Introduction
Preference-based summary scores of health are useful for tracking population health, comparing groups, and performing cost-effectiveness analyses [1]. Preference-based scoring functions are estimated by having individuals value a set of health-state descriptions. Valuation procedures include standard gamble, time trade-off, and visual analog scales [2–4].
The health-state descriptive space used for preference-based measures has consisted of a fixed set of health domains and levels for each domain [5–10]. For example, the EuroQol-5D-3L has 5 health domains: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression, with 3 levels on each (no problems, some problems, extreme problems) [5].
In the last decade, there have been significant advancements in health-state description systems. The Patient-Reported Outcomes Measurement Information System (PROMIS®) is a major effort sponsored by the National Institutes of Health to advance measuring health through state-of-the-science qualitative and quantitative methods [11,12]. In particular, PROMIS utilizes item response theory (IRT) [13] to create unidimensional item banks for health domains (e.g., pain, physical function) calibrated on a common metric. Any set of items selected from the item bank can be used to estimate an individual’s score (“theta”) for a domain. The PROMIS domains are usually reported as a T-scores which are constructed with a mean of 50 and standard deviation of 10 relative to a target population (e.g., the U.S. general population).
Leveraging the improvements in health descriptive systems has the potential to improve preference-based measurement. However, because item banks comprise a large number of items, one can imagine many permutations and combinations of items that could be combined into a health state description for valuation. Bookmarking methods and scale judgement methods, which build descriptive vignettes from 5 items, have recently been used to create PROMIS item bank health-state descriptions for minimally important difference studies and establishing clinically relevant classifications [14,15]. Here, we describe and evaluate 4 different methods for presenting health state descriptions from the PROMIS item banks for use in preference valuation. These methods preserve the advantages of IRT by linking the descriptions to the underlying unidimensional construct.
Methods
Creation of health-state descriptions
We selected 3 PROMIS item banks which cover disparate aspect of health: depression [16], physical function [17] and sleep disturbance [18]. Each item in these banks has 5 possible response options (i.e., never, rarely, sometimes, often, or always). We created health-state descriptions from those items through a combination of item calibration data and qualitative analysis by domain experts as described below. We evaluated 4 different approaches: a single item (1S), 2 items presented separately (2S), 2 items presented together (2T), and 5 items presented together (5T).
Selection of the items used for the 1S, 2S, and 2T sets started by examining the theta estimate for each response category for each item in each domain, such as would be produced if only those responses were used to estimate theta. For example, the depression item bank has the item, “I felt sad … never, rarely, sometimes, often, or always.” The associated theta estimates for the five possible responses are −0.96, −0.03, 0.67, 1.38, and 2.08.
The depression item bank was Emotional Distress – Depression v1.0. Parameter estimates were from the PROMIS Wave 1 sample. The physical function item bank was Physical Function v1.2. Parameter estimates were from PROMIS 1 Wave 1 with Extension sample. The sleep disturbance item bank was Sleep Disturbance v1.0. The parameter estimates were from PROMIS Sleep Wave 1. [see http://www.healthmeasures.net/index.php and https://www.assessmentcenter.net]
To select a single item for the 1S method, we presented the 5 items with the largest range to domain experts who then selected the most representative item. For the 2S and 2T methods, we wanted to capture a wide range of domain scores. We selected a set of 5 items which, based on the IRT parameters, best covered the highest range of the target concept (i.e., physical function) and selected 5 items which, based on the IRT parameters, best covered the lowest range of the concept. These 10 items were then presented to domain experts who picked 1 item from the highest set and 1 item from the lowest set which they felt captured the important aspects of the domain. For depression, those aspects were mood and anhedonia. For physical function, they were mobility and dexterity. For sleep disturbance, they were sleep restfulness and duration.
Domain experts were asked to avoid items which shared content with other domains. For example, one of the items with the highest theta estimates in the sleep disturbance item bank is “I felt sad at bedtime …” This item was not considered because it may have content overlap with depression.
