Abstract
We present two cases of women who suffered from neurotrophic keratopathy (one of them had undergone penetrating keratoplasty) which had led to corneal thinning. Tachosil® was used as an adjuvant treatment after topical medication by itself failed in both cases. To our knowledge, there are no reported cases of the use of Tachosil® in corneal grafts.
Keywords: Corneal graft, corneal ulcer, neurotrophic keratopathy, Tachosil®
Tachosil® is a fibrin sealant patch resulting from equine collagen coated with human fibrinogen and thrombin,[1] which forms a fibrin clot when exposed to body fluids allowing the collagen to adhere to the tissue surface.[2] It is mainly used by different surgical specialties in order to achieve hemostasis, although other uses such as preventing chylothorax[3] or during prosthesis implantation in patients with Peyronie's disease[4] have been described.
Case Report
The first case corresponds to a 95-year-old Caucasian female patient who was referred to our hospital for eye redness in her right eye. Her medical history included hypertension and diabetes mellitus. For over 8 years she had been under ophthalmological treatment with artificial tears, autologous serum eye drops, and bandage contact lens due to continuous corneal epithelial defects as a result of neurotrophic keratopathy secondary to diabetes mellitus.
Anterior segment slit lamp examination revealed conjunctival hyperemia, superficial punctate keratitis, and a positive-fluorescein-staining paracentral area of local corneal thinning one-by-two millimeters [Fig. 1a]. No signs of anterior chamber inflammation or infection were present and the patient referred no pain. A piece of twisted cotton was used to qualitatively examine corneal sensitivity, being difficult for the patient to tell if the cotton piece was touching or not her cornea and no blinking response was obtained.
Figure 1.
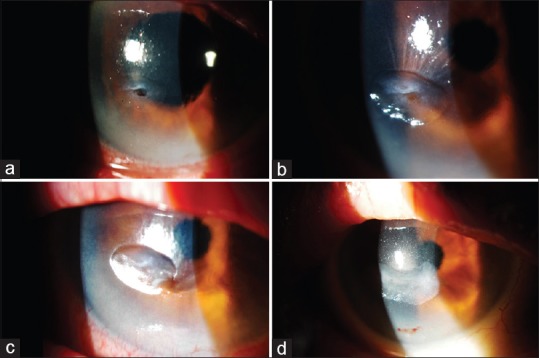
Evolution of paracentral corneal thinning in patient 1. (a). At diagnosis. (b). After first Tachosil® use. (c). After second Tachosil® use. (d). After third Tachosil® use
As the corneal defect was not limited to the corneal epithelium, we considered that a surgical approach to mechanically cover the defect was needed in order to avoid perforation as medical treatment itself would fail to control the situation in the short term. However, a corneal transplant or conjunctival coating was not considered as the best options due to the patient's age, corneal neurotrophism, and the defect's location. We did not have access to amniotic membrane in that moment, so we decided to use Tachosil®. Using topical anesthesia, the Tachosil® sponge previously cut to the correct size, was placed over the corneal defect, and physiological saline solution was used to enhance the adherence of the collagen to the corneal tissue. It was then covered with a bandage contact lens for 24 hours in order for the patch not to move from place.
The treatment was repeated on three occasions spacing 3 days each patching. A layer of fibrin was formed over the corneal defect and beyond its margins and although a leukoma remained, the corneal thinning and therefore the perforation risk were corrected with no need of major surgical interventions [Fig. 1b–d]. Topical medication including autologous serum and artificial tears was continued.
The second case corresponds to a 72-year-old Caucasian female patient who was referred to our hospital for eye redness in her right eye. She had undergone penetrating keratoplasty as a result of a facial chemical burn 6 years ago, which had also lead to multiple eyelid surgeries leaving a severe eye occlusion defect. She was under treatment with artificial tears, autologous serum eye drops, and lubricant eye gels. Slit lamp examination revealed conjunctival hyperemia and a positive-fluorescein-staining local corneal thinning associated to local corneal neovascularization secondary to corneal exposure, with no signs of infection [Fig. 2a]. The patient referred no pain. A piece of twisted cotton was used to qualitatively examine corneal sensitivity, but again no blinking response was obtained.
Figure 2.
