Abstract
Objectives
In recent years, the increase in utilisation of bone substitutes in the reconstruction of bone defects has been fuelled by donor site complications associated with autologous bone harvesting. However the ability of bone substitute to stimulate bone union while maintaining fracture reduction has been a topic of debate. Cerament Bone Void Filler (CBVF) is a novel biphasic and injectable ceramic bone substitute that has high compressive strength and the ability to promote cancellous bone healing.
Materials and Method
This is a retrospective study to evaluate the surgical outcome of utilising CBVF in the treatment of depressed metaphyseal bone fractures over a two year period. The patients were followed up for at least six months after surgery and clinical parameters such as wound site complications were collated. Radiographic imaging was evaluated to determine loss of fracture reduction and rate of cement resorption.
Results
Thirteen patients with depressed metaphyseal fractures were enrolled, which included: (i) one proximal humerus fracture; (ii) three tibial plateau fractures; and (iii) nine calcaneal fractures. None of the patients showed significant collapse in fracture reduction after six months of follow up. Cement resorption was noted in one patient as early as three weeks after surgery. There were no cases of cement leak or wound site complications.
Conclusion
Cerament Bone Void Filler (CBVF) is a promising bone graft substitute in the management of depressed metaphyseal bone fractures, with the ability to maintain fracture reduction despite cement resorption.
Keywords: Cerament, Bone cement, Metaphyseal fracture
1. Introduction
Depressed metaphyseal fractures often result in significant bone defects after anatomical reduction. Autologous iliac bone graft has been considered the gold standard in the filling of bone voids due to its favourable osteogenic, osteoconductive and osteoinductive properties.1
However, the increase in operative time and complications associated with autologous bone graft harvesting such as bleeding, fracture, infection and donor site pain have fuelled the search for a better alternative.
Allograft is a viable option to autologous bone graft in filling bone defects. However there are concerns regarding the potential for infectious diseases transmission and unpredictable structural strength during preparation.
Synthetic bone substitutes have gained popularity among orthopaedic surgeons over the years as they have undergone significant improvements in their biological and biomechanical properties.
Cerament Bone Void Filler (CBVF) is a novel biphasic ceramic bone substitute which is composed of 60% calcium sulphate (CS) and 40% hydroxyapatite (HA) mixed with water soluble radio-contrast agent iohexol to form an injectable paste. It has high compressive strength and the ability to promote cancellous bone in-growth.2
The aim of this study is to evaluate the effectiveness of CBVF in maintaining fracture reduction and any associated complications in the treatment of depressed metaphyseal fractures in our institution.
2. Materials and Methodology
This is a retrospective review of patients who sustained depressed metaphyseal fractures requiring surgical fixation and the use of CBVF. These patients were admitted to a level one trauma centre under the care of a single primary fellowship-trained surgeon over a two years period from January 2015 to December 2016. The study was conducted with ethics approval from Institution Review Board.
Patients who sustained calcaneal fractures, tibial plateau fractures or proximal humerus fractures were included in our study.
Clinical notes were reviewed at least 6 months postoperatively to document any complications. Radiographic imaging was obtained during each follow up to monitor loss of fracture reduction and cement resorption. We measured Bohler's angle in calcaneal fracture cases, step deformity in tibial plateau cases, and angle of inclination in proximal humerus cases.
3. Results
A total of 13 patients with depressed metaphyseal fractures were enrolled, which included: (i) one proximal humerus fracture; (ii) three tibial plateau fractures; and (iii) nine calcaneal fractures. The median age for our study was 46 years old. Six patients sustained their injury during work while 7 cases were non-work related injury.
Among the 9 patients who sustained calcaneal fractures, there were 2 Sanders II and 7 Sanders III calcaneal fractures. One patient sustained a twisting injury and 8 patients sustained the injury from accidental fall from height. Four patients underwent percutaneous fixation and 5 patients underwent open reduction and internal fixation via a lateral extensile approach.
One patient, who was a tourist, was lost to follow up as she returned to her country after operation. Complete cement resorption was observed as early as 4 weeks after operation and latest by 14 weeks after operation, with an average of 9.75 weeks. Patients started full weight bearing mobilisation as early as 4 weeks after operation and an average of 6 weeks. We found no statistical significance (p > 0.05) between immediate post operative angle and their corresponding angles on subsequent follow ups for all the patients, indicating no significant loss of reduction.
Among the 3 patients who sustained tibial plateau fractures, 2 patients sustained Schatzker II tibial plateau fractures while the other patient sustained a Schatzker V tibial plateau fracture. All patients fell from height.
One of the 2 patients who sustained Schatzker II tibial plateau fractures was a tourist and returned to his native country one month after surgery. Xray was performed 1 month after surgery for him and showed no loss of fracture reduction.
