Abstract
Background
Corticosteroids, plasma exchange, and intravenous immunoglobulin (IVIG) have been standard-of-care treatments for chronic inflammatory demyelinating polyneuropathy (CIDP) for more than 2 decades. Despite guideline recommendations for best clinical practices, heterogeneity in patient presentation and the course of treatment for CIDP remains. There is limited literature regarding the real-world treatment patterns of and costs associated with CIDP.
Objective
To analyze and describe the real-world treatment patterns of and economic burden associated with CIDP.
Methods
This retrospective cohort study evaluated the treatment patterns and CIDP-related healthcare costs over a 2-year follow-up period for patients with newly diagnosed CIDP who had commercial insurance, using claims data from the IMS LifeLink PharMetrics Plus Claims database between 2009 through 2014. Treatment-naïve patients with newly diagnosed CIDP were evaluated for 2 years postdiagnosis, which captured the treatments used and the resource utilization. The patients were defined as receiving active CIDP therapy (ie, IVIG, immunosuppressants, oral or intravenous steroids, or plasma exchange) or active surveillance.
Results
Of the 525 patients identified with newly diagnosed CIDP, 55.2% of patients were prescribed only steroid therapy, and 25.3% of patients were prescribed an IVIG therapy during the 2-year follow-up. The median time to the initial treatment was shortest for patients receiving plasma exchange alone (0.03 months) or in combination with a steroid (0.03 months), followed by IVIG plus another therapy (0.53 months), and then IVIG alone (0.71 months). Initiating therapy with steroids alone took the longest mean time (6.51 months) to start the treatment. The median length of time to receive therapy was longest for the steroid plus plasma exchange cohort (21.8 months), followed by the steroid plus immunosuppressant cohort (10.1 months), and the 2 IVIG cohorts (9.04 months for IVIG alone and 9.82 months for IVIG plus another therapy). The mean total CIDP-specific 2-year follow-up costs were highest for the cohort that received IVIG alone ($119,928) or with an additional therapy ($133,334) and lowest for patients who received active surveillance ($3723) or steroids alone ($3101).
Conclusions
Steroid therapy was initiated later and resulted in a shorter duration of treatment than other treatment options for patients with CIDP, which may reflect diagnostic uncertainty, disease severity or remission, therapeutic challenge to determine diagnosis, or the side-effect profile of steroids. The use of steroids alone was the most common prescribed treatment for CIDP. Further research is needed to understand the rationale for treatment decisions in this patient population and their potential impact on patients and health plans.
Keywords: chronic inflammatory demyelinating polyneuropathy, CIDP, economic burden, healthcare costs, intravenous immunoglobulin, IVIG, plasma exchanges, steroids, treatment patterns
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an inflammatory disorder of the peripheral nervous system. The classic clinical features of CIDP include symmetrical weakness in proximal and distal muscles, sensory loss, imbalance, impaired ambulation, and disease progression for 8 weeks or more.1,2 In clinical practice, however, patients may present with heterogeneity in their clinical and electrophysiologic features.1 The disease course for CIDP can be relapsing and remitting or progressive, and approximately 66% of patients have progressive disease.1 Individual heterogeneity in disease severity and disability, as well as treatment response, affect the choice of initial and long-term therapy.2,3 Although prevalence estimates vary widely (from 1.9 to 7.7 per 100,000), a US study examining medical records spanning 20 years in Olmsted County, MN, estimated the prevalence of CIDP to be 8.9 per 100,000 persons and the annual incidence of CIDP to be 1.6 per 100,000.4 The disorder generally affects individuals aged 40 to 60 years, and is more common in men than in women.1
KEY POINTS
-
▸
Chronic inflammatory demyelinating polyneuropathy (CIDP) affects the peripheral nervous system characterized by muscle weakness, imbalance, and impaired ambulation.
-
▸
Current guidelines for CIDP recommend first-line treatment with corticosteroids, plasma exchange, and intravenous immunoglobulin (IVIG).
-
▸
This retrospective cohort study is among the first to evaluate the real-world treatment patterns and economic burden of CIDP for patients with commercial insurance, using claims data.
-
▸
During a 2-year follow-up, 55.2% of patients received steroid therapy alone, 25.3% received IVIG therapy, and immunosuppressive therapy and plasma exchanges were rarely used.
