Abstract
Background
Familial adenomatous polyposis (FAP) is an autosomal dominant colorectal tumor characterized by numerous adenomatous colonic polyps that often lead to colon cancer. Although most patients with FAP harbored germline mutations in APC gene, it was recently recognized that patients with clinical FAP, but without detectable pathogenic mutations, could be associated with somatic mosaic APC mutation.
Methods
We reanalyzed the nest-generation sequencing (NGS) gene panel testing results of patients who were diagnosed with FAP, but did not have APC mutations, at Yonsei Cancer Prevention Center between July 2016 and March 2018. We tested several variant calling algorithms to identify low level mosaic variants. In one patient with a low frequency APC mutation, NGS analysis was performed together with endoscopic biopsy. Variant calling tools HaplotypeCaller, MuTect2, VarScan2, and Pindel were used. We also used 3′-Modified Oligonucleotides (MEMO)-PCR or conventional PCR for confirmation.
Results
Among 28 patients with clinical suspicion of FAP but no detectable pathogenic variants of colonic polyposis associated genes, somatic mosaic pathogenic variants were identified in seven patients. The variant allele frequency ranged from 0.3 to 7.7%. These variants were mostly detected through variant caller MuTect2 and Pindel, and were further confirmed using mutant enrichment with MEMO-PCR.
Conclusions
The NGS with an adequate combination of bioinformatics tools is effective to detect low level somatic variants in a single assay. Because mosaic APC mutations are more frequent than previously thought, the presence of mosaic mutations must be considered when analyzing genetic tests of patients with FAP.
Electronic supplementary material
The online version of this article (10.1186/s12920-019-0553-0) contains supplementary material, which is available to authorized users.
Keywords: Next-generation sequencing, APC, Somatic mosaic mutation, Familial adenomatous polyposis, Colorectal cancer
Background
Familial adenomatous polyposis (FAP, OMIM#175100) is an autosomal dominant colorectal tumor syndrome characterized by numerous adenomatous colonic polyps that are prone to progress to colon cancer. The majority of patients with FAP harbor a germline mutation in the APC gene on chromosome 5q21. A few other genes, such as MUTYH, POLD1, and POLE, are also associated with hereditary colonic polyposis [1–4]. However, one-fifth of patients with FAP are apparently sporadic without any familial history [5, 6]. It has been widely recognized that some of these sporadic FAP patients have somatic mosaic APC mutations [5–12].
Conventionally, genetic tests for hereditary cancer are performed with leukocyte DNA using PCR and Sanger sequencing. Unlike germline mutations, somatic mutations show various mutant allele frequencies in leukocytes. As a result, a small fraction of mosaic mutations are missed in routine genetic analyses optimized for germline variants, partly due to limited sensitivity of the testing method.
Next-generation sequencing (NGS) has been rapidly adopted in the clinical field. In combination with extensive bioinformatics analysis, NGS can identify a wide range of variants in a single assay, including single nucleotide variations (SNVs), small to large insertions or deletions (indels), and copy number variations. Furthermore, with higher sensitivity, NGS may identify previously undetected variants. Nevertheless, identifying somatic mutations with small variant allele frequencies (VAFs) requires careful consideration throughout the entire process of acquiring sequencing data, choosing analytic tools, and interpreting final results.
Here, we analyzed peripheral blood samples from patients with unexplained FAP using NGS to estimate the frequency of somatic mosaic mutations in the APC gene. We also sought to determine appropriate bioinformatics algorithms for detecting mutations in the APC gene with small VAFs in peripheral blood.
Method
Patients and samples
Among patients who underwent NGS for hereditary cancer between July 2016 and March 2018, 53 were suspicious for FAP on colonoscopy (Table 1). A list of genes included in the NGS panel is provided in Additional file 1: Table S1. Among these 53 patients, 28 were without detectable pathogenic variants in colonic polyposis associated genes (i.e., APC, MUTYH, POLE, and POLD1), and they were subjected to further bioinformatics analysis. If available, colonic polyp specimens obtained during colonoscopy were analyzed. Written informed consent was obtained for all patients. The current study was approved by our institutional review board.