The 2 other patients who sustained tibial plateau fractures started full weight bearing mobilisation as early as 6 weeks after operation and an average of 7.5 weeks. Complete resorption of cement was observed as early as 9 weeks after operation and an average of 10.5 weeks, with no joint subsidence noted.
The patient who sustained a three-part proximal humerus fracture underwent open reduction and plate fixation. The angle of inclination noted during the latest follow up was 138° with no significant change throughout her follow up duration. Cement resorption was noted as early as 3 weeks with no loss of fracture reduction.
None of the patients experienced cement leakage, complex regional pain syndrome, neuroma or exostosis formation. Soft tissue complications such as wound infection and wound dehiscence were also not encountered.
4. Discussion
The popularity of bone substitutes as a viable alternative to autologous bone grafting has propelled research and development in terms of their efficacy and safety profile. These brought about improved biomechanical and biological properties, as well as more favourable side effects and complications.
In a prospective randomised controlled trial by Russell et al., the authors evaluated the use of bioabsorbable calcium phosphate bone substitute and autologous iliac bone graft for defect augmentation in tibial plateau fracture and concluded that bone substitute had lower subsidence rate than bone graft.3 The lower rate of loss of fracture reduction was also echoed in a meta-analysis of randomised controlled trials conducted by Bajammal et al.4
Bone substitute also demonstrated higher fatigue strength and ultimate load than bone graft in a cadaveric study conducted by McDonald et al.5
The recent Cochrane review by McNamara et al.6 on the surgical fixation methods for tibial plateau fractures concluded that patients experienced prolong pain from harvest site in the autologous iliac bone graft group and the evidence did not contradict the use of bone substitutes.
Cerament Bone Void Filler (CBVF) is a novel biphasic ceramic bone substitute that aims to emulate bone remodelling properties with the penetration of nutrients and growth factors into its microporous hydroxyapatite construct during the resorption of the calcium sulphate component. This leads to infiltration of osteoclasts and macrophages, resulting in early bone in-growth.7,8
Lundusi et al.9 and Rauschmann et al.10 demonstrated that Cerament was able to provide sufficient mechanical support and stability in tibial plateau fractures and vertebral fractures respectively. In the former study, cement resorption was complete after an average of 5 months ranging between 3 and 8 months.
Cerament bone cement resorption was demonstrated as early as 3 weeks with an average time of 9.27 weeks in our series. The rate of cement resorption was much faster than described by other authors. We postulated the increase in resorption rate to early mobilisation and the tropical climate in our country.
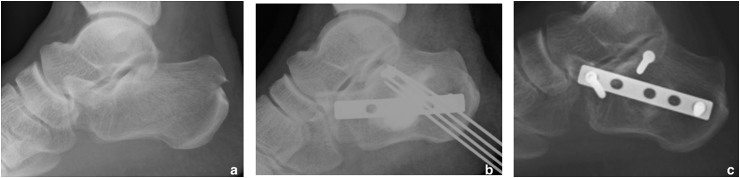
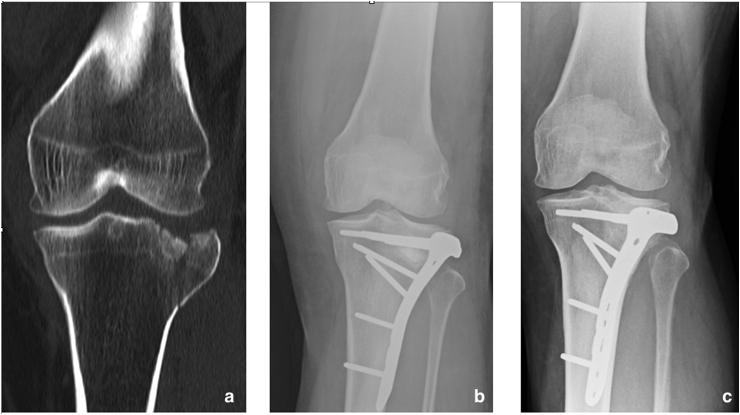
Many fear joint subsidence in the use of bone substitutes especially with calcium sulphate cements due to the more rapid resorption rate. In our series, we observed that there was no significant loss of fracture reduction with the use of CBVF even when we mobilised our patients as early as 4 weeks for calcaneal fractures and 6 weeks for tibial plateau fractures (Fig. 1, Fig. 2). Our study may provide basis that Cerament emulates bone remodelling with the infiltration of osteoclasts and macrophages, resulting in early bone in-growth and higher fatigue strength.
Fig. 1.
Calcaneal fracture. (a) Pre-op, (b) immediate post op, (c) 9 moths follow up.
Fig. 2.
Tibial Plateau fracture (a) pre-op, (b) Immediate post op, (c) 8 months follow up.