-
▸
The median time to first treatment was shortest with plasma exchange alone or in combination with a steroid, followed by IVIG plus another therapy, and then IVIG alone.
-
▸
The mean total 2-year costs were highest for IVIG alone ($119,928) or with another therapy ($133,334) and lowest for active surveillance ($3723) or steroids alone ($3101).
-
▸
The use of steroids alone was prescribed most often, but the treatment patterns were unexpected.
-
▸
Further research is needed to explore the rationale of the treatment decision-making for patients with CIDP.
Several groups have proposed diagnostic criteria for CIDP, including the European Federation of Neurological Societies (EFNS), Peripheral Nerve Society (PNS),5 and the American Academy of Neurology (AAN).6 Most diagnostic criteria sets rely on a combination of clinical, electrodiagnostic, and laboratory features to eliminate other disorders that may mimic CIDP. However, the diagnosis of CIDP can be challenging in real-world clinical practice, as was outlined by Allen and Lewis.7
The primary goals of treatment for CIDP are to reduce the symptoms, improve functional status, and maintain long-term disease remission.1,8–10 The first-line treatments for CIDP include corticosteroids, plasma exchange, and intravenous immunoglobulin (IVIG).5 Corticosteroids have demonstrated good short-term efficacy and a longer remission period.1 Although steroids are generally inexpensive, they have potentially serious side effects and are tolerated poorly when used for long-term therapy.1 Plasma exchange is an effective treatment option for CIDP and has a rapid onset of therapeutic benefit; however, patients who receive this treatment are the quickest to have a relapse, thus requiring repeated plasma exchanges, which are invasive and lengthy.1,11,12 In addition, plasma exchange is expensive and labor intensive, and its long-term use may require central-line peripheral venous access.1,11 As such, the AAN recommends plasma exchange for the short-term treatment of CIDP (Level A recommendation).13
IVIG has been a standard-of-care treatment for patients with CIDP for more than 2 decades, with 50% to 70% of patients responding to IVIG treatment.8,14,15 Immunoglobulins have a quick onset of action and a more sustained treatment effect than plasma exchange, and the AAN evidence-based treatment guidelines recommend using IVIG for the long-term treatment of CIDP (Level A).16 The EFNS/PNS treatment guidelines recommend using IVIG as the initial therapy (Level A) for various forms of CIDP.5
Alternative immunosuppressive treatment regimens, such as azathioprine, mycophenolate mofetil, oral methotrexate, and rituximab, are sometimes used in patients whose disease has not improved with these conventional treatments, in patients whose disease has improved and they still have frequent relapses, or in patients with intolerable side effects.5,11 However, alternative therapies have limited robust data to support their efficacy and remain an alternative to first-line therapy.1,11 Patients with very mild symptoms that do not affect activities of daily living may be monitored without treatment (ie, active surveillance).
Despite the availability of consensus guidelines, very limited information is available about the real-world treatment patterns for CIDP, especially the long-term treatment, as well as the economic burden associated with CIDP in the United States. Given the limited information available, the objective of this study was to evaluate the 2-year treatment patterns, along with medical and pharmacy healthcare costs for patients with newly diagnosed CIDP, based on diagnosis codes in a commercially insured US population.
Methods
This study used integrated healthcare claims data from the IMS LifeLink PharMetrics Plus Claims database between January 1, 2009, through June 30, 2014. The database contains administrative medical and pharmacy claims, as well as eligibility records for more than 103 managed healthcare plans, encompassing more than 150 million lives, approximately 90 million of whom have medical and pharmacy benefits. Patients in the majority of 3-digit zip codes and in every metropolitan statistical area of the United States are represented in the database, with coverage of data from 90% of US hospitals and 80% of all US doctors. The approximate distribution of health plans is 80% commercial, 3% Medicaid, and 1.7% Medicare, with the remaining health plans categorized as “other.” All the data in the study database are compliant with the Health Insurance Portability and Accountability Act of 1996 to protect patient privacy.
Study Design
In this descriptive study we used a retrospective cohort design to identify patients with a diagnosis of CIDP (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] code 357.81). The index date was defined as the date of the earliest medical claim with a diagnosis code for CIDP. The patients had to be aged ≥18 years at the first diagnosis of CIDP, have no diagnosis codes for CIDP or CIDP-related treatment in the 12-month preindex period, and have continuous health plan enrollment with medical and pharmacy benefits during the 12-month preindex period and the 2-year follow-up period after their initial diagnosis of CIDP. Patients who did not receive a CIDP-related treatment after their index diagnosis had to have a second diagnosis of CIDP at least 90 days after their index CIDP diagnosis date to confirm their diagnosis of CIDP. The full set of exclusion criteria are provided in Table 1.