All descriptions used in the valuations are included in online Appendix A. In the 1S method, each response to the selected item was presented separately for a total of 5 descriptions. In the 2S method, each item response was presented separately; because each item has 5 response options, there was a total of 10 descriptions. In the 2T method, the 2 items were presented together. Item parameter information was used to create the most likely response combinations for a total of 9 descriptions. Creation of the 5T descriptions followed the procedure outlined by Cook and colleagues [14] where a theta score is selected and then a representative set of 5 items and their responses at that theta score are selected. We created 5T descriptions at increments of 0.5 on the theta score. There were 8 depression descriptions, 9 physical function descriptions, and 9 sleep disturbance descriptions.
Community Sample
We recruited 118 adults from metropolitan Pittsburgh, Pennsylvania using the Clinical and Translational Science Institute’s Research Participant Registry [https://researchrecruitment.pitt.edu/ctsi/home/about] to participate in a video-recorded, in-person interview at a research office. Participants responded to an advertisement on the registry’s website. Inclusion criteria were age 18 years or older and to be comfortable communicating in English. There were no other inclusion or exclusion criteria. Participants were paid $35.
Evaluation Procedure
We assigned participants to evaluate a single health domain from the 3 domains. The first 40 participants completed depression, the next 40 completed sleep disturbance, and the last 38 completed physical function. Participants first completed the 8-item short form of the domain to familiarize themselves with the concept. The health descriptions for each of the 4 methods were printed on individual cards (e.g., 4 “card sets”). Then they evaluated each of the 4 card sets in random order. They first ranked the cards from best to worst. Second, the best and worst cards were used as anchors on a 0–100 visual analog scale and respondents were asked to place the other cards on the scale. Third, respondents evaluated the cards using the standard gamble on a chance board. In the standard gamble, their best and worst cards were used as the best and worst outcomes, with the others as intermediate outcomes [6,7]. Respondents assessed each card set’s difficulty by using a 7-category response scale (1 = very easy to 7 = very hard).
After completing all 4 card sets, respondents completed a self-administered questionnaire with demographic information, the subjective numeracy scale [19], the Iron-Wood religiosity scale [20], self-rated health, number of physician visits per year, number of times hospitalized, and experience with conditions that limit a person’s ability to take care of him or herself. Finally, respondents were asked questions about the meaningfulness and realism of the cards in semi-structured exit interviews.
Analyses
We compared the results from the 4 methods in several ways. First, we examined the range of item bank theta scores captured. Second, we compared the monotonicity of mean valuations across the methods; monotonicity was considered violated if the rank order of health-states by valuation was different at least twice from the rank order of health-states by theta. Third, we compared the methods by participant assessments of difficulty on the 7-point response scale. Fourth, we evaluated participant reports from the semi-structured exit interviews.
Results
We recruited 118 participants. The mean age of the sample was 37 (SD=16, range 18 – 71); 63% were female; and 54% were white and 34% were African-American (Table 1). The sample included a range of educational backgrounds, experience with the domain to which they were assigned, and experience with other health problems that limit a person’s ability to take care of him or herself. Thirty percent of participants reported their health as excellent whereas 48% reported their health as very good, 19% as good, 3% as fair, and 0% as poor. The in-person interview took an average of 44 minutes.
