism. Journal of Consulting and Clinical Psychology, 73(3), 525–538. 10.1037/0022-006X.73.3.525 [DOI] [PubMed] [Google Scholar]
- Smith T (2001). Discrete Trial Training in the Treatment of Autism. Focus on Autism and Other Developmental Disabilities, 16(2), 86–92. 10.1177/108835760101600204 [DOI] [Google Scholar]
- Smith T, & Iadarola S (2015). Evidence Base Update for Autism Spectrum Disorder. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 44(6), 897–922. 10.1080/15374416.2015.1077448 [DOI] [PubMed] [Google Scholar]
- Smith T, Klorman R, & Mruzek DW (2015). Predicting Outcome of Community-Based Early Intensive Behavioral Intervention for Children with Autism. Journal of Abnormal Child Psychology, 43(7), 1271–1282. 10.1007/s10802-015-0002-2 [DOI] [PubMed] [Google Scholar]
- Stahmer AC, Collings NM, & Palinkas LA (2005). Early Intervention Practices for Children With Autism: Descriptions From Community Providers. Focus on Autism and Other Developmental Disabilities, 20(2), 66–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahmer AC, Reed S, Lee E, Reisinger EM, Connell JE, & Mandell DS (2015). Training Teachers to use Evidence-Based Practices for Autism: Examining Procedural Implementation fidelity. Psychology in the Schools, 52(2), 181–195. 10.1002/pits.21815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahmer AC, Schreibman L, & Cunningham AB (2011). Toward a technology of treatment individualization for young children with autism spectrum disorders. Brain Research, 1380, 229–239. 10.1016/j.brainres.2010.09.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (2007). Using multivariate statistics. Allyn & Bacon/Pearson Education. [Google Scholar]
- Thurm A, Lord C, Lee L-C, & Newschaffer C (2007). Predictors of Language Acquisition in Preschool Children with Autism Spectrum Disorders. Journal of Autism and Developmental Disorders, 37(9), 1721–1734. 10.1007/s10803-006-0300-1 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Education. (2017). 39th Annual Report to Congress on the Implementation of the Individuals with Disabilities Education Act, 2017.
- Vivanti G (2017). Individualizing and combining treatments in autism spectrum disorder: Four elements for a theory-driven research agenda. Current Directions in Psychological Science, 26(2), 114–119. [Google Scholar]
- White SW, Scahill L, Klin A, Koenig K, & Volkmar FR (2007). Educational Placements and Service Use Patterns of Individuals with Autism Spectrum Disorders. Journal of Autism and Developmental Disorders, 37(8), 1403–1412. 10.1007/s10803-006-0281-0 [DOI] [PubMed] [Google Scholar]