Table 1.
Patients with clinical suspicion of familial adenomatous polyposis and mutation characteristics
| Total | 53 |
| Phenotype | |
| Typical FAP | 18 |
| Attenuated FAP | 35 |
| Age of onset | 39 (19–81) |
| Gene panel results | |
| Pathogenic APC variants | 25 |
| Sequence variation | 23 |
| Deletion or duplication | 2 |
| Patients without pathogenic variants | 28 |
| Further analysis | |
| Mosaicism | 7 |
| Unexplained | 21 |
DNA extraction and sequencing
Genomic DNA was extracted from peripheral blood using the QIAamp DNA Blood Mini Kit (Qiagen, Venlo, The Netherlands). For paraffin-embedded tissue samples, Maxwell® RSC DNA FFPE Kits (Promega, Madison, WI, USA) were used to extract genomic DNA. The amount of input DNA was approximately 500 ng. DNA was fragmented to segments between 150 and 250 bp using the Bioruptor® Pico Sonication System (Diagenode, Liege, Belgium) and then end-repaired and ligated to Illumina adapters (Illumina, San Diego, CA, USA) and indices. Sequencing libraries were then hybridized with capture probes (Celemic, Seoul, Korea). Enriched DNA was then amplified, and clusters were generated and sequenced on a NextSeq 550 instrument (Illumina) with 2 × 151 bp reads. All procedures were performed per the manufacturers’ instructions.
Data analysis and interpretation
The Burrows-Wheeler alignment tool (0.7.12) was used to align reads to human genomic reference sequences (GRCh37) [13]. To identify SNVs and indels, the HaplotypeCaller in the genome analysis tool kit (GATK) package (3.8–0) was used [14]. All mutations were annotated using ANNOVAR and VEP (87) software [15, 16]. Detected variants were further examined by visual verification using the Integrative Genomic Viewer (IGV) [17]. Variants confirmed to be true-positive were further verified by searching the literature and databases.
In addition to HaplotypeCaller and MuTect2 in GATK (3.8–0) and VarScan2 (2.4.0) were used for further bioinformatics analysis of patients without mutations [18, 19]. To detect medium to large indels, Pindel (0.2.0) was used [20], and results from the four algorithms were compared.
Confirmation test
Low level variants in two patients were further confirmed using conventional PCR and Sanger sequencing. Two patients with VAFs on below the detection limit of conventional tests were subjected to mutant enrichment with 3′-modified oligonucleotides (MEMO)-PCR, followed by Sanger sequencing, which is based on the use of a 3’modified oligonucleotide primer that blocks extension of the normal allele but enables extension of the mutated allele [21]. Primers used in MEMO–PCR are shown in Additional file 1: Table S2. For another two patients, Sanger sequencing of colonic polyp specimens was performed.
Results
Patients and NGS statistics
There were 53 patients with a clinical diagnosis of FAP, and 25 pathogenic variants in APC were discovered by NGS for hereditary cancer panel using HaplotypeCaller. Among variants, 23 were sequence variations, and two were partial deletions. They all had VAFs around 0.5 suggestive of germline origin (Additional file 1: Table S3). In the remaining 28 patients, no pathogenic or likely pathogenic variants were observed upon NGS: They comprised patients with a large number of colonic polyps identified on colonoscopy, but no family history of disease associated with colonic polyps (Table 2). One patient had a family history of maternal rectal cancer, although the cancer was not of polyposis type and was diagnosed at the age of 70 years, which can hardly be seen to be associated with APC gene mutation. After reanalysis with additional variant calling tools, seven mosaic mutations in APC were detected in seven patients, comprising 13.2% (7/53) of all patients suspicious for FAP (Table 2). The median depth of coverage in the gene panel was 691×, with a maximum depth of 7976×. The median depth of coverage for APC was 2877×, ranging from 2185× to 4076 × .