Table 1.
Identification of Final Study Population
| Sequential attrition | Patients remaining,a N (%) |
|---|---|
| Index diagnosis date between January 1, 2010, and June 30, 2012 | 5399 (41.9) |
| Continuous eligibility between 1-year preindex and 2 years postindex | 2182 (16.9) |
| Aged ≥18 years at index diagnosis date | 2135 (16.6) |
| No exclusionary diagnosis during the 3-year patient-specific study time frame | 1063 (8.2) |
| No treatment of interest in the 12-month preindex period (ie, IVIG, corticosteroid, immunosuppressant, plasma exchange) | 879 (6.8) |
| Total population of treated patients, plus untreated patients with a second diagnosis of CIDP within >90 days of index diagnosis of CIDP | 525 (4.1) |
| Final sample size | 525 (4.1) |
Number of patients remaining after each exclusion.
CIDP indicates chronic inflammatory demyelinating polyneuropathy; IVIG, intravenous immunoglobulin.
The patients who met these criteria were placed into cohorts based on the presence or absence of active CIDP therapy. Patients were defined as receiving active CIDP therapy if they had a therapy that was identified with Healthcare Common Procedure Coding System codes or National Drug Codes during the 2-year follow-up period for IVIG, immunosuppressants, oral or intravenous steroids, or plasma exchange. The patients without any evidence of active treatment were considered to have active surveillance; these patients also had 2 diagnosis claims of CIDP at least 90 days apart. The IVIG drugs included Carimune, Flebogamma, Gammagard, Gammaplex, Gamunex-C, Octagam, and Privigen. The steroids included oral or intravenous dexamethasone, methylprednisolone, prednisolone, and prednisone. The immunosuppressive drugs included azathioprine, cyclophosphamide, cyclosporine, methotrexate, mycophenolate mofetil, rituximab, and tacrolimus.
To further ensure that treatments were related to CIDP, patients who had additional medical diagnoses where IVIG, immunosuppressants, or plasma exchange could be recommended were excluded from the study. Accordingly, the study design attempted to minimize biases in identifying patients who were newly diagnosed with CIDP and/or patients who received previous treatment for CIDP, hence the use of the term “newly diagnosed,” which refers solely to the first observed ICD-9-CM diagnosis code for CIDP, with a 12-month diagnosis-free period before that first claim. Because we had no access to patient records, there was no clinician or patient confirmation on the accuracy of this diagnosis.
Study Parameters
The study cohort was characterized using baseline demographics of age, sex, region of the United States, and Charlson Comorbidity Index (CCI) score. The outcomes were evaluated over the 2-year follow-up period and captured the treatments used for CIDP, if any, and the type of resource utilization. The treatment patterns were described as the time to treatment initiation, which was calculated as the median number of months between the index diagnosis date and start of that specific therapy, and the duration of treatment, defined as the median number of months between the first and last administration of that treatment, by treatment type. For example, patients with evidence of having received an IVIG would have their length of IVIG therapy calculated from the first administration of the index IVIG to the last administration of any IVIG. The median CIDP-specific costs were defined as the cost of all medical claims during the 2-year follow-up period with a primary diagnosis of CIDP and all costs associated with treatments for CIDP.
All the data are presented descriptively using percentages for categorical variables and means with standard deviations (SDs) for continuous variables. All analyses were conducted using SAS version 9.3 (SAS Institute Inc; Cary, NC).
Results
A total of 525 patients met all the study inclusion criteria (Table 1). The patients’ baseline demographic and clinical characteristics are shown in Table 2. Patients with a new CIDP code had a mean age of 56.1 years (SD, 13.5 years), were predominantly male (57.9%), largely from the Southern US region (41.1%; which reflects the larger population size within this US Census region), and had a mean CCI score of 1.4 (SD, 1.8).
Table 2.
Patient Demographic and Clinical Characteristics
| Characteristics | Overall sample (N = 525) |
|---|---|
| Age, mean (SD), yrs | 56.1 (13.5) |
| Male, N (%) | 304 (57.9) |
| US region | |
| East, N (%) | 145 (27.6) |
| Midwest, N (%) | 131 (25.0) |
| South, N (%) | 216 (41.1) |
| West, N (%) | 33 (6.3) |
| Charlson Comorbidity Index, mean (SD) | 1.4 (1.8) |
SD indicates standard deviation.
