Introduction
Filoviruses cause outbreaks associated with 25–90% human lethality (Outbreaks Chronology Ebola virus, https://www.cdc.gov/vhf/ebola/outbreaks/history/chronology.html and Outbreak Table Marburg Virus, https://www.cdc.gov/vhf/marburg/resources/outbreak-table.html). Most outbreaks occurred in sub-Saharan Africa, although the Reston virus (RESTV) species of ebolavirus is native to Asia, and several infected individuals traveled from outbreak zones in Africa to North America and Europe. Due to their lethality and potential for weaponization, filoviruses are classified as both NIAID Category A Priority Pathogens and CDC Category A Agents of Bioterrorism.
The Filovirus family has three genera: Ebolavirus, Marburgvirus, and Cuevavirus. Although the diseases caused by these viruses are clinically similar, ebolaviruses represent the largest global disease burden. Of the six known Ebolavirus species, four are documented to cause severe disease in humans, with Ebola virus (EBOV) (previously known as Zaire ebolavirus) being the most common. The 2014–2016 EBOV outbreak caused over 28,000 infections and over 11,000 deaths [~41% case fatality rate (CFR)] (2014–2016 Ebola virus outbreak in West Africa, https://www.cdc.gov/vhf/ebola/history/2014-2016-outbreak/index.html). Previous EBOV outbreaks have had CFRs of up to 90% [1]. The second most lethal virus is Sudan virus (SUDV), which is associated with a ~50% CFR and has caused at least six outbreaks [2–4]. Bundibugyo virus (BDBV) has emerged twice with ~25–50% CFR [5,6]. Finally, in 1994 a Taï forest virus (TAFV) infection was documented in a single patient, who survived, but this virus has not reemerged [7]. RESTV is thought to be non-pathogenic in humans, but infections in nonhuman primates (NHPs) are lethal [8]. A sixth ebolavirus, Bombali virus (BOMV), was recently discovered based on RNA analysis of free-tailed bats in Sierra Leone [9], although little is known about its potential to infect humans. A related genus Marburgvirus includes the species Marburg virus and Ravn virus, both of which are highly lethal to humans. Since their discovery in 1967, 13 outbreaks of marburgvirus infections have occurred, with CFRs ranging from 23%−90%. The most recent marburgvirus disease outbreak occurred in October 2017, when 5 individuals were infected and 3 died (60% CFR) [10].
Filovirus virions exist as long filaments that are coated with the viral surface glycoprotein termed GP. GP is the only viral protein expressed on the virus surface and mediates host cell attachment and entry. In host producer cells, newly-transcribed GP is post-translationally processed by furin cleavage to yield GP1 and GP2, which remain linked by a single disulfide bond [11]. GP1 bears the receptor-binding subunit, whereas GP2 encodes the fusion machinery [12–15]. Three GP1-GP2 heterodimers associate to form mature GP trimers on the viral surface [16–18].
Initial attachment of filoviruses to target cells is thought to be initiated via interactions between virions and cell surface lectins [19], membrane phosphatidylserine, or TIM-1 proteins [20]. Following internalization by macropinocytosis [21–23], the virion enters the endosome. During maturation, the endosome acidifies, and host cathepsins proteolytically process GP to remove the glycan cap and mucin-like domains from GP1. The remaining processed GP is termed cleaved GP (GPCL) [24]. This processing reveals the receptor binding site (RBS) of the GP protein to allow GPCL to bind domain C of the host receptor Niemann-Pick C1 (NPC1-C) [25–27]. Through a mechanism that remains unclear, binding of GPCL to NPC1-C promotes fusion between target cell and viral membranes to facilitate subsequent entry of the viral genetic material into the target cell cytoplasm. Due to its surface exposure and critical role in viral entry, GP is the main target for immunotherapeutic and vaccine development.
At the C terminus of GP1 lies the glycan cap followed by the heavily glycosylated mucin-like domain (MLD), both of which are positioned on the upper/outer regions of the GP trimer [16]. GP2 contains, in sequential order, an N-terminal peptide (separated from GP1 by furin cleavage), an internal fusion loop (IFL, consisting of the IFLloop, IFLstem, and IFLbase), two heptad repeats (HR1 and HR2), a membrane proximal external region (MPER), and a C-terminal transmembrane domain [17,28]. HR1 wraps around the base of the GP1 receptor-binding core, while HR2 creates a “stalk” that connects the core of GP to the viral membrane [17]. The organization of GPs across ebolaviruses is highly similar, and many portions of the GP are similar between ebolaviruses and marburgviruses [17,29–31]. However, marburgvirus GPs differ in the presence of a marburgvirus-specific “wing” domain and the likely absence of a well-ordered glycan cap [31–33].
Monoclonal antibody (mAb) therapies are currently on the front line of experimental treatments used for filoviruses [34,35]. Some mAb therapies have been shown to confer complete protection to non-human primates (NHPs), even if administered late in the disease course [36–40]. This feature is an important consideration given that the filovirus infection prodrome is virtually identical to common, co-circulating diseases such as typhoid fever and malaria [41], and as a result may be diagnosed later in the disease course. A large number of other anti-GP neutralizing antibodies have been isolated from both human survivors and immunized animals [29,38,39,42–53]. The structures of several of these antibody-GP complexes have been determined, which has allowed categorization of the most commonly recognized epitopes on GP [54,55].