Table 1:
Sample Demographics
| Depression | Physical Function | Sleep Disturbance | Combined Sample | |
|---|---|---|---|---|
| N | 40 | 40 | 38 | 118 |
| Age mean | 42.5 | 32.0 | 35.4 | 36.7 |
| Age range | 20–71 | 18–69 | 19–68 | 18–71 |
| Female | 60.0% | 60.0% | 68.4% | 62.7% |
| Domain limitation experience, personal | 40.0% | 35.0% | 21.0% | 32.2% |
| Domain limitation experience, caregiver | 7.5% | 5.0% | 2.6% | 5.1% |
| Domain limitation experience, family | 50.0% | 72.5% | 47.4% | 56.8% |
| Domain limitation experience, work | 10.0% | 15.0% | 13.1% | 12.7% |
| General limitation experience, personal | 22.5% | 22.5% | 13.1% | 19.5% |
| General limitation experience, caregiver | 25% | 20.0% | 13.1% | 19.5% |
| General limitation experience, family | 62.5% | 80.0% | 50.0% | 64.4% |
| General limitation experience, work | 17.5% | 25.0% | 10.5% | 17.8% |
| Doctor visits per year (range) | 0–20 | 0–15 | 1–12 | 0–20 |
| Ever hospitalized | 57.5% | 52.5% | 50.0% | 53.4% |
| Race | ||||
| White | 50.0% | 47.5% | 63.2% | 53.5% |
| Black | 40.0% | 35.0% | 26.3% | 33.9% |
| Asian | 0% | 7.5% | 2.6% | 3.4% |
| Other | 7.5% | 7.5% | 5.3% | 6.9% |
| Hispanic | 5.0% | 2.5% | 2.6% | 3.4% |
| Education | ||||
| High school | 20.0% | 7.5% | 10.5% | 12.7% |
| Some college | 30.0% | 60.0% | 31.6% | 40.7% |
| College | 15.0% | 20.0% | 21.1% | 18.6% |
| Some post-graduate | 15.0% | 7.5% | 10.5% | 11.0% |
| Post-graduate | 20.0% | 5.0% | 26.3% | 16.7% |
| Self-rated health | ||||
| Excellent | 27.5% | 27.5% | 34.2% | 30.0% |
| Very good | 40.0% | 50.0% | 55.3% | 48.3% |
| Good | 27.5% | 17.5% | 10.5% | 18.6% |
| Fair | 5.0% | 5.0% | 0% | 3.4% |
| Poor | 0% | 0% | 0% | 0% |
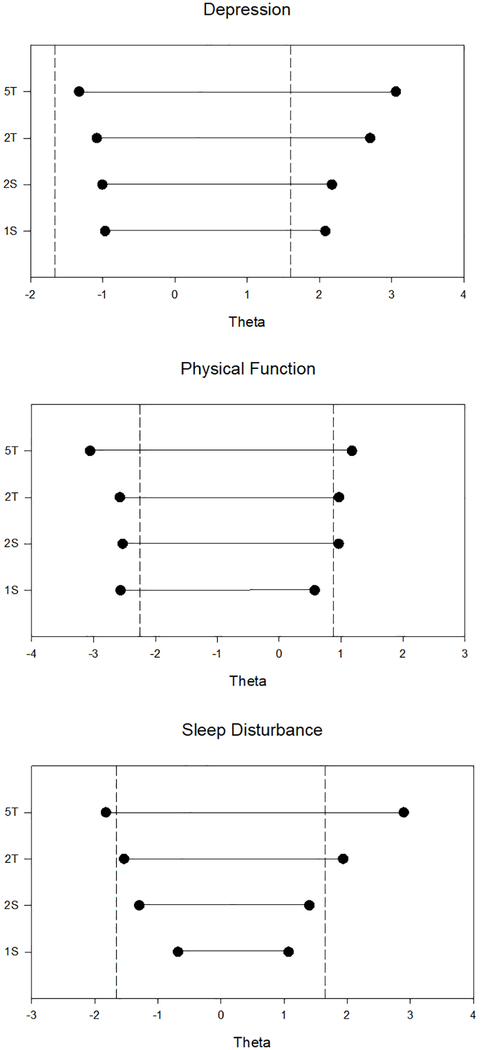
As seen in Figure 1, the 1S method had the narrowest range of theta scores for each domain. The 5T method always had the widest range and the 2T method had the second widest range. The figure includes dashed lines to indicate the 5th and 95th percentile scores for the item bank’s calibration sample [21–23]. Though these samples are not perfectly representative of the U.S. general population [24], they provide an indicator of the distribution of scores in the general population.
Figure 1:
Range of item bank theta scores captured by each method. IS is a single item, 2S is two items presented separately, 2T is two items presented together, and 5T is five items presented together.
Vertical dashed lines represent the area of theta that captures 90% of the item bank calibration sample.