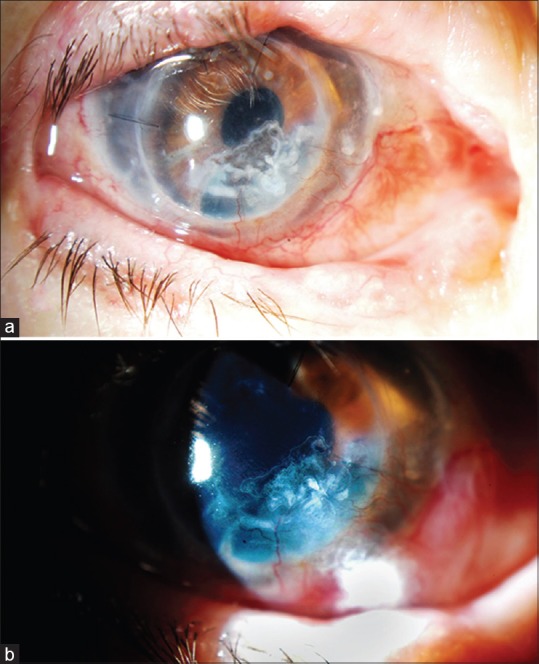
Evolution of corneal thinning in corneal graft in patient 2. (a). At diagnosis. (b). After second Tachosil® use
We decided to use Tachosil® due to the risk of perforation and corneal graft failure. In this case, a new corneal graft was not considered due to intense neovascularization and in that moment we did not have access to amniotic membrane. After repeating the treatment two times using the same method as described above [Video Clip 1], a significant improvement was achieved (no significant corneal dellen was appreciated after this) and the necessity of undergoing another penetrating keratoplasty was avoided. However, a mild corneal leukoma persisted [Fig. 2b].
Discussion
Tachosil® has been described in medical literature as a useful treatment in different keratopathies, especially when other therapeutical options are not available or not indicated in certain patients. Corneal micro- and macroperforations using Tachosil® as an isolated treatment[5,6,7] or combined with amniotic membrane[8] have been described as the main ophthalmological applications of Tachosil®. However, there are no reported cases of its use in corneal grafts.
In our experience, it was successful as a first-line treatment in severe complications of neurotrophic corneal ulcers (excessive corneal thinning with perforation risk) after applying it several times, although a leukoma remained in both cases, making it less useful if corneal defects are located near the visual axis. Although it is not a definite treatment for neurotrophic keratopathy, it can avoid further complications caused by this disorder such as ocular perforations, by creating a collagen membrane over corneal defects. It represents a simple solution in cases in which patients are not good candidates for corneal keratoplasty and other corneal bandages such as amniotic membrane are not available.
Conclusion
Neurotrophic corneal defects usually represent a challenge for clinical physicians due to the lack of effective treatments. Further investigation should be considered in to study the role of Tachosil® and compare its effectiveness with other biological adhesives as there are no reported studies concerning its ophthalmological use.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video available on: www.ijo.in
References
- 1.Glineur D, Hendrikx M, Krievins D, Stradins P, Voss B, Waldow T, et al. A randomized, controlled trial of VerisetTM hemostatic patch in halting cardiovascular bleeding. Med Devices (Auckland, NZ) 2018;11:65–75. doi: 10.2147/MDER.S145651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiarelli M, Achilli P, Guttadauro A, et al. Chylothorax after mediastinal ganglioneuroma resection treated with fibrin sealant patch: A case report. J Thorac Dis. 2017;9:E748–51. doi: 10.21037/jtd.2017.08.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vida VL, Padalino MA, Barzon E, Stellin G. Efficacy of fibrinogen/thrombin-coated equine collagen patch in controlling lymphatic leaks. J Card Surg. 2012;27:441–2. doi: 10.1111/j.1540-8191.2012.01461.x. [DOI] [PubMed] [Google Scholar]
- 4.Garcia-Gomez B, Ralph D, Levine L, Moncada-Iribarren I, Djinovic R, Albersen M, et al. Grafts for Peyronie's disease: A comprehensive review. Andrology. 2018;6:117–26. doi: 10.1111/andr.12421. [DOI] [PubMed] [Google Scholar]
- 5.Cañones-Zafra R, Benítez-Herreros J, Kubiak K, Montes-Mollón MA, Jiménez-Parras R. Sterile non-traumatic corneal perforation treated with Tachosil®. Arch Soc Esp Oftalmol. 2011;86:264–6. doi: 10.1016/j.oftal.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Feliciano-Sánchez A, García-Gil R. Non-infectious corneal macroperforations treated with a combination of Tachosil(®) and Tutopach(®). A report of 2 cases. Arch Soc Esp Oftalmol. 2014;89:250–3. doi: 10.1016/j.oftal.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Hurtado-Sarrió M, Duch-Samper A, Cisneros-Lanuza A, Díaz-Llopis M. Tachosil: A new alternative for the treatment of non-traumatic corneal perforations. Br J Ophthalmol. 2009;93:1410–1. doi: 10.1136/bjo.2009.158949. [DOI] [PubMed] [Google Scholar]
- 8.Grau AE, Durán JA. Treatment of a large corneal perforation with a multilayer of amniotic membrane and TachoSil. Cornea. 2012;31:98–100. doi: 10.1097/ICO.0b013e31821f28a2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