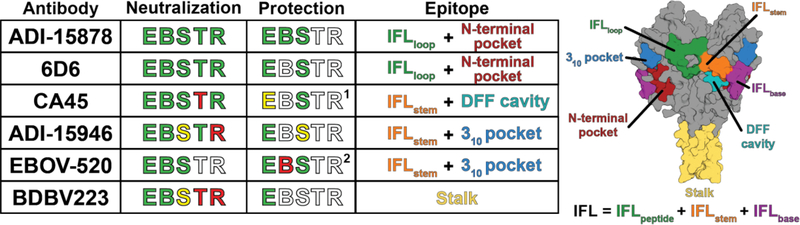
GP antibodies can be grouped into several epitope classes: the GP1 glycan cap, the head/apex of GP1, IFL binders in the “waist” region of GP, the HR2 stalk of GP2, and several linear epitopes within the MLD (Figure 1) [56]. Each epitope class has at least one antibody that offers protection in the EBOV mouse model of infection [38,39,43–45,47,55,56]. Most of these mAbs are specific for EBOV, and about 45% cross-react to only one other filovirus, typically another member of the ebolavirus genus [35]. A rare few neutralize several of the ebolaviruses. No mAbs are known that can neutralize all the filoviruses, ebolaviruses and marburgviruses alike, in their natural, unprocessed forms. Since timing, location and causative virus of any new outbreak are each nearly impossible to predict, antibody therapeutics that are broadly cross-reactive are needed. This review focuses on six currently known antibodies which broadly cross-react among the ebolaviruses: ADI-15946, ADI-15878 [57], EBOV-520 [58], BDBV223 [59], CA45 [60], and 6D6 [61] and discusses the structural features that may confer this broad cross-reactivity.
Figure 1.
Overview of broadly neutralizing ebolavirus antibodies
Antibodies
Four of the six broadly cross-reactive antibodies (ADI-15946, ADI-15878, EBOV-520, and BDBV223) were isolated from human survivors of ebolavirus disease [57–59]. Among these, BDBV223 was isolated from a survivor of Bundibugyo virus infection in 2007, and the other three were from survivors of EBOV infection in the 2014–2016 outbreak (ADI-15946, ADI-15878, and EBOV-520). Meanwhile, antibodies CA45 and 6D6 originated from an immunized non-human primate [60] and mouse [61], respectively.
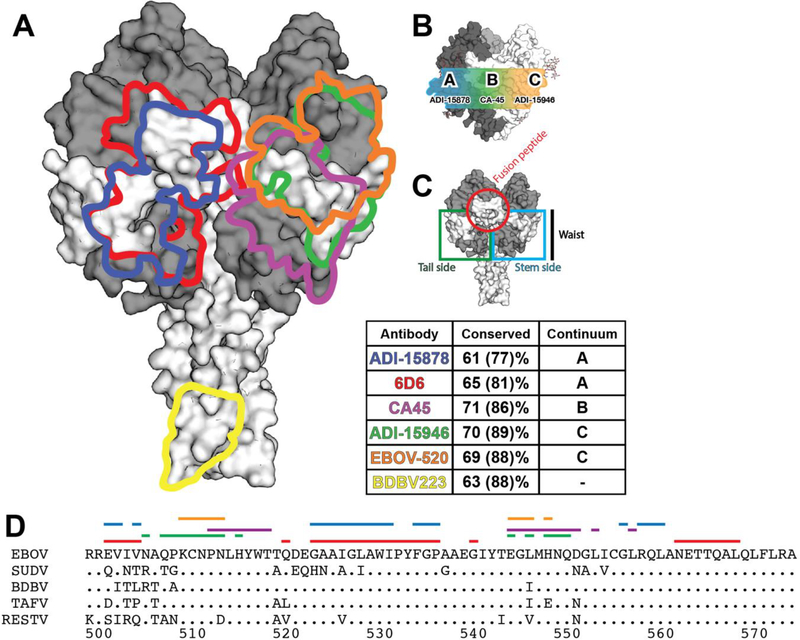
Notably, five of the six cross-reactive antibodies recognize epitopes that include at least part of the IFL (Figure 1). This feature was perhaps not surprising given the high sequence conservation of the IFL among ebolavirus GPs: 63% sequence identity within the IFL compared to 41% identity for the overall GP. These epitopes involving the IFL span horizontally across a central portion of the GP molecule, termed the “waist”, and have somewhat distinct footprints, termed positions A-C (Figure 2) [30]. The site located on the corner of GP that lies at the intersection of sites A and C typically promotes elicitation of more strain-specific antibodies [17,29,39].
Figure 2.
Antibody footprints. (A)
Among the six broadly cross-reactive antibodies, 6D6 and ADI-15878 have the broadest neutralization activity. Both target the IFLloop (Position A) along the GP waist. The crystal structure of ADI-15878 in complex with EBOV GP revealed that this antibody binds a hydrophobic pocket that is normally hidden beneath the N-terminal tail of GP2 [30]. The CDRs H3 and H2 of ADI-15878 reach underneath an N-linked glycan at N563 [30] and into the pocket where W99 of CDR H3 and L54 of CDR H2 form close hydrophobic contacts. The binding of ADI-15878 into this cryptic N-terminal pocket rather than on top of the GP2 N-terminal tail that typically covers the pocket is likely critical to the broad reactivity since the amino acid sequence of the pocket is highly conserved, whereas the N-terminal tail sequence is highly divergent.
6D6, imaged by electron microscopy in complex with EBOV GP, has a similar footprint to ADI-15878 and identical pan-ebolavirus cross-reactivity. Although the currently available structure does not have sufficient resolution to determine precise amino acid contacts, the similar footprint and reactivity suggest that 6D6 likely also binds into the conserved N-terminal pocket and avoids the non-conserved N-terminal tail [62]. The 6D6 epitope includes most of the IFLloop, and likely engages more of the IFLloop than does ADI-15878 [62]. The IFLloop and the N-terminal pocket in site A are 60 and 86% identical (28 and 14% similar) across the ebolavirus genus.