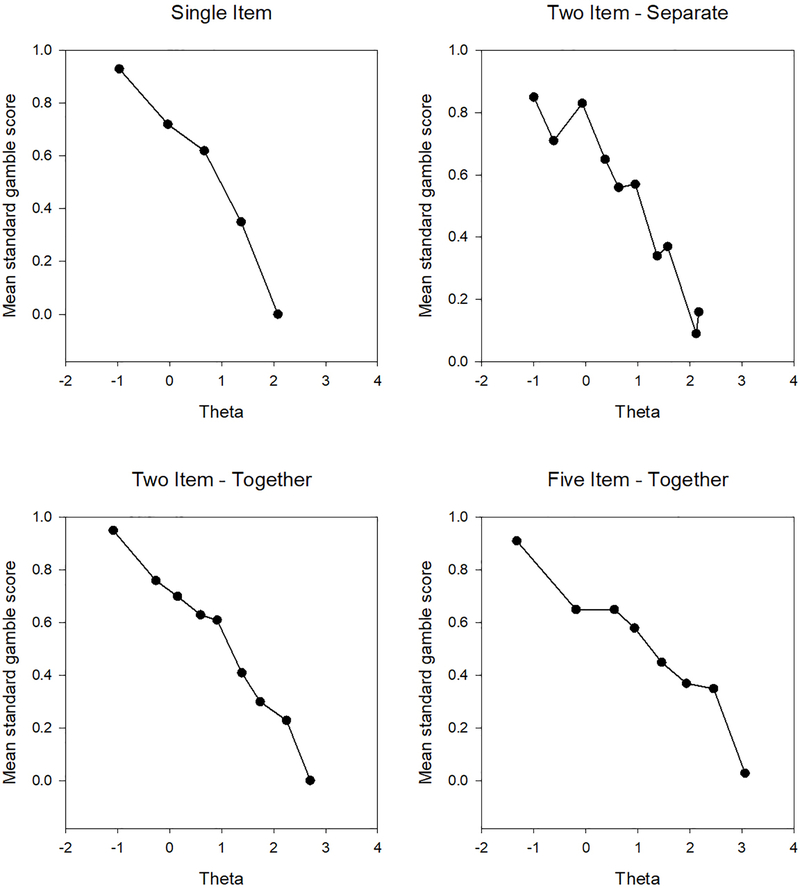
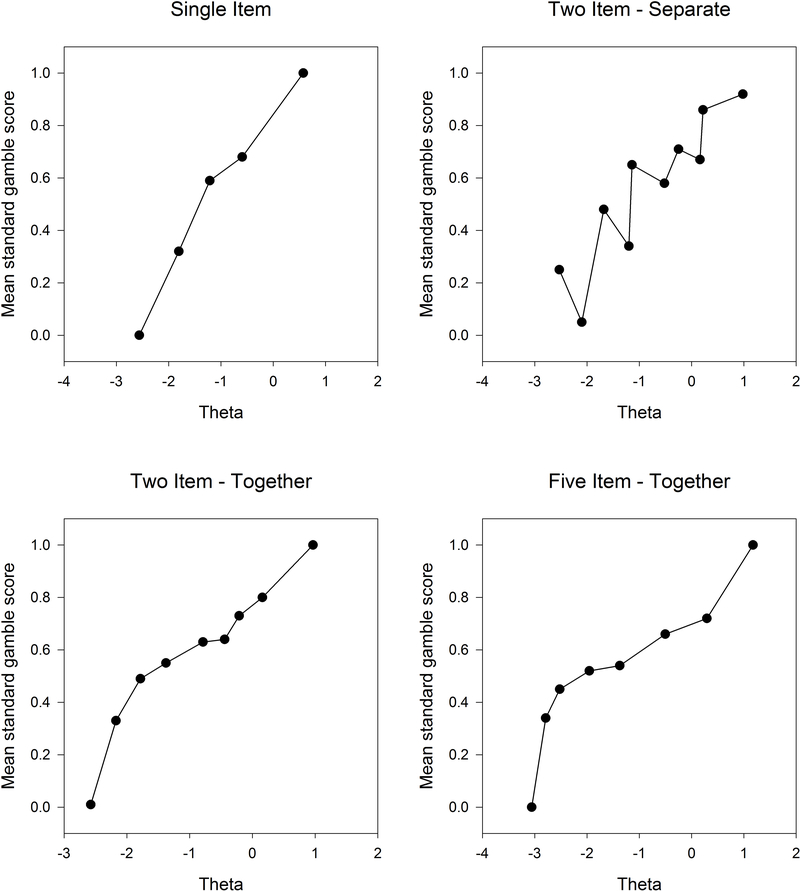
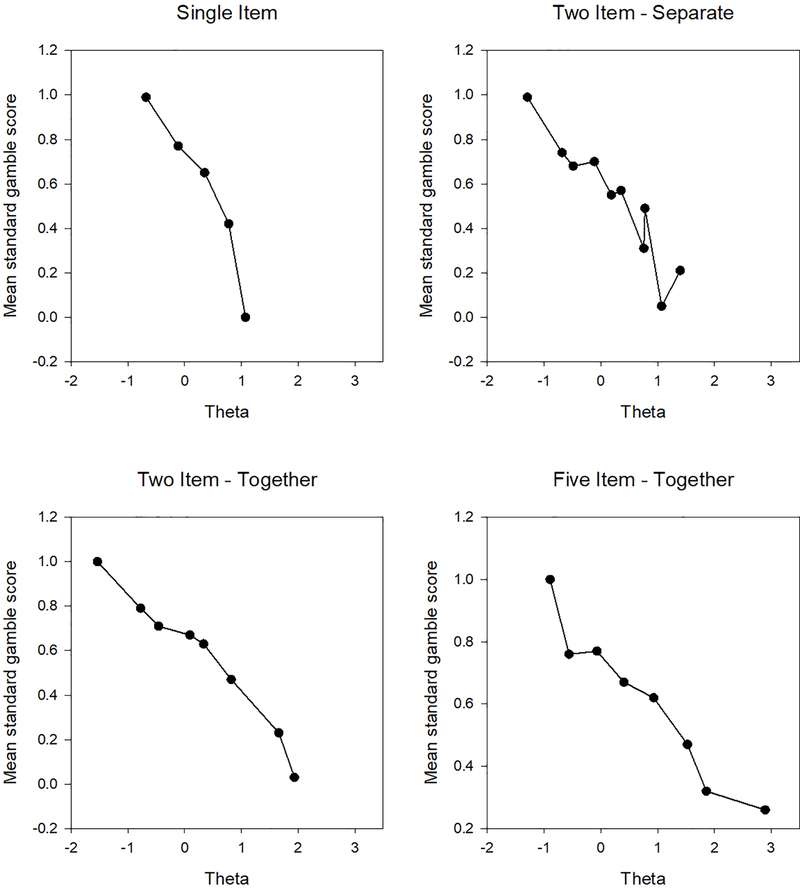
There was a monotonic relationship between item bank theta estimate and mean standard gamble estimate was found for the 1S, 2T, and 5T methods in all 3 domains (Figure 2a, 2b, 2c). With the 2S method, mean standard gamble estimates trended with theta scores, but monotonicity was violated several times. Figure 2a illustrates the results for the depression item bank, 2b for physical function, and 2c for sleep disturbance.
Figure 2a).
Mean standard gamble scores for each presentation method in the Depression item bank.
Figure 2b).
Mean standard gamble scores for each presentation method in the Physical Function item bank.
Figure 2c).
Mean standard gamble scores for each presentation method in the Sleep Disturbance item bank.
Across all 3 item banks, 74% of participants found 1S to be easiest and 71% found 5T to be most difficult. Mean difficulty assessments for the combined sample on the 7-point response scale were 2.25 (1S), 3.04 (2T), 3.25 (5T), and 3.34 (2S). The rank order of difficulty was the same in each domain.
In exit interviews, participants generally reported all 4 methods to be similarly meaningful and realistic. Most participants reported that the 5T method provided too much information; a notable exception was a participant who had personal experience with the item bank she was evaluating (depression) and found the rich descriptions helpful. Participants reported that the 1S method was easiest, but that the 2T method was still manageable. Many participants found the 2S method frustrating, as they had difficulty comparing single responses from different items.