Table 2.
Clinical features and variants detected by NGS in patients with somatic APC mosaicism
| ID | Age at onset | Number of polyps | Colorectal carcinoma | Family history | Specimen | Mutation detected | Variant callers (variants allele frequency) | Median depth | Confirmation test | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HC | MuTect2 | VarScan2 | Pindel | ||||||||||
| P1 | 40~49 | 100 s | No | None | leukocyte | c.3295_3296del | p.Val1099PhefsTer19 | ND | 0.077 | ND | 0.068 | 2668 | MEMO-PCR |
| P1 | polyp | c.3295_3296del | p.Val1099PhefsTer19 | 0.206 | 0.206 | 0.228 | 0.197 | 790 | |||||
| P2 | 40~49 | 100 s | Adenocarcinoma | None | leukocyte | c.3860_3861dup | p.Gly1288Ter | ND | 0.035 | 0.094 | 0.032 | 2497 | MEMO-PCR |
| P3 | 30~39 | 200 s | No | None | leukocyte | c.3577_3578del | p.Gln1193ValfsTer14 | ND | 0.003 | ND | 0.003 | 4076 | Tissue |
| P4 | 50~59 | 50–70 | Adenocarcinoma | None | leukocyte | c.1754delT | p.Leu585ProfsTer5 | ND | 0.018 | ND | 0.020 | 2960 | |
| P5 | 40~49 | 30–50 | No | Maternal rectal cancer at the age of 70 | leukocyte | c.694C > T | p.Arg232Ter | ND | 0.034 | ND | ND | 2185 | Tissue |
| P6 | 40~49 | 20–30 | No | None | leukocyte | c.3566C > G | p.Ser1189Ter | 0.114 | 0.114 | 0.114 | ND | 3624 | Sanger sequencing |
| P7 | 30~39 | 300 s | Adenoma | None | leukocyte | c.3211_3238dup | p.Glu1080AlafsTer10 | 0.195 | 0.275 | ND | 0.174 | 1310 | Sanger sequencing |
HC HaplotypeCaller, MEMO Mutant enrichment with 3′-modified oligonucleotides, ND Not detected
Somatic variant detection depends on bioinformatics tools
Somatic mosaic mutations detected in APC are summarized in Table 2. An additional seven somatic mosaic pathogenic variants were identified by further analysis of sequencing data with MuTect2, VarScan2, and Pindel. The seven mutations are known to cause FAP. Five insertion/deletions resulting in a frameshift mutation were identified by both MuTect2 and Pindel tools, and two nonsense variants went undetected by Pindel, as would be expected. The VAFs thereof range from 0.3 to 7.7%. Only two variants (P2 and P6) with relatively high VAFs were detected by VarScan2, and none of the variants with a VAF below 10% were detected by HaplotypeCaller. All variants were identified by IGV (Fig. 1).
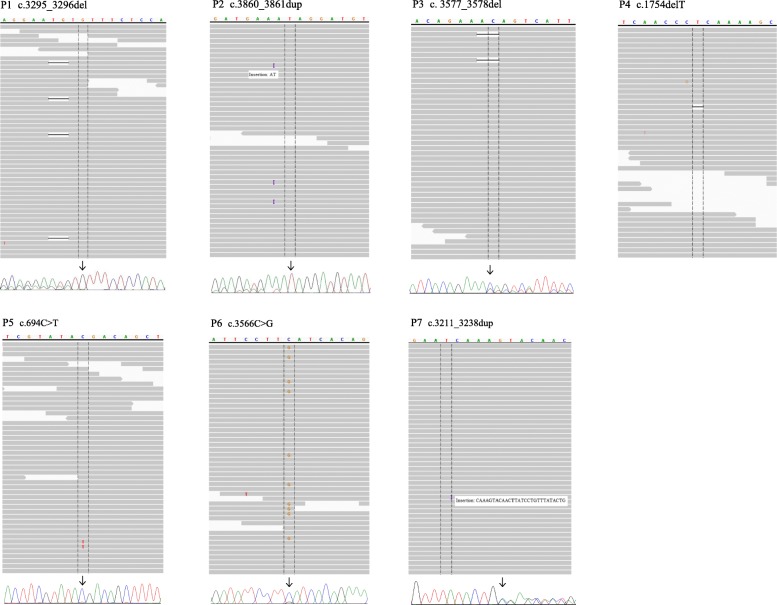
Fig. 1.