CA45 was previously categorized as a fusion loop binder, although the structure reveals that it engages neither the loop portion of the IFL assembly nor the N-terminal pocket [63]. Instead, the majority of the CA45 epitope lies in the IFLstem region (site B) (Figure 2), which has a lower degree of sequence conservation compared to the fusion peptide, but still has 68% sequence identity (86% similarity) across ebolaviruses. CA45 also binds beneath the IFLstem of the GP fusion loop into a site referred to as the “DFF” cavity formed by D192, F193 and F194 [63,64]. The DFF cavity lies at the interface between GP1 and GP2 in the vicinity of the lower attachment site of the cathepsin cleavage loop, which was previously identified as a binding site for toremifene [64] and other small molecule inhibitors [65]. The CA45 epitope comprises equal parts of GP1 and GP2 (~50% buried molecular surface each subunit). The antibody residue that lies deepest in the cavity is F100a, which interacts via Van der Waals forces with the eleven hydrophobic side chains (six from GP2 and five from GP1) lining the pocket and a π-stacking interaction with GP2 residue Y517. This key F100a side chain is positioned almost precisely where the phenyl ring of toremifene is located in the drug-GP complex structure [64]. Although the mechanism of 6D6-mediated neutralization is unclear, the targeting of the DFF cavity by both antibodies and small molecules highlights the vulnerability of this GP epitope.
Isolated from the same survivor as ADI-15878, ADI-15946 neutralizes at least three of the ebolaviruses and binds the IFLstem between the fusion loop and the base, at a third major site on the GP waist, site C (Figure 2). ADI-15946 is unique among the other cross-reactive antibodies for which high resolution structures are available in that it binds into another conserved feature termed the 310 pocket, which is normally occupied by the β17-β18 loop of the GP1 glycan cap. ADI-15946 appears to outcompete the glycan cap as it also binds to uncleaved GP that retains the glycan cap and neutralizes virions bearing uncleaved GP. ADI-15946 has enhanced neutralization activity in the rVSV-EBOV system [ 55] when the glycan cap is removed by cleavage or when the glycan cap is repositioned following binding of an antibody that targets the β17-β18 loop termed FVM09 [66]. EBOV-520 has a similar footprint to ADI-15946 [58] ad also neutralizes both EBOV and BDBV. However, only EBOV-520 fully neutralizes SUDV (ADI-15946 weakly neutralizes SUDV), underscoring the relative variability of this epitope. A high-resolution structure of EBOV-520 is needed to illuminate the mechanisms by which binding at site C affords its greater neutralization potency toward SUDV.
Another epitope associated with cross-reactivity is the GP stalk/MPER. This region is highly conserved (72% identical, 92% similar) across ebolaviruses, and several neutralizing/protective antibodies have been raised that target this epitope. Also, this region appears to contain the only known linear epitope that is targeted by a cross-reactive antibody. The structure of the human survivor antibody BDBV223 in complex with BDBV GP has been determined by both negative stain EM and crystallography [59,67, (King et al., unpublished)]. BDBV223 targets a site that lies beneath the glycan linked to N618 and engages the GP stalk through several hydrogen bonds and a salt bridge to GP D624. SUDV bears a D624N substitution, and insertion of a D624N point mutation into the BDBV GP stalk abrogates BDBV223 binding [67]. The affinity afforded by the formation of a salt bridge between the antibody and the aspartic acid side chain in GP may be critical for neutralization. Comparison of the crystal structure of the Fab-epitope complex to the unbound (apo) Fab alone reveals that each heavy chain CDR of BDBV223 rearranges to bind the GP stalk through an induced fit mechanism (King et al., unpublished). The crystal structure also showed that BDBV223 binds only a single stalk at a time and that its mode of binding, in which CDR H3 wraps about the helical stalk, precludes formation of the close trimeric assembly observed for the unbound EBOV stalk [25,30,63,64]. Thus, BDBV223 binding appears to be incompatible with a compact trimeric stalk assembly. Moreover, binding of BDBV223 is incompatible with the proposed position of the GP spike in the viral membrane based on cryo-electron microscopy. Lifting or bending of the GP relative to the viral membrane may thus be required for BDBV223 anchoring, and antibody binding could stabilize an alternate conformation of the GP spike.
Although these antibodies are broadly cross-reactive with ebolaviruses, their activity does not extend to marburgviruses. Marburgvirus GPs are significantly divergent from ebolavirus GPs and share only ~30% sequence identity. Further, antibodies that neutralize marburgvirus infection target epitopes that are either unique to marburgvirus or are more exposed in marburgvirus compared to ebolavirus. Indeed, some neutralizing antibodies target a “wing” epitope in GP2 that only exists in marburgviruses due to the distinct location of the furin cleavage site in marburgvirus relative to the ebolaviruses that results in the inclusion of 65 residues in the marburgvirus GP2 N-terminus. The most potent neutralizing antibodies against marburgviruses target the receptor binding site in GP, a site that appears to be exposed to immune surveillance in marburgvirus infection but not ebolavirus infection. Analysis of sera from a human survivor of marburgvirus infection revealed an abundance of antibodies against the receptor-binding site [68], whereas such antibodies are exceedingly rare in survivors of natural ebolavirus infection. Further, crystal structures of EBOV and Ravn GPs show that while the glycan cap domain in EBOV is ordered and covers the receptor binding site [17,29], in marburgvirus the corresponding regions are disordered and do not mask the receptor-binding site [31].