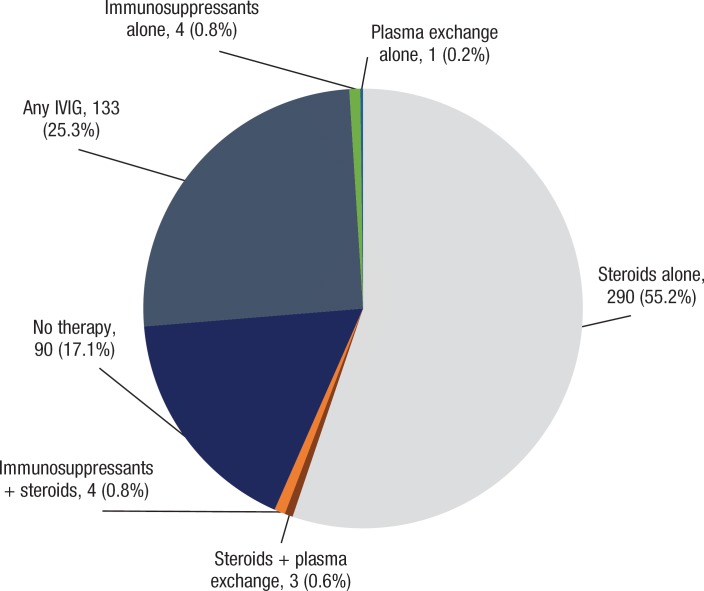
The distribution of index therapies within 2 years of the index diagnosis date are shown in Figure 1. A total of 17.1% of the patients had evidence of active surveillance, because they did not receive any therapy within 2 years of their reported 2 CIDP diagnoses. In the 2-year follow-up period, 55.2% of the patients with a new diagnosis code for CIDP were prescribed steroid therapy alone, and 25.3% of the patients were prescribed an IVIG therapy, which reflected the patient cohort with the lowest mean CCI score. Patients who were prescribed an IVIG most frequently received IVIG with a steroid (45.9%) or an IVIG alone (45.1%). Immunosuppressive therapies and plasma exchange, either alone or in combination with other treatments for CIDP, were rarely prescribed (Figure 1).
Figure 1. Distribution of Index Therapies within 2 Years of Index Diagnosis Date.
IVIG indicates intravenous immunoglobulin.
Time to Start and Duration of CIDP Therapy
The median length of time (in months) between the first CIDP diagnostic code and the first claim for therapy is shown in Table 3. The time to the start of initial treatment was shortest for patients who received plasma exchange alone or in combination with a steroid (median, 0.03 months), which means the plasma exchange therapy happened on the same date as the index CIDP diagnosis. This treatment was followed by IVIG plus another therapy (median, 0.53 months); IVIG alone (median, 0.71 months); a steroid plus immunosuppressant therapy (median, 2.02 months); immunosuppressant therapy alone (median, 4.18 months); and steroid use alone (median, 6.51 months).
Table 3.
Median Number of Months Between CIDP Diagnosis and Receipt of Therapy, and Median Number of Months Receiving Therapy
| Study cohorts | ||||||||
|---|---|---|---|---|---|---|---|---|
| IVIG with/without another CIDP treatmenta (N = 133) | IVIG alone (N = 60) | IVIG + another CIDP treatmenta (N = 73) | Steroid alone (N = 290) | Steroid + plasma exchange (N = 3) | Steroid + immunosuppressant (N = 4) | Immunosuppressant alone (N = 4) | Plasma exchange alone (N = 1) | |
| Median number of months between CIDP diagnosis and treatment | ||||||||
| Receipt of first treatment | ||||||||
| Treatment with any of the therapies below (using the product that was received first) | 0.53 | 0.71 | 0.53 | 6.51 | 0.03 | 2.02 | 4.18 | 0.03 |
| IVIG | 0.69 | 0.71 | 0.66 | – | – | – | – | – |
| Steroid | 5.01 | – | 5.01 | 6.51 | 0.46 | 7.21 | – | – |
| Immunosuppressant | 4.45 | – | 4.45 | – | – | 3.06 | 4.18 | – |
| Plasma exchange | 10.5 | – | 10.50 | – | 0.03 | – | – | 0.03 |
| Median number of months receiving treatmentb | ||||||||
| IVIG | 9.79 | 9.04 | 9.82 | – | – | – | – | – |
| Steroid | 3.77 | – | 3.77 | 1.87 | 21.82 | 5.69 | – | – |
| Immunosuppressant | 4.36 | – | 4.36 | – | – | 10.10 | 6.81 | – |
| Plasma exchange | 3.45 | – | 3.45 | – | 0.69 | – | – | 0.03 |
Steroid and/or immunosuppressant and/or plasma exchange.