Visual verification of variants with Integrative Genomic Viewer (IGV) and sequencing chromatogram with secondary confirmation test results. Variants with low fractions in IGV reflect NGS results from analyzing peripheral blood. The corresponding sequencing chromatograms are the results of MEMO-PCR of peripheral blood for P1 and P2, conventional PCR of polyp tissue for P3 and P5, and conventional PCR of peripheral blood for P6 and P7
Colonic polyp samples from a patient (P1) were subjected to NGS analysis. As shown in Table 2, a somatic mutation found in leukocytes was enriched in the colonic polyp from 7 to 20%, which confirmed the causative effect of the mutation.
Confirmation test
Six of the seven somatic variants were further confirmed by a second method (Table 2 and Fig. 1). From patients P1 to P5, variants went undetected by conventional PCR and sequencing using DNA from leukocytes because of low VAF; two variants (P6 and P7) of relatively high VAF were identified by conventional Sanger sequencing. Two pathogenic variants (P1 and P2) were further confirmed using MEMO-PCR, followed by Sanger sequencing. For P3 and P5, colonic polyp specimens were sequenced by conventional PCR and sequencing to confirm the effect of mutations, and suggested that the causative mutations had been enriched and present at higher fractions in polyp tissue.
Discussion
Familial adenomatous polyposis, an autosomal dominant colorectal tumor syndrome characterized by numerous colorectal adenomatous polyps, is associated with an almost 100% lifetime risk of colorectal cancer if not detected and removed. The majority of patients with FAP harbor a germline mutation in the APC gene, and patients typically report family members with the same condition, confirming its autosomal dominant inheritance.
Approximately 10 to 25% of patients with FAP present as sporadic cases [5, 6]. It has been widely recognized that somatic mosaic mutation in APC is associated with FAP and is more frequent than previously thought [5, 6, 8, 9]. Since the somatic mutation is invariably a de novo event, patients with mosaic APC mutation typically have no family history of FAP. Previous reports have described enrichment of APC mutation from white blood cells to colonic mucosa and adenomas, confirming the critical role of mosaic mutation in tumorigenesis [5, 6, 8, 22].
In the present study, seven cases with mosaic APC mutations were highly suspected to have FAP based on endoscopic findings, but had no pathogenic variants in genes known to be associated with this condition and no family history of colonic polyposis. The mutation profile of colon tissue was not verified in four patients, and there is a high probability that the colonic lesions shared the same mutation as blood cells. Considering the ectodermal and endodermal origins of blood cells and colonic epithelia, respectively, we presume that the mutations in these cases occurred during early embryogenesis before separation of the two layers [5, 8, 23]. Because this process occurs before germ cell differentiation, the presence of germ cells with the same mutation and transmission thereof to descendants cannot be ruled out. Thus, genetic counseling is necessary, and children of probands might require genetic testing.
APC somatic mosaicism is known to be associated with both classical and attenuated FAP [5, 6]. In seven patients with APC somatic mosaicism in this study, the median age of onset was 45 years (range 31–53), while that of patients with germline mutations was 34 years. The number of polyps in patients with APC somatic mosaicism was round 100 or smaller, while patients with classical FAP presented with more than 100 polyps [24]. Collectively, the patients with somatic mosaic APC mutations tended to exhibit an attenuated phenotype.