Mechanism of neutralization
Filovirus GPs mediate receptor binding and conformational changes that drive fusion of target cell and virus membranes. Formation of GPCL following processing by cathepsin enzymes in the infected cell facilitates receptor binding by the ebolaviruses and may also promote conformational changes in GP and membrane fusion. Antibodies that mechanically interfere with virus entry may block any of these steps. Those antibodies that target the NPC1-C binding site, such as the panel elicited against marburgvirus, directly block receptor binding [31,68]. Curiously, the ebolavirus cross-reactive antibody EBOV-520 also blocks receptor binding, yet binds to the side of the GP assembly, not into the receptor-binding trough or in a manner that would sterically interfere with NPC-1 binding [58]. Determination of a high-resolution structure of EBOV-520 in complex with GP would illuminate its mechanism of neutralization.
The ebolavirus cross-reactive antibody CA45 binds in the location of the cathepsin cleavage loop, in site B of the GP waist. CA45, as well as ADI-15946 (site C) and ADI-15878 (site A) similarly interfere with cathepsin cleavage [57,58,60,62,67], but do not directly bind to the expected cleavage site [30].
Antibodies against different regions of the IFL may interfere with conformational changes associated with membrane fusion itself. Antibodies 6D6 and ADI-15878 that bind the hydrophobic IFLloop bridge the IFL to the rest of the GP core and likely prevent its separation from the GP complex and subsequent penetration into the target cell membrane. Antibodies against the IFL stem and base (site B (CA45) and site C (ADI-15946 and EBOV-520)) may function similarly. Although structures of filovirus GP in its pre-fusion and post-fusion conformations are available [14,15], little is understood about the triggers and refolding pathways associated with this conformational change. Thus, the precise mechanisms by which antibodies interfere with membrane fusion await further elucidation.
Vaccine importance
In addition to developing broadly protective therapeutics, designing a broadly protective vaccine is a top priority. Although the rVSV-EBOV vaccine appears to be effective against EBOV [69], whether this vaccine will also offer protection against other known ebolaviruses or variants is unclear. A population of antibodies elicited by this vaccine may be cross-reactive, as was seen for several human antibodies such as ADI-15878 and ADI-15946 that were elicited in Americans infected with Ebola virus and who were presumably filovirus naïve prior to being infected while caring for patients during the 2014–2016 outbreak. The majority of the antibody response to the EBOV vaccines currently deployed, however, is thought to be EBOV-specific.
No vaccines are yet approved for SUDV, BDBV or other ebolaviruses. Illuminating where the desired broadly reactive antibodies anchor illustrates sites that could be enhanced in future immunogens in order to improve the breadth of activity. First, the epitope of ADI-15878 (and potentially 6D6) demonstrates that avoidance of the GP2 N-terminal peptide and engagement of the N-terminal pocket is desirable for achieving broad cross-reactivity. Antibodies such as ADI-15878 may not be difficult to elicit by immunization as evidenced by the only 6% divergence in the heavy chain variable domain of ADI-15878 compared to its germline precursor [55]. Improved antigen design, such as an antigen that has a more flexible (or absent) N-terminal tail may further promote elicitation of this class of antibodies (Figure 3a–c). Second, ADI-15946 and EBOV-520 illustrate that the 310-pocket is another site of vulnerability that is normally occupied by the β17-β18 loop of the glycan cap. Designing an uncleaved ebolavirus GP with a non-binding or absent β17-β18 loop (or more simply using GPCL) as an antigen may be effective in raising this class of antibodies (Figure 3d–f). Finally, CA45 can access the DFF cavity that is normally occupied by the cathepsin cleavage loop (Figure 3g–i). This interaction is facilitated by F100a of the CA45 CDR H3 that appears to occupy a similar binding conformation as F194 of the cleavage loop [63]. Removal of the cathepsin cleavage loop may therefore be one approach for creating an immunogen that favors production of such antibodies. Of course, combining these strategies into a single antigen may help to elicit these types of broadly neutralizing antibodies from a single vaccine immunogen.
Figure 3.
Cryptic epitopes engaged by ADI-15946, ADI-15878, and CA45. (a) The N-terminal pocket (red) is shown on the surface of EBOV GP (PDB: 5JQ3 [60]) with the N-terminal tail removed. (b) The N-terminal tail engages the highly conserved N-terminal pocket directly through I504 and D506, likely impeding recognition by the immune system. (c) ADI-15878 engages the N-terminal pocket through heavy chain CDRs 1–3, most importantly with W103. (d) The 310-pocket (blue) is shown with the β17–β18 loop removed. (e) The β17–β18 loop engages the 310-pocket primarily through two hydrophobic-aromatic residues (F290 and W291). (f) ADI-15946 engages this pocket through CDR-H3, with three hydrophobic residues (W110, L111, and L112) localized in the binding pocket. (g) The DFF cavity targeted by CA45 is shown in cyan. This pocket is bound by the cathepsin cleavage loop (h) in apo-GP. CDR H3 of CA45 binds into this pocket (i) with F100a appearing to bind similarly to F194 of the cathepsin cleavage loop.
Conclusions:
Development of vaccines and therapeutics with broad activity against ebolaviruses and marburgviruses is a major goal of public health efforts. First-generation antibody therapeutics and vaccines are EBOV-specific [38–40,69,70], but were created before these cross-reactive antibodies were identified and these potential new vaccination strategies were revealed. Important next steps in the field will be use of these broadly reactive antibodies as therapeutics and as design templates to develop broadly protective vaccines.
Highlights:
Several structures are now available of broadly reactive antibodies in complex with GP
Many broadly reactive antibodies bind along the “waist” of GP in three primary competition groups
Several broadly reactive antibodies access cryptic epitopes on GP
Antibody-directed modifications of GP may enhance vaccine design
Acknowledgements:
The authors acknowledge NIAID grant U19109762 for the Viral Hemorrhagic Fever Immunotherapeutic Consortium for support. LBK acknowledges F30AI136410 and JCM acknowledges training grant 5T32AI007354-27 for additional support. This is manuscript #29779 from The Scripps Research Institute.
