1. Introduction
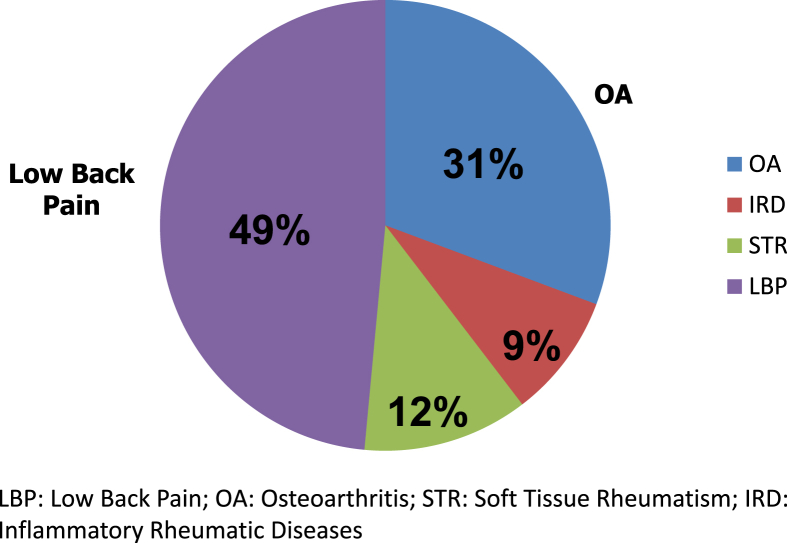
Low Back Pain (LBP) is a common clinical problem in out patient practice. LBP, osteoarthritis, soft tissue rheumatism and inflammatory rheumatic diseases constitute the ‘Big 4′ of rheumatology-four musculoskeletal conditions most commonly encountered in the community (Fig. 1). The importance of LBP can also be gauged by the following facts: nearly 75% of the population will have back pain at some time in their life, back symptoms are the most common cause of disability in the young and middle aged, back pain is the commonest occupational injury, and last but not the least, LBP is associated with substantial economic burden. Back pain can be acute, subacute or chronic LBP based upon duration (acute <1 month, subacute from 1 to 3 months, and chronic >3 months or if pain occurs episodically within a 6-month period).
Fig. 1.
“Big 4” of rheumatology.
2. Myths & facts
-
•
Acute LBP has a favorable natural history with most episodes resolving in a few weeks (Box 1).
-
•
Mechanical causes account for the majority (90%) of cases of LBP while systemic diseases account for only ∼10% cases (Box 2).
-
•
Nonspecific back pain (defined as back pain without signs of a serious underlying condition such as cancer, infection, cauda equina syndrome, spinal stenosis, radiculopathy, vertebral compression fracture or ankylosing spondylitis) is the commonest cause of mechanical LBP. Degenerative changes on lumbar imaging are usually considered nonspecific as they correlate poorly with symptoms.
-
•
Clues which point towards a serious/systemic disease, are enumerated in Box 3.
-
•
Inflammatory back pain can be very often differentiated from mechanical back pain on clinical grounds (Table 1)
-
•
Inflammatory LBP is typical of spondarthritides (SpA). These conditions are characterized by male preponderance; HLA B27 positivity; asymmetric oligoarthritis involving large joints of lower limbs; absence of rheumatoid factor and sacroiliitis.
-
•
Red flag signs in LBP include saddle anesthesia, bladder/bowel involvement, asymmetric loss of deep tendon reflexes, pulse inequality, hypotension or circulatory instability. These mandate search for underlying conditions like cauda equina syndrome, epidural abscess, rupture of aortic aneurysm or dissection of aorta etc.
-
•
Malignancy as a cause of LBP is very uncommon (only 1 in 1000 patients).
-
•
Sciatica (LBP with radiation below the knee) suggests nerve root compromise due to mechanical pressure. A straight leg raise (SLR) is reproduction of the patient's sciatica between 30 and 70° of leg elevation and has a relatively high sensitivity (91%) but modest specificity (26%) for diagnosing herniated disc. The crossed SLR test (when the unaffected leg is lifted) is more specific (88%) but less sensitive (29%).
-
•
Chronic LBP may be due to psychological reasons or malingering - a diagnosis of exclusion to be entertained only if physical causes have been carefully excluded.
-
•
Investigations in LBP should be kept to a minimum except in patients with neurologic deficits or where serious/systemic disease is suspected. Over reliance on radiographs/imaging should be avoided (Box 4).
-
•
Patients with nonspecific low back pain should be advised to remain active. Bed rest is counterproductive both in acute and chronic LBP.
-
•
Epidural steroids and traction are not recommended in acute LBP.
-
•
Surgical intervention is needed in a small proportion of patients. Surgical intervention based only on radiologic findings is often unsuccessful and is best avoided.
Box 1. Natural History of Acute Low Back Pain.
-
•
40% cases recover within 1 week
-
•
80% cases recover within 3 weeks
-
•
90% cases recover within 6 weeks
-
•
Only 7–10% cases experience symptoms for >6 months
-
•
Only 1% cases require surgical intervention.
Box 2. Causes of Low Back Pain.
| Mechanical 90% | Systemic/Inflammatory/Infectious Diseases 10% |
|---|---|
|
|
Box 3. When to suspect Systemic/Serious Disease as a cause of LBP.
-
•
Fever and weight loss
-
•
Pain with recumbency/Nocturnal Pain
-
•
Morning stiffness ≥1 hour
-
•
Localised bone pain
-
•
Visceral Pain, abdominal mass, rectal mass
-
•
Age >50 years
-
•
Previous history of cancer
-
•
Sphincter incontinence/Neurological deficit
Table 1.
Differentiating inflammatory from mechanical LBA
| Mechanical | Inflammatory | |
|---|---|---|
| Example | PIVD | SpA |
| Onset | May be acute | Insidious |
| Age | Any age | Usually <40 years |
| Morning stiffness | ± | +++ |
| Exercise | Aggravates | Relieves |
| Rest | Improves | Worsens |
| Other features | APRs normal | Buttock ache, other joints, eyes, APRs increased |
PIVD= Prolapse intervertebral disc; SpA = Spondyloarthritis; APR = Acute phase reactants.
Box 4. Why overreliance on imaging in LBP should be avoided.
-
•
Patients with back pain of mechanical origin often have normal x-rays
-
•
In patients <50 years of age the yield of abnormal findings is 1:2500
-
•
Patients with impressive radiologic abnormalities may be totally asymptomatic
-
•
Evident radiographic abnormalities are often not responsible for symptoms
-
•
Congenital abnormalities frequently seen on radiographs like spina bifida, Schmorl's nodes are unlikely causes of back pain
-
•
After the age of 50, nearly two-thirds of normal individuals show degenerative changes
-
•
Nearly 2/3rd patients with radiographic evidence of lumbar disc degeneration are asymptomatic
-
•
Significant radiation
Conflicts of interest
Nil.