Testing with NGS and analysis with MuTect2 and Pindel algorithms detected low level mosaic mutations of the APC gene that were assumed to cause the disease. While somatic mosaic mutation of the APC gene has recently been recognized, conventional sequencing methods have limited sensitivity in the detection thereof. Even with deep sequencing by NGS, variants with low VAF might be missed if analyses are based on the assumption that they are heterozygotes with an allele frequency of at least 0.3. Care must be taken when analyzing and interpreting hereditary cancer genes known to be mutated in a mosaic pattern, such as APC and PPM1D [25, 26]. The possibility of low-level mosaic mutation should be considered.
There are several previous reports on the detection of somatic mosaic mutations of the APC gene [5–11]. To detect low-level mutant alleles, various methods have been used, including denaturing high-performance liquid chromatography, protein truncation test, and high-resolution melting analysis [5–7]. These are less feasible to apply in routine genetic testing for hereditary cancer. We produced sequencing data in a single assay and analyzed them with several algorithms to detect low level variants. GATK HaplotypeCaller is widely used to identify germline variants, and MuTect2 and VarScan2 are optimized to identify variants in cancer specimens [14, 18, 19]. Pindel is a split-read analysis tool for medium to large indels [20]. Among the four variant callers used, only MeTect2 and Pindel could detect low-level mosaic pathogenic variants, with VAFs of 0.2–0.8%. The NGS method has a sensitivity of 10− 5~10− 6 with adequate sequencing quality and sequencing depth. In addition to adequate analytic tools, it is worth emphasizing the importance of sufficient read depth and careful visual verification to distinguish true variants because tools used to detect low-level variants tend to produce more false positive results.
Conclusions
We confirmed the clinical utility of NGS testing with adequate combination of bioinformatics tools in detecting low-level somatic variants and deletions in a single assay. We also discovered that mosaic APC mutation may be more frequent than previously thought. Accordingly, the presence of mosaic mutation should be considered when analyzing genetic tests in patients with FAP.
Additional file
Table S1. Genes included in the hereditary cancer panel. Table S2. Primers used in the MEMO-PCR to confirm low-level variants in APC. Table S3. Pathogenic or likely pathogenic germline APC variants in patients suspicious for familial adenomatous polyposis. Table S4. All variants identified from NGS hereditary cancer panel. (DOCX 58 kb)
Acknowledgements
We thank Eunsun Lee, Jiwoong Gang, Junyoung Hong, and Jongsun Park for performing experiments for NGS and conventional sequencing.
Abbreviations
- FAP
Familial adenomatous polyposis
- GATK
Genome analysis tool kit
- IGV
Integrative Genomic Viewer
- indels
Insertions or deletions
- MEMO
Mutant enrichment with 3′-modified oligonucleotides
- NGS
Next-generation sequencing
- SNV
Single nucleotide variation
- VAF
Variant allele frequency
Authors’ contributions
BK and DW analyzed the sequencing data and wrote the manuscript. MJ and HK participated in data analysis and pathology review. TK, JRC, and STL enrolled the patients, designed the study, and revised the manuscript. All authors have read and approved the manuscript.
Funding
There was no funding source regarding this study.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to the policy of the laboratory but are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was approved by the Severance Hospital Institutional Review Board.(4–2018-0556). Written consents were obtained from all patients tested for NGS of a hereditary cancer panel.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Borahm Kim and Dongju Won contributed equally to this work.
Contributor Information
Borahm Kim, Email: BKIM0819@yuhs.ac.
Dongju Won, Email: WDJBABO@yuhs.ac.
Mi Jang, Email: MJROSE511@yuhs.ac.
Hoguen Kim, Email: HKYONSEI@yuhs.ac.
Jong Rak Choi, Email: CJR0606@yuhs.ac.
Tae Il Kim, Phone: 82-2-2228-1965, Email: TAEILKIM@yuhs.ac.