Columns are described from left to right. Listed antibodies are shown according to their originally published name. Neutralization and protection columns display neutralization/protection capacity against the five ebolavirus species (E: EBOV, B: BDBV, S: SUDV, T: TAFV, R: RESTV). Green indicates >70% neutralization/protection, yellow indicates >40%, red indicates <40%. White indicates that the neutralization/protection activity toward these species is not known. All protection data were from BALB/c mice experiments unless otherwise indicated. The Epitope column shows the multiple epitopes recognized by the antibody colored according to scheme shown on the crystal structure (right, PDB: 5JQ3). The colors indicate the location of key structural features on GP, and not the footprints of each antibody. The glycan cap, cathepsin cleavage loop, and N-terminal tail present in the crystal structure are not shown for clarity.
Footnotes
CA45= EBOV and SUDV: guinea pigs. BDBV results only published as cocktail.
EBOV-520= EBOV: BALB/c mice, SUDV: guinea pigs, BDBV: ferrets.
Footprints of cross-reactive antibodies overlaid on the surface of EBOV GP (PDB: 5JQ3 [64]) and colored according to the table inset. (B) Organization of the epitope continuum on the GP “waist”. (C) Relative locations of the GP2 N-terminal tail, the fusion peptide, and the IFLstem within the GP waist. (D) Sequence alignment of ebolavirus GPs along the IFL. Epitopes of the individual antibodies (within the IFL) are highlighted according to their respective color in (A). This chart illustrates contact residues only within the IFL and does not include contact residues in GP1 or other sections of GP2. The percentage of sequence conservation was calculated over the entire indicated epitope and the value in parentheses represents the percentage of sequence similarity.
The N-terminal pocket (red) is shown on the surface of EBOV GP (PDB: 5JQ3 [64]) with the N-terminal tail removed. (B) The N-terminal tail engages the highly conserved N-terminal pocket directly through I504 and D506, likely impeding recognition by the immune system. (C) ADI-15878 engages the N-terminal pocket through heavy chain CDRs 1–3, most importantly with W103. (D) The 310-pocket (blue) is shown with the β17-β18 loop removed. (E) The β17-β18 loop engages the 310-pocket primarily through two hydrophobic-aromatic residues (F290 and W291). (F) ADI-15946 engages this pocket through CDR-H3, with three hydrophobic residues (W110, L111, and L112) localized in the binding pocket. (G) The DFF cavity targeted by CA45 is shown in cyan. This pocket is bound by the cathepsin cleavage loop (H) in apo-GP. CDR H3 of CA45 binds into this pocket (I) with F100a appearing to bind similarly to F194 of the cathepsin cleavage loop.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Liam B. King, Email: lking@scripps.edu.
Jacob C. Milligan, Email: jacobmil@scripps.edu.
Brandyn R. West, Email: bwest@scripps.edu.
Sharon L. Schendel, Email: schendel@scripps.edu.
References:
- 1.Formenty P, Libama F, Epelboin A: Outbreak of Ebola hemorrhagic fever in the Republic of the Congo, 2003: a new strategy? Medecine Tropicale: Revue du Corps de Sante Colonial 2003, 63(3):291–295. [PubMed] [Google Scholar]
- 2.Shoemaker T, MacNeil A, Balinandi S, Campbell S, Wamala JF, McMullan LK, Downing R, Lutwama J, Mbidde E, Ströher U, et al. : Reemerging Sudan Ebola virus disease in Uganda, 2011. Emerg Infect Dis 2012, 18:1480–1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Albariño CG, Shoemaker T, Khristova ML, Wamala JF, Muyembe JJ, Balinandi S, Tumusiime A, Campbell S, Cannon D, Gibbons A, et al. : Genomic analysis of filoviruses associated with four viral hemorrhagic fever outbreaks in Uganda and the Democratic Republic of the Congo in 2012. Virology 2013, 442:97–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baron RC, McCormick JB, Zubeir OA: Ebola virus disease in southern Sudan: hospital dissemination and intrafamilial spread. Bull World Health Organ 1983, 61:997–1003. [PMC free article] [PubMed] [Google Scholar]
- 5.MacNeil A, Farnon EC, Wamala J, Okware S, Cannon DL, Reed Z, Towner JS, Tappero JW, Lutwama J, Downing R, et al. : Proportion of deaths and clinical features in Bundibugyo Ebola virus infection, Uganda. Emerg Infect Dis 2010, 16:1969–1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Towner JS, Sealy TK, Khristova ML, Albariño CG, Conlan S, Reeder SA, Quan P-L, Lipkin WI, Downing R, Tappero JW, et al. : Newly discovered ebola virus associated with hemorrhagic fever outbreak in Uganda. PLoS Pathog 2008, 4:e1000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Formenty P, Hatz C, Le Guenno B, Stoll A, Rogenmoser P, Widmer A: Human infection due to Ebola virus, subtype Cote d’Ivoire: clinical and biologic presentation. J Infect Dis 1999, 179 Supp 1:S48–53. 10.1086/514285 [DOI] [PubMed] [Google Scholar]
- 8.Geisbert TW, Jahrling PB, Hanes MA, Zack PM: Association of Ebola-related Reston virus particles and antigen with tissue lesions of monkeys imported to the United States. J Comp Pathol 1992, 106:137–152. [DOI] [PubMed] [Google Scholar]
- 9.Goldstein T, Anthony SJ, Gbakima A, Bird BH, Bangura J, Tremeau-Bravard A, Belaganahalli MN, Wells HL, Dhanota JK, Liang E, et al. : The discovery of Bombali virus adds further support for bats as hosts of ebolaviruses. Nat Microbiol 2018, doi: 10.1038/s41564-018-0227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO | Marburg virus disease – Uganda. 2017,
