Retinal astrocytomas (RAs) are benign, glial tumors of the retinal nerve fiber layer that arise from retinal astrocytes. They may be associated with tuberous sclerosis, neurofibromatosis, or can also be found incidentally as an isolated presentation.[1] We herein discuss multicolor imaging (MC) in RA.
A 40-year-old female patient came for routine eye check up. Best-corrected visual acuity was 20/20 in both the eyes. The right eye was normal. Fundus examination of the left eye showed creamy white, semi-translucent, well-circumscribed, elevated lesion superior to the optic disc [Fig. 1a]. MC highlighted mulberry appearance of the lesion and green shift corresponding to the entire extent of tumor mass [Fig. 1b]. In infrared reflectance (IR), lesion was hyporeflective with its margins well delineated [Fig. 1c]. Fundus autofluorescence (FAF) showed typical hyperautofluorescence [Fig. 1d]. Green reflectance (GR) [Fig. 2a] and blue reflectance (BR) [Fig. 2b] highlighted calcification as multiple hyperreflective dots. Spectral domain optical coherence tomography (SD-OCT) showed moth-eaten optically empty spaces and area of retinal thickening adjacent to the elevated lesion [Fig. 2c]. Tumor margins were better delineated on MC [Fig. 1b] and IR [Fig. 1c].
Figure 1.
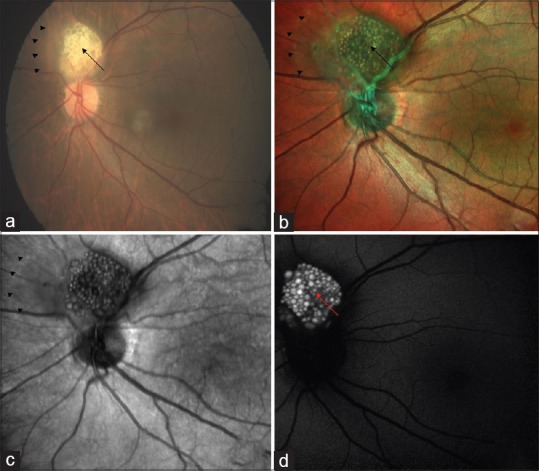
Color fundus photography of left eye (a) showing creamy white, semi-translucent, well-circumscribed, elevated lesion superior to the optic disc (black arrow). Multicolor imaging (b) highlighted mulberry appearance of the lesion (black arrow) and green shift corresponding to entire extent of tumor mass (arrow heads). In infrared reflectance (c), lesion was hyporeflective with its margins well delineated (arrow heads). Fundus autofluorescence (d) showed typical hyperautofluorescence
Figure 2.
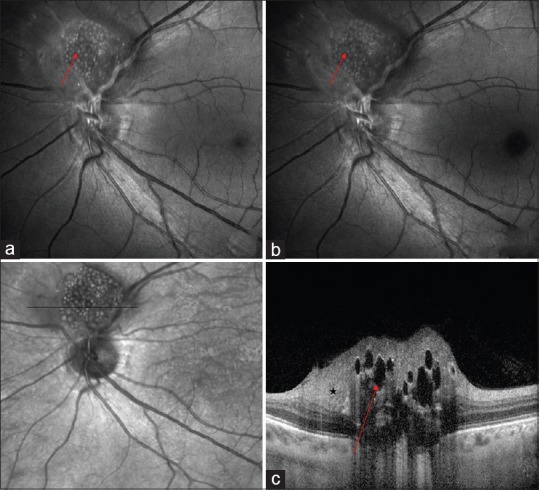
Green reflectance (a) and blue reflectance (b) highlighted calcification as multiple hyperreflective dots (red arrows). Spectral domain optical coherence tomography (c) showed moth-eaten optically empty spaces (red arrow) and area of retinal thickening adjacent to the elevated lesion (star)
RA should be differentiated from similar looking lesions including choroidal osteoma, optic nerve head drusen, chorioretinitis, retinoblastoma,[2] and Von Hippel angiomas. SD-OCT features described by Shields et al. were gradual dome-shaped elevation with hyperreflectivity, retinal disorganization, and a characteristic moth-eaten appearance.[3] Semenova et al. had described multimodal imaging in RA.[4] In their series, fundus fluorescein angiography was helpful in delineating tumor vascularity and FAF picked up intralesional calcification as hyperautofluorescent spots. MC is a novel innovative noninvasive retinal imaging modality.[5] MC with its component images highlighted extent of the lesion (IR) and internal character like calcification (GR and BR) excellently. Clinicians may consider MC as an additional tool in their imaging armoury to document and monitor RA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ulbright TM, Fulling KH, Helveston EM. Astrocytic tumors of the retina. Differentiation of sporadic tumors from phakomatosis-associated tumors. Arch Pathol Lab Med. 1984;108:160–3. [PubMed] [Google Scholar]
- 2.Chawla B, Khurana S, Sen S, Sharma S. Clinical misdiagnosis of retinoblastoma in Indian children. Br J Ophthalmol. 2014;98:488–93. doi: 10.1136/bjophthalmol-2013-304321. [DOI] [PubMed] [Google Scholar]
- 3.Shields CL, Roe R, Yannuzzi LA, Shields JA. Solitary circumscribed “pearl white” retinal mass (so-called retinal astrocytic proliferation) resides in deep retina or beneath retina: Findings on multimodal imaging in 4 cases. Retin Cases Brief Rep. 2017;11:18–23. doi: 10.1097/ICB.0000000000000278. [DOI] [PubMed] [Google Scholar]
- 4.Semenova E, Veronese C, Ciardella A, Marcheggiani EB, Shah S, De-Pablo-Gomez-de-Liaño L, et al. Multimodality imaging of retinal astrocytoma. Eur J Ophthalmol. 2015;25:559–64. doi: 10.5301/ejo.5000627. [DOI] [PubMed] [Google Scholar]
- 5.Tan AC, Fleckenstein M, Schmitz-Valckenberg S, Holz FG. Clinical application of multicolor imaging technology. Ophthalmologica. 2016;236:8–18. doi: 10.1159/000446857. [DOI] [PubMed] [Google Scholar]