Seung-Tae Lee, Phone: 82-2-2228-2450, Email: LEE.ST@yuhs.ac.
References
- 1.Elsayed FA, Kets CM, Ruano D, van den Akker B, Mensenkamp AR, Schrumpf M, et al. Germline variants in POLE are associated with early onset mismatch repair deficient colorectal cancer. Eur J Hum Genet. 2015;23(8):1080–1084. doi: 10.1038/ejhg.2014.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mazzei F, Viel A, Bignami M. Role of MUTYH in human cancer. Mutat Res. 2013;743-744:33–43. doi: 10.1016/j.mrfmmm.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 3.Newton KF, Mallinson EK, Bowen J, Lalloo F, Clancy T, Hill J, et al. Genotype-phenotype correlation in colorectal polyposis. Clin Genet. 2012;81(6):521–531. doi: 10.1111/j.1399-0004.2011.01740.x. [DOI] [PubMed] [Google Scholar]
- 4.Palles C, Cazier JB, Howarth KM, Domingo E, Jones AM, Broderick P, et al. Germline mutations affecting the proofreading domains of POLE and POLD1 predispose to colorectal adenomas and carcinomas. Nat Genet. 2013;45(2):136–144. doi: 10.1038/ng.2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aretz S, Stienen D, Friedrichs N, Stemmler S, Uhlhaas S, Rahner N, et al. Somatic APC mosaicism: a frequent cause of familial adenomatous polyposis (FAP) Hum Mutat. 2007;28(10):985–992. doi: 10.1002/humu.20549. [DOI] [PubMed] [Google Scholar]
- 6.Hes FJ, Nielsen M, Bik EC, Konvalinka D, Wijnen JT, Bakker E, et al. Somatic APC mosaicism: an underestimated cause of polyposis coli. Gut. 2008;57(1):71–76. doi: 10.1136/gut.2006.117796. [DOI] [PubMed] [Google Scholar]
- 7.Out AA, van Minderhout IJ, van der Stoep N, van Bommel LS, Kluijt I, Aalfs C, et al. High-resolution melting (HRM) re-analysis of a polyposis patients cohort reveals previously undetected heterozygous and mosaic APC gene mutations. Familial Cancer. 2015;14(2):247–257. doi: 10.1007/s10689-015-9780-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iwaizumi M, Tao H, Yamaguchi K, Yamada H, Shinmura K, Kahyo T, et al. A novel APC mosaicism in a patient with familial adenomatous polyposis. Hum Genome Var. 2015;2:15057. doi: 10.1038/hgv.2015.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spier I, Drichel D, Kerick M, Kirfel J, Horpaopan S, Laner A, et al. Low-level APC mutational mosaicism is the underlying cause in a substantial fraction of unexplained colorectal adenomatous polyposis cases. J Med Genet. 2016;53(3):172–179. doi: 10.1136/jmedgenet-2015-103468. [DOI] [PubMed] [Google Scholar]
- 10.Yamaguchi K, Komura M, Yamaguchi R, Imoto S, Shimizu E, Kasuya S, et al. Detection of APC mosaicism by next-generation sequencing in an FAP patient. J Hum Genet. 2015;60(5):227–231. doi: 10.1038/jhg.2015.14. [DOI] [PubMed] [Google Scholar]
- 11.Benson AA, Shirts BH, Jacobson A, Pritchard CC, Walsh T, Jacob H, et al. Polyposis caused by low APC mosaicism. J Genet Syndr Gene Ther. 2016;7(1):281.