Overall, participants were generally engaged in the task and expressed thoughtful reasoning about their responses. For example, a small subset of participants found the best (by theta) depression health-states to be “unnatural” saying that rarely feeling sad was preferable to never feeling sad.
Discussion
The construction of health-states for valuation studies requires a careful balance between descriptive richness in content and respondent burden. Historically, the health-states used in valuation studies have either been created de novo by instrument developers (HUI, EQ-5D) or taken from an existing static health descriptive system (SF-6D, FACT) [5–10,25]. Item response theory has modernized health descriptive systems by calibrating items on underlying constructs; from such item banks, a small set of informative items can be used to measure the construct. We have developed a method to present an item bank for valuation. This method uses the advantages of item response theory, particularly knowledge about an item’s location on the underlying construct, to improve the descriptive system for a preference-based scoring system [26].
Based on responses to these methods, we recommend approach 2T: select 2 representative items from an item bank and present them together. We compared 2T with 3 other methods: using a single item (1S), using 2 items separately (2S), and using 5 items together (5T). While evaluating a single item (1T) was easiest for participants, this method captured significantly less of the item bank’s range than evaluating 2 items together. As a result, using a single item would be more likely to produce ceiling and floor effects. Presenting 2 items separately covers a wider range of the item bank, but was more difficult for our participants, who reporting finding it hard to compare responses to the 2 items, perhaps because we had purposefully chosen ones that capture different aspects of the health domain. Using the same 2 items to create a single health-state was easier for the participants, captured a wide range of the theta distribution, and had a monotonic relationship to standard gamble valuations. Presenting 5 items together also captured a wide range of the item bank and produced monotonic functions. However, participants found it very complex, cognitively burdensome, and unnecessarily detailed.
To ensure that the widest range of the construct is captured, thereby reducing ceiling and floor effects, we recommend that those 2 items have values at each end of the theta distribution. We also recommend not relying solely on measurement properties, but also having experts review the content of the items to ensure that they capture key aspects of the health domain (i.e.,for depression, selecting items to capture both mood and anhedonia). Once the items are selected, the item information can be used to produce likely combinations of responses for valuation tasks. These valuation tasks can be completed by either the general population or subgroups of interest, such as patients with a specific health condition.
This study has several limitations. First, it used a convenience community sample which is not fully representative of the United States; it had 2.5 times as many Black respondents, 1.6 times as many respondents with educational attainment higher than a bachelor’s degree, and one-fifth as many Hispanic respondents as the general US population in the 2010 census. The sample had varying age, race, educational, and health backgrounds from a single city in the United States and we do not believe that the particular geographic area from which participants were sampled would have a significant effect on our findings. Second, we tested 4 distinct methods to present item banks for valuation, but there are certainly other possible methods which we did not consider. Future work may find that an intermediate approach, such as using 3 or 4 items, may be preferable to using 2. We would recommend testing any other approach using the same criteria as this study: the range of item bank scores captured, monotonicity in mean valuations, participant assessments of difficulty, and semi-structured exit interviews with participants. Third, we assume but do not test that the specific items selected from an item bank will have no impact on the valuations; future work should directly test this assumption. It should be noted that the valuations obtained in this study are not intended for applied research; rather, they were meant to test different methodologies. Fourth, we tested the methods with 3 different item banks but have not tested the methods in item banks measuring domains like cognition, pain, or social function.
In conclusion, we have developed an acceptable method to present health-state descriptions for IRT-calibrated item banks. This method uses 2 carefully selected items and presents them in combination. It captures a wide area of the underlying construct, is readily understood by community members, and produces monotonic valuations over the underlying construct. Our recommendation is strengthened by consistent findings in 3 distinct item banks: depression, physical functioning, and sleep disturbance. While the present study used PROMIS as an exemplar, the method can be applied to any descriptive system developed using IRT.
Supplementary Material
Table 2.