- 11.Sanchez A, Yang ZY, Xu L, Nabel GJ, Crews T, Peters CJ: Biochemical analysis of the secreted and virion glycoproteins of Ebola virus. J Virol 1998, 72:6442–6447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee J, Nyenhuis DA, Nelson EA, Cafiso DS, White JM, Tamm LK: Structure of the Ebola virus envelope protein MPER/TM domain and its interaction with the fusion loop explains their fusion activity. Proc Natl Acad Sci U S A 2017, 114:E7987–E7996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gregory SM, Harada E, Liang B, Delos SE, White JM, Tamm LK: Structure and function of the complete internal fusion loop from Ebolavirus glycoprotein 2. Proc Natl Acad Sci U S A 2011, 108:11211–11216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koellhoffer JF, Malashkevich VN, Harrison JS, Toro R, Bhosle RC, Chandran K, Almo SC, Lai JR: Crystal structure of the Marburg virus GP2 core domain in its postfusion conformation. Biochemistry 2012, 51:7665–7675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weissenhorn W, Carfí A, Lee KH, Skehel JJ, Wiley DC: Crystal structure of the Ebola virus membrane fusion subunit, GP2, from the envelope glycoprotein ectodomain. Mol Cell 1998, 2:605–616. [DOI] [PubMed] [Google Scholar]
- **16.Beniac DR, Booth TF: Structure of the Ebola virus glycoprotein spike within the virion envelope at 11 Å resolution. Sci Rep 2017, 7:46374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee JE, Fusco ML, Hessell AJ, Oswald WB, Burton DR, Saphire EO: Structure of the Ebola virus glycoprotein bound to an antibody from a human survivor. Nature 2008, 454:177–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee JE, Saphire EO: Neutralizing ebolavirus: structural insights into the envelope glycoprotein and antibodies targeted against it. Curr Opin Struct Biol 2009, 19:408–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Favier A-L, Gout E, Reynard O, Ferraris O, Kleman J-P, Volchkov V, Peyrefitte C, Thielens NM: Enhancement of Ebola Virus Infection via Ficolin-1 Interaction with the Mucin Domain of GP Glycoprotein. J Virol 2016, 90:5256–5269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kondratowicz AS, Lennemann NJ, Sinn PL, Davey RA, Hunt CL, Moller-Tank S, Meyerholz DK, Rennert P, Mullins RF, Brindley M, et al. : T-cell immunoglobulin and mucin domain 1 (TIM-1) is a receptor for Zaire Ebolavirus and Lake Victoria Marburgvirus. Proc Natl Acad Sci U S A 2011, 108:8426–8431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aleksandrowicz P, Marzi A, Biedenkopf N, Beimforde N, Becker S, Hoenen T, Feldmann H, Schnittler H-J: Ebola virus enters host cells by macropinocytosis and clathrin-mediated endocytosis. J Infect Dis 2011, 204 Suppl 3:S957–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nanbo A, Imai M, Watanabe S, Noda T, Takahashi K, Neumann G, Halfmann P, Kawaoka Y: Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLoS Pathog 2010, 6:e1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saeed MF, Kolokoltsov AA, Albrecht T, Davey RA: Cellular entry of ebola virus involves uptake by a macropinocytosis-like mechanism and subsequent trafficking through early and late endosomes. PLoS Pathog 2010, 6:e1001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM: Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science 2005, 308:1643–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *25.Bornholdt ZA, Ndungo E, Fusco ML, Bale S, Flyak AI, Crowe JE Jr, Chandran K, Saphire EO: Host-Primed Ebola Virus GP Exposes a Hydrophobic NPC1 Receptor-Binding Pocket, Revealing a Target for Broadly Neutralizing Antibodies. MBio 2016, 7:e02154–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **26.Wang H, Shi Y, Song J, Qi J, Lu G, Yan J, Gao GF: Structural basis of Ebola virus entry: viral glycoprotein bound to its endosomal receptor Niemann-Pick C1. 2016, doi: 10.2210/pdb5f18/pdb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller EH, Obernosterer G, Raaben M, Herbert AS, Deffieu MS, Krishnan A, Ndungo E, Sandesara RG, Carette JE, Kuehne AI, et al. : Ebola virus entry requires the host-programmed recognition of an intracellular receptor. EMBO J 2012, 31:1947–1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **28.Lee J, Nyenhuis DA, Nelson EA, Cafiso DS, White JM, Tamm LK: Structure of the Ebola virus envelope protein MPER/TM domain and its interaction with the fusion loop explains their fusion activity. Proc Natl Acad Sci U S A 2017, 114:E7987–E7996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dias JM, Kuehne AI, Abelson DM, Bale S, Wong AC, Halfmann P, Muhammad MA, Fusco ML, Zak SE, Kang E, et al. : A shared structural solution for neutralizing ebolaviruses. Nat Struct Mol Biol 2011, 18:1424–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **30.West BR, Moyer CL, King LB, Fusco ML, Milligan JC, Hui S, Saphire EO: Structural Basis of Pan-Ebolavirus Neutralization by a Human Antibody against a Conserved, yet Cryptic Epitope. MBio 2018, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *31.King LB, Fusco ML, Flyak AI, Ilinykh PA, Huang K, Gunn B, Kirchdoerfer RN, Hastie KM, Sangha AK, Meiler J, et al. : The Marburgvirus-Neutralizing Human Monoclonal Antibody MR191 Targets a Conserved Site to Block Virus Receptor Binding. Cell Host Microbe 2018, 23:101–109.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fusco ML, Hashiguchi T, Cassan R, Biggins JE, Murin CD, Warfield KL, Li S, Holtsberg FW, Shulenin S, Vu H, et al. : Protective mAbs and Cross-Reactive mAbs Raised by Immunization with Engineered Marburg Virus GPs. PLoS Pathog 2015, 11:e1005016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.King LB, West BR, Schendel SL, Saphire EO: The structural basis for filovirus neutralization by monoclonal antibodies. Curr Opin Immunol 2018, 53:196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO | Ebola vaccines, therapies, and diagnostics. 2015,