Calculated from first administration/prescription fill date to the last administration/prescription end date for any medication in the class.
CIDP indicates chronic inflammatory demyelinating polyneuropathy; IVIG, intravenous immunoglobulin.
The median length of time (in months) on therapy is shown in Table 3. The median length of therapy was longest for the steroid plus plasma exchange cohort (21.82 months; N = 3), followed by the steroid plus immunosuppressant cohort (10.1 months; N = 4) and the 2 IVIG cohorts (9.04 months-9.82 months for IVIG alone and IVIG in combination, respectively). The median number of months receiving the index therapy was shortest for the steroid-only cohort at 1.9 months. In cohorts where steroids and immunosuppressive drugs and/or IVIG were used, the median length of steroid use increased.
Given that the initiation of steroid therapy was longer for the other therapies, and the duration of therapy was shorter for patients receiving steroids, an ad hoc assessment was conducted to further characterize the nature of steroid use in the steroid-only cohort. We examined the longest duration of continuous steroid therapy, which was defined as steroid use without a gap of ≥0 days. The median duration of continuous steroid therapy was 6 days, with 76.6% of the steroid-only cohort having continuous steroid therapy for 1 to 29 days; 10% had 30 to 59 days of continuous steroid therapy; 4.1% had 60 to 89 days of continuous steroid therapy; 7.2% had 90 to 360 days of continuous steroid therapy, and 2.1% had >360 days of continuous steroid therapy.
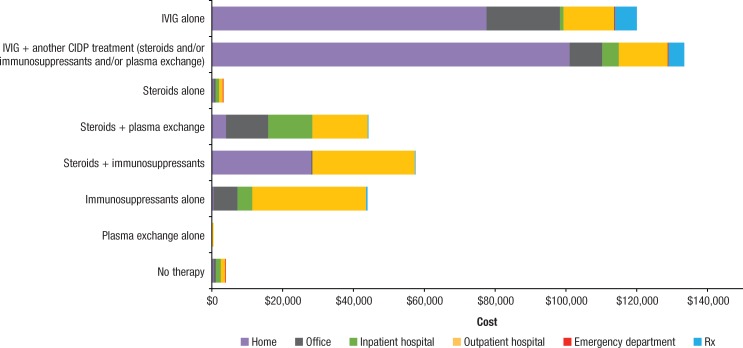
Costs
The mean total CIDP-specific 2-year follow-up cost was highest for the cohort that received IVIG with an additional therapy (mean, $133,334) and lowest for patients who had active surveillance ($3723) or those who received steroids alone ($3101; Figure 2). When costs by site of care were investigated, the majority of IVIG infusion costs were found to be in the home rather than in the clinic or hospital setting. However, costs for other CIDP treatments were more equally distributed throughout other sites of care.
Figure 2. Mean Disease-Specific Costs by Cohort, 2 Years Postindex.
CIDP indicates chronic inflammatory demyelinating polyneuropathy; IVIG, intravenous immunoglobulin.
Discussion
To our knowledge, this US retrospective database study is one of the first to examine treatment patterns and disease-related costs among patients with CIDP who were initiating treatment in a real-world setting. We identified only 1 previous study that examined resource utilization and costs in a small sample of patients with CIDP across 9 US commercial health plans.17 Our study indicated that over a 2-year follow-up period, 55.2% of patients with a new diagnosis code for CIDP were prescribed steroid therapy alone and 25.3% of patients were prescribed an IVIG therapy (alone or in combination). When therapies were used in combination, immunotherapy was the last treatment added to the regimen. This is consistent with clinical practice and with guidelines that suggest that immunosuppressive drugs may be used when first-line therapies (ie, steroids, IVIG, or plasma exchange) are not effective and/or tolerable; to date, there is low-quality evidence for the clinical benefit of immunosuppressive agents in the treatment of patients with CIDP.1,5
Our findings about IVIG use were similar to the results from Guptill and colleagues, who indicated IVIG use in 26% of patients.17 However, Guptill and colleagues showed that steroids, primarily prednisone, were used in only 16% of patients with CIDP.17 Steroids may be used in shorter bursts in an effort to minimize the risk for steroid-related complications associated with prolonged therapy (eg, osteoporosis). Accordingly, the differences in rates observed in our study could have resulted from the longer follow-up in our study, as well as a reflection of lower disease severity of the CIDP (eg, a trial of steroids to gauge a response), uncertainty regarding the diagnosis of CIDP, or hesitancy to commit patients to more costly treatments.