Difficulty assessments on a 7-point Likert scale (1 = very easy to 7 = very hard) for each presentation method. IS is a single item, 2S is two items presented separately, 2T is two items presented together, and 5T is five items presented together.
| Depression n=40, mean (SD) | Physical Function n=40, mean (SD) | Sleep Disturbance n=38, mean (SD) | Combined Sample n=118, mean (SD) | |
|---|---|---|---|---|
| 1S | 2.38 (1.35) | 2.03 (1.10) | 2.33 (1.46) | 2.25 (1.31) |
| 2S | 3.25 (1.37) | 3.53 (1.71) | 2.97 (1.35) | 3.25 (1.49) |
| 2T | 3.05 (1.52) | 3.12 (1.64) | 2.94 (1.65) | 3.04 (1.60) |
| 5T | 3.23 (1.44) | 3.45 (1.65) | 3.34 (1.51) | 3.34 (1.53) |
Acknowledgments
Janel Hanmer was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number KL2TR001856. The project was supported by the National Institutes of Health through Grants Number UL1TR000005 and UL1TR001857, and a supplement to the PROMIS statistical center grant 3U54AR057951–04S4. The funding agreements ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Funding: This study was supported by: the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number KL2TR001856; National Institutes of Health through Grants Number UL1TR000005 and UL1TR001857, and a supplement to the PROMIS statistical center grant 3U54AR057951–04S4. The funding agreements ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to report.
Compliance with Ethical Standards:
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. IRB approval for the project was obtained from the University of Pittsburgh (PRO14110193).
Contributor Information
Janel Hanmer, Department of General Internal Medicine, University of Pittsburgh Medical Center, 230 McKee Place, Suite 600, Pittsburgh, PA 15213..
David Cella, Department of Medical Social Sciences, Northwestern University Feinberg School of Medicine, Chicago, Il..
David Feeny, Department of Economics, McMaster University, Hamilton, ON, Canada; Health Utilities Incorporated, Dundas, ON, Canada..
Baruch Fischhoff, Department of Engineering and Public Policy and Institute for Politics and Strategy, Carnegie Mellon University, Pittsburgh, PA..
Ron D. Hays, Division of General Internal Medicine & Health Services Research, UCLA, Los Angeles, CA..
Rachel Hess, Division of Health System Innovation and Research, University of Utah Schools of the Health Sciences, Salt Lake City, UT..
Paul A Pilkonis, Department of Psychiatry, University of Pittsburgh Medical Center, Pittsburgh, PA..
Dennis Revicki, Outcomes Research, Evidera, Bethesda, MD..
Mark Roberts, Department of General Internal Medicine, University of Pittsburgh Medical Center, Pittsburgh, PA and Department of Health Policy and Management, University of Pittsburgh, Pittsburgh, PA..
Joel Tsevat, Division of General Internal Medicine, University of Texas Health Science Center, Department of Medicine, San Antonio, TX..
Lan Yu, Department of General Internal Medicine, University of Pittsburgh Medical Center, Pittsburgh, PA..
References
- 1.McHorney CA (1999). Health status assessment methods for adults: past accomplishments and future challenges. Annual Rev Public Health, 20, 309–35. [DOI] [PubMed] [Google Scholar]
- 2.Torrance, 1986; [Google Scholar]
- 3.Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, & Stoddart GL (2005). Methods for the economic evaluation of health care programmes (3rd ed.). Oxford: Oxford University Press. [Google Scholar]
- 4.Neumann Peter J., Sanders Gillian D., Russell Louise B., Siegel Joanna E., and Ganiats Theodore G., eds., Cost-Effectiveness in Health and Medicine, Second Edition, New York, Oxford University Press, 2016. [Google Scholar]
- 5.Brooks R, Rabin R, de Charro F (2003). The Measurement and Valuation of Health Status Using EQ-5D: A European Perspective. Dordrecht, The Netherlands: Kluwer Academic Publishers. [Google Scholar]
- 6.Feeny D, Furlong W, Torrance GW, et al. (2002). Multiattribute and singleattribute utility functions for the health utilities index mark 3 system. Med Care, 40, 113–128. [DOI] [PubMed] [Google Scholar]
- 7.Feeny D, Torrance G, Furlong W (1996). Health Utilities Index In: Spilker B, ed. Quality of Life and Pharmacoeconomics in Clinical Trials. Philadelphia, PA: Lippincott-Raven Press. [Google Scholar]