- **35.Saphire EO, Schendel SL, Fusco ML, Gangavarapu K, Gunn BM, Wec AZ, Halfmann PJ, Brannan JM, Herbert AS, Qiu X, et al. : Systematic Analysis of Monoclonal Antibodies against Ebola Virus GP Defines Features that Contribute to Protection. Cell 2018, 174:938–952.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dye JM, Herbert AS, Kuehne AI, Barth JF, Muhammad MA, Zak SE, Ortiz RA, Prugar LI, Pratt WD: Postexposure antibody prophylaxis protects nonhuman primates from filovirus disease. Proc Natl Acad Sci U S A 2012, 109:5034–5039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mire CE, Geisbert JB, Borisevich V, Fenton KA, Agans KN, Flyak AI, Deer DJ, Steinkellner H, Bohorov O, Bohorova N, et al. : Therapeutic treatment of Marburg and Ravn virus infection in nonhuman primates with a human monoclonal antibody. Sci Transl Med 2017, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **38.Qiu X, Wong G, Audet J, Bello A, Fernando L, Alimonti JB, Fausther-Bovendo H, Wei H, Aviles J, Hiatt E, et al. : Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature 2014, 514:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **39.Corti D, Misasi J, Mulangu S, Stanley DA, Kanekiyo M, Wollen S, Ploquin A, Doria-Rose NA, Staupe RP, Bailey M, et al. : Protective monotherapy against lethal Ebola virus infection by a potently neutralizing antibody. Science 2016, 351:1339–1342. [DOI] [PubMed] [Google Scholar]
- *40.Pascal KE, Dudgeon D, Trefry JC, Anantpadma M, Sakurai Y, Murin CD, Turner HL, Fairhurst J, Torres M, Rafique A, et al. : Development of clinical-stage human monoclonal antibodies that treat advanced Ebola virus disease in non-human primates. J Infect Dis 2018, doi: 10.1093/infdis/jiy285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mehedi M, Groseth A, Feldmann H, Ebihara H: Clinical aspects of Marburg hemorrhagic fever. Future Virol 2011, 6:1091–1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *42.Bornholdt ZA, Turner HL, Murin CD, Li W, Sok D, Souders CA, Piper AE, Goff A, Shamblin JD, Wollen SE, et al. : Isolation of potent neutralizing antibodies from a survivor of the 2014 Ebola virus outbreak. Science 2016, 351:1078–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **43.Zhao X, Howell KA, He S, Brannan JM, Wec AZ, Davidson E, Turner HL, Chiang C-I, Lei L, Fels JM, et al. : Immunization-Elicited Broadly Protective Antibody Reveals Ebolavirus Fusion Loop as a Site of Vulnerability. Cell 2017, 169:891–904.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *44.Flyak AI, Shen X, Murin CD, Turner HL, David JA, Fusco ML, Lampley R, Kose N, Ilinykh PA, Kuzmina N, et al. : Cross-Reactive and Potent Neutralizing Antibody Responses in Human Survivors of Natural Ebolavirus Infection. Cell 2016, 164:392–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wilson JA, Hevey M, Bakken R, Guest S, Bray M, Schmaljohn AL, Hart MK: Epitopes involved in antibody-mediated protection from Ebola virus. Science 2000, 287:1664–1666. [DOI] [PubMed] [Google Scholar]
- 46.Zhang Q, Gui M, Niu X, He S, Wang R, Feng Y, Kroeker A, Zuo Y, Wang H, Wang Y, et al. : Potent neutralizing monoclonal antibodies against Ebola virus infection. Sci Rep 2016, 6:25856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **47.Furuyama W, Marzi A, Nanbo A, Haddock E, Maruyama J, Miyamoto H, Igarashi M, Yoshida R, Noyori O, Feldmann H, et al. : Discovery of an antibody for pan-ebolavirus therapy. Sci Rep 2016, 6:20514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Holtsberg FW, Shulenin S, Vu H, Howell KA, Patel SJ, Gunn B, Karim M, Lai JR, Frei JC, Nyakatura EK, et al. : Pan-ebolavirus and Pan-filovirus Mouse Monoclonal Antibodies: Protection against Ebola and Sudan Viruses. J Virol 2015, 90:266–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reynard O, Volchkov VE: Characterization of a Novel Neutralizing Monoclonal Antibody Against Ebola Virus GP. J Infect Dis 2015, 212 Suppl 2:S372–8. [DOI] [PubMed] [Google Scholar]
- 50.Sobarzo A, Groseth A, Dolnik O, Becker S, Lutwama JJ, Perelman E, Yavelsky V, Muhammad M, Kuehne AI, Marks RS, et al. : Profile and persistence of the virus-specific neutralizing humoral immune response in human survivors of Sudan ebolavirus (Gulu). J Infect Dis 2013, 208:299–309. [DOI] [PubMed] [Google Scholar]