Even with our sensitivity analysis, diagnostic inaccuracies associated with CIDP are likely confounding this cohort. A recent retrospective study examined the diagnostic and treatment information from the records of 59 consecutive patients who were referred to the study investigators with a diagnosis of CIDP to understand the extent of misdiagnosis of CIDP and the contributing factors.7 The study investigators used the EFNS/PNS diagnostic criteria to determine a diagnosis of CIDP. The investigators found that 47% of the patients referred with a diagnosis of CIDP did not meet the minimal EFNS/PNS criteria for a diagnosis. Misdiagnosis can be attributed to a number of factors, including misunderstanding the clinical hallmarks of CIDP, the misinterpretation of electrophysiologic studies, overreliance on mild or moderate cerebrospinal fluid protein elevations, or failure to define objective responses to treatment. Future research will be needed to confirm results in clinically confirmed patients with mild versus moderate or severe CIDP.
Our study also found evidence of a diagnosis of CIDP without subsequent treatment in almost 20% of patients. In clinical practice, the severity of disease may dictate treatment,18 and the patterns seen here could support that. We could be witnessing physicians being good stewards of the treatments available for CIDP, reserving plasma exchange for the patients with the most severe disease, IVIG for patients with moderate-to-less-severe disease, steroids for patients with mild severity CIDP, and a watch-and-wait regimen for the patients with very mild severity CIDP. However, it is possible that these cases may also represent diagnostic uncertainty, which highlights the need for better diagnostic approaches to CIDP and immune-mediated neuropathies.
In addition, in our study, patients generally received plasma exchange and IVIG either at the time of diagnosis or within the first month after diagnosis, which suggests that these patients may have presented with severe symptoms requiring a fast onset of therapeutic action. On average, the time to treatment for steroids and immunosuppressant therapy averaged more than 4 months postdiagnosis. In addition, the patients who received treatment with IVIG continued therapy for longer than patients using steroids alone. This may reflect the differences in the time to disease recurrence after weaning of the different treatments, because patients who have been successfully treated with steroids have the longest time to CIDP relapse, IVIG has a more median time, and plasma exchange a much shorter time to relapse.10,19 Delays and discontinuation in treatment for specific therapies could also reflect physician reservation about the diagnosis, as well as the safety and efficacy of treatment options.
A key aspect of this study was to highlight the costs associated with CIDP-related care. Despite the potential for the misclassification of a diagnosis of CIDP, the study highlights the costs incurred by healthcare plans for patients identified as having CIDP. The mean total costs for patients receiving treatment for CIDP were highest for IVIG therapy, ranging from $111,406 and $117,233 over the 2-year period. The patients who received steroids alone or who were classified as having active surveillance incurred much lower costs, less than $4000 annually. Again, this may indicate that physicians are reserving the more costly treatment for patients with more severe CIDP and the less costly treatment for patients with less severe CIDP.
When the costs were evaluated by site of care, home infusion visits were a primary site of care in CIDP-specific costs for the patients receiving IVIG. Home infusions are generally safe, effective, convenient, and less costly than infusions in other sites of care (eg, physician office, outpatient hospital), making this a frequently used site of care for infusions, either by choice or through health plan benefit design.20,21 In their study, Guptill and colleagues found that 72% of IVIG infusions were administered in the home setting.17
Our findings fill an important evidentiary gap in terms of how patients with an ICD-9-CM diagnosis code for CIDP are being treated in the United States and their associated costs. When the use of steroids for less than 30 days was not considered active treatment and was considered for uses other than the treatment of CIDP, IVIG was used more frequently for long-term therapy and bore a higher cost burden to payers, and home infusion visits were the primary site of care for patients with CIDP.