- 12.Necker J, Kovac M, Attenhofer M, Reichlin B, Heinimann K. Detection of APC germ line mosaicism in patients with de novo familial adenomatous polyposis: a plea for the protein truncation test. J Med Genet. 2011;48(8):526–529. doi: 10.1136/jmg.2011.089474. [DOI] [PubMed] [Google Scholar]
- 13.Li H. Toward better understanding of artifacts in variant calling from high-coverage samples. Bioinformatics. 2014;30(20):2843–2851. doi: 10.1093/bioinformatics/btu356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DePristo MA, Banks E, Poplin R, Garimella KV, Maguire JR, Hartl C, et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat Genet. 2011;43(5):491–498. doi: 10.1038/ng.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010;38(16):e164. doi: 10.1093/nar/gkq603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McLaren W, Pritchard B, Rios D, Chen Y, Flicek P, Cunningham F. Deriving the consequences of genomic variants with the Ensembl API and SNP effect predictor. Bioinformatics. 2010;26(16):2069–2070. doi: 10.1093/bioinformatics/btq330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robinson JT, Thorvaldsdottir H, Winckler W, Guttman M, Lander ES, Getz G, et al. Integrative genomics viewer. Nat Biotechnol. 2011;29(1):24–26. doi: 10.1038/nbt.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koboldt DC, Zhang Q, Larson DE, Shen D, McLellan MD, Lin L, et al. VarScan 2: somatic mutation and copy number alteration discovery in cancer by exome sequencing. Genome Res. 2012;22(3):568–576. doi: 10.1101/gr.129684.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cibulskis K, Lawrence MS, Carter SL, Sivachenko A, Jaffe D, Sougnez C, et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat Biotechnol. 2013;31(3):213–219. doi: 10.1038/nbt.2514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ye K, Schulz MH, Long Q, Apweiler R, Ning Z. Pindel: a pattern growth approach to detect break points of large deletions and medium sized insertions from paired-end short reads. Bioinformatics. 2009;25(21):2865–2871. doi: 10.1093/bioinformatics/btp394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee ST, Kim JY, Kown MJ, Kim SW, Chung JH, Ahn MJ, et al. Mutant enrichment with 3′-modified oligonucleotides a practical PCR method for detecting trace mutant DNAs. J Mol Diagn. 2011;13(6):657–668. doi: 10.1016/j.jmoldx.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stoffel EM, Koeppe E, Everett J, Ulintz P, Kiel M, Osborne J, et al. Germline genetic features of young individuals with colorectal cancer. Gastroenterology. 2018;154(4):897–905. doi: 10.1053/j.gastro.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jansen AM, Crobach S, Geurts-Giele WR, van den Akker BE, Garcia MV, Ruano D, et al. Distinct patterns of somatic mosaicism in the APC gene in neoplasms from patients with unexplained adenomatous polyposis. Gastroenterology. 2017;152(3):546–9.e3. doi: 10.1053/j.gastro.2016.10.040. [DOI] [PubMed] [Google Scholar]
- 24.Knudsen AL, Bisgaard ML, Bulow S. Attenuated familial adenomatous polyposis (AFAP). A review of the literature. Familial Cancer. 2003;2(1):43–55. doi: 10.1023/A:1023286520725. [DOI] [PubMed] [Google Scholar]
- 25.Ruark E, Snape K, Humburg P, Loveday C, Bajrami I, Brough R, et al. Mosaic PPM1D mutations are associated with predisposition to breast and ovarian cancer. Nature. 2013;493(7432):406–410. doi: 10.1038/nature11725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swisher EM, Harrell MI, Norquist BM, Walsh T, Brady M, Lee M, et al. Somatic mosaic mutations in PPM1D and TP53 in the blood of women with ovarian carcinoma. JAMA Oncol. 2016;2(3):370–372. doi: 10.1001/jamaoncol.2015.6053. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Genes included in the hereditary cancer panel. Table S2. Primers used in the MEMO-PCR to confirm low-level variants in APC. Table S3. Pathogenic or likely pathogenic germline APC variants in patients suspicious for familial adenomatous polyposis. Table S4. All variants identified from NGS hereditary cancer panel. (DOCX 58 kb)
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to the policy of the laboratory but are available from the corresponding author on reasonable request.