In our literature review, we noted that many studies evaluated the use of Cerament for tibial plateau fracture and spine augmentation.3,5,7,10 In our series, we extended the use of Cerament to calcaneal and proximal humerus fractures. The ease of use and ability to maintain fracture reduction made Cerament a suitable bone substitute option in our management of these fractures.
Calcaneal and tibial plateau fractures commonly affect economically viable patients and hence early mobilisation with no significant joint subsidence allows earlier return to work for these patients. Cost analysis was not performed in our series. However, earlier return to work would result in the reduction in loss of income that could offset the higher initial cost for Cerament.
Safety is one of the concerns in the usage of bone cement. Complications due to the effect of bone void filler to the surrounding tissue were not encountered in our series. We did not experience any complication from cement leakage, wound infection or dehiscence.
Our study is limited by its small sample size and heterogenous sample resulting in minimal power analysis. Due to the inherent characteristic of our patient group where follow up would be terminated once settlement of workman compensation, we were not able to evaluate long term clinical outcome and complications associated with the use of CBVF. Further well designed, randomised controlled trials are still warranted to validate these results.
5. Conclusion
With the data presented in our study, Cerament Bone Void Filler (CBVF) has shown to be a promising bone graft substitute in the management of metaphyseal bone fractures. It is able to maintain fracture reduction despite early cement resorption and mobilisation.
Conflicts of interest
Quan You Yeo and Ernest Beng Kee Kwek declare that they have no conflict of interest.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jcot.2018.08.014.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Keating J.F., McQueen M.M. Substitutes for autologous bone graft in orthopaedic trauma. J Bone Joint Surg Br. 2001;83:3–8. doi: 10.1302/0301-620x.83b1.11952. [DOI] [PubMed] [Google Scholar]
- 2.Nusselt T., Hofmann A., Wachtlin D., Gorbulev S., Rommens P.M. CERAMENT treatment of fracture defects (CERTiFy): protocol for a prospective, multicenter, randomized study investigating the use of CERAMENT™ bone void filler in tibial plateau fractures. Trials. 2014;15:75. doi: 10.1186/1745-6215-15-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Russell T.A., Leighton R.K., Alpha B.S.M.T.P.F.S.G. Comparison of autogenous bone graft and endothermic calcium phosphate cement for defect augmentation in tibial plateau fractures. A multicenter, prospective, randomized study. J Bone Joint Surg Am. 2008;90:2057–2061. doi: 10.2106/JBJS.G.01191. [DOI] [PubMed] [Google Scholar]
- 4.Bajammal S.S., Zlowodzki M., Lelwica A., Tornetta P., 3rd, Einhorn T.A., Buckley R. The use of calcium phosphate bone cement in fracture treatment: a meta-analysis of randomized trials. J Bone Joint Surg Am. 2008;90:1186–1196. doi: 10.2106/JBJS.G.00241. [DOI] [PubMed] [Google Scholar]
- 5.McDonald E., Chu T., Tufaga M., Marmor M., Singh R., Yetkinler D. Tibial plateau fracture repairs augmented with calcium phosphate cement have higher in situ fatigue strength than those with autograft. J Orthop Trauma. 2011;25:90–95. doi: 10.1097/BOT.0b013e3181e3e28f. [DOI] [PubMed] [Google Scholar]
- 6.McNamara I.R., Smith T.O., Shepherd K.L. Surgical fixation methods for tibial plateau fractures. Cochrane Database Syst Rev. 2015;9 doi: 10.1002/14651858.CD009679.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hatten H.P., Jr., Voor M.J. Bone healing using a bi-phasic ceramic bone substitute demonstrated in human vertebroplasty and with histology in a rabbit cancellous bone defect model. Intervent Neuroradiol. 2012;18:105–113. doi: 10.1177/159101991201800114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abramo A., Geijer M., Kopylov P., Tägil M. Osteotomy of distal radius fracture malunion using a fast remodeling bone substitute consisting of calcium sulfate and calcium phosphate. J Biomed Mat Res B Applied Biomaterials. 2010;92:281–286. doi: 10.1002/jbm.b.31524. [DOI] [PubMed] [Google Scholar]
- 9.Lundusi R., Gasbarra E., D'Arienzo M., Piccioli A., Tarantino U. Augmentation of tibial plateau fractures with an injectable bone substitute: CERAMENT™. Three year follow-up from a prospective study. BMC Muscoskel Disord. 2015;16:115. doi: 10.1186/s12891-015-0574-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rauschmann M., Vogl T., Verheyden A., Pflugmacher R., Werba T., Schmidt S. Bioceramic vertebral augmentation with a calcium sulphate/hydroxyapatite composite (Cerament™ SpineSupport) in vertebral compression fractures due to osteoporosis. Eur Spine J. 2010;19(6):887–892. doi: 10.1007/s00586-010-1279-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.