Limitations
Some important study limitations must be noted. The use of administrative claims in a retrospective study is limited by a lack of data on patients’ clinical presentation, diagnostic information, and severity of disease, which may provide important insights into the selection of particular therapies.
Claims data are collected for the purpose of billing and reimbursement, not research. Therefore, the diagnoses may be coded incorrectly or undercoded, which could introduce measurement error and selection bias. Although the age and sex of our cohort generally reflect the epidemiology of patients with CIDP,4 there is variability in the clinical presentation of CIDP and the various diagnostic criteria. Therefore, it is possible that patients with inflammatory neuropathies other than CIDP were included in the sample.
Finally, the results of this study are generalizable to a commercially insured population of patients with CIDP in the United States and may not reflect treatment patterns and disease-related economic consequences outside of this studied population. Further research is needed to confirm the results of this study in commercially insured and Medicare populations. Ideally, a study design where a diagnosis of CIDP could be confirmed and clinical outcomes were assessed would further our knowledge of the treatment of CIDP in the United States. Based on the results of our study, the further exploration of steroid use patterns is also warranted, as we would have expected a pattern of continuous use in a true CIDP population.
Conclusions
Despite the study limitations, the findings presented in this study provide important insights into the treatment and health plan costs of patients with an ICD-9-CM diagnosis of CIDP in the United States, which to date, have been extremely limited. This study is among the first to examine the treatment patterns and CIDP-related healthcare costs in newly diagnosed patients with CIDP based on real-world claims data. The sole use of steroids was the most common treatment prescribed, but patterns of less than 30 days of use may reflect an active surveillance population, misdiagnosis during follow-up, or the use of steroids in short bursts to minimize complications. When we limited our analysis to more typical corticosteroid patterns for CIDP, IVIG is used more frequently and bears a higher cost burden to payers.
We also saw a longer-than-expected time to steroid initiation and a shorter-than-expected duration of treatment. From a clinical perspective, the type of patients who received short-duration therapy and the delay of treatment initiation after an initial diagnosis were unexpected and may reflect diagnostic uncertainty, disease severity, or the side-effect profile associated with steroids. Further research is needed to explore the rationale for treatment decision-making and to replicate the findings from this study in a population with clinically confirmed CIDP.
Funding Source
This study was funded by Grifols SSNA.
Author Disclosure Statement
Dr Guptill received a grant unrelated to this article from the Grifols Foundation and was an investigator on a clinical trial of IVIG in myasthenia gravis sponsored by Grifols; Dr Runken is an employee of Grifols; Dr Eaddy, Dr Lunacsek, and Ms Fuldeore are employees of Xcenda, which received funding from Grifols for their consulting on this article.
Contributor Information
Jeffrey T. Guptill, Associate Professor of Neurology, Duke Clinical Research Institute, Duke University, Durham, NC.
M. Chris Runken, Senior Director Global HEOR, Grifols SSNA, Research Triangle Park, NC.
Michael Eaddy, Vice President, Scientific Consulting, Xcenda, Palm Harbor, FL.
Orsolya Lunacsek, Director, Scientific Consulting, Xcenda.
Rupali M. Fuldeore, Manager, Scientific Consulting, Xcenda.
References
- 1. Gorson KC. An update on the management of chronic inflammatory demyelinating polyneuropathy. Ther Adv Neurol Disord. 2012;5:359–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Köller H, Kieseier BC, Jander S, Hartung HP. Chronic inflammatory demyelinating polyneuropathy. N Engl J Med. 2005;352:1343–1356. [DOI] [PubMed] [Google Scholar]
- 3. Ripellino P, Fleetwood T, Cantello R, Comi C. Treatment of chronic inflammatory demyelinating polyneuropathy: from molecular bases to practical considerations. Autoimmune Dis. 2014;2014:201657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Laughlin RS, Dyck PJ, Melton LJ, III, et al. Incidence and prevalence of CIDP and the association of diabetes mellitus. Neurology. 2009;73:39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Van den Bergh PYK, Hadden RDM, Bouche P, et al. European Federation of Neurological Societies/Peripheral Nerve Society Guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society—first revision. Eur J Neurol. 2010;17:356–363. Erratum in: Eur J Neurol. 2011;18:796. [DOI] [PubMed] [Google Scholar]
- 6. Ad Hoc Subcommittee of the American Academy of Neurology AIDS Task Force. Research criteria for diagnosis of chronic inflammatory demyelinating polyneuropathy (CIDP): report from an ad hoc subcommittee of the American Academy of Neurology AIDS Task Force. Neurology. 1991;41:617–618. [PubMed] [Google Scholar]
- 7. Allen JA, Lewis RA. CIDP diagnostic pitfalls and perception of treatment benefit. Neurology. 2015;85:498–504. [DOI] [PubMed] [Google Scholar]
- 8. Hughes RAC, Donofrio P, Bril V, et al; for the ICE study group. Intravenous immune globulin (10% caprylate-chromatography purified) for the treatment of chronic inflammatory demyelinating polyradiculoneuropathy (ICE study): a randomised placebo-controlled trial. Lancet Neurol. 2008;7:136–144. Erratum in: Lancet Neurol. 2008;7:771. [DOI] [PubMed] [Google Scholar]
- 9. van Schaik IN, Bril V, van Geloven N, et al; for the PATH study group. Subcutaneous immunoglobulin for maintenance treatment in chronic inflammatory demyelinating polyneuropathy (PATH): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. 2018;17:35–46. Errata in: Lancet Neurol. 2018;17:26; Lancet Neurol. 2018;17:661. [DOI] [PubMed] [Google Scholar]
- 10. Rajabally YA. Long-term immunoglobulin therapy for chronic inflammatory demyelinating polyradiculoneuropathy. Muscle Nerve. 2015;51:657–661. [DOI] [PubMed] [Google Scholar]
- 11. Dyck PJB, Tracy JA. History, diagnosis, and management of chronic inflammatory demyelinating polyradiculoneuropathy. Mayo Clin Proc. 2018;93:777–793. [DOI] [PubMed] [Google Scholar]
- 12. Mehndiratta MM, Hughes RAC, Pritchard J. Plasma exchange for chronic inflammatory demyelinating polyradiculoneuropathy. Cochrane Database Syst Rev. August 2015:CD003906. [DOI] [PMC free article] [PubMed]
- 13. Cortese I, Chaudhry V, So YT, et al. Evidence-based guideline update: plasmapheresis in neurologic disorders: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2011;76:294–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hahn AF, Bolton CF, Zochodne D, Feasby TE. Intravenous immunoglobulin treatment in chronic inflammatory demyelinating polyneuropathy. A double-blind, placebo-controlled, cross-over study. Brain. 1996;119:1067–1077. [DOI] [PubMed] [Google Scholar]
- 15. Mendell JR, Barohn RJ, Freimer ML, et al. Randomized controlled trial of IVIg in untreated chronic inflammatory demyelinating polyradiculoneuropathy. Neurology. 2001;56:445–449. [DOI] [PubMed] [Google Scholar]
- 16. Patwa HS, Chaudhry V, Katzberg H, et al. Evidence-based guideline: intravenous immunoglobulin in the treatment of neuromuscular disorders: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2012;78:1009–1015. [DOI] [PubMed] [Google Scholar]
- 17. Guptill JT, Bromberg MB, Zhu L, et al. Patient demographics and health plan paid costs in chronic inflammatory demyelinating polyneuropathy. Muscle Nerve. 2014;50:47–51. [DOI] [PubMed] [Google Scholar]
- 18. Oaklander AL, Lunn MPT, Hughes RAC, et al. Treatments for chronic inflammatory demyelinating polyradiculoneuropathy (CIDP): an overview of systematic reviews. Cochrane Database Syst Rev. January 2017:CD010369. [DOI] [PMC free article] [PubMed]
- 19. Nobile-Orazio E, Cocito D, Jann S, et al; for the IMC trial group. Frequency and time to relapse after discontinuing 6-month therapy with IVIg or pulsed methylprednisolone in CIDP. J Neurol Neurosurg Psychiatry. 2015;86:729–734. [DOI] [PubMed] [Google Scholar]
- 20. Le Masson G, Solé G, Desnuelle C, et al. Home versus hospital immunoglobulin treatment for autoimmune neuropathies: a cost minimization analysis. Brain Behav. 2018;8:e00923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Polinski JM, Kowal MK, Gagnon M, et al. Home infusion: safe, clinically effective, patient preferred, and cost saving. Healthc (Amst). 2017;5:68–80. [DOI] [PubMed] [Google Scholar]