- 51.Takada A, Feldmann H, Stroeher U, Bray M, Watanabe S, Ito H, McGregor M, Kawaoka Y: Identification of protective epitopes on ebola virus glycoprotein at the single amino acid level by using recombinant vesicular stomatitis viruses. J Virol 2003, 77:1069–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maruyama T, Rodriguez LL, Jahrling PB, Sanchez A, Khan AS, Nichol ST, Peters CJ, Parren PW, Burton DR: Ebola virus can be effectively neutralized by antibody produced in natural human infection. J Virol 1999, 73:6024–6030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shedlock DJ, Bailey MA, Popernack PM, Cunningham JM, Burton DR, Sullivan NJ: Antibody-mediated neutralization of Ebola virus can occur by two distinct mechanisms. Virology 2010, 401:228–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *54.Misasi J, Gilman MSA, Kanekiyo M, Gui M, Cagigi A, Mulangu S, Corti D, Ledgerwood JE, Lanzavecchia A, Cunningham J, et al. : Structural and molecular basis for Ebola virus neutralization by protective human antibodies. Science 2016, 351:1343–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **55.Wec AZ, Herbert AS, Murin CD, Nyakatura EK, Abelson DM, Fels JM, He S, James RM, de La Vega M-A, Zhu W, et al. : Antibodies from a Human Survivor Define Sites of Vulnerability for Broad Protection against Ebolaviruses. Cell 2017, 169:878–890.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Erica Ollmann Saphire Sharon L. Schendel, Fusco Marnie L., Gangavarapu Karthik, Gunn Bronwyn M., et al. : Systematic analysis of monoclonal antibodies against Ebola virus GP defines features that contribute to protection. Submitted [date unknown], [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wec AZ, Herbert AS, Murin CD, Nyakatura EK, Abelson DM, Fels JM, He S, James RM, de La Vega M-A, Zhu W, et al. : Antibodies from a Human Survivor Define Sites of Vulnerability for Broad Protection against Ebolaviruses. Cell 2017, 169:878–890.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **58.Gilchuk P, Kuzmina N, Ilinykh PA, Huang K, Gunn BM, Bryan A, Davidson E, Doranz BJ, Turner HL, Fusco ML, et al. : Multifunctional Pan-ebolavirus Antibody Recognizes a Site of Broad Vulnerability on the Ebolavirus Glycoprotein. Immunity 2018, 49:363–374.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Flyak AI, Shen X, Murin CD, Turner HL, David JA, Fusco ML, Lampley R, Kose N, Ilinykh PA, Kuzmina N, et al. : Cross-Reactive and Potent Neutralizing Antibody Responses in Human Survivors of Natural Ebolavirus Infection. Cell 2016, 164:392–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhao X, Howell KA, He S, Brannan JM, Wec AZ, Davidson E, Turner HL, Chiang C-I, Lei L, Fels JM, et al. : Immunization-Elicited Broadly Protective Antibody Reveals Ebolavirus Fusion Loop as a Site of Vulnerability. Cell 2017, 169:891–904.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Furuyama W, Marzi A, Nanbo A, Haddock E, Maruyama J, Miyamoto H, Igarashi M, Yoshida R, Noyori O, Feldmann H, et al. : Discovery of an antibody for pan-ebolavirus therapy. Sci Rep 2016, 6:20514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **62.Milligan JC, Parekh DV, Fuller KM, Igarashi M, Takada A, Saphire EO: Structural Characterization of Pan-ebolavirus Antibody 6D6 Targeting the Fusion Peptide of the Surface Glycoprotein. J Infect Dis 2018, doi: 10.1093/infdis/jiy532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **63.Janus BM, van Dyk N, Zhao X, Howell KA, Soto C, Aman MJ, Li Y, Fuerst TR, Ofek G: Structural basis for broad neutralization of ebolaviruses by an antibody targeting the glycoprotein fusion loop. Nat Commun 2018, 9:3934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhao Y, Ren J, Harlos K, Jones DM, Zeltina A, Bowden TA, Padilla-Parra S, Fry EE, Stuart DI: Toremifene interacts with and destabilizes the Ebola virus glycoprotein. Nature 2016, 535:169–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ren J, Zhao Y, Fry EE, Stuart DI: Target Identification and Mode of Action of Four Chemically Divergent Drugs against Ebolavirus Infection. J Med Chem 2018, 61:724–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Howell KA, Brannan JM, Bryan C, McNeal A, Davidson E, Turner HL, Vu H, Shulenin S, He S, Kuehne A, et al. : Cooperativity Enables Non-neutralizing Antibodies to Neutralize Ebolavirus. Cell Rep 2017, 19:413–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Flyak AI, Kuzmina N, Murin CD, Bryan C, Davidson E, Gilchuk P, Gulka CP, Ilinykh PA, Shen X, Huang K, et al. : Broadly neutralizing antibodies from human survivors target a conserved site in the Ebola virus glycoprotein HR2–MPER region. Nature Microbiology 2018, doi: 10.1038/s41564-018-0157-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Flyak AI, Ilinykh PA, Murin CD, Garron T, Shen X, Fusco ML, Hashiguchi T, Bornholdt ZA, Slaughter JC, Sapparapu G, et al. : Mechanism of Human Antibody-Mediated Neutralization of Marburg Virus. Cell 2015, 160:893–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Henao-Restrepo AM, Camacho A, Longini IM, Watson CH, Edmunds WJ, Egger M, Carroll MW, Dean NE, Diatta I, Doumbia M, et al. : Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ça Suffit!). Lancet 2017, 389:505–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.PREVAIL II Writing Group, Multi-National PREVAIL II Study Team, Davey RT Jr, Dodd L, Proschan MA, Neaton J, Neuhaus Nordwall J, Koopmeiners JS, Beigel J, Tierney J, et al. : A Randomized, Controlled Trial of ZMapp for Ebola Virus Infection. N Engl J Med 2016, 375:1448–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]