- 8.Kaplan RM, Anderson JP. A general health policy model: update and applications. Health Serv Res 1988; 23:203–234. [PMC free article] [PubMed] [Google Scholar]
- 9.Brazier JE, Roberts J (2004). The estimation of a preference-based measure of health from the SF-12. Med Care, 42, 851–859. [DOI] [PubMed] [Google Scholar]
- 10.Brazier J, Roberts J, Deverill M (2002). The estimation of a preference-based measure of health from the SF-36. J Health Econ, 21, 271–292. [DOI] [PubMed] [Google Scholar]
- 11.Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, et al. (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH roadmap cooperative group during its first two years. Med Care, 45 (5), S3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cella D, Riley W, Reeve B, Stone A, Young S, Rothrock N, et al. (2010). Initial item banks and first wave testing of the Patient-Reported Outcomes Measurement Information System (PROMIS) network: 2005–2008. J Clin Epidemiol, 63(11), 1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Embretson SE, Reise SP Item response theory for psychologists. New York, NY, Psychology Press; 2000. [Google Scholar]
- 14.Cook KF, Victorson DE, Cella D, Schalet BD, & Miller D (2015). Creating meaningful cut-scores for Neuro-QOL measures of fatigue, physical functioning, and sleep disturbance using standard setting with patients and providers. Quality of Life Research, 24(3), 575–589. [DOI] [PubMed] [Google Scholar]
- 15.Thissen D, Liu Y, Magnus B, Quinn H, Gipson DS, Dampier C, … & Gross HE (2016). Estimating minimally important difference (MID) in PROMIS pediatric measures using the scale-judgment method. Quality of Life Research, 25(1), 13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, & Cella D (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): depression, anxiety, and anger. Assessment, 18(3), 263–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rose M, Bjorner JB, Gandek B, Bruce B, Fries JF, & Ware JE (2014). The PROMIS Physical Function item bank was calibrated to a standardized metric and shown to improve measurement efficiency. Journal of clinical epidemiology, 67(5), 516–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buysse DJ, Yu L, Moul DE, Germain A, Stover A, Dodds NE, … & Pilkonis PA (2010). Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep, 33(6), 781–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McNaughton CD, Cavanaugh KL, Kripalani S, Rothman RL, & Wallston KA (2015). Validation of a short, 3-item version of the Subjective Numeracy Scale. Medical Decision Making, 35(8), 932–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ironson G, Solomon GF, Balbin EG, O’Cleirigh C, George A, Kumar M, … & Woods TE (2002). The Ironson-Woods Spirituality/Religiousness Index is associated with long survival, health behaviors, less distress, and low cortisol in people with HIV/AIDS. Annals of Behavioral Medicine, 24(1), 34–48. [DOI] [PubMed] [Google Scholar]
- 21.PROMIS Depression Scoring Manual (2015) https://www.assessmentcenter.net/documents/PROMIS%20Depression%20Scoring%20Manual.pdf Accessed August 2017.
- 22.PROMIS Physical Function Scoring Manual (2015) https://www.assessmentcenter.net/documents/PROMIS%20Physical%20Function%20Scoring%20Manual.pdf Accessed August 2017.
- 23.PROMIS Sleep Disturbance Scoring Manual (2015) http://www.healthmeasures.net/images/promis/manuals/PROMIS_Sleep_Disturbance_Scoring_Manual.pdf Accessed August 2017.
- 24.Liu H, Cella D, Gershon R, Shen J, Morales LS, Riley W, & Hays RD (2010). Representativeness of the patient-reported outcomes measurement information system internet panel. Journal of clinical epidemiology, 63(11), 1169–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dobrez D, Cella D, Pickard AS, Lai JS, & Nickolov A (2007). Estimation of patient preference-based utility weights from the functional assessment of cancer therapy—general. Value in Health, 10(4), 266–272. [DOI] [PubMed] [Google Scholar]
- 26.Hanmer J, Feeny D, Fischhoff B, Hays RD, Hess R, Pilkonis PA, … & Yu L (2015). The PROMIS of QALYs. Health and quality of life outcomes, 13(1